Abstract
Objective
The aim of this study was to evaluate whether periodontal treatment in patients with periodontitis and hyperlipidemia may have any influence on plasma lipids and pro-inflammatory cytokine levels.
Material and methods
We randomly assigned 109 patients with hyperlipidemia and chronic periodontitis into group 1 (n = 55) and group 2 (n = 54). Patients in group 1 underwent a standard cycle of supragingival mechanical scaling and polishing. Patients in group 2 underwent the adjunctive full-mouth intensive removal of subgingival dental plaque biofilms with the use of scaling and root planning. Periodontal parameters, total cholesterol (TC), triglyceride (TRG), high-density lipoprotein cholesterol (HDL-C), low-density lipoprotein cholesterol (LDL-C), tumor necrosis factor-alpha (TNF-α), interleukin(IL)-1β(IL-1β), and IL-6 were evaluated before treatment and 2 and 6 months after treatment.
Results
Two and 6 months after treatment, TRG levels were significantly lower in group 2 than in group 1 (P < 0.05), and the levels of HDL-C were significantly higher (P < 0.05). Two and 6 months after therapy, the levels of TNF-α were significantly lower in group 2 than in group 1 (P < 0.05), as were the levels of IL-1β (P < 0.001) and IL-6 (P < 0.001).
Conclusions
Intensive periodontal treatment of participants with hyperlipidemia and chronic periodontitis improved serum lipid levels and decreased circulating pro-inflammatory cytokine levels.
Clinical relevance
This study showed that intensive treatment of periodontitis results in an improvement in serum lipid levels and a decrease in serum proinflammatory cytokine levels in patients with periodontitis and hyperlipidemia. These findings may contribute to present knowledge that periodontal therapy may be beneficial for individuals with hyperlipidemia.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Cardiovascular disease is set to become the major cause of death worldwide [1]. The serum lipid profile is a major risk factor for developing a risk of cardiovascular disease. Hyperlipidemia is considered as one of the major cardiovascular disease risk factors [2].
Periodontitis is induced by bacterial plaque, which accumulates on the tooth surface and stimulates a host response in the adjacent gingiva that can lead to the destruction of connective tissue and bone surrounding the tooth [3]. Clinical signs of the disease are often seen in middle age, and it is a very common disease in adults.
Recent epidemiological reports suggest that periodontitis is one of the key risk factors for the onset of cardiovascular diseases [4–6]. On the other hand, a causal relation has been demonstrated between high serum lipid levels and periodontitis. Recent studies illustrate the existence of a relation between periodontal disorders and hyperlipidemia, which power the probable effect of periodontal disease as an underlying factor for hyperlipidemia [7–9]. Periodontitis-induced bacteremia and endotoxemia have been shown to cause an elevation of serum proinflammatory cytokines, such as TNF-α, IL-1β, and IL-6, which were demonstrated to produce alterations in lipid metabolism, leading to hyperlipidemia [10].
We hypothesized that the removal of the infectious and inflammatory burden of periodontal disease through periodontal therapy could be associated with an improvement in serum lipid profile. The aim of the present study was to evaluate whether periodontal treatment with scaling and root planning supplemented with chlorhexidine in patients with periodontitis and hyperlipidemia may have any influence on plasma lipids and systemic proinflammatory cytokine levels.
Material and methods
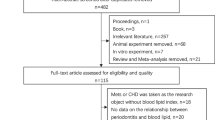
This was a parallel-group, single-blind, randomized, and controlled trial of 6-month duration. The study design is summarized in Fig. 1. The protocol was approved by the Ethical Committee of the First People’s Hospital of Lianyungang City. After being informed on the purpose of the study, the patients signed informed consent forms. Research was conducted according to the principles outlined in the Declaration of Helsinki on experimentation involving human subjects.
