Abstract
Background: Studies examining the association between periodontal disease and coronary heart disease have shown a consistent but weak to moderate relationship. Limited data have been reported in women and the role of smoking has not been fully clarified. Methods/Results: A population-based case–control study examining the association between periodontal disease (PD) and acute non-fatal myocardial infarction (MI) was conducted in Erie and Niagara counties in Western New York State. Cases (574) were discharged alive from local hospitals with MI diagnosis. Controls (887) were county residents randomly selected from the NY State Department of Motor Vehicles rolls and Health Care Financing Administration files. Periodontal disease was assessed using clinical attachment loss (CAL). Among men (415 cases), the odds ratio (OR) of the association between mean CAL (mm) and MI, adjusting for the effects of age, body mass index (BMI), physical activity, hypertension, cholesterol, diabetes, and total pack-years of cigarette smoking was 1.34 (1.15–1.57). In women (120 cases), the corresponding OR was 2.08 (1.47–2.94). The estimate of this association among non-smokers, also adjusting for age, gender, BMI, physical activity, hypertension, cholesterol, diabetes, and total pack-years of cigarette smoking, was 1.40 (1.06–1.86), while it was 1.49 (1.26–1.77) among smokers. Conclusions: This study provides evidence of an association between PD and incident MI in both genders. This association appears to be independent from the possible confounding effect of smoking.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal disease, a chronic infectious process, may contribute to atherogenesis and/or thromboembolic events in coronary heart disease (CHD). Experimental evidence and biological plausibility appear to support this hypothesis [1–3]. The majority of clinical and epidemiological findings and a recent meta-analysis confirm the presence of a weak to moderate association [4–12]. However, the studies to date have been limited to men and controversies are present regarding the causal nature of this observed association. For example, cigarette smoking is strongly associated with both periodontal disease and CHD. It is not clear whether smoking modifies the effect of periodontal disease on CHD development or if it plays a role of confounder. The aim of the present study was to determine whether the association between periodontal disease and CHD is present in both genders and to assess the role of cigarette smoking in this association.
Methods
Study sample
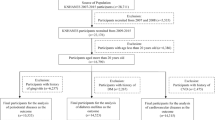
A population-based case–control study of periodontal disease and myocardial infarction was conducted in Erie and Niagara counties in Western New York State between September 1997 and December 2001.
Cases were men and women, aged 35 to 69 years, admitted to all hospitals in Erie and Niagara counties with a diagnosis of incident myocardial infarction and discharged alive. Additional inclusion criteria were no known prior history of any form of CHD, symptomatic angina, or diagnosis of cardiovascular disease (CVD) for which dietary or drug therapy had been prescribed, and free of cancer. We utilized the World Health Organization criteria for the definition of MI [13], hospital discharge diagnoses with International Classification of Diseases (ICD-9) codes of 410 were considered MIs [14]. Determination of incident MI was based on information found in the patients’ medical records and confirmed by personal physicians. Vital status was determined either from hospital lists, medical records, or physician notifications.
Controls were identified from a random sample of residents of Erie and Niagara counties. Controls had to meet the same criteria as cases (i.e., no known prior history of CHD, angina, or CVD, and free of cancer) and without MI. Potential controls aged 35–64 years were identified from a list provided by the New York State Department of Motor Vehicles. This source was used because it is known that 95% of New York residents in this age group have a driver’s license. Controls aged 65 to 69 years were identified from the Health Care Financing Administration lists. This source was used because it includes virtually all individuals in the age range of interest [15].
Cases and controls with at least six natural teeth, eligible and willing to participate were invited to the Center for Preventive Medicine at the University at Buffalo for an interview and physical and dental examinations. Non-white participants were excluded due to their small numbers; blacks and others numbered 118 out 1,603 of the total population. In addition, there was a big difference in characteristics between the white and non-whites. Thus, the present study assessed the association between periodontal disease and myocardial infarction among only white participants. Of the 1,485 white participants (participation rate of approximately 59%), a total of 574 cases and 887 controls (n = 1,461) had complete data on periodontal disease and the outcome MI, and were included in the present study.
All procedures used in this study were peer-reviewed and approved by the National Institutes of Health, the Institutional Review Board of the University at Buffalo, and the Human Subjects Committees of the hospitals in Erie and Niagara counties.
