Abstract
Objectives
Increased collagenolytic activity in diabetes may compromise collagen membrane (CM) survival. Tetracycline (TTC) possesses anti-collagenolytic properties and delays CM degradation. This study evaluated macrophage and capillary infiltration within CMs in diabetic rats.
Materials and methods
Diabetes was induced in 20 Wistar rats by streptozotocin and 20 served as controls. Biotin-labeled CM discs were immersed in either TTC (50 mg/ml) or PBS. In each animal, 2 discs (TTC and control) were implanted under the parietal periosteum and rats were sacrificed at 2 or 4 weeks post-implantation. The area and thickness of the residual disc collagen were measured following staining with streptavidin, and the number of macrophages and blood vessels within the membranes was determined using specific antibodies (to CD68 and transglutaminase II, respectively).
Results
Diabetes significantly reduced the area and thickness of the CMs, while TTC increased CM thickness significantly in both groups of rats at 2 and 4 weeks. Diabetes increased the number of macrophages (∼eightfold at 2 weeks and ∼fourfold at 4 weeks), but TTC had no significant effect. Finally, diabetes increased the number of blood vessels within the discs (∼threefold at 2 weeks and ∼twofold at 4 weeks), while TTC had no effect.
Conclusions
Diabetes increases degradation of native CMs and the number of blood vessels and macrophages within them. TTC immersion delays CM degradation without an apparent effect on macrophage and blood vessel penetration.
Clinical relevance
Enhanced CM degradation in diabetic conditions which impair guided regenerative procedure outcome is apparently related to increased blood vessel formation and macrophage infiltration.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Collagen membranes are routinely applied in guided tissue regeneration (GTR) and guided bone regeneration (GBR) procedures. Such barrier membranes prevent site repopulation by rapidly growing cells (i.e., epithelial, fibroblasts), thus enabling hard tissue progenitor cell proliferation and differentiation into osteoblasts, periodontal ligament fibroblasts, and cementoblasts [1]. Collagen membrane longevity plays a crucial role in the success of regenerative procedures [2–5], and their early degradation or premature exposure to the oral environment has a detrimental effect on bone regeneration [4, 6–8]. Collagen membrane degradation depends on collagenolytic activity of the host tissues [9]. During healing, cells within the surgical site release into the wound area matrix metalloproteinases (MMPs), which participate in the degradation of collagen membranes. [9, 10]. This process can be slowed down either by physiological downregulation of collagen-degrading enzymes, such as MMPs, by specific tissue inhibitors of matrix metalloproteinases (TIMPs) [11] or by increasing the chemical stability of the membranes by cross-linking during their production [12]. Tetracycline (TTC), an antibiotic agent possessing anti-collagenolytic properties, has been also shown to slow down the degradation of collagen membranes by inhibiting MMP activity [13–15].
We previously reported that immersion of collagen membranes in a TTC solution prior to their implantation reduces their degradation in vitro [16] and in vivo in healthy animals [17]. Since decreased levels of TIMPs and elevated activity of MMPs were found in skin tissues of rats with STZ-induced diabetes [18], enhanced degradation of collagen membranes is expected in diabetic animals, as has been shown in our recent study [19]. We also recently demonstrated that TTC delayed the degradation of collagen membranes in diabetic rats. [19] Hyperglycemia and resultant AGE (advanced glycation end-product) formation are considered to be major causal factors in the pathogenesis of diabetic complications [20]. Receptors for AGE (RAGE) have been identified on the cell surface of several cell types associated with a heightened inflammatory response and involved in the pathogenesis of these complications. These cell types include mononuclear phagocytes, endothelial cells, fibroblasts, smooth muscle cells, and lymphocytes [21, 22], suggesting that hyperglycemia-associated AGEs may directly stimulate an inflammatory reaction, including attraction and enhancement of macrophage activity via RAGE.