Subjects
Subjects were recruited from patients seeking treatment at the First People’s Hospital of Lianyungang City. One hundred nine subjects diagnosed with hyperlipidemia and moderate-to-advanced chronic periodontitis were recruited for the study. The criteria for inclusion in the study were the following: (1) Subjects had to meet at least one of the following criteria for the diagnosis of hyperlipidemia: triglyceride (TRG) levels >2.26 mmol/L; high density lipoprotein cholesterol (HDL-C) levels <1.04 mmol/L; or low density lipoprotein cholesterol (LDL-C) levels >4.14 mmol/L and (2) the presence of ≥20 scorable teeth and the diagnosis of adult chronic periodontitis with the presence of at least four teeth with a probing depth (PD) >4 mm, clinical attachment loss (AL) ≥2 mm, and radiographic evidence of bone loss.
Exclusion criteria included systemic illnesses (i.e., diabetes mellitus, cancer, human immunodeficiency syndrome, bone metabolic diseases, or disorders that compromise wound healing, radiation, or immunosuppressive therapy), pregnancy or lactation, systemic antibiotics taken within the previous 6 months, use of cholesterol reduction medication during the past 6 months, and subgingival scaling and root planing or surgical periodontal therapy in the last year.
A baseline periodontal examination was performed, and complete medical and dental histories were collected by a blind examiner. Current smokers were defined as participants who smoked at least one cigarette per day, former smokers as those who had stopped smoking more than 1 year before the study began, and never smokers as those who had never smoked in their life. Patients were randomly assigned with the use of a computer-generated table into group 1 (n = 55) and group 2 (n = 54). Allocation was concealed by the use of opaque envelopes, which were opened by the therapist on the day the treatment was administered. All individuals were evaluated at the baseline and at 2 and 6 months after periodontal treatment.
Periodontal examination and therapy
Periodontal data were recorded by a single examiner, who was unaware of the treatment assignments, at base line and 2 and 6 months after administration of the therapy. The following data will be recorded: (1) Number of present teeth. (2) Bleeding on probing (BOP), the presence of BOP will be expressed as yes/no at each site. The extent of BOP will be reported as a percentage of all sites. (3) Probing pocket depth (PD), distance in millimeters from the gingival margin to the periodontal pocket as measured with a calibrated periodontal probe. (4) Gingival margin level (GML), distance in millimeters from the cemento-enamel junction (CEJ) to the gingival margin. (5) Clinical attachment level (CAL), distance in millimeters from the CEJ to the deepest aspect of the periodontal sulcus or pocket.
PD, GML, and CAL will be recorded at six sites per tooth. PD and CAL will be reported in each patient as follows: (1) mean PD and (2) mean CAL. The number of sites per patient with PD ≥ 4 mm and BOP was determined for each examination. Persisting pockets ≥4 mm with BOP are commonly perceived as needing additional treatment in clinical practice.
All patients were given instructions in basic oral hygiene. Patients in group 1 received a conventional adult prophylaxis, consisting in one session of supragingival removal of plaque biofilm with the use of mechanical scaling and coronal polishing. Patients in group 2 will be treated using the one-stage full-mouth disinfection protocol consisting in the following procedures: (1) Administration of local anesthesia (lidocaine (1 %) with epinephrine). (2) Scaling and root planing with ultrasonic devices and curettes, four quadrants in one session. (3) Tongue brushing with a 1 % chlorhexidine gel (1 min). (4) Mouth rinsing with a 0.2 % chlorhexidine solution (2 min). (5) Subgingival chlorhexidine (1 %) irrigation in all pockets. (6) Twice daily rinsing with chlorhexidine (1 min) during 14 days after the periodontal intervention.
Patients in group 1 were treated in exactly the same manners as described for group 2 only after completion of this 6-month study. Consequently, group 1 acted as a control group for the duration of the study but was not denied further treatment in the longer term. Patients in whom periodontal disease progressed received immediate care from a periodontist and were withdrawn from this study.
Biochemical assessments
Biochemical assessments were performed in baseline and at 2 and 6 months after periodontal treatment. Blood samples were collected to measure TRG, total cholesterol (TC), LDL-C, HDL-C, TNF-α, IL-1β, and IL-6. The samples were obtained after a 12-h fasting period from an antecubital vein. Biochemical assessments were performed in the Clinical Biochemistry Laboratory of the First People’s Hospital of Lianyungang City. Serum lipid levels were determined by using routine enzymatic methods. Serum levels of TNF-α, IL-1β, and IL-6 were measured by enzyme-linked immunosorbent assay (ELISA) (Quantikine HS, R&D Systems).
