Abstract
Objectives
Geranylgeraniol (GGOH) has been reported as a potential treatment option for bisphosphonate-associated osteonecrosis of the jaws (BP-ONJ). The aim of this study was to analyze the effects of GGOH on endothelial progenitor cells (EPC) after bisphosphonate treatment in vitro.
Materials and methods
EPC were incubated with different nitrogen (N-BPs: ibandronate, pamidronate, zoledronate) and a non-nitrogen-containing bisphosphonates (NN-BP: clodronate) with and without GGOH. Cell viability was measured by MTT and PrestoBlue assay. Migration ability was analyzed with a Boyden and Scratch assay. Apoptosis rates were determined by colony-forming, Tunel and ToxiLight assays.
Results
Negative effects of N-BPs on EPC were shown in all tests without GGOH. The substitution of GGOH demonstrated significantly increased cell viability (MTT: p each N-BP ≤0.004; PrestoBlue: p each N-BP <0.001) and migration ability (Boyden: p each N-BP <0.001; Scratch: p each N-BP <0.001). Concerning the apoptosis rates, increased EPC colony densities (p each N-BP ≤0.009), decreased numbers of apoptotic cells in the Tunel assay (p each N-BP <0.001), and a decreased adenylate kinase release in the ToxiLight assay (p each N-BP ≤0.03) were observed. For the clodronate-treated cells, no significant differences could be detected with or without GGOH in any assay (p each N-BP/NN-BP >0.05).
Conclusions
GGOH cell treatment reversed the negative effects of bisphosphonates on EPC.
Clinical relevance
These findings support the hypothesis that systemic or local GGOH treatment might lead to new therapeutic strategies for BP-ONJ.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Bisphosphonate-associated osteonecrosis of the jaws (BP-ONJ) is a side effect of bisphosphonate therapy with an increasing incidence [1]. To date, the pathophysiology has not been clarified in detail, and there still is no effective causal therapy or prevention strategy.
Concerning the pathophysiology, several theories are being discussed in the literature. A multifactorial genesis is very likely. Typical theories describe reduced bone remodelling, an impact on the soft tissues and the immune system, and trigger factors such as periodontal disease and enoral wounds. Some research focuses on the strong negative influence of bisphosphonates on angiogenesis as a pathophysiological contributing factor since BP-ONJ might be an avascular necrosis [2–4]. This theory is supported by the fact that other recently developed antiangiogenic agents are also associated with the occurrence of osteonecroses of the jaws, e.g., anti-VEGF-antibodies and tyrosine-kinase inhibitors [5, 6]. Bisphosphonates’ negative influence on mature endothelial cells in vitro has already been reported [7, 8], and it has been confirmed in vivo in mice treated with bisphosphonates [9]. This is reflected in in vivo investigations on BP-ONJ patients, showing a reduced density of circulating endothelial cells and decreased VEGF serum concentrations [10, 11]. In vitro studies showing bisphosphonates had a negative impact on endothelial progenitor cells (EPC) supported the in vivo results [12]. These findings, which are also reflected in in vivo investigations on BP-ONJ patients showing a reduced density of circulating EPC, led to the assumption that EPC might play a role in BP-ONJ development and therefore might be of scientific interest [10].
In addition to the unknown pathophysiology, there is no effective causal therapy for this disease to date.
Small necrotic areas can be treated by a conservative BP-ONJ management, while in advanced stages, surgical treatment should be preferred [13, 14]. Therapeutic options such as hyperbaric oxygen and soft laser therapy could not meet the expectations placed in them [15–18]. For these reasons, there was and still is a necessity for new therapy options.
Regarding this matter, a recent study focused on the molecular pharmacological point of action of nitrogen-containing bisphosphonates (N-BPs), which is decreasing the synthesis of the isoprenoid geranylgeraniol (GGOH) in the mevalonate pathway. It was demonstrated that the negative effects of N-BPs on cell characteristics of endothelial cells, fibroblasts, and osteoblasts could be reversed by GGOH substitution [18].
Therefore, with respect to the relevance of EPC and angiogenesis in BP-ONJ development, the aim of this study was to analyze the effects of GGOH substitution on EPC viability, migration ability and apoptosis rate after bisphosphonate treatment in vitro.