During wound healing, activated platelets release several cytokines as well as VEGF (vascular endothelial growth factor) upon injury. VEGF then attracts circulating neutrophils and monocytes to the site of injury as part of the normal inflammatory response [23]. In addition, VEGF induces the formation of new blood vessels in the wound area. Oxidative stress is an exaggerated, unbalanced production of reactive oxygen species (ROS) known to be one of the major mechanisms of many diabetic complications [24]. Many cellular and molecular alterations seen in diabetic models can be explained by elevated glucose-mediated oxidative stress and VEGF over-expression [25]. Thus, alterations in angiogenesis and inflammatory responses are frequently associated with diabetes. We have recently reported [19] that collagen membranes implanted in diabetic rats are subject to exaggerated degradation, compared with normoglycemic animals, and that this was associated with an increased vascular and inflammatory infiltrate.
The aim of the present study was to quantify the number of macrophages and blood vessels infiltrating into native collagen membranes during their degradation in both diabetic and normoglycemic rats and to test whether tetracycline, which mitigates membrane degradation, might affect this process.
Materials and methods
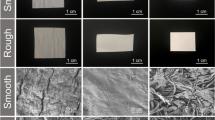
The study comprised of forty 12-week-old male Wistar rats. Diabetes was induced in half of the animals (n = 20) after overnight fasting, with a single intraperitoneal administration of streptozotocin (STZ, Sigma Chemical Co., St. Louis, MO, USA), a well-accepted diabetogenic agent, at 65 mg/kg of body weight. The rest of the animals were given a similar volume of the citrate buffer (0.01 M, pH 4.3) and served as normoglycemic controls. Blood glucose level was evaluated at regular intervals using a glucometer (Accu-Chek, Roche Diagnostics, F. Hoffmann-La Roche, Basel, Switzerland) according to the manufacturer’s instructions. Bilayered collagen membranes (BioGide®, Geistlich Pharma, Wolhusen, Switzerland) were cut with a disposable biopsy punch (Miltex Instrument Company, Lake Success, NY, USA) to 5-mm diameter discs. Average weight of the discs was 2.0 ± 0.1 mg. Membrane labeling with biotin has been previously described [20]. Briefly, all discs were labeled with 3 mg/ml AH-BNHS (aminohexanoyl-biotin-N-hydroxy-succinimide ester, Zymed Laboratories, Inc., San Francisco, CA, USA) for 1 h at room temperature and then washed overnight with three changes of PBS (Ca2+-Mg2+-free; pH 7.4) to remove unbound biotin. Half of the biotin-labeled membrane discs were immersed in tetracycline HCL (50 mg/ml) (TTC, Tevacycline, Teva Pharmaceuticals Ltd. Petah Tikva, Israel) for 1 h as previously described [20] followed by washing in PBS. The remaining discs were immersed only in PBS. All of the above membrane processing was performed in an aseptic environment; therefore, there was no need for membrane re-sterilization.
All animal surgeries were performed by the same experienced operator (CN). The surgical protocol for membrane implantation has been previously described [20]. Briefly, the dorsal part of the skin covering the scalp was shaved and aseptically prepared for surgery. A U-shaped incision was made in the scalp extending posteriorly over the parietal bone to enable elevation of a full thickness flap. A high-speed water-cooled diamond wheel-shaped bur was used to create two similar, 5-mm diameter shallow (approximately 1 mm deep) bony defects on the midline of the parietal bone without exposing the dura mater.
Two different collagen membrane discs (one immersed in TTC and the other in PBS) were placed in each animal (Fig. 1a). Soft tissues were repositioned to cover the implanted membranes and then the dermal tissues were sutured with resorbable sutures (Vycril Rapide, Ethicon, Madrid, Spain).
