Abstract
Objectives
The purpose of this study was to analyze the influence of the shape of various implants and the density of substrate on primary stability using a combination of methods.
Materials and methods
Fifty-four Neodent® brand cylindrical and conical implants with different prosthetic platforms were used. Implants were inserted into a pork rib bone and polyurethane blocks. Primary stability was assessed by insertion torque (IT), resonance frequency analysis (RFA), and pullout strength. Screws were also analyzed by scanning electron microscopy (SEM) before insertion and after removal to justify their use for inserting in different substrates.
Results
The conical cone morse implant had the highest average for all of the assays performed and was significantly different (p < 0.05) from the cylindrical implants for IT in the bone, pullout strength in the 40 per cubic foot (PCF) polyurethane, and the bone. The internal hex cylindrical implant had the lowest averages, which were significantly different (p < 0.05) from the conical implants for IT and RFA in the bone, pullout strength in the 40 PCF polyurethane, and the bone. The IT, RFA, and pullout strength assays were moderately correlated, and the photomicrographs did not reveal changes in the implants.
Conclusions
The analysis of different implants showed a better primary stability of tapered implants; the density of the substrate influences the primary stability and the 15 PCF polyurethane was not adequate to evaluate primary stability; correlation was obtained between the different methodologies of analysis of primary stability.
Clinical relevance
The study shows the influence of different implant macro-geometries and densities of substrates on primary stability.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The interaction between the bone tissue and the implant is responsible for the long-term success of oral treatments using supported prosthetic implants. For this biological process, called osseointegration, to occur, a group of factors should be taken into consideration. These factors can be related to the patient, such as overall and oral health and bone density and volume, as well as to the surgical technique and to the implant itself, including its shape, size, and surface treatment [1–3].
Primary stability, a prerequisite for osseointegration [4] resulting from the mechanical interaction between bone tissue and the implant during surgical insertion, may be affected by the macro-geometry of the screw, surface roughness [5], and surgical technique and primarily functions to inhibit micromovement of the implant, promotes proliferation and differentiation of the osteoblast cells, and inhibits fibrous tissue invasion and encapsulation [6].
The macro-geometry of the implant may directly support or interfere with primary stability, as diameter, length, shapes, and thread pitch [1] determine the primary bone/implant interaction and are fundamental for strengthening or weakening the osseointegration process. The morphological structure characteristics of the screw can function to strengthen the anchoring of the implant to the bone, minimize micromovement and shear forces, and maintain the bone edge [7].
Primary stability can be assessed before applying the load to predict osseointegration and to select the most adequate type of load for each clinical situation [8]. Currently, insertion torque (IT) and resonance frequency analysis (RFA) are the most commonly used methods employed in clinical practice for evaluating primary stability. For in vitro experiments, the pullout strength assay analyzes the resistance of the implants based on the physical and chemical properties of the screw [9].
The field is constantly proposing various macro- and microstructure implant models, but controversies still exist regarding the actual effect of shape on primary stability and the efficacy of the various methods for its assessment. Therefore, the aim of this study was to evaluate, in vitro, the influence of implant shape, on primary stability using several different substrate densities and correlating several methods.
Materials and methods
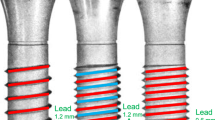
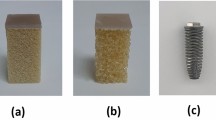
A total of 54 commercially pure titanium (cp Ti) implants (Neodent®, Curitiba, Paraná, Brazil) with six different macro-designs (n = 9) were analyzed. Cylindrical (Titamax®) and conical (Alvim®) implants were used. Of the cylindrical implants, nine had external hex (EH) prosthetic connections, nine had internal hex (IH) connections, and nine had cone morse (MC) connections. The same was true for the conical implants. All of the implants had particle-blasted surfaces.