Materials and methods
Bisphosphonates
The three nitrogen-containing bisphosphonates (N-BPs) ibandronate (Bondronat®; Roche, Welwyn Garden City, UK), pamidronate (Pamifos®; Medac GmbH, Wedel, Germany), and zoledronate (Zometa®; Novartis, Nürnberg, Germany) as well as the non-nitrogen-containing bisphosphonate (NN-BP) clodronate (Bonefos®; Bayer, Leverkusen, Germany) were used. The concentrations used for the bisphosphonates (BP 0, 5, and 50 μM) and GGOH (10 µM; Sigma, Steinheim, Germany) have been evaluated in previous experiments [7, 8, 12, 16, 18, 19].
EPC culture assay
Mononuclear cells (MNCs) were isolated by density gradient centrifugation from human peripheral blood with Biocoll (Biochrom KG, Berlin, Germany) like previously described by Ziebart et al. [12, 20]. After isolation, total MNCs (8 × 106 cells/ml medium) were seeded on 25-cm2 culture flasks coated with human fibronectin (Sigma) and maintained in endothelium basal medium (EBM; Lonza, Basel Switzerland) supplemented with endothelium growth medium (EGM; Lonza) SingleQuots, 100 ng/ml vascular endothelium growth factor (VEGF; Sigma), and 20 % fetal calf serum (FCS; Sigma).
Cell viability
MTT assay
For the 3-(4,5-dimethyl-2-thiazolyl)-2,5-diphenyl 2H-tetrazolium bromide assay (MTT assay), EPC were transferred into six-well plates (Sigma; EPC 250,000 cells/well). After 24 h, the cells were incubated with different bisphosphonate concentrations (0, 5, and 50 μM) and GGOH (10 μM). The control groups received no GGOH. After 72 h, the cell viability was evaluated using the MTT colorimetric assay (Sigma). Viable cells ferment tetrazolium bromide to formazan, which can be photometrically measured after cell lysis using a Synergy HT Multi-Mode Microplate Reader (corresponding setting: absorbance; BioTek Instruments, Winooski, USA).
PrestoBlue assay
The PrestoBlue assay (Invitrogen, Darmstadt, Germany) was used to analyze the EPC viability at different points of measurements and more frequently compared to the MTT assay. Six-well plates (Sigma) were prepared similar to the MTT assay (EPC 250,000 cells/well). After 24 h, the cells were incubated with the mentioned bisphosphonates in increasing amounts (0, 5, and 50 μM) and GGOH (10 μM). The control groups received no GGOH. At 0, 24, 48, and 72 h after applying 10 % PrestoBlue, the reduction induced color switchover of resazurin to resorufin was measured with a Synergy HT Multi-Mode Microplate Reader (corresponding setting: fluorescence; BioTek Instruments).
Migration
Boyden migration assay
For the migration assay, a 24-well Boyden chamber assay system (Thin-Cert©; Greiner BioOne, Essen, Germany) was used according to the manual as previously described [2, 8]. EPC were cultured in 24-well plates (Greiner BioOne; EPC 100,000 cells/well). After 24 h, EPC were incubated with 50 μM of the different bisphosphonates for 72 h in two diverse test lines with and without GGOH (10 μM) and then transferred into the migration chambers (Greiner BioOne; EPC 12,500 cells/chamber). The cells were stained after 24 h with Calcein-AM fluorescent dye (Invitrogen). The inserts were transferred to the wells of freshly prepared black 24-well plates (Sigma) containing 500 μl Trypsin-EDTA (Invitrogen) per well and incubated for 10 min in a cell culture incubator at 37 °C and 5 % CO2. The inserts were discarded, and 250 μl of each well of the Trypsin-EDTA solution, containing the detached migratory cells, was transferred to a well of flat-bottom black 24-well plates with transparent bottom (Sigma). A Synergy HT Multi-Mode Microplate Reader (corresponding setting: fluorescence; BioTek Instruments) was used for quantification.
Scratch assay
For the Scratch assay, EPC were transferred into six-well plates (Sigma; EPC 250,000 cells/well). After 24 h, a scratch wound using a sterile pipette tip (Sigma) was performed, and the size of the gap was measured and set to 100 %. The cells were incubated with the mentioned bisphosphonates (50 μM) and GGOH (10 μM). The control groups received no GGOH. The closing of the scratch wound was measured for 72 h or until the scratch wounds were closed.