Data collection
Demographic characteristics were assessed by questionnaire. Weight was measured with a beam balance scale and height with a wall-mounted ruler using standard protocol. Body mass index (BMI) was computed as weight in kilograms divided by height in meters squared. Family history of heart disease, presence of hypertension, diabetes, cholesterol level, use of hormone replacement therapy for women, and self-report on frequency of physical activities in hours per week throughout the participant’s entire life (“lifetime physical activities”) were determined.
It is worth noting that family history of heart disease in the present study referred to any diagnosis such as heart disease or cardiovascular disease, high blood pressure, stroke, heart attack, by-pass surgery, angioplasty, or other forms of vascular disease such as phlebitis, intermittent claudication, or aneurysm in first degree relatives.
Participants were categorized as non-smokers if they reported never smoking or had smoked <100 cigarettes in their entire life; former smokers if they reported to have ever smoked ≥100 cigarettes, but had quit smoking at the time of interview; or current smokers if they currently smoked.
Alcohol drinking status was ascertained during the interview and participants were categorized as lifetime or irregular abstainers, non-current drinkers (not drinking within 30 days prior to the time of interview), or current drinkers.
Periodontal measurements
Mean clinical attachment loss (CAL in mm) of the whole mouth was used to determine periodontal status. CAL was obtained indirectly from the measurement of probing depth (PD) and the distance between the cemento-enamel junction (CEJ) and the gingival margin (GM). PD was measured and recorded automatically using the Florida Probe System [16]. Measurements were made at six sites per tooth for all teeth except third molars, but only inter-proximal sites were used to compute the mean CAL. The GM-CEJ distance was measured manually at six sites per tooth for all teeth except third molars and teeth whose CEJ was difficult to locate due to the presence of crowns or overhanging restorations. Severe periodontal disease was defined as a full mouth mean CAL of ≥3 mm. Plaque and calculus indices were assessed as well [17] and recorded as a measure of oral hygiene status.
Examiners were trained and calibrated before the study was conducted according to the protocol developed by Grossi et al. [18] and tested by Araujo et al. [19]. Intra-examiner variability, measured by standard deviation within examiner, ranged from 0.36 to 0.62 mm (overall 0.46 mm) when measuring probing depth in subjects with moderate or severe periodontal disease [18]. Later in the study, Araujo et al. found intra-examiner variability ranged from 0.38 to 0.42 mm (mean 0.40 ± 0.02 mm), and the inter-examiner variability ranged from 0.12 to 0.18 mm (mean 0.16 ± 0.02 mm) [19].
Statistical analyses
The association between periodontal status and MI, as well as potential interactions between variables, were examined using multiple logistic regression analyses. Level of significance of α = 0.05 was used as indication of statistical significance. Models were built hierarchically. The variable of interest, CAL, was always kept in the model. All covariates available in this study were entered into the model one at a time. Covariates included age, gender, educational level, BMI, lifetime physical activity, smoking status, pack-years of cigarette smoking, drinking status, family history of heart disease, hypertension or high blood pressure, high blood cholesterol, diabetes, use of hormone replacement therapy (women), menopausal status (women), and plaque and calculus indices. Variables that contributed to the change in the estimate of the association between periodontal disease and MI were retained. In addition, standard risk factors for cardiovascular disease were retained in the model regardless of their contribution to change in the estimate. Odds ratios along with 95% confidence intervals (95% CI) were obtained. All analyses were completed with the use of SPSS [20] and/or SAS [21] statistical packages.
Results
Characteristics of cases and controls by gender are presented in Table 1.
In men, cases were younger and less educated more likely to be current or former smokers and less likely to have never smoked than controls. In addition, lifetime total pack-years of cigarettes smoking was higher among cases than controls. As expected, cases were more likely than controls to have hypertension, high blood cholesterol, and diabetes.
Related to periodontal status, cases (35.6%) were more likely than controls (21.0%) to have more clinical attachment loss (CAL) as evidenced by more mean CAL ≥3 mm, and poorer oral hygiene than controls as measured by higher plaque and calculus indices.
In women, cases were more likely than controls to be post-menopause, overweight and less educated. More cases than controls were current or former smokers and fewer were never smokers. Also, cases tended to smoke more than controls in terms of lifetime total pack-years of cigarette smoking. Cases were less likely to be current alcohol drinkers or non-current drinkers than controls. As with men, women cases were more likely than controls to have hypertension, high blood cholesterol and diabetes.
Regarding the oral health conditions, women cases had worse periodontal status as evidenced by a higher percentage of CAL ≥ 3 mm and poorer oral hygiene (higher plaque and calculus indices than women controls.
