Abstract
Objectives
The present study evaluated the degradation of collagen matrix (CM) immersed in tetracycline (TTC) or phosphate-buffered saline (PBS) in diabetic and normoglycemic rats.
Materials and methods
Diabetes was induced in 15 rats by systemic streptozotocin (STZ) (experimental); 15 healthy rats served as controls. One day before implantation 60 CM disks, 5 mm in diameter, were labeled with biotin: 30 were immersed in tetracycline (TTC) and 30 in PBS. One disk of each type was implanted subdermally in each rat. Animals were euthanized after 3 weeks, and tissue specimens containing the disks were prepared for histologic analysis. Horseradish peroxidase (HRP)-conjugated streptavidin was used to detect the remaining biotinylated collagen. Residual collagen area within the CM disks was analyzed and compared to baseline.
Results
Diabetes significantly increased the CM degradation. Immersion of the CM disks in a 50-mg/mL TTC solution before implantation decreased its degradation both in diabetic and normoglycemic rats.
Conclusions
Diabetes significantly increases collagen matrix degradation; immersion of collagen matrix in TTC before implantation decreases its degradation in both diabetic and normoglycemic conditions.
Clinical relevance
Immersion of medical collagen devices in TTC may be an effective means to decrease their resorption rate and increase their effectiveness, especially in situations with increased degradation such as diabetes.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Implantation of medical collagen products is a routine procedure in oral surgery [1]. Most commonly, it is used in the form of collagen barrier membranes in guided tissue regeneration (GTR) and guided bone regeneration (GBR) procedures. Collagen is a natural choice for many xenogeneic tissue matrices due to its high biocompatibility, low antigenicity, as well as the possibility of safely controlling its biodegradability by cross-linking reagents [2–8].
Collagen membranes have also been used with varying degrees of success as an alternative to autologous tissue grafts, aiming to improve the gingival biotype by increasing the thickness and width of the keratinized mucosa around teeth and implants [9, 10]. Recently, a novel collagen matrix (CM) (Mucograft®, Geistlich Pharma AG Wolhusen, Switzerland) has been designed for similar purposes, with application in soft tissue augmentation procedures. The CM consists of pure porcine type I and III collagen extracted and purified without additional cross-linking [11, 12]. It is subsequently engineered into a bi-layered matrix of approximately 3.5–4.0 mm thickness. The outer smooth layer is thin and made up of tightly packed collagen fibers to promote tissue adherence and facilitate wound healing. The inner roughened surface is a thick porous structure, which is placed against the host tissue, providing a space, initially for blood clot formation and then for tissue in-growth [11–15].
Although CM was primarily designed for oral soft tissue defect grafting, providing an adequate alternative to autologous soft tissue, it has also been shown to eliminate adverse effects such as disruption of the adjacent soft tissue architecture, loss of vestibular depth, and needs for a second surgical site, thus reducing morbidity [11–16]. An extended survival time of the CM seems to be important to improve soft tissue in-growth into the implanted collagen scaffold.
In vivo collagen implant degradation and remodeling depend on several tissue characteristics [17]. During healing, cells within the surgical site release matrix metalloproteinases (MMPs) which contribute to implant degradation [18, 19]. The catabolic effect of MMPs on implanted collagen may also be delayed by collagen stabilization such as increasing inter-molecular cross-linking [2–5, 20–22]. Immersion of collagen membranes in tetracycline (TTC) has been suggested as an additional means to delay the degradation of non-cross-linked collagen membranes both in vitro and in vivo, probably due to its anti-collagenolytic activity [23–26].
Diabetes is a prevalent and debilitating disease affecting a multitude of organs. The common denominator for most of the diabetic complications is an exaggerated and prolonged inflammatory response, including excessive production of pro-inflammatory cytokines, such as tumor necrosis factor α and interleukin-1 [27, 28]. The diabetic condition is also accompanied by increased numbers of immune cells, such as neutrophils and macrophages [27] as well as excessive amounts and activity of MMPs [29]. Together with a reduction in tissue inhibitors of metalloproteinases (TIMP) activity [30], these changes result in exaggerated collagenolytic activity in diabetic tissues that may potentially jeopardize the integrity and longevity of implanted collagen devices. Indeed, we have recently shown that uncontrolled diabetes increases the degradation rate of collagen membranes implanted in rats and that immersion in TTC delayed their degradation both in normoglycemic and diabetic animals [31]. The present study was undertaken to evaluate the effects of diabetes and immersion in TTC on the degradation of collagen matrix in vivo.