Apoptosis
Colony-forming assay
To examine the effects on colony-forming (CF) ability, EPC were transferred into six-well plates (Sigma; EPC 250,000 cells/well). After 24 h, the cells were incubated with the bisphosphonates (0, 5, and 50 μM) and GGOH (10 μM). The control groups received no GGOH. After 72 h EPC were transferred and cultured in MethoCult© culture medium (STEMCELL Technologies, Vancouver, Canada) on six-well plates (Sigma) for 14 days, like described in the manufacturer’s protocol. After 14 days, the culture plates were analyzed for colony formation.
Tunel assay
For the apoptosis assay, EPC were seeded in six-well plates (Sigma; EPC 250,000 cells/well). After 24 h, cells were incubated with the bisphosphonates (50 μM) and GGOH (10 μM) for 72 h. Controls received no GGOH. Next, cells were dissolved in trypsin-EDTA (Invitrogen) and centrifuged onto coverslips (Sigma) at 2000 rpm for 5 min. Then, cells were fixed with 3 % paraformaldehyde (Sigma) for 10 min at room temperature (RT), permeabilized with 0.1 % Triton X-100 (Sigma), 0.1 % sodium citrate (Sigma) for 2 min on ice, washed twice with phosphate-buffered saline (PBS; Invitrogen), pH 7.4, and incubated for 1 h at 37 °C in the dark with a dUTP nick end labeling (TUNEL) reaction mixture (Boehringer, Indianapolis, USA) for in situ detection of cell death. After washing twice with PBS (Invitrogen), pH 7.4, the cells were incubated at RT with the Hoechst solution (Sigma) for 5 min. All Hoechst-positive nuclei as well as TUNEL-positive nuclei were visualized using a Zeiss Axioplan fluorescence microscope (Carl Zeiss, Göttingen, Germany) as previously described [2].
ToxiLight assay
The ToxiLight BioAssay (Lonza) is a cytotoxicity assay that measures the release of adenylate kinase (AK) from damaged cells. Six-well plates (Sigma) were prepared similarly to the MTT assay (EPC 250,000 cells/well). After 24 h, the cells were incubated with the bisphosphonates (0, 5, and 50 μM) and GGOH (10 μM). The control groups received no GGOH. After 0, 24, 48, and 72 h, the supernatant was mixed with ToxiLight dissolution and the emitted light intensity was measured using a Synergy HT Multi-Mode Microplate Reader (corresponding setting: luminescence; BioTek Instruments).
Statistical analysis
Each experiment has been performed in triplicate. Comparisons were analyzed by ANOVA (post hoc test: Tukey) for experiments with more than two subgroups (SPSS version 17.0; IBM, Ehningen, Germany). Considered as statistically significant were p values ≤0.05. The black bar in the middle of each box represents the median. The box includes all values between the 25th and the 75th percentile. Whiskers indicate values within 1.5 interquartile range (IQR). Outliers within 3 IQR are represented as circles. Outliers outside of 3 IQR are represented as asterisks.
Asterisks demonstrate a statistically significant difference between the test line without GGOH and the test line with GGOH for the particular point of measurement (p ≤ 0.05).
Results
Cell viability
MTT assay
In the NN-BP clodronate group, no significantly decreased cell viability could be observed for any of the tested BP concentrations (5, 50 μM; p each ≥0.905), and GGOH had no effect (p each ≥0.808).
For the N-BP ibandronate (50 μM), a significantly decreased cell viability was observed (p < 0.001) and a significantly increased cell viability after GGOH substitution could be demonstrated (p < 0.001). Incubation with pamidronate or zoledronate decreased the cell viability significantly for both concentrations (pamidronate 5, 50 μM; p each ≤0.005; zoledronate 5, 50 μM; p each ≤0.001). The substitution of GGOH increased cell viability (pamidronate: p each ≤0.004; zoledronate: p each <0.002; Fig. 1).