The association between CAL and incident MI stratified by gender are presented in Table 2. Unadjusting for any other factors (except gender), the estimates of the association were 1.52 (95% CI 1.32–1.76) and 2.83 (95% CI 2.11–3.80) in men and women, respectively. Adjusting for the effects of age, BMI, physical activity, hypertension, cholesterol, diabetes, and total pack-years of cigarette smoking, the odds ratios of the association were 1.34 (95% CI 1.15–1.57), (P < 0.001) in men and 2.08 (95% CI 1.47–2.94), (P < 0.001) in women.
When participants were stratified by smoking status (Table 2), unadjusting for the effects of any other factors (except smoking status), non-smokers had an odds ratio of 1.54 (95% CI 1.20–1.98), (P = 0.001), while smokers had an odds ratio of 1.91 (95% CI 1.63–2.23). When adjusting for the effects of age, gender, BMI, physical activity, hypertension, cholesterol, diabetes, and total pack-years of cigarette smoking, the estimates of the association became 1.40 (95% CI 1.06–1.86), (P = 0.02) in non-smokers and 1.49 (95% CI 1.26–1.77), (P < 0.001) among smokers.
Discussion
The present population based case–control study provides evidence of an association between periodontal disease and incident non-fatal MI in women. In addition, there appears to be a dose–response relationship with greater risk with higher levels of CAL and the association appears to be independent of smoking.
Previous studies assessed and reported on the relationship between periodontal disease and CHD in women [4, 22]. The study by Mattila et al. found no association between dental infections and coronary atheromatosis [4]. However, this study was limited by the lack of adequate statistical power (as it included analysis of only 12 women) and by the use of a crude and non-specific measure of oral health. The prospective study by Jansson et al. assessed the relationship between a marginal bone loss index and mortality due to CVD. The association among women aged less than 45 years was reported to be not significant, but the data were not shown [23]. In contrast, we had good numbers of women cases (131) and controls (502) and a thorough evaluation of periodontal status making us confident in our findings.
The role of smoking on the association between periodontal disease and CHD has been actively debated with some authors suggesting that smoking is a causal confounding factor. Some previous studies that examined the association between periodontal disease and risk of CHD in non-smokers did not see a significant association [22–24]. For example, the study by Hyman reported negative findings in non-smokers. However, this study was limited by its cross-sectional nature, its reliance on of self-reported (non validated) history of heart attack, and a somewhat limited measurement of periodontal disease (measured only from two randomly selected quadrants of the mouth, one upper and one lower). The underestimation of both the outcome and the exposure may have lead to underestimation of the association.
In the present study, it is worthy to stress that a very comprehensive measure of smoking that includes not only categorization of smokers and non-smokers but also a measure of lifetime exposure (intensity) was used. Findings from our data set suggest the association between periodontal disease and incident MI to be independent from smoking as indicated by the adjusted data in men and by the findings in smokers and non-smokers in women. The observed association between CAL and MI in non-smokers provides greater evidence that periodontal disease, independently of the effect of smoking, could affect CHD.
The periodontal measurement CAL was chosen in the present study because it reflects a well established of periodontal disease in both clinical research and clinical practice. We decided to use the continuous variable in order to provide the maximal statistical power for the analyses. In addition, we used a definition of ≥3 mm for severe disease as it has been used in prior studies [24].
An advantage of this study is the population-based study sample assuring a greater level of comparability with the general population. It included a population at high risk of developing the outcome (i.e. men and women aged 35 to 69 years) so that a large number of MI cases were covered in this case–control design. In addition, detailed information on clinical measurements of periodontal disease, smoking, and a wide variety of potential confounders was collected and was able to be evaluated.
Our control group, recruited from two different sources, consisted of a sub-sample of the overall controls from “The Western New York Health Study (WNYHS)”. To determine whether the control sample from the WNYHS was of a selected nature, we compared selected characteristics of our participants with those of participants aged 35–79 years from the National Health and Nutrition Examination Survey (NHANES III) conducted in the United States between 1988 and 1994. There were no major differences in the characteristics considered between participants in the WNYHS and those of the NHANES III [15].
The relatively large number of women in the study allowed us to examine the association between periodontal disease and MI in both genders. In addition, this study is one of the few that could examine the association between periodontal disease and CHD independently of the effect of a shared risk factor, smoking.