Materials and methods
This animal research comprised of 30 12-week-old male Wistar rats. Methods were in strict compliance with the protocol approved by the Institutional Animal Care and Use Committee of the Tel Aviv University. Diabetes was induced in 15 animals (experimental group) with a single intraperitoneal administration of streptozotocin (STZ, Sigma Chemical, St. Louis, MO), (65 mg/kg body weight) diluted in citrate buffer (0.01 M, pH 4.3). Blood glucose levels were evaluated once a week using a glucometer (Accu-Chek, Roche Diagnostics, Basel, Switzerland) according to the manufacturer’s instructions. The remaining 15 rats were given similar volumes of citrate buffer and served as normoglycemic controls.
CM sheets were used to aseptically prepare 5-mm-diameter disks using a disposable biopsy punch (Miltex Instrument Company, Lake Success, NY). The disks were labeled with biotin as previously described [23, 31]. Briefly, 1 day before implantation, the disks were incubated with aminohexanoyl-biotin-N-hydroxy-succinimide ester (Zymed Laboratories, San Francisco, CA) at 3 mg/mL for 1 h at room temperature and then washed overnight with three changes of sterile phosphate-buffered saline (PBS) (Ca2+/Mg2+ free, pH 7.4). Half of the biotin-labeled CM disks were immersed in TTC (Tevacycline, Teva Pharmaceutical Industries, Petah Tikva, Israel) (50 mg/mL) for 1 h, followed by washing in PBS. The other half was immersed solely in PBS. The TTC concentration of 50 mg/mL was chosen based on previous in vitro and in vivo experiments that found it to be the most effective [23, 24].
A rectangular area measuring approximately 15 × 30 mm along the animal’s back was shaved and aseptically prepared for surgery. Two dermal pouches were surgically created over the paravertebral area, 5 and 15 mm caudally to an imaginary line between the ears. Semi-lunar incisions were made perpendicular to the midsagittal line, and a full-thickness dermal flap was elevated by separating the skin from the underlying fascia within the epifascial plane. Pouches were made slightly larger than the disks to enable passive CM flat placement. One disk was placed in each pouch, with the smooth surface facing the skin. Each disk was stabilized by a 6–0 nylon suture (Assut, Pully-Lausanne, Switzerland) to the underlying tissues. The dermal flaps were repositioned and sutured with resorbable 4–0 Vicryl sutures (Vicryl Rapide, Ethicon, Madrid, Spain).
Animals were sacrificed 21 days after surgery with an overdose of ketamine chlorohydrate (Rhone Merieux, Lyon, France, 90 mg/kg body weight) and xylazine (Vitamed, Bat-Yam, Israel, 10 mg/kg body weight), followed by asphyxiation with carbon dioxide. A single evaluation time was chosen at 3 weeks since due to animals’ uncontrolled diabetic condition, a longer observation was not possible. Prior to euthanasia, blood was collected from the tail vein for final glucose measurements. The surgical scars were identified, and the skin over the sites was dissected out by separating the dermal tissue together with the underlying fascia and the disks and removed en bloc.
The tissue blocks were trimmed, separated in two parts (experiment/control), and fixed in 10 % neutral buffered formalin. After fixation, the sutures were carefully removed and the specimens were washed and dehydrated in ethanol and xylene and embedded in paraffin. Sagittal 5-μm-thick sections were made, and those including the central area of each disk were selected for analysis. Horseradish peroxidase (HRP)-conjugated streptavidin (Zymed Laboratories) was used according to the manufacturer’s protocol to detect biotinylated collagen. The slides were incubated with a solution of one drop of enzyme and washed with PBS for 5 min at room temperature, followed by detection with a substrate kit containing 3,3′-diaminobenzidine (DAB, ScyTek, Logan, UT, USA) as substrate and mounted with an aqueous solution of glycerol vinyl alcohol (Zymed). Two similar disks (immersed in PBS or TTC) that had not been implanted were processed for histology and served as baseline.
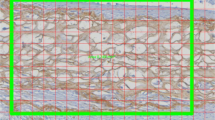
Blinded histometric evaluation was performed by one single investigator (AS). Stained sections were photographed with a digital camera mounted on a light microscope (Laborlux K, Leitz, Wetzlar, Germany) at a final magnification of ×40. Digital images were taken from the most central section of each sample by selecting the longest CM profiles and analyzed with an image analysis system (OSTEO, R & M Biometrics, Nashville, TN). A region of interest (ROI) was determined as a rectangle (0.7 mm × 0.45 mm), which was superimposed on five adjacent areas in each disk. The number of pixels that were positively stained within the ROI was recorded (Fig. 1).