MTT assay. X-axis = experimental groups and different bisphosphonate concentrations (μM = micromolar); Y-axis = cell viability, optical density at 550 nm (AU = absorbance units); Asterisks indicate significant difference between the test line without GGOH (no GG) and the test line with GGOH (+ GG; p ≤ 0.05)
PrestoBlue assay
With clodronate no difference between the two test lines with and without GGOH could be demonstrated for any BP concentration at any point of time (p each ≥0.991).
For 50 μM ibandronate, the substitution of GGOH increased the cell viability significantly after 48 and 72 h (p each <0.001). Between the two pamidronate test lines with and without GGOH, a significantly increased cell viability for the BP concentration of 5 μM after 72 h (p < 0.001) and for the BP concentration of 50 μM after 48 and 72 h could be detected (p < 0.001 for each). For the zoledronate concentrations of 5 and 50 μM, the substitution of GGOH revealed a significantly increased cell viability after 48 and 72 h (p each <0.001; Fig. 2).
PrestoBlue assay. X-axis = experimental groups, different points of measurement and different bisphosphonate concentrations (μM = micromolar); Y-axis = cell viability (RFU = relative fluorescence units); Asterisks indicate significant difference between the test line without GGOH (no GG) and the test line with GGOH (+ GG; p ≤ 0.05)
Migration
Boyden migration assay
Compared to the control group, the NN-BP clodronate showed no significantly decreased migration ability (p = 1.0). GGOH had no influence (p = 0.977).
The other BPs decreased the migration ability significantly in comparison to the control group (p < 0.001 each), and the substitution of GGOH showed a positive effect (p < 0.001 each; Fig. 3)
Scratch assay
There were no statistical significant differences in the clodronate group with or without GGOH (p each ≥0.922).
For all N-BP, a significantly increased scratch wound closure after GGOH substitution could be demonstrated after 48 and 72 h (p each ≤0.001; Fig. 4).
Scratch assay. X-axis = experimental groups and different points of measurement; Y-axis = open scratch wound area (in %) compared to the starting point after 0 h (set to 100 %); Asterisks indicate significant difference between the test line without GGOH (no GG) and the test line with GGOH (+ GG; p ≤ 0.05)
Apoptosis
Colony-forming assay
The NN-BP clodronate did not decrease the colony density in the different concentrations (5, 50 μM; p each ≥0.93), and the substitution of GGOH had no effect (p each ≥0.907).
Ibandronate decreased the colony density significantly only at a concentration of 50 μM (p < 0.001), and the addition of GGOH for this BP concentration had a reversing effect (p < 0.001). Pamidronate and zoledronate reduced the colony density at 5 and 50 μM (p each <0.001). The GGOH substitution had a positive effect for both BPs (ibandronate: p each ≤0.009; zoledronate: p each <0.001; Fig. 5).
Tunel assay
Compared to the control group, the NN-BP clodronate showed no significantly increased apoptosis rate (p = 0.631) and no significant difference by adding GGOH (p = 1.0).
For each of the tested N-BPs, a significantly increased apoptosis rate could be observed in comparison to the control group (p each <0.001) and a significantly reduced apoptosis rate after GGOH substitution could be demonstrated (p each <0.001; Fig. 6).
ToxiLight assay
Neither clodronate nor the additional substitution of GGOH had any effect (p each ≥0.315).
The substitution of GGOH on EPC treated with ibandronate, pamidronate, or zoledronate reduced the release of adenylate kinase (AK) significantly for 5 μM of BP after 48 and 72 h (ibandronate p ≤ 0.03 each; pamidronate p ≤ 0.004 each; zoledronate p ≤ 0.001each) and for 50 μM after 24, 48, and 72 h (ibandronate: p < 0.001 each; pamidronate and zoledronate: p < 0.001 each; Fig. 7a, b).
a, b ToxiLight assay. a clodronate, ibandronate; b pamidronate, zoledronate. X-axis = experimental groups, different points of measurement and different bisphosphonate concentrations (μM = micromolar); Y-axis = adenylate kinase (AK) release (RLU = relative luminescence units); Asterisks indicate significant difference between the test line without GGOH (no GG) and the test line with GGOH (+ GG; p ≤ 0.05)
Discussion
Overall, the results of this study demonstrated that the negative influences of nitrogen-containing bisphosphonates on EPC could be reversed by geranylgeraniol in vitro.