There is not a clear explanation of the reason(s) that women when exposed to periodontal disease appear to be at much higher risk of MI than men. However, it should be pointed out that a higher susceptibility of women compared to men is evident with other risk factors as with diabetes, HDL-cholesterol, triglycerides, or the cluster of these risk factors such as in metabolic syndrome [25, 26]. In addition, recent findings suggested that the association between metabolic syndrome and periodontal disease is higher among women than men [27]. The proposed hypothesis is that inflammation increases cardiovascular risk particularly in women [26]. A prospective study among women found that incidence of hypertension was associated with increased serum C-reactive protein [28]. Furthermore, according to the findings from the Framingham heart study, carotid-intima media thickness is associated with serum C-reactive protein only in women; not in men [29].
Our study has some limitations that need to be considered when interpreting the results. The response rates, although only 45.4–60% for different recruitment waves, are similar to other studies conducted in the US that required a visit to a clinical center and a long complex examination and interview.
In order to check for significant bias, comparisons were made of a number of selected characteristics from a brief set of questions regarding socio-demographic and life style characteristics of participants and non-participants. This information was obtained from the phone interview of all individuals prior to their agreement or refusal to participate in the study. These characteristics for participants and non-participants are summarized by case status in Table 3. Overall the characteristics of participants and non-participants are not very different. There was not a particular pattern (healthier or sicker) observed among the characteristics that appeared to be significantly different. Participant controls were older than non-participant counterparts. Among cases, there were more male participants than non-participants. In addition, participants appeared to be more educated and had more alcohol consumption in a month than non-participant counterparts.
Concerning smoking status, participants (either MI cases or controls) were overall less likely to be smokers than non-participants. Since smoking is a strong risk factor for periodontal disease, we might assume that both MI case and control participants had better periodontal status than the MI case and control non-participants. In such case, our findings might represent an underestimation of the true association, and these findings may be generalizable only to populations with similar characteristics.
Another limitation is that those who died from their MI (either out of hospital or during hospitalization) were not included in the study. Thus, the true association between periodontal disease and risk of MI may be underestimated. The study by Beck and colleagues (1996) revealed stronger association between periodontal disease and fatal CHD compared to non-fatal CHD [10]. Therefore, the risk presented here may very well be an underestimation of the role of periodontal disease in MI etiology.
In summary, our study indicates that the observed association found between periodontal disease and CHD is consistent across genders, and is independent of the potential confounding effect of smoking. Further study needs to be done to ascertain whether the consistently observed link between periodontal disease and CHD is causal in nature. If a cause–effect relationship is confirmed, the high prevalence of periodontal disease will make prevention and treatment of this disease an important tool for the prevention of CHD, one of the major causes of death and disability.
References
Herzberg MC, MacFarlane GD, Gong K, Armstrong NN, Witt AR, Eroclspm PR, Meyer MW. The platelet interactivity phenotype of Streptococcus sanguis influences the course of experimental endocarditis. Infect Immun 1992;60:4809–18.
Herzberg MC, MacFarlane GD, Liu P, Erickson PR. The platelet as an inflammatory cell in periodontal diseases: interactions with Porphyromonas gingivalis. In: Genco RJ, Hamada S, Lehner T, McGhee JR, Mergenhagen SE, editors. Molecular pathogenesis of periodontal disease. Washington, DC: American Society for Microbiology; 1994. p. 247.
Haraszthy VI, Zambon JJ, Trevisan M, Zeid M, Genco RJ. Identification of periodontal pathogens in atheromatous plaques. J Periodontol 2000;71:1554–60.
Mattila KJ, Valle MS, Nieminen MS, Valtonen VV, Hietaniemi KL. Dental infections and coronary atherosclerosis. Atherosclerosis 1993;103:205–11.
Mattila KJ, Nieminen MS, Valtonen VV, Rasi VP, Kesaniemi YA, Syrjala SL, Jungell PS, Isoluoma M, Hietaniemi K, Jokinen MJ. Association between dental health and acute myocardial infarction. Br Med J 1989;298:779–82.
Mattila KJ, Valtonen VV, Nieminen MS, Huttunen JK. Dental infection and the risk of new coronary events: prospective study of patients with documented coronary heart disease. Clin Infect Dis 1995;20:588–92.
Emingil G, Buduneli E, Aliyev A, Atilla G. Association between periodontal disease and acute myocardial infarction. J Periodontol 2000;71:1882–6.
Joshipura KJ, Rimm EB, Douglass CW, Trichopoulos D, Ascherio A, Willett WC. Poor oral health and coronary heart disease. J Dent Res 1996;75:1631–6.