One hundred sixty-two bone blocks of polyurethane (PU) (Nacional Ossos®, Jaú, SP, Brazil) measuring 15 × 15 × 30 mm were used to simulate the following bone densities: 0.24, 0.32, and 0.64 g/cm3 (15, 20, and 40 per cubic foot (PCF), respectively); according to the classification proposed by Lekholm and Zarb (1985), PU 15 PCF simulates the bone type III, PU 20 PCF the bone types II and III, and the PU 40 PCF the bone type I. In addition to PU, 54 20-mm-long blocks of a pork rib bone were used to simulate the osseous variability in the oral cavity. Substrates were drilled using the sequence of burs recommended by the manufacturer for each implant model. The last bit had a smaller diameter than the screw. Implants were inserted from the lowest to highest density of PU, so the increasing density of the PU could not affect the morphological structure of the screws. The last substrate used was the rib bone. During insertion, the torque was measured for each 90° turn of the implant using a Mackena® digital torque meter (Mackena Indústria e Comércio Ltda., São Paulo, São Paulo, Brazil).
Because the same 54 implants were used for insertion in the various substrate types and densities, they were analyzed using a scanning electron microscope (EVO MA 10, Carl ZEISS) before and after insertion for each assay to control for possible morphological changes to the screw surface. Two magnifications were used: 40× for analyzing the implant dimensions and 100× to analyze the apical region [10].
After IT was measured, primary stability was assessed by RFA using an Osstell Mentor (Integração Diagnostics AB, Göteborgsvägen, Suécia). The frequency transducer (SmartPeg) was connected to the implant, and the implant stability quotient (ISQ) was measured four times for each inserted screw. The average and standard deviation were calculated for subsequent comparison and discussion.
In addition to IT and RFA, the pullout assay was performed according to ASTM F543. Each implant, inserted into a substrate, was connected to a universal testing machine (EMIC® model DL-10000N, São José dos Pinhais, Paraná, Brazil) using a device made specifically for this study. After positioning the substrate/implant in the machine, an axial traction force was applied with a constant velocity of 2 mm/min and a 200 kg load cell. For all implants, a preload of 10 N and a 30-s settling time were used. The data for the maximum pullout force were obtained using Software Tesc 1.13.
After the normality of the data was verified using the Kolmogorov-Smirnov test, analysis of variance (ANOVA) followed by the Tukey test (α = 5 %) was used. Pearson’s test for correlation was used to measure the correlation between methods.
Results
Insertion torque
The various implant shapes were not significantly different when inserted into 15 PCF PU (p > 0.05). The conical implants performed better than the cylindrical implants in the 20 PCF PU, where higher averages were measured for the IH conical (33.89 ± 3.48) and MC conical (33.00 ± 2.91) implants, which were also similar to each other (p > 0.05). Conversely, the MC cylindrical (9.44 ± 0.72) and EH cylindrical (9.89 ± 0.60) implants had lower averages. The conical implants were also better in 40 PCF PU, where the highest average was measured for the MC conical implant (47.89 ± 1.36), which was similar to the other implants with the same shape (p > 0.05). The MC cylindrical implant had a lower average and was significantly different than the conical implants (p < 0.05). In the bone, the highest average IT was measured for the MC conical implant (73.33 ± 21.79) and the lowest for the IH cylindrical implant (22.22 ± 6.90) (Table 1).
Resonance frequency analysis
RFA did not reveal any statistically significant differences (p > 0.05) between the implants inserted at the different PU densities. In the bone, the IH cylindrical and IH conical had the lowest averages, which were similar to each other (p > 0.05) (Table 2).
Pullout assay
In the pullout assay, the implants inserted into 15 PCF PU were not significantly different (p > 0.05). In 20 PCF PU, the highest average was measured using the MC conical implant (298 ± 37.54), and this value was not different than that of the other conical implants (p > 0.05). The lowest average was measured for the IH cylindrical implant (51.65 ± 11.93). In 40 PCF PU, the MC conical implant had the highest average (910 ± 85.77) and was significantly different than the other implants (p < 0.05). The IH cylindrical implant had the lowest average. In the bone, the highest average was also measured for the MC conical implants and the lowest for the IH cylindrical implants (Table 3).
Pearson correlation
To verify the correlation between the methods used to assess primary stability, a Pearson correlation was used (Table 4).
In the Pearson analysis,
-
1.
Values >0.70 (positive or negative) indicate strong correlation.
-
2.
Values 0.30 to 0.70 (positive or negative) indicate moderate correlation.
-
3.
Values 0 to 0.30 indicate weak correlation.