The residual collagen area measured in each section was calculated as percentage of the respective baseline measurements according to the formula: collagen area at 21 days × 100/baseline collagen area. For statistical purposes, measurements from each CM disc were averaged and evaluated with two-way ANOVA with repeated measures. Several sections from each specimen were also stained with hematoxylin and eosin (H&E) or with picro-sirius red (PSR) to be viewed under polarized light for identification and histological observations of the surrounding tissues.
Results
One animal from the diabetes group died 3 days after diabetes induction. All the other animals injected with STZ became hyperglycemic (blood glucose >250 mg/dL) by day 4. Post-surgical healing was uneventful in the remaining 29 animals. During dissection, the dark nylon sutures were visible and the disks were identifiable. All 58 CM specimens were prepared for histology. Four specimens (2 from the diabetic TTC-treated group and 2 from the diabetic non-TTC-treated group) were damaged during the preparation process: these and their counterparts were dropped from further study, thus, only 25 pairs of CM discs were available for analysis.
Histological observation of sections stained with avidin, H&E, and PSR revealed CM in the form of relatively thick collagen bundles, twisting and entangling along the disk, regardless of the experimental conditions (asterisk in Fig. 2a–d). Thin fibrils were also present (arrows in Fig. 2b–d) among the thick fibers. Their presence was confirmed by the PSR-stained specimens observed under polarized light (Fig. 2d), in which the thick fibers appeared dark red (representing mature [implanted] collagen), while the thin fibrils appeared light green/yellow (representing young collagen). These findings are consistent with an in-growth of new connective tissue into the implanted CM. The collagen bundles of the CM were more condensed peripherally, with no visible difference between the smooth “denser” and rough “spongy” zones in most specimens (Fig. 2b). The borders of the CM disk showed little integration with the surrounding connective tissue. Small clusters of inflammatory cells were located within several CM disks (Fig. 3a, b).
Observation of sections stained with biotin-avidin, which showed only the implanted matrix in the various groups, revealed significant gaps within the residual collagen. The extent of gaps in CM that had been implanted in diabetic rats appeared greater than those in normoglycemic rats (Fig. 4). This was borne out by histometric measurements, which revealed that the mean collagen content in PBS-immersed disks declined from 57.5 ± 4.4 % in normoglycemic animals to 44.7 ± 6.4 % in hyperglycemic rats (P < 0.001). Pre-implantation incubation of CM in TTC increased the area of residual collagen in both groups: to 73.4 ± 7.3 % in normoglycemic rats and to 55.5 ± 6.3 % in diabetic rats (P < 0.001) (Table 1). Differences were between groups (normoglycemic and hyperglycemic) and between TTC- and PBS-immersed disks; within each group were statistically significant.
Discussion
Collagen matrix such as the one used in our study has previously been evaluated after implantation in animals and humans [11–16]. To our knowledge however, this is the first study analyzing the degradation of subcutaneously implanted untreated and TTC-treated CM in both normoglycemic and diabetic animals. The animal model of STZ-induced type 1 diabetes in Wistar rats and the biometric evaluation of the residual collagen in the implanted CM disks were chosen based on previous experiments, in which native collagen barriers were stained before implantation with biotin and evaluated following in vivo implantation [23, 24, 26, 31].
The main findings of this study were that CM degradation rate was significantly higher in uncontrolled, STZ-induced diabetes, compared to normoglycemic conditions, and that immersion of the CM in TTC at 50 mg/mL prior to implantation significantly reduced the CM degradation rate both in diabetic and normoglycemic animals. These results are comparable to similarly treated collagen regenerative membranes implanted over defects in the rat parietal bone [31]. Although both materials are engineered using a similar source of collagen, the difference in the degradation rate between the two could be expected. The regenerative membrane has a denser arrangement of collagen fibers that are designed to act as a tissue barrier and to reduce tissue and cell penetration. As such, it is expected to be more resistant to degradation and tissue integration. On the other hand, the collagen matrix contains a major component of “spongy” loose fibers, providing a resorbable scaffold which favors tissue in-growth and integration, resulting in a more rapid degradation. It is noteworthy however, that implantation sites in the different models were not similar, making direct comparisons not appropriate.
The present histological analysis showed that CM thickness was reduced from about 4.0 mm to less than 1.0 mm. Apparently, this reduction in thickness may have occurred after wetting the disks and during handling and covering it by the dermal flap, at the expense of the spaces within the collagen network.