In this context, the following references will give a detailed overview over the exact mode of action of bisphosphonates in the mevalonate pathway and the function of geranylgeraniol [18, 21–24].
The strongest influence of GGOH substitution could be observed after N-BP pamidronate and zoledronate incubation, which are the bisphosphonates most frequently associated with BP-ONJ development [2, 4, 7–9]. There was no effect in the NN-BP treated EPC, since NN-BPs work as ATP-analogues and are not involved in the mevalonate pathway.
The improved EPC viability, migration ability, and decreased apoptosis rate after bisphosphonate incubation and GGOH treatment might be of special significance for BP-ONJ development and therapy with regard to the physiological functionality of EPC. After deriving from the bone marrow, EPC migrate to the vascular system, where they circulate and differentiate into mature endothelial cells [25–28]. Through the vessel system, the circulating EPC can reach the action sites, such as wounds or necrotic areas that need microvessel creation and revascularization. They then leave the vessel system by migration through the vascular wall and migrate into the surrounding tissues and the wound area, where they can stimulate the revascularization in two main ways: First, EPC stimulate the sprouting angiogenesis as well as the intussusceptive angiogenesis from preexisting vessels through the strong autocrine and paracrine effects of the production of several pro-angiogenic growth factors such as VEGF. Second, they can migrate into the surrounding tissues, inducing the development of completely new vessels through a process called neovasculogenesis [12, 18, 25–28]. Within this complex biochemical cascade, there are two points where bisphosphonates can interact and influence EPC: First, due to the accumulation of bisphosphonates in the entire skeleton and the long half-life of over 20 years depending on the specific bisphosphonate, they might interact with the EPC in the bone marrow and influence the release of EPC from the bone marrow niches through reduced cell viability and migration ability. Second, the local bisphosphonate concentrations in the hard and soft tissues of the oral cavity could interact with the stationary vessel cells and EPC in the mandibular bone, supporting the development and maintenance of BP-ONJ due to the strong negative influence on their viability and migration ability directly on site. It might be possible that at the above described points of action (bone marrow, oral tissues) bisphosphonates induce an EPC apoptosis, which automatically leads to a completely switched off EPC viability and migration ability. Overall, the associated impairment of microvessel creation might result in a significantly decreased wound healing of the oral hard and soft tissues, e.g., after surgical procedures, which could consequently result in the development of BP-ONJ.
Assuming BP-ONJ is caused in some way by the antiangiogenic properties of bisphosphonates on EPC, and therefore on the bone and soft tissue vascularization, GGOH might be an option for BP-ONJ prevention and therapy. For N-BPs, GGOH could restore the restriction of EPC viability, migration ability, and apoptosis rate back to regular conditions, which might result in normal revascularization.
An important question in this context is the potential mode of GGOH application in patients [18]. Since the effects of N-BPs on tumor cells can be at least partially neutralized by GGOH, a systematic GGOH application might decrease the pharmacological power of the applied bisphosphonates in the entire body and therefore also reduce the intended effects and the positive benefits of the bisphosphonates on the tumor growth in patients with malignant diseases [29–31]. In contrast, a topical application of GGOH with mouth rinses or local drug delivery systems could be performed to treat and prevent the development of BP-ONJ [18]. Therefore, further studies should focus on the optimal administration method, the exact indication, and the adequate concentration and duration of GGOH treatment. In addition, a better understanding of GGOH pharmacokinetics is absolutely essential to prevent possible side effects of GGOH treatment like the abovementioned [18].
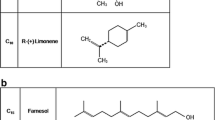
It is interesting that many other substances of the isoprenoid family, such as eugenol, farnesol, R-limonene, menthol, and squalene, are not able to have a positive effect on bisphosphonate-treated cells such as HUVEC, fibroblasts, and osteogenic cells. Only GGOH seems to harbor this effect [32]. In comparison to pro-angiogenic growth factors such as VEGF or prominin, GGOH offers the advantage of working directly on the N-BPs’ pharmacological point of action, while VEGF or prominin would only indirectly stimulate angiogenesis. This study has also some limitations. Since this study has been designed as an in vitro study, it is debatable if the isolated EPCs demonstrate the same cell performance after bisphosphonate treatment in vitro as in an in vivo situation. Further, it is unknown if the bisphosphonate concentrations we used in the cell cultures can sufficiently imitate the bisphosphonate concentrations affecting on EPCs in the in vivo situation. Consequently, it is absolutely necessary to transfer the findings of this study in an in vivo model in order to overcome the mentioned limitations and to gather more information with reference to the outstanding questions.