Twenty animals were sacrificed after 14 days and 20 after 28 days (10 diabetic and 10 control each time), with an overdose of ketamine chlorhydrate (Rhone Merieux, Lyon, France) (90 mg/kg body weight) and xylazine (Vitamed, Bat-Yam, Israel) (10 mg/kg body weight), followed by asphyxiation with carbon dioxide (CO2). Prior to euthanasia, blood was collected from the tail vein for final glucose measurements. Dermal tissues were dissected leaving the periosteum undisturbed, and the calvaria including surrounding tissues were retrieved, fixed in 4 % neutral buffered formalin, decalcified for 5 weeks in 10 % EDTA, washed, dehydrated in ethanol and xylene, and embedded in paraffin. Sagittal 5-μm sections were made, and those that included the central area of each of the two bony defects were selected for further analysis. Horseradish peroxidase-conjugated streptavidin (Zymed) was used according to the manufacturer’s protocol to detect biotinylated collagen. Slides were incubated with a solution of one enzyme drop in 1 ml of 10 mM PBS, pH 7.4 for 5 min at room temperature, followed by detection with a DAB substrate kit (ScyTek, Logan, UT, USA) and were mounted with an aqueous solution of glycerol vinyl alcohol (Zymed). Two neighboring sagittal sections were used for immunohistochemistry. Endogenous peroxidase activity was blocked with 3 % H2O2 for 10 min. Antigen retrieval was performed with 0.1 % proteinase K in PBS for 15 min at 37° (for CD68) or by heating under pressure of the sections in a citrate buffer, pH = 6, for a total of 12 min (for TGII). Nonspecific binding sites were blocked by incubation with Background Buster (Innovex, Richmond, CA, USA) for 40 min. Primary antibodies used were a mouse anti-rat CD68 monoclonal antibody (Millipore Corporation, Billerica, MA, USA) (at a 1:50 dilution) for macrophage identification and a mouse anti-transglutaminase II (TGII) monoclonal antibody (TG100, Thermo Fisher Scientific, Waltham, MA, USA) (at a 1:100 dilution) for the identification of endothelial cells [26]. Both antibodies were diluted in an antibody diluent (Zytomed, Berlin, Germany) and were incubated with the sections for 1 h at room temperature. Bound primary antibodies were identified with a goat anti-mouse HRP-conjugated antibody (Invitrogen Carlsbad, CA, USA), incubated for 30 min at room temperature, and followed by a hematoxylin counterstain. Negative controls were performed by omitting the primary antibody.
Histological evaluations were performed by the same experienced investigator (OM). Stained sections were photographed with a digital camera mounted on a light microscope (Laborlux K, Leitz, Wetzlar, Germany) using a ×10 objective. Multiple digital images were taken and stored for each sample and analyzed by an Image Analysis System (OSTEO, R&M Biomatrics, Nashville, TN, USA). In each block, the central part of the membrane was identified by measuring the underlying bone defect. A region of interest (ROI) was created as a rectangle, 1.2 mm × 0.5 mm, which was superimposed on five adjacent areas (fields) in each disc. The number of pixels that were positively stained within the ROI was registered (Fig. 1b). Two non-implanted biotin-labeled discs (one immersed in TTC and the other in PBS) were processed in the same manner and served as baseline. The residual collagen area measured in each section was calculated as percentage of the respective baseline measurements according to the following formula: collagen area at 2 or 4 weeks divided by baseline collagen area and multiplied by 100. In addition, residual membrane thickness was measured in each field. In each slide, mean of the measurements of area/thickness within each disc served as a unit for statistical analysis. Several slides from each specimen were also stained with hematoxylin and eosin to identify the surrounding tissues.
For macrophage and capillary counts, discs were divided into four consecutive 1000 × 850 μm fields that covered the entire thickness of the discs, and positive cells were counted per field. Since membrane thickness (and with it the probability of finding macrophages or blood vessels) varied greatly between 2 and 4 weeks and between healthy and diabetic rats, “per field” counts were divided by membrane thickness and multiplied by 100, i.e., a cell count per 0.1 mm2 (1000 × 100 microns) was derived.