Morrison HI, Ellison LF, Taylor GW. Periodontal disease and risk of fatal coronary heart and cerebrovascular diseases. J Cardiovasc Risk 1999;6:7–11.
Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Periodontal disease and cardiovascular disease. J Periodontol 1996;67 Suppl 10:1123–37.
Mattila KJ, Asikainen S, Wolf J, Jousimies-Somer H, Valtonen V, Nieminen M. Age, dental infections, and coronary heart disease. J Dent Res 2000;79:756–60.
Danesh J. Coronary heart disease, Helicobacter pylori, dental disease, Chlamydia pneumoniae, and cytomegalovirus: meta-analyses of prospective studies. Am Heart J 1999;138(5 Pt 2):S434–7.
Beaglehole R, Stewart AW, Butler M. Comparability of old and new World Health Organization criteria for definite myocardial infarction. Int J Epidemiol 1987;16:373–6.
International Classification of Diseases. 9th revisions. Clinical modification. 4th ed. 1995;198–9.
Trevisan M, Dorn J, Falkner K, Russell M, Ram M, Muti P, Freudenheim JL, Nochajaski T, Kathy H. Drinking pattern and risk of non-fatal myocardial infarction: a population-based case-control study. Addiction 2004;99(3):313–22.
Gibbs CH, Hirschfeld JW, Lee JG, Low SB, Magnusson I, Thousand RR, Yerneni P, Clark WB. Description and clinical evaluation of a new computerized periodontal probe – the Florida probe. J Clin Periodontol 1988;5:137–44.
Machtei EE, Norderyd J, Koch G, Dunford R, Grossi S, Genco RJ. The rate of periodontal attachment loss in subjects with established periodontitis. J Periodontol 1993;64:713–8.
Grossi SG, Dunford RG, Ho A, Koch G, Machtei EE, Genco RJ. Sources of error for periodontal probing measurements. J Periodontal Res 1996;31:330–6.
Araujo MWB, Hovey K, Benedek J, Grossi SG, Dorn J, Wactawski-Wende J, Genco RJ, Trevisan M. Reproducibility of probing depth measurements using a constant force electronic probe: analysis of inter- and intra-examiner variability. J Periodontol 2003;74:18–22.
SPSS. SPSS version 11.5 reference guide. Chicago, IL. 2004.
SAS Institute Inc.: SAS/STAT User’s Guide, Version 9. Cary, NC: SAS Institute Inc. 2002.
Jansson LLS, Frithiof L, Theobald H. Relationship between oral health and mortality in cardiovascular diseases. J Clin Periodontol 2001;28:762–8.
Hujoel PP, Drangsholt M, Spiekerman C, DeRouen TA. Periodontal disease and coronary heart disease risk. JAMA 2000;284:1406–10.
Hyman JJ, Winn DM, Reid BC. The role of cigarette smoking in the association between periodontal disease and coronary heart disease. J Periodontol 2002;73:988–94.
Roeters van Lennep JE, Westeveld HT, Erkelens DW, van Der Wall EE. Risk factors for coronary heart disease: implications of gender. Cardiovasular Res 2002;53(3):538–49.
Regitz-Zagrosek V, Lehmkuhl E, Weickert MO. Gender differences in the metabolic syndrome and their role for cardiovascular disease. Clin Res Cardiol 2006;95(3):136–47.
Andriankaja OM, Dunford R, DeNardin E. The association between metabolic syndrome and periodontal disease. J Dent Res 2006 [abstract 2152].
Sesso HD, Buring JE, Rifai N, Blake GJ, Gaziano JM, Ridker PM. C-reactive protein and the risk of developing hypertension. JAMA 2003;290:2945–51.
Wang TJ, Nam B, Wilson PWF, Wolf PA, Levy D, Polak JF, D’Agostino RB, O’Donnell CJ. Association of C-reactive protein with carotid atherosclerosis in men and women: the Framingham heart study. Arterioscler Thromb Vasc Biol 2002;22:1662–7.
Acknowledgments
This project was supported by grants from the National Institute of Health, NIH and the National Institute of Dental and Craniofacial Research, NIDCR: AA 09399 and DE013585: Dr. Maurizio Trevisan; DE12085: Dr. Robert Genco. The authors thank the staff and all participants in this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Andriankaja, O.M., Genco, R.J., Dorn, J. et al. Periodontal disease and risk of myocardial infarction: the role of gender and smoking. Eur J Epidemiol 22, 699–705 (2007). https://doi.org/10.1007/s10654-007-9166-6
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10654-007-9166-6