Morphological analysis of the implants
Scanning electron microscopy (SEM) analysis of the implants did not reveal any morphological differences between photomicrographs taken before and after the mechanical tests, just accumulation of organic material between the threads from the implant (Figs. 1 and 2).
Discussion
The influence of primary stability on osseointegration has been difficult to predict, as it depends not only on bone density and IT but also on characteristics related to the macro- and microgeometry of the screw [11]. Biomechanical aspects of primary stability can be evaluated using the IT, RFA, removal torque, and pullout assay methods, along with histological measurements [12].
To limit and overcome the shortcomings of these analyses and based on the principle that the macro-geometry of the implant is one of the most important factors governing initial stability [13], this study investigated the influence of six implant designs inserted into various substrate types and densities on primary stability using the correlation of the following methods: IT, RFA, pullout test, and morphological analysis by SEM.
The external surface of the implant directly interferes with osseointegration, as it is in close contact with the bone tissue [14]. Using SEM, one can analyze detailed morphological and surface differences in the implants to find defects in the screw or to characterize the surface. In this study, photomicrographs taken before and after the mechanical tests were compared, and no differences in thread configuration, cracks, or fractures in the screw were identified, justifying the use of the same implant in several substrates.
Conical and cylindrical implants are the shapes most commonly found commercially. Conical implants promote a uniform bone compaction and distribute forces to the surrounding bone more equally [15]. In this study, conical implants performed significantly better in the IT and pullout tests in 20 and 40 PCF PU and in the pork rib bone, consistent with the literature, where other studies have shown significantly improved primary stability, ease of insertion, and resistance in conical implants compared to cylindrical implants [16].
The width of the screw increases primary stability, as it anchors better in the buccal and lingual cortexes, has a larger implant/bone surface area, and increases resistance to traction. When the bone is less dense, size selection (length/width) of the implant determines treatment success [17]. The conical implant groups used in this study had the same dimensions, 4.3 mm diameter by 10 mm length; the cylindrical implant groups were 4.0 mm diameter by 11 mm long, except for the cylindrical screw with an IH platform, which had a slightly smaller diameter of 3.75 mm.
Screw dimensions were selected based on the various commercially available prosthetic platforms and implant sizes. The slightly smaller diameter of the IH cylindrical implant did not interfere with the primary stability measured by IT and RFA when compared to the other cylindrical implants inserted into 15 and 20 PCF PU. However, in the 40 PCF PU and rib bone, this implant model had a statistically lower pullout strength than the others in the same group—the EH cylindrical and MC cylindrical screws—possibly due to the different external characteristics of this screw.
Implant’s threads increase its contact area with the bone and improve the load distribution at the implant/bone interface, improving primary stability [18]. In this study, the cylindrical implant with an IH platform performed poorly for IT, pullout test, and RFA compared to the other cylindrical screws. According to the manufacturer, this implant model is indicated for types I and II bone and is advantageous because it has a double thread, allowing for more rapid installation with less trauma, high cutting power, and a small thread in the neck region. However, this screw was difficult to insert, especially in the pork rib bone and the 40 PCF PU—the substrates with the highest density and corresponding to type I bone by the classification system [19]—and required different burs than those recommended by the manufacturer to be used.
In the study, the implants showed different insertion torque values; however, although the type of platform interferes with the screw shape to ensure the strength of implants, the variation in insertion torque cannot be assigned to only one factor, but a set of factors that characterize each of macro-geometry implant models and the density of the bone where the implants were inserted.
Bone volume and density are associated with surgical implantation success. The characteristics of natural bone (density, rigidity, hardness) vary widely in the mouth as a whole or even in the same bone segment, affecting primary stability [12]. To simulate this bone variability, pork rib bones were used in this study [11, 18] in addition to the PU blocks, which are made of a consistent and uniform material with physical properties similar to the human bone [12], allowing the effect of the substrate heterogeneity in the analysis of implant shape.
When bone quality is not favorable, contact between the bone and implant decreases, harming primary stability [20, 21]. In this study, clinical bone conditions were simulated using different artificial bone densities, 15, 20, and 40 PCF, and natural bone samples (pork rib bone). In the three assessment methods used for primary stability, IT, RFA, and pullout test, none of the implants were significantly different when inserted into 15 PCF PU, with a density comparable to type III bone. The similar study [22] reported similar results for IT in type II and type III bones and suggested that factors related to bone density and implant design directly affect primary stability.