Mean values were analyzed with two-way ANOVA with repeated measures, where treatment with TTC/PBS was the within-subject variable and health status (normo- vs hyper-glycemia) was the between-subject variable. P values equal to or smaller than 0.05 were considered to represent a statistically significant difference.
Results
All 20 STZ-injected rats demonstrated glucose level >250 mg/dl after 4 days and, accordingly, were considered diabetic. Animals injected with citrate buffer did not develop diabetes and, therefore, served as a normoglycemic control group. Healing following the surgical procedures for the collagen disc implantation was uneventful in all animals.
The area of residual collagen in PBS-immersed discs was lower in diabetic compared with normoglycemic rats (52.2 % ± 3.0 vs. 68.4 % ± 6.2 of baseline, respectively (P < 0.0001), at 2 weeks (Fig. 2a) and 11.8 ± 9.0 vs 25.6 % ± 4.7 of baseline, respectively (P < 0.01), at 4 weeks (Fig. 2b)). Immersion in TTC slightly but not significantly increased the area of residual collagen both in diabetic and normoglycemic animals.
a Residual collagen area (mean and sd) of discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 2 weeks. Three dollar signs represent the effect of diabetes, P < 0.0001. b Residual collagen area (mean and sd) of discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 4 weeks. Two dollar signs represent the effect of diabetes, P < 0.01
Diabetes also reduced significantly the residual membrane thickness of PBS-immersed discs (269.9 ± 63.2 vs 444.2 ± 15.9 μm (P < 0.0001) at 2 weeks (Fig. 3a) and 103.1 ± 53.6 vs 247.1 ± 56.6 μm (P < 0.001) at 4 weeks (Fig. 3b). TTC significantly increased residual collagen membrane (CM) thickness in both normoglycemic and hyperglycemic rats at 2 weeks (P = 0.05) and 4 weeks (P < 0.01). Membrane thickness of TTC-immersed discs was 4–11 % greater than that of PBS-immersed discs at 2 weeks and 22–47 % greater at 4 weeks. The magnitude of the TTC effect was invariably more pronounced in diabetic rats.
a Residual membrane thickness (mean and sd) of discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 2 weeks. Three dollar signs represent the effect of diabetes, P < 0.0001. An asterisk represents the effect of TTC, P = 0.05. b Residual membrane thickness (mean and sd) of discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 4 weeks. Two dollar signs represent the effect of diabetes, P < 0.001. Double asterisks represent the effect of TTC, P < 0.01
Diabetes markedly increased the number of mononuclear CD-68 positive cells (putative macrophages) which inhabited the PBS-immersed membrane discs (Fig. 4a): ∼eightfold (from 0.97 ± 0.5 per 0.1 mm2 to 8.3 ± 4.5 (P < 0.0001) at 2 weeks (Fig. 4b)) and ∼fourfold (from 4.8 ± 2.2 to 20.7 ± 22.3 (P = 0.05) at 4 weeks (Fig. 4c). Immersion in TTC reduced the number of CD-68 positive cells at 4 weeks, but this effect did not reach statistical significance due to a large variability.
a Photomicrographs of CD-68 positive cells (arrows) within the membrane placed in a normoglycemic (H) or a diabetic (S) rat showing that their number is clearly greater in the latter. NC = negative control. Final magnification = ×100. b Number (mean and sd) of mononuclear CD-68 positive cells within the membrane discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 2 weeks. Three dollar signs represent the effect of diabetes, P < 0.0001. c Number (mean and sd) of mononuclear CD-68 positive cells within the membrane discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 4 weeks. One dollar sign represents the effect of diabetes, P = 0.05
Diabetes also greatly increased the number of TGII-positive blood vessels within the PBS-immersed membrane discs (Fig. 5a): ∼threefold (from 2.2 ± 0.9 per 0.1 mm2 to 7.3 ± 3.4 (P < 0.0001) at 2 weeks (Fig. 5b)) and ∼twofold (from 5.3 ± 3.7 to 10.4 ± 13.6 at 4 weeks (Fig. 5c); this difference did not reach statistical significance). TTC had no effect on the number of blood vessels in either group of rats.