Outcomes
The primary outcomes were the differences in serum lipid parameters at baseline and at 2 and 6 months after periodontal treatment. Secondary outcomes were the between-group differences in proinflammatory cytokine levels and periodontal parameters (Time frame: Baseline, 2 and 6 months after periodontal treatment).
Statistical analysis
Power analysis and sample size estimation were performed. We calculated that a minimum of 108 patients would be need to enrolled to detect a difference of 0.3 mmol/L in TC level between the two treatment groups, with a standard deviation of the mean difference of 0.7 mmol/L at a two-sided alpha level of 5 and 90 % power [11]. The software Power Analysis and Sample Size (NCSS/PASS, version 13.0.6; NCSS, Kaysville, UT, USA) was used to perform the sample size calculation. All statistical analyses were performed using the intention-to-treat principle. Continuous, normally distributed variables were reported as mean ± standard deviation (SD). Baseline characteristics of the patients were compared between the two groups using independent t test for normally distributed variables and chi-square test for categorical variables. We performed a repeated-measures analysis of variance (ANOVA) to determine differences in the primary outcome and secondary outcomes between the two groups and over time, using a conservative F test for the interaction between time and treatment group. The Greenhouse-Geisser correction for the F test was used to adjust the degrees of freedom for deviation from sphericity. Logarithmic transformation of the data was performed when appropriate, and post hoc Fisher’s paired and unpaired tests of least-significant difference were performed and interpreted with the use of the Bonferroni-Holm adjustment for multiple comparisons. A two-side P value <0.05 was considered statistical significant. The statistical analysis was performed using statistical software (SPSS, version 17.0; SPSS Inc., Chicago, IL, USA).
Results
After applying the inclusion and exclusion criteria, 121 patients with advanced chronic periodontitis and hyperlipidemia met the recruitment criteria. Of these 121 patients, 12 declined to participate. A total of 109 patients underwent randomization, of whom 98 (50 assigned to group 1 and 48 to group 2) completed the trial, attending all study visits. No patients reported any adverse events or side-effects during the study.
Patient characheristics
The baseline characteristics are summarized in Table 1. At baseline age, sex, education level, smoking status, alcohol use, and body-mass index were all similar between the two groups (P > 0.05). During the study period, patients did not report changes in lifestyle issues, including exercise, diet, smoking, and medications.
Periodontal outcomes
The periodontal parameters at baseline and 2 and 6 months after periodontal therapy are indicated in Table 2. Repeated-measures ANOVA of the periodontal outcomes showed a significant interaction between treatment and time (P < 0.001). As compared with group 1, group 2 had lower PD and CAL values, as well as lower percentages of sites with BOP 2 months after therapy (P < 0.001) and 6 months after therapy (P < 0.001). Patients in group 2 had lower number of sites with PD ≥ 4 mm and BOP than those in group 1, 2 months after therapy (P < 0.001) and 6 months after therapy (P < 0.001). Similarly, patients in group 2 had lower percentages of sites with PD ≥ 4 mm than those in group 1, 2 months after therapy (P < 0.001) and 6 months after therapy (P < 0.001).
Serum lipid levels
Table 3 shows the serum lipid parameters of the study groups. Two and 6 months after treatment, TRG levels were significantly lower in group 2 than in group 1 (P < 0.05), and levels of HDL-C were significantly higher (P < 0.05). However, levels of TC and LDL-C were slightly, but not significantly lower in group 2 than in group 1, 2 months after therapy and 6 months after therapy.
Serum proinflammatory cytokine levels
The serum levels of TNF-α, IL-1β, and IL-6 at baseline and 2 and 6 months after periodontal therapy are presented in Table 4. Repeated-measures ANOVA of the serum cytokine levels showed a significant interaction between treatment and time (P < 0.05). Two and 6 months after therapy, levels of TNF-α were significantly lower in group 2 than in group 1 (P < 0.05), as were the levels of IL-1β (P < 0.001) and IL-6 (P < 0.001).