Our previous [31] and present data showed that diabetes increases the rate of degradation of native collagen barriers and CM. Various reports have shown that in diabetes, the levels and activity of MMPs are higher and that those of TIMPs are lower [10, 12]. Although the present study did not quantitate the inflammatory infiltration peripheral to the CM, it appeared to be more marked in the diabetic animals compared with the normoglycemic ones. This observation is consistent with our previous findings [31]. Noteworthy, other studies have shown that macrophage infiltration into the kidney is increased in rats with STZ-induced diabetes [32] and that diabetes may lead to enhanced monocyte chemoattractant protein-1 levels that may be responsible for the recruitment of these inflammatory cells [33]. It would, therefore, follow that an increased inflammatory reaction in diabetic rats could lead to faster degradation of collagen matrix.
TTC and its chemically modified non-antimicrobial derivatives inhibit the catalytic activities of human collagenases and gelatinases, especially the neutrophil MMP [15–17]. We have previously shown that immersion of a bi-layered porcine collagen membrane in a 50-mg/mL TTC solution significantly delayed its degradation after implantation on the rat calvaria [26, 31]. The present study shows similar results when using CM both in diabetic and normoglycemic rats. This effect may be advantageous in procedures where CM is used, especially in submucosal implantation aimed to increase tissue volume, since prolonged scaffold function may enhance connective tissue in-growth. Thus, immersion of medical collagen devices in TTC may be an effective means to decrease their resorption rate and increase their effectiveness, especially in situations with increased degradation such as diabetes.
Conclusions
Diabetes significantly increases collagen matrix degradation; immersion of collagen matrix in tetracycline before implantation decreases its degradation in both diabetic and normoglycemic conditions.
References
Chiapasco M, Zaniboni M, Boisco M (2006) Augmentation procedures for the rehabilitation of deficient edentulous ridges with oral implants. Clin Oral Implants Res 17(Suppl 2):136–159
Pfeifer J, Van Swol RL, Ellinger R (1989) Epithelial exclusion and tissue regeneration using a collagen membrane barrier in chronic periodontal defects: a histologic study. Int J Periodontics Restorative Dent 9:262–273
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Cross-linked and non-cross-linked collagen barrier membranes disintegrate following surgical exposure to the oral environment: a histological study in the cat. Clin Oral Implants Res 19:760–766
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Long-term bio-degradation of cross-linked and noncross-linked collagen barriers in human guided bone regeneration. Clin Oral Implants Res 19:295–302
Singh MP, Stefko J, Lumpkin JA, Rosemblatt J (1995) The effect of electrostatic charge interactions on release rates of gentamicin from collagen matrices. Pharmacol Res 12:1205–1210
Freiss W (1998) Collagen—biomaterial for drug delivery. Eur J Pharm Biopharm 45:113–136
Goissis G, Marcantônio E Jr, Marcantônio RA, Lia RC, Cancian DC, de Carvalho WM (1999) Biocompatibility studies of anionic collagen membranes with different degree of glutaraldehyde cross-linking. Biomaterials 20:27–34
Tanaka S, Avigad G, Eikenberry EF, Brodsky B (1988) Isolation and partial characterization of collagen chains dimerized by sugar-derived cross-links. J Biol Chem 263:17650–17657
Hämmerle CH, Jung RE, Feloutzis A (2002) A systematic review of the survival of implants in bone sites augmented with barrier membranes (guided bone regeneration) in partially edentulous patients. J Clin Periodontol 29(Suppl 3):226–231
Wallace SS, Froum SJ (2003) Effect of maxillary sinus augmentation on the survival of endosseous dental implants. A systematic review. Ann Periodontol 8:328–343
McGuire MK, Scheyer ET (2010) Xenogeneic collagen matrix with coronally advanced flap compared to connective tissue with coronally advanced flap for the treatment of dehiscence-type recession defects. J Periodontol 81:1108–1117
Nevins M, Nevins ML, Kim SW, Schupbach P, Kim DM (2011) The use of mucograft collagen matrix to augment the zone of keratinized tissue around teeth: a pilot study. Int J Periodontics Restorative Dent 31:367–367