a Photomicrographs of TG-II positive lumen-associated blood vessels (arrows) within the membrane placed in a normoglycemic (H) or a diabetic (S) rat showing that their number is clearly greater in the latter. NC = negative control. Final magnification = ×100. b Number (mean and sd) of TG-II positive lumen-associated blood vessels within the membrane discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 2 weeks. Three dollar signs represent the effect of diabetes, P < 0.0001. c Number (mean and sd) of TG-II positive lumen-associated blood vessels within the membrane discs immersed in PBS (black bars) or TTC (white bars) in normoglycemic (H) and diabetic (S) rats at 4 weeks. No significant differences were found
In conclusion, STZ-induced diabetes in rats was associated with exaggerated collagen membrane degradation and increased infiltration of the membranes with macrophages and blood vessels. Immersion of the membranes in TTC mitigated membrane degradation without an apparent effect on macrophage and blood vessel infiltration.
Discussion
In agreement with our previous study [19], collagen membrane degradation was markedly enhanced in uncontrolled, STZ-induced, diabetes compared to a normoglycemic situation. Various reports have shown that, in diabetes, the levels of tissue MMPs are higher and those of TIMPs are lower [18, 27]. Since the inflammatory infiltration of the tissues surrounding the CMs was more marked in the animals with diabetes compared to those with normoglycemia [19], the resulting increased levels of MMPs, typical for diabetes mellitus [18], may have contributed to the enhanced degradation of CMs compared to normoglycemic conditions.
In agreement with the proposed association between an exacerbation of inflammation and CM degradation, diabetes increased fourfold to eightfold the number of mononuclear CD-68 positive cells (putative macrophages) which inhabited the membrane discs. Macrophage accumulation is common to many diabetic complications and is attributed to increased nonenzymatic glycation of proteins (formation of advanced glycation end products (AGEs)) and oxidative stress (OxS) [28].
AGEs may affect many cell types by binding the receptor for AGEs (RAGE) and inducing the local formation of molecules that attract and retain macrophages such as monocyte chemoattractant protein-1 (MCP-1) and macrophage migration inhibitory factor (MIF) [28]. These activated macrophages, in turn, secrete a variety of pro-inflammatory mediators such as IL-1 and TNFα and contribute to diabetic tissue injury by producing reactive oxygen species (ROS) and MMPs [28]. Given the known enhancement of inflammation by diabetes in many tissues, other cells not assayed here (e.g., PMNs) could also be more abundant within the membranes in the diabetic animals.
In this study, a twofold to threefold increase in the number of TGII-positive blood vessels within the membrane discs was found in diabetic animals. Aberrant angiogenesis in different tissues can play a role in the pathogenesis of many complications of diabetes (e.g., retinopathy, nephropathy). [29] Vascular endothelial growth factor (VEGF) is a major inducer of angiogenesis and lymphangiogenesis, because it is a highly specific mitogen for endothelial cells. Its signal transduction involves binding to tyrosine kinase receptors and results in endothelial cell proliferation, migration, and new vessel formation [30]. It has been implicated as one of the mediators for proliferative angiogenesis in diabetes-associated pathologies [31–33].
The elevation in growth factors, particularly VEGF, is responsible for the vascular dysfunction via numerous mechanisms [34]. The average number of VEGF-stained vessels in diabetic retinas is significantly higher than in the nondiabetic ones. Vascular endothelial growth factor expression is increased in diabetic subjects, and its immunoreactivity is correlated with increased vascular permeability to macromolecules [35]. In support of its involvement, anti-VEGF therapy is used to treat exaggerated angiogenesis in the diabetic retina. [36] Also of interest is the finding that the amount of VEGF is increased in the periodontium of diabetic patients with periodontitis [37].