A successful implant normally has an ISQ value above 65; an ISQ <50 may indicate potential failure or an increased risk of failure [4]. In this study, although the ISQ values were favorable for primary stability, the different groups of implants tested were not statistically significant (p > 0.05) in any PU density. The implants inserted in the pork rib bone were similar, except for the IH cylindrical screws, which had a higher average ISQ (p < 0.05).
The correlations for RFA/pullout test (p = 0.461) and RFA/IT (p = 0.634) were moderate based on the Pearson analysis. While the different models were significantly different for the IT and pullout tests, they were similar in the RFA, suggesting, as observed in the literature, a discrepancy between RFA and the other methods for assessing primary stability, implant contact, such as IT, removal, bone mineral density, and histological analysis of the bone-implant interface [23]. These results demonstrate that using a single method to evaluate primary stability is not reliable.
Comparing the pullout test results with IT also returned a moderate Pearson correlation (p = 0.658). In this case, forces increased proportionally to bone density and differed between implant models, with the conical implants performing better than the cylindrical implants. These findings have also been described in the literature [24, 25], showing that the pullout test is correlated with IT and screw characteristics and is thought to be an objective method for evaluating the mechanical resistance of the implants.
As for an implant that performs best for most of the substrates and in the methods used, the results show that conical implants are better than the cylindrical implants, as the conical implant with an MC platform had the highest averages for the methods used [26]. Conversely, the cylindrical implant with an IH platform had worse results than the other implants with the same shape and the conical implants, likely due to the shape of its neck. These results indicate that the shape and external characteristics of the screw strongly affect its biomechanics and primary stability.
Conclusions
In summary, it can be concluded that comparison of the various implant shapes demonstrated that the conical implants had better primary stability; analysis of the various types of substrates showed that 15 PCF PU did not have enough resistance to analyze implant shape; the density of 40 PCF PU and the pork rib bone showed better results for primary stability; the correlation between the methods was moderate, indicating that all of the methods effectively assess primary stability.
References
Rabel A, Köhler SG, Schmidt-Westhausen AM (2007) Clinical study on the primary stability of two dental implant systems with resonance frequency analysis. Clin Oral Investig 11:257–265
Chang CL, Chen CS, Huang CH, Hsu ML (2012) Finite element analysis of the dental implant using a topology optimization method. Med Eng Phys 34:999–1008
Desai SR, Desai MS, Katti G, Karthikeyan I (2012) Evaluation of design parameters of eight dental implant designs: a two-dimensional finite element analysis. Niger J Clin Pract 15:176–181
Kim DS, Lee WJ, Choi SC, Lee SS, Heo MS, Huh KH, Kim TI, Yi WJ (2014) Comparison of dental implant stabilities by impact response and resonance frequencies using artificial bone. Med Eng Phys 36:715–720
Mazzo CR, Reis AC, Shimano AC, Valente ML (2012) In vitro analysis of the influence of surface treatment of dental implants on primary stability. Braz Oral Res 26:313–317
Jung UW, Kim S, Lee IK, Kim MS, Lee JS, Kim HJ (2013) Secondary stability of microthickness hidroxyapatite-coated dental implants installed without primary stability in dogs. Clin Oral Implants Res 25:1169–1174
Premnath K, Sridevi J, Kalavathy N, Nagaranjani P, Sharmila MR (2013) Evaluation of stress distribution in bone of different densities using different implant designs: a three-dimensional finite element analysis. J Indian Prosthodont Soc 13:555–559
Bayarchimeg D, Namgoong H, Kim BK, Kim MD, Kim S, Kim TI, Seol YJ, Lee YM, Ku Y, Rhyu IC, Lee EH, Koo KT (2013) Evaluation of the correlation between insertion torque and primary stability of dental implants using a block bone test. J Periodontal Implant Sci 43:30–36