Discussion
This study showed that intensive treatment of periodontitis results in an improvement in serum lipid levels and a decrease in serum proinflammatory cytokine levels in patients with periodontitis and hyperlipidemia. Two and 6 months after treatment, TRG levels were significantly lower in group 2 than in group 1, and levels of HDL-C were significantly higher. Levels of TNF-α, IL-1β, and IL-6 were significantly lower in group 2 than in group 1, 2 months after therapy and 6 months after therapy.
In the present study, group 2 showed very good periodontal response to treatment; BOP, PD, and CAL showed a very significant improvement as were published in previous papers [12, 13]. Patients in group 2 had lower number of sites with PD ≥ 4 mm and BOP than those in group 1, 2 months after therapy and 6 months after therapy. This result could be associated with a lower additional treatment requirement throughout follow-up.
There are several studies regarding the effect of periodontal treatment on serum lipid levels in systemic healthy subjects with periodontitis. The results of these studies, however, are somewhat inconsistent. Lösche et al. in 2005 assayed plasma lipid concentration before and 3 months after periodontal therapy in 32 patients suffering from periodontitis. Although periodontal therapy resulted in dramatical decreases in local inflammation and tissue destruction, the difference between plasma lipid levels before and after treatment was not significant [14]. Pejcic et al. in 2011 measured concentration of lipids in patients with periodontitis before and 3, 6, and 12 months after local periodontal treatment. Periodontal therapy resulted in a significant reduction of local inflammation and tissue destruction. The levels of TC, LDL-C, and TRG were significantly decreased after treatment [15]. However, in another study conducted by D’Aiuto et al., lipid marker changes were insignificant between standard periodontal treatment and control groups, and some reductions of TC and LDL-C were present only in the intensive periodontal treatment group [11]. Earlier studies have produced inconsistent results as to whether periodontal therapy has an effect on lipoproteins levels. We assume that the factors that explain the inconsistencies are mainly related to study design, adjustment for confounder, and other methodological details. However, these studies have almost all been conducted in systemically healthy subjects with periodontitis.
To date, there are only two studies assessing the effect of periodontal treatment on serum lipid levels in patients with periodontitis and hyperlipidemia [16, 17]. In this present study, the periodontal treatment significantly changed the plasma levels of TRG and HDL-C. This is in agreement with the uncontrolled study in the literature that evaluated the effect of periodontal initial therapy on the serum level of lipid in subjects with periodontitis and hyperlipidemia [16]. In that study of 20 participants, the TC and TRG levels reduced significantly at 3 months after periodontal therapy comparing with baseline. At the same time, a significant increase of HDL-C was observed. However, in another study conducted by Oz et al., in the third month, there was a substantial decline in TC and LDL-C profiles in the treatment group and between the two groups [17]. In the current study, levels of TC and LDL-C were slightly, but not significantly lower in group 2 than in group 1, 2 months after therapy and 6 months after therapy.
Serum proinflammatory cytokines may play an important role in the association between periodontal disease and hyperlipidemia [18]. To our knowledge, there are currently no published studies assessing the effect that periodontal treatment has on the serum levels of TNF-α, IL-1β, and IL-6 in participants with periodontitis and hyperlipidemia. Periodontal therapy has been shown in several studies to decrease the levels of some proinflammatory cytokines. Most such studies employed conservative therapies such as scaling, root planing, and antibiotic treatment to show decreases in mediators such as TNF-α, IL-1β, and IL-6 [19–24]. However, some other investigations have reported controversial results [25–27]. Ide et al. [25] reported no statistically significant changes in the level of TNF-α, IL-1β, and IL-6 following a single course of periodontal treatment. In this current study, the periodontal treatment significantly decreased the levels of proinflammatory cytokines. Two and 6 months after therapy, levels of TNF-α were significantly lower in group 2 than in group 1, as were the levels of IL-1β and IL-6.