Thus, the accelerated degradation of collagen membranes we found in type 1 diabetic rats is associated with increased infiltration of macrophages and blood vessels and, in general, with an increased inflammatory reaction.
Previous findings from our research group have shown that immersion of a bilayered porcine CM in a 50-mg/ml TTC solution significantly delays its degradation after implantation in the rat calvaria in both healthy and diabetic animals at 3 weeks [17, 19]. The present study, in which the same concentration of TTC was used, corroborates these data (especially at 4 weeks). TTC and its chemically modified non-antimicrobial derivatives inhibit the catalytic activities of human collagenases and gelatinases, especially the neutrophil MMP [38–40]. MMPs, also designated matrixins, hydrolyze components of the extracellular matrix. These proteinases play a central role in many biological processes, such as embryogenesis, normal tissue remodeling, wound healing, and angiogenesis, and in diseases such as atheroma, arthritis, cancer, and tissue ulceration [11]. In the context of collagen membrane longevity, excessive MMP activity, such as that found in diabetic tissues, will undoubtedly lead to more rapid membrane degradation. Thus, TTC immersion of collagen barriers is a simple and effective means to prolong their survival.
It is interesting to note that while TTC was effective in reducing CM degradation, it had no significant effect on the infiltration of macrophages and no effect at all on the infiltration of blood vessels. On one hand, TTC reduced the number of macrophage at 4 weeks; however, the difference did not achieve statistical significance due to a large variability. It is possible that a larger group of animals might have produced a more definitive result concerning macrophage number. On the other hand, this observation may imply that the increased number of inflammatory cells and blood vessels in diabetic tissues is not affected by the presence of TTC within the membranes but that the actual MMP-mediated degradation of the membranes can be slowed down by TTC.
Our results should be extrapolated to human clinical situations (e.g., GBR procedures) with caution. Firstly, our model differs from a clinical oral situation in that membranes were implanted in surgically created shallow defects in the calvaria, which is a closed, noncontaminated, extraoral environment. Implantation of similar membranes under the oral mucosa/gingiva may follow a different pattern of degradation with time and may result in a different presence of macrophages due to possible contamination. Second, soft tissue healing in rats is faster and less prone to hindrance, compared to that in humans, so that the time frame needed to assess these variables in human tissues should inevitably be longer.
Conclusion
Accelerated degradation of implanted collagen membranes in type 1 diabetic rats was accompanied with increased infiltration of macrophages and blood vessels. Pre-implantation immersion of the membranes in 50 mg/ml TTC slowed down their degradation without an apparent effect on the number of infiltrating macrophages or blood vessels.
References
Lundgren D, Laurell L, Gottlow J, Rylander H, Mathisen T, Nyman S, Rask M (1995) The influence of the design of two different bioresorbable barriers on the results of guided tissue regeneration therapy. An intra-individual comparative study in the monkey. J Periodontol 66:605–612
Patino MG, Neiders ME, Andreana S, Noble B, Cohen RE (2002) Collagen as an implantable material in medicine and dentistry. J Oral Implantol 28:220–225
Pfeifer J, Van Swol RL, Ellinger R (1989) Epithelial exclusion and tissue regeneration using a collagen membrane barrier in chronic periodontal defects: a histologic study. Int J Periodontics Restorative Dent 9:262–273