References
Walter C, Sagheb K, Bitzer J, Rahimi-Nedjat R, Taylor KJ (2014) Analysis of reasons for osteonecrosis of the jaws. Clin Oral Investig [Epub ahead of print]
Pabst AM, Ziebart T, Koch FP, Taylor KY, Al-Nawas B, Walter C (2012) The influence of bisphosphonates on viability, migration, and apoptosis of human oral keratinocytes—in vitro study. Clin Oral Investig 16:87–93
Hagelauer N, Pabst AM, Ziebart T, Ulbrich H, Walter C (2014) In vitro effects of bisphosphonates on chemotaxis, phagocytosis, and oxidative burst of neutrophil granulocytes. Clin Oral Investig [Epub ahead of print]
Walter C, Laux C, Sagheb K (2014) Radiologic bone loss in patients with bisphosphonate-associated osteonecrosis of the jaws: a case-control study. Clin Oral Investig 18:385–390
Van Poznak C (2010) Osteonecrosis of the jaw and bevacizumab therapy. Breast Cancer Res Treat 122:189–191
Koch FP, Walter C, Hansen T, Jäger E, Wagner W (2011) Osteonecrosis of the jaw related to sunitinib. Oral Maxillofac Surg 15:63–66
Walter C, Klein MO, Pabst A, Al-Nawas B, Duschner H, Ziebart T (2010) Influence of bisphosphonates on endothelial cells, fibroblasts, and osteogenic cells. Clin Oral Investig 14:35–41
Walter C, Pabst A, Ziebart T, Klein MO, Al-Nawas B (2011) Bisphosphonates affect migration ability and cell viability of HUVEC, fibroblasts and osteoblasts in-vitro. Oral Dis 17:194–199
Pabst AM, Ziebart T, Ackermann M, Konerding MA, Walter C (2013) Bisphosphonates' antiangiogenic potency in the development of bisphosphonate-associated osteonecrosis of the jaws: influence on microvessel sprouting in an in vivo 3D Matrigel assay. Clin Oral Investig 18:1015–1022
Allegra A, Oteri G, Nastro E, Alonci A, Bellomo G, Del Fabro V et al (2007) Patients with bisphosphonates-associated osteonecrosis of the jaw have reduced circulating endothelial cells. Hematol Oncol 25:164–169
Santini D, Vincenzi B, Avvisati G, Dicuonzo G, Battistoni F, Gavasci M et al (2002) Pamidronate induces modifications of circulating angiogenic factors in cancer patients. Clin Cancer Res 8:1080–1084
Ziebart T, Pabst A, Klein MO, Kaemmerer P, Gauss L, Bruellmann D et al (2011) Bisphosphonates: restrictions for vasculogenesis and angiogenesis: inhibition of cell function of endothelial progenitor cells and mature endothelial cells in vitro. Clin Oral Investig 15:105–111
Van den Wyngaert T, Claeys T, Huizing MT, Vermorken JB, Fossion E (2009) Initial experience with conservative treatment in cancer patients with osteonecrosis of the jaw (ONJ) and predictors of outcome. Ann Oncol 20:331–336
Williamson RA (2010) Surgical management of bisphosphonate induced osteonecrosis of the jaws. Int J Oral Maxillofac Surg 39:251–255
Freiberger JJ, Padilla-Burgos R, Chhoeu AH, Kraft KH, Boneta O, Moon RE et al (2007) Hyperbaric oxygen treatment and bisphosphonate-induced osteonecrosis of the jaw: a case series. J Oral Maxillofac Surg 65:1321–1327
Freiberger JJ (2009) Utility of hyperbaric oxygen in treatment of bisphosphonate-related osteonecrosis of the jaws. J Oral Maxillofac Surg 67:96–106
Vescovi P, Manfredi M, Merigo E, Meleti M, Fornaini C, Rocca JP et al (2010) Surgical approach with Er:YAG laser on osteonecrosis of the jaws (ONJ) in patients under bisphosphonate therapy (BPT). Lasers Med Sci 25:101–113
Ziebart T, Koch F, Klein MO, Guth J, Adler J, Pabst A et al (2011) Geranylgeraniol – a new potential therapeutic approach to bisphosphonate associated osteonecrosis of the jaw. Oral Oncol 47:195–201