Sanz M, Lorenzo R, Aranda JJ, Martin C, Orsini M (2009) Clinical evaluation of a new collagen matrix (Mucograft prototype) to enhance the width of keratinized tissue in patients with fixed prosthetic restorations: a randomized prospective clinical trial. J Clin Periodontol 36:868–876
Lorenzo R, Garcia V, Orsini M, Martin C, Sanz M (2012) Clinical efficacy of a xenogeneic collagen matrix in augmenting keratinized mucosa around implants: a randomized controlled prospective clinical trial. Clin Oral Implants Res 23:316–324
Camelo M, Nevins M, Nevins ML, Schupbach P, Kim DM (2012) Treatment of gingival recession defects with xenogenic collagen matrix: a histologic report. Int J Periodontics Restorative Dent 32:167–173
Herford AS, Akin L, Cicciu M, Maiorana C, Boyne PJ (2010) Use of a porcine collagen matrix as an alternative to autogenous tissue for grafting oral soft tissue defects. J Oral Maxillofac Surg 68:1463–1470
Abraham LC, Dice JF, Lee K, Kaplan DL (2007) Phagocytosis and remodeling of collagen matrices. Exp Cell Res 313:1045–1055
Reynolds JJ, Hembry RM, Meikle MC (1994) Connective tissue degradation in health and periodontal disease and the roles of matrix metalloproteinases and their natural inhibitors. Adv Dent Res 8:312–319
Armstrong DG, Jude EB (2002) The role of matrix metalloproteinases in wound healing. J Am Podiatr Med Assoc 92:12–18
Minabe M, Kodama T, Kogou T et al (1989) Different cross-linked types of collagen implanted in rat palatal gingiva. J Periodontol 60:35–43
DeLustro F, Condell RA, Nguyen MA, McPherson JM (1986) A comparative study of the biologic and immunologic response to medical devices derived from dermal collagen. J Biomed Mater Res 20:109–120
Hämmerle CH, Jung RE (2003) Bone augmentation by means of barrier membranes. Periodontol 33:36–53, 2000
Moses O, Nemcovsky CE, Tal H, Zohar R (2001) Tetracycline modulates collagen membrane degradation in vitro. J Periodontol 72:1588–1593
Zohar R, Nemcovsky CE, Kebudi E, Artzi Z, Tal H, Moses O (2004) Tetracycline impregnation delays collagen membrane degradation in vivo. J Periodontol 75:1096–1101
Moses O, Vitiral D, Aboody G et al (2008) Bio-degradation of three different collagen membranes in the rat calvaria: a comparative study. J Periodontol 79:905–911
Moses O, Shemesh A, Aboody G, Tal H, Weinreb M, Nemcovsky CE (2009) Systemic TTC delays degradation of three different collagen membranes in rat calvaria. Clin Oral Implants Res 20:189–195
Pacios S, Kang J, Galicia J et al (2012) Diabetes aggravates periodontitis by limiting repair through enhanced inflammation. FASEB J 26:1423–1430
Graves DT, Kayal RA (2008) Diabetic complications and dysregulated innate immunity. Front Biosci 13:1227–1239
Xu F, Zhang C, Graves DT (2013) Abnormal cell responses and role of TNF-α in impaired diabetic wound healing. Biomed Res Int 2013, 754802. doi:10.1155/2013/754802
Thrailkill KM, Clay Bunn R, Fowlkes JL (2009) Matrix metalloproteinases: their potential role in the pathogenesis of diabetic nephropathy. Endocrine 35:1–10
Eliezer M, Nemcovsky CE, Romanos G et al (2013) Opposing effects of diabetes and tetracycline on the degradation of collagen membranes in rats. J Periodontol 84:529–534
Hartner A, Veelken R, Wittmann M, Cordasic N, Hilgers KF (2005) Effects of diabetes and hypertension on macrophage infiltration and matrix expansion in the rat kidney. BMC Nephrol 27(6):6
Fornoni A, Ijaz A, Tejada T, Lenz O (2008) Role of inflammation in diabetic nephropathy. Curr Diabetes Rev 4:10–17, Review
Acknowledgments
This study was supported by the Gerald A Niznick Chair of Implantology at Tel Aviv University, Israel. Mucograft® was donated by Geistlich Pharma AG Wolhusen, Switzerland.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This study was approved by Institutional Animal Care and Use Committee of the Tel Aviv University.
Conflict of interest
The authors declare that they have no competing interests.
Additional information
In partial fulfillment for the degree of D.M.D. of Asaf Shely from the Maurice and Gabriela Goldschleger School of Dental Medicine, Tel Aviv University, Tel Aviv, Israel.
Rights and permissions
About this article
Cite this article
Tal, H., Weinreb, M., Shely, A. et al. Tetracycline impregnation affects degradation of porcine collagen matrix in healthy and diabetic rats. Clin Oral Invest 20, 1237–1242 (2016). https://doi.org/10.1007/s00784-015-1615-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1615-0