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Cross-linked and non-cross-linked collagen barrier membranes disintegrate following surgical exposure to the oral environment: a histological study in the cat. Clin Oral Implants Res 19:760–766
Chung KM, Salking LM, Stein MD, Freedman AL (1990) Clinical evaluation of biodegradable collagen membrane in GTR. J Periodontol 61:732–736
Zitzmann NU, Naef R, Schärer P (1997) Resorbable versus nonresorbable membranes in combination with Bio-Oss for guided bone regeneration. Int J Oral Maxillofac Implants 12:844–852
Machtei EE (2001) The effect of membrane exposure on the outcome of regenerative procedures in humans: a meta-analysis. J Periodontol 72:512–516
Tal H, Kozlovsky A, Artzi Z, Nemcovsky CE, Moses O (2008) Long-term bio-degradation of cross-linked and non-cross-linked collagen barriers in human guided bone regeneration. Clin Oral Implants Res 19:295–230
Reynolds JJ, Hembry RM, Meikle MC (1994) Connective tissue degradation in health and periodontal disease and the roles of matrix metalloproteinases and their natural inhibitors. Adv Dent Res 8:312–319
Armstrong DG, Jude EB (2002) The role of matrix metalloproteinases in wound healing. J Am Podiatr Med Assoc 92:12–18
Visse R, Nagase H (2003) Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ Res 92:827–839
Minabe M, Kodama T, Kogou T, Tamura T, Hori T, Watanabe Y, Miyata T (1989) Different crosslinked types of collagen implanted in rat palatal gingiva. J Periodontol 60:35–43
Golub LM, McNamara TF, D’Angelo G, Greenwald RA, Ramamurthy NS (1987) A non-antimicrobial chemically modified tetracycline inhibits mammalian collagenase activity. J Dent Res 66:1310–1314
Golub LM, Lee HM, Ryan ME, Giannobile WV, Payne J, Sorsa T (1998) Tetracyclines inhibit connective tissue breakdown by multiple non-antimicrobial mechanisms. Adv Dent Res 12:12–26
Greenwald RA, Golub LM, Ramamurthy NS, Chowdhury M, Moak SA, Sorsa T (1998) In vitro sensitivity of the three mammalian collagenases to tetracycline inhibition: relationship to bone and cartilage degradation. Bone 22:33–38
Moses O, Nemcovsky CE, Tal H, Zohar R (2001) Tetracycline modulates collagen membrane degradation in vitro. J Periodontol 72:1588–1593
Zohar R, Nemcovsky CE, Artzi Z, Kebudi E, Tal H, Moses O (2004) Tetracycline inhibits collagen membrane degradation in-vivo in a dose-dependent manner. J Periodontol 75:1096–1101
Yang C, Zhu P, Yan L, Chen L, Meng R, Lao G (2009) Dynamic changes in matrix metalloproteinase 9 and tissue inhibitor of metalloproteinase1 levels during wound healing in diabetic rats. J Am Podiatr Med Assoc 99:489–496
Eliezer M, Nemcovsky C, Romanos G, Kozlovsky A, Tal H, Kolerman R, Weinreb M, Moses O (2013) Opposing effects of diabetes and tetracycline on the degradation of collagen membranes in rats. J Periodontol 84:529–534
Pfeiffer A, Schatz H (1995) Diabetic microvascular complications and growth factors. Exp Clin Endocrinol Diabetes 103:7–14
Schmidt AM, Yan SD, Brett J, Mora R, Nowygrod R, Stern D (1993) Regulation of human mononuclear phagocyte migration by cell surface-binding proteins for advanced glycation end products. J Clin Invest 91:2155–2168
Radoff S, Vlassara H, Cerami A (1988) Characterization of a solubilized cell surface binding protein on macrophages specific for proteins modified nonenzymatically by advanced glycosylated end products. Arch Biochem Biophys 263:418–423
Hoeben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA (2004) Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 56:549–580
Yamagishi S, Ueda S, Matsui T, Nakamura K, Okuda S (2008) Role of advanced glycation end products (AGEs) and oxidative stress in diabetic retinopathy. Curr Pharm Des 14:962–968 Review