Pang X, Huang Y (2012) Physical properties of nano-HAs/ZrO2 coating on surface of titanium materials used in dental-implants and its biological compatibility. J Nanosci Nanotechnol 12:902–910
Valente ML, Shimano AC, Mazzo CR, Lepri CP, dos Reis AC (2014) Analysis of the surface deformation of dental implants submitted to pullout and insertion test. Indian J Dent Res 25:32–35
Freitas AC Jr, Bonfante EA, Giro G, Janal MN, Coelho PG (2012) The effect of implant design on insertion torque and immediate micromotion. Clin Oral Implants Res 23:113–118
Elias CN, Rocha FA, Nascimento AL, Coelho PG (2012) Influence of implant shape, surface morphology, surgical technique and bone quality on the primary stability of dental implants. J Mech Behav Biomed Mater 16:169–180
Javed F, Ahmed HB, Crespi R, Romanos GE (2013) Role of primary stability for successful osseointegration of dental implants: factors of influence and evaluation. Interv Med Appl Sci 5:162–167
Jarmar T, Palmquist A, Brånemark R, Hermansson L, Engqvist H, Thomsen P (2008) Characterization of the surface properties of commercially available dental implants using scanning electron microscopy, focused ion beam, and high-resolution transmission electron microscopy. Clin Implant Dent Relat Res 10:11–22
Dos Santos MV, Elias CN, Cavalcanti Lima JH (2011) The effects of superficial roughness and design on the primary stability of dental implants. Clin Implant Dent Relat Res 13:215–223
Wu SW, Lee CC, Fu PY, Lin SC (2012) The effects of flute shape and tread profile on the insertion torque and primary stability of dental implants. Med Eng Phys 34:797–805
Shemtov-Yona K, Rittel D, Levin L, Machtei EE (2014) Effect of dental implant diameter on fatigue performance. Part I: mechanical behavior. Clin Implant Dent Relat Res 16:172–177
Chowdhary R, Jimbo R, Thomsen C, Carlsson L, Wennerberg A (2013) Biomechanical evaluation of macro and micro designed screw-type implants: an insertion torque and removal torque study in rabbits. Clin Oral Implants Res 24:342–346
Lekholm U, Zarb GA (1985) Patient selection and preparation. In: Branemark PI, Zarb G, Albrektsson T (eds). Tissue-integrated prostheses: osseointegration in clinical Dentistry. Quintessence, pp 199–209.
Trisi P, Berardi D, Paolantonio M, Spoto G, D’Addona A, Perfetti G (2013) Primary stability, insertion torque, and bone density of conical implants with internal hexagon: is there a relationship? J Craniofac Surg 24:841–844
Herekar M, Sethi M, Ahmad T, Fernandes AS, Patil V, Kulkarni H (2014) A correlation between bone (B), insertion torque (IT), and implant stability (S): BITS score. J Prosthet Dent 112:805–810
Kim SJ, Kim MR, Rim JS, Chung SM, Shin SW (2010) Comparison of implant stability after different implant surface treatments in dog bone. J Appl Oral Sci 18:415–420
Da Cunha H, Francischone CE, Filho HN, de Oliveira RC (2004) A comparison between cutting torque and resonance frequency in the assessment of primary stability and final torque capacity of standard and TiUnite single-tooth implants under immediate loading. Int J Oral Maxillofac Implants 19:578–585
Wegmann K, Gick S, Heidemann C, Pennig D, Neiss WF, Müller LP, Eysel P, Sobottke R (2013) Biomechanical evaluation of the primary stability of pedicle screws after augmentation with an innovative bone stabilizing system. Arch Orthop Trauma Surg 133:1493–1499
Helgeson MD, Kang DG, Lehman RA Jr, Dmitriev AE, Luhmann SJ (2013) Tapping insertional torque allows prediction for better pedicle screw fixation and optimal screw size selection. Spine J 13:957–965
Jimbo R, Tovar N, Anchieta RB, Machado LS, Marin C, Teixeira HS, Coelho PG (2014) The combined effects of undersized drilling and implant macrogeometry on bone healing around dental implants: an experimental study. Int J Oral Maxillofac Surg 43:1269–1275
Acknowledgments
We thank the foundation for supporting the research in the state of São Paulo (FAPESP—process number 2012/09208-0) and for funding the study.
Conflict of interest
The authors declare that they have no conflict/s of interest related to the present study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Valente, M.L.d.C., de Castro, D.T., Shimano, A.C. et al. Analysis of the influence of implant shape on primary stability using the correlation of multiple methods. Clin Oral Invest 19, 1861–1866 (2015). https://doi.org/10.1007/s00784-015-1417-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1417-4