Otto S, Pautke C, Opelz C, Westphal I, Drosse I, Schwager J et al (2010) Osteonecrosis of the jaw: effect of bisphosphonate type, local concentration, and acidic milieu on the pathomechanism. J Oral Maxillofac Surg 68:2837–2845
Ziebart T, Yoon CH, Trepels T, Wietelmann A, Braun T, Kiessling F et al (2008) Sustained persistence of transplanted proangiogenic cells contributes to neovascularization and cardiac function after ischemia. Circ Res 103:1327–1334
Crick DC, Andres DA, Waechter CJ (1997) Novel salvage pathway utilizing farnesol and geranylgeraniol for protein isoprenylation. Biochem Biophys Res Commun 237:483–487
Walker K, Olson MF (2005) Targeting Ras and Rho GTPases as opportunities for cancer therapeutics. Curr Opin Genet Dev 15:62–68
Oades GM, Senaratne SG, Clarke IA, Kirby RS, Colston KW (2003) Nitrogen containing bisphosphonates induce apoptosis and inhibit the mevalonate pathway, impairing Ras membrane localization in prostate cancer cells. J Urol 170:246–252
Iguchi K, Nakano T, Usui S, Hirano K (2006) Incadronate inhibits aminopeptidase N expression in prostatic PC-3 cells. Cancer Lett 237:223–233
Urbich C, Heeschen C, Aicher A, Sasaki K, Bruhl T, Farhadi MR et al (2005) Cathepsin L is required for endothelial progenitor cell-induced neovascularization. Nat Med 11:206–213
Asahara T, Murohara T, Sullivan A, Silver M, van der Zee R, Li T et al (1997) Isolation of putative progenitor endothelial cells for angiogenesis. Science 275:964–967
Asahara T, Masuda H, Takahashi T, Kalka C, Pastore C, Silver M et al (1999) Bone marrow origin of endothelial progenitor cells responsible for postnatal vasculogenesis in physiological and pathological neovascularization. Circ Res 85:221–228
Aicher A, Kollet O, Heeschen C, Liebner S, Urbich C, Ihling C et al (2008) Wnt antagonist Dickkopf-1 mobilizes vasculogenetic progenitor cells via activation of the bone marrow endosteal stem cell niche. Circ Res 103:796–803
Shipman CM, Croucher PI, Russell RGG, Helfrich MH, Rogers MJ (1998) The bisphosphonate incardinate (YM175) causes apoptosis of human myeloma cells in vitro by inhibiting the mevalonate pathway. Cancer Res 58:5294–5297
Coxon JP, Oades GM, Kirby RS, Colston KW (2004) Zoledronic acid induces apoptosis and inhibits adhesion to mineralized matrix in prostate cancer cells via inhibition of protein prenylation. BJU Int 94:164–170
Virtanen SS, Vaananen HK, Harkonen PL, Lakkakorpi PT (2002) Alendronate inhibits invasion of PC-3 prostate cancer cells by affecting the mevalonate pathway. Cancer Res 62:2708–2714
Hagelauer N, Ziebart T, Pabst AM, Walter C (2014) Bisphosphonates inhibit cell functions of HUVECs, fibroblasts and osteogenic cells via inhibition of protein geranylgeranylation. Clin Oral Investig [Epub ahead of print]
Conflict of interest
The authors declare that there is no conflict of interest. Christian Walter has received speaker fees from Roche and Riemser and funding from Novartis for a different study.
Role of funding source
None
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pabst, A.M., Krüger, M., Ziebart, T. et al. Isoprenoid geranylgeraniol: the influence on cell characteristics of endothelial progenitor cells after bisphosphonate therapy in vitro. Clin Oral Invest 19, 1625–1633 (2015). https://doi.org/10.1007/s00784-014-1394-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1394-z