The mechanism by which periodontitis might affect serum lipid levels remains unclear. Periodontitis involves bacterial infection with a range of gram-negative, anaerobic bacteria that induce local and systemic elevations of pro-inflammatory cytokines such as tumor necrosis factor-alpha (TNF-α), interleukin (IL)-1β (IL-1β), and IL-6 [28, 29]. The pro-inflammatory cytokines might produce alterations in lipid metabolism, such as increased LDL-C and triglycerides, due to increased hepatic lipogenesis, lipolysis from adipose tissue, or reduced blood clearance [10].
In conclusion, the present short-term, randomized clinical trial shows that intensive periodontal treatment improves serum lipid levels and decreases serum proinflammatory cytokine levels in patients with hyperlipidemia and chronic periodontitis. Because of the small number of subjects examined, caution is warranted in generalizing this date to all patients affected by periodontitis. Moreover, environmental variables, such as eating and physical activity habits, and socioeconomic conditions can interfere with the study results, since they are confounders that are difficult to control. It is apparent that large-sized multicenter randomized controlled clinical trials are needed to confirm or reject the above findings.
References
Sniderman AD, Furberg CD (2008) Age as a modifiable risk factor for cardiovascular disease. Lancet 371:1547–1549
Satoh H, Tomita K, Fujii S, Kishi R, Tsutsui H (2009) Lower high-density lipoprotein cholesterol is a significant and independent risk for coronary artery disease in Japanese men. J Atheroscler Thromb 16:792–798
Graves DT (1999) The potential role of chemokines and inflammatory cytokines in periodontal disease progression. Clin Infect Dis 28:482–490
Friedewald VE, Kornman KS, Beck JD, Genco R, Goldfine A et al (2009) The American Journal of Cardiology and Journal of Periodontology Editors’ Consensus: periodontitis and atherosclerotic cardiovascular disease. Am J Cardiol 104:59–68
Andriankaja OM, Genco RJ, Dorn J, Dmochowski J, Hovey K et al (2007) Periodontal disease and risk of myocardial infarction: the role of gender and smoking. Eur J Epidemiol 22:699–705
Bahekar AA, Singh S, Saha S, Molnar J, Arora R (2007) The prevalence and incidence of coronary heart disease is significantly increased in periodontitis: a meta-analysis. Am Heart J 154:830–837
Katz J, Chaushu G, Sharabi Y (2001) On the association between hypercholesterolemia, cardiovascular disease and severe periodontal disease. J Clin Periodontol 28:865–868
Katz J, Flugelman MY, Goldberg A, Heft M (2002) Association between periodontal pockets and elevated cholesterol and low density lipoprotein cholesterol levels. J Periodontol 73:494–500
Jain A, Batista EL Jr, Serhan C, Stahl GL, Van Dyke TE (2003) Role for periodontitis in the progression of lipid deposition in an animal model. Infect Immun 71:6012–6018
Iacopino AM, Cutler CW (2000) Pathophysiological relationships between periodontitis and systemic disease: recent concepts involving serum lipids. J Periodontol 71:1375–1384
D’Aiuto F, Nibali L, Parkar M, Suvan J, Tonetti MS (2005) Short-term effects of intensive periodontal therapy on serum inflammatory markers and cholesterol. J Dent Res 84:269–273
Llambés F, Silvestre FJ, Hernández-Mijares A, Guiha R, Caffesse R (2008) The effect of periodontal treatment on metabolic control of type 1 diabetes mellitus. Clin Oral Investig 12:337–343
Almaghlouth AA, Cionca N, Cancela JA, Décaillet F, Courvoisier DS et al (2014) Effect of periodontal treatment on peak serum levels of inflammatory markers. Clin Oral Investig 18:2113–2121
Lösche W, Marshal GJ, Apatzidou DA, Krause S, Kocher T et al (2005) Lipoprotein-associated phospholipase A2 and plasma lipids in patients with destructive periodontal disease. J Clin Periodontol 32:640–644
Pejcic A, Kesic L, Brkic Z, Pesic Z, Mirkovic D (2011) Effect of periodontal treatment on lipoproteins levels in plasma in patients with periodontitis. South Med J 104:547–552