Caldwell RB, Bartoli M, Behzadian MA, El-Remessy AE, Al-Shabrawey M, Platt DH, Liou GI, Caldwell RW (2005) Vascular endothelial growth factor and diabetic retinopathy: role of oxidative stress. Curr Drug Targets 6:511–524
Schwarz F, Rothamel D, Herten M, Sager M, Becker J (2006) Angiogenesis pattern of native and cross-linked collagen membranes: an immunohistochemical study in the rat. Clin Oral Implants Res 17(4):403–409
Han SY, Jee YH, Han KH, et al. (2006) An imbalance between matrix metalloproteinase-2 and tissue inhibitor of matrix metalloproteinase-2 contributes to the development of early diabetic nephropathy. Nephrol Dial Transplant 21:2406–2416
Tesch GH (2007) Role of macrophages in complications of type 2 diabetes. Clin Exp Pharmacol Physiol 34:1016–1019
Tahergorabi Z, Khazaei M (2012) Imbalance of angiogenesis in diabetic complications: the mechanisms. Int J Prev Med 3:827–838
Hoben A, Landuyt B, Highley MS, Wildiers H, Van Oosterom AT, De Bruijn EA (2004) Vascular endothelial growth factor and angiogenesis. Pharmacol Rev 56:549–580
Hammes HP, Lin J, Bretzel RG, Brownlee M, Breier G (1998) Upregulation of the vascular endothelial growth factor/vascular endothelial growth factor receptor system in experimental background diabetic retinopathy of the rat. Diabetes 47:401–406
Gardlik R, Fusekova I (2014) Pharmacologic therapy for diabetic retinopathy. Semin Ophthalmol. doi:10.3109/08820538.2013.859280
Nakagawda T, Sato W, Kosugi T, Johnson RJ (2013) Uncoupling of VEGF with endothelial NO as a potential mechanism for abnormal angiogenesis in the diabetic nephropathy. J Diabetes Res 2013:184539
Tilton RG (2002) Diabetic vascular dysfunction: links to glucose-induced reductive stress. Micros Res Tech. 57:390–407
Mathews MK, Merges C, McLeod DS, Lutty GA (1997) Vascular endothelial growth factor and vascular permeability changes in human diabetic retinopathy. Invest Ophthalmol Vis Sci 38:2729–2741
Osaadon P, Fagan XJ, Lifshitz T, Levy J (2014) A review of anti-VEGF agents for proliferative diabetic retinopathy. Eye (Lond) 28:510–520
Unlü F, Güneri PG, Hekimgil M, Yeşilbek B, Boyacioğlu H (2003) Expression of vascular endothelial growth factor in human periodontal tissues: comparison of healthy and diabetic patients. J Periodontol 74:181–187
Carmeli E, Kodesh E, Nemcovsky CE (2009) Tetracycline therapy for muscle atrophy due to immobilization. J Musculoskelet Neuronal Interact 9:81–88
Golub LM, Ramamurthy NS, McNamara TF, Greenwald RA, Rifkin BR (1991) Tetracyclines inhibit connective tissue breakdown: new therapeutic implications for an old family of drugs. Crit Rev Oral Biol Med 2:297–321
Ramamurthy NS, Vernillo AT, Greenwald RA, Lee HM, Sorsa T, Golub LM, Rifkin BR (1993) Reactive oxygen species activate and tetracyclines inhibit rat osteoblast collagenase. J Bone Miner Res 8:1247–1253
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
This study was not funded by an external agency or institute but by internal (departmental) resources.
Conflict of interest
The authors declare that they have no competing interests.
Ethical approval
All applicable international, national, and/or institutional guidelines for the care and use of animals were followed. All procedures performed in this study were in accordance with the ethical standards of the Tel-Aviv University Faculty of Medicine and were approved by its Animal Care and Use Committee.
Rights and permissions
About this article
Cite this article
Moses, O., Eliezer, M., Nemcovsky, C. et al. Accelerated degradation of collagen membranes in diabetic rats is associated with increased infiltration of macrophages and blood vessels. Clin Oral Invest 20, 1589–1596 (2016). https://doi.org/10.1007/s00784-015-1635-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1635-9