Duan JY, Ou-Yang XY, Zhou YX (2009) Effect of periodontal initial therapy on the serum level of lipid in the patients with both periodontitis and hyperlipidemia. Beijing Da Xue Xue Bao 41:36–39
Oz SG, Fentoglu O, Kilicarslan A, Guven GS, Tanrtover MD et al (2007) Beneficial effects of periodontal treatment on metabolic control of hypercholesterolemia. South Med J 100:686–691
Fentoğlu Ö, Köroğlu BK, Hiçyılmaz H, Sert T, Özdem M et al (2011) Pro-inflammatory cytokine levels in association between periodontal disease and hyperlipidaemia. J Clin Periodontol 38:8–16
Iwamoto Y, Nishimura F, Soga Y, Takeuchi K, Kurihara M et al (2003) Antimicrobial periodontal treatment decreases serum C-reactive protein, tumor necrosis factor-alpha, but not adiponectin levels in patients with chronic periodontitis. J Periodontol 74:1231–1236
D’Aiuto F, Parkar M, Andreou G, Suvan J, Brett PM et al (2004) Periodontitis and systemic inflammation: control of the local infection is associated with a reduction in serum inflammatory markers. J Dent Res 83:156–160
Marcaccini AM, Meschiari CA, Sorgi CA, Saraiva MC, de Souza AM et al (2009) Circulating interleukin-6 and high-sensitivity C-reactive protein decrease after periodontal therapy in otherwise healthy subjects. J Periodontol 80:594–602
Vidal F, Figueredo CM, Cordovil I, Fischer RG (2009) Periodontal therapy reduces plasma levels of interleukin-6, C-reactive protein, and fibrinogen in patients with severe periodontitis and refractory arterial hypertension. J Periodontol 80:786–791
Liu K, Meng H, Lu R, Xu L, Zhang L et al (2010) Initial periodontal therapy reduced systemic and local 25-hydroxy vitamin D(3) and interleukin-1 beta in patients with aggressive periodontitis. J Periodontol 81:260–266
Shimada Y, Komatsu Y, Ikezawa-Suzuki I, Tai H, Sugita N et al (2010) The effect of periodontal treatment on serum leptin, interleukin-6, and C-reactive protein. J Periodontol 81:1118–1123
Ide M, Jagdev D, Coward PY, Crook M, Barclay GR et al (2004) The short-term effects of treatment of chronic periodontitis on circulating levels of endotoxin, C-reactive protein, tumor necrosis factor-alpha, and interleukin-6. J Periodontol 75:420–428
Yamazaki K, Honda T, Oda T, Ueki-Maruyama K, Nakajima T et al (2005) Effect of periodontal treatment on the C-reactive protein and proinflammatory cytokine levels in Japanese periodontitis patients. J Periodontal Res 40:53–58
Behle JH, Sedaghatfar MH, Demmer RT, Wolf DL, Celenti R et al (2009) Heterogeneity of systemic inflammatory responses to periodontal therapy. J Clin Periodontol 36:287–294
Page RC (1991) The role of inflammatory mediators in the pathogenesis of periodontal disease. J Periodontal Res 26:230–242
Page RC, Kornman KS (1997) The pathogenesis of human periodontitis: an introduction. Periodontol 2000 14:9–11
Acknowledgments
The authors thank Yan-Hui Li for her help with statistical analyses. This study was self-funded by the authors and their institutions. Mr. Fu is the major person to complete this study.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Compliance with ethical standards
The protocol was approved by the Ethical Committee of the First People’s Hospital of Lianyungang City. After being informed on the purpose of the study, the patients signed informed consent forms. Research was conducted according to the principles outlined in the Declaration of Helsinki on experimentation involving human subjects.
Conflict of interest
The authors declare that they have no competing interests.
Rights and permissions
About this article
Cite this article
Fu, YW., Li, XX., Xu, HZ. et al. Effects of periodontal therapy on serum lipid profile and proinflammatory cytokines in patients with hyperlipidemia: a randomized controlled trial. Clin Oral Invest 20, 1263–1269 (2016). https://doi.org/10.1007/s00784-015-1621-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1621-2