Abstract
Objectives
The aim of this multi-center, randomized controlled trial was to assess the impact of missing posterior support on the risk for temporomandibular disorder (TMD) pain by comparing patients with either shortened dental arches (SDA) or molar replacement by removable dental prostheses (RDP).
Methods
A sample of 215 patients with bilateral molar loss in at least one jaw was consecutively recruited in 14 prosthodontic departments of dental schools in Germany. Of the initial sample, 152 patients (mean age: 59.7 years; 53.9 % female) received randomly allocated interventions (SDA: n = 71; RDP: n = 81). Presence of TMD pain was assessed using patients’ self-reports and was verified by physical examination and by pain intensity, as the mean of current pain, worst pain, and average pain in the last 6 months, with 10-point ordinal rating scales. Assessments were performed before treatment and at follow-ups until 60 months after treatment. Impact of interventions on TMD risk and pain intensity was computed by applying logistic and linear random-intercept models.
Results
Tooth replacement (RDP) did not significantly change the risk for self-reported (odds ratio [OR]: 1.1; confidence interval [CI]: 0.4 to 3.4) or clinically verified (OR: 0.7; CI: 0.1 to 4.3) TMD pain compared to no tooth replacement (SDA). Mean characteristic pain intensity was virtually identical in both groups (Coeff: 0.01; CI: −0.30 to 0.32).
Conclusion
Retaining or preservation of an SDA is not a major risk factor for TMD pain over the course of 5 years when compared to molar replacement with RPDs.
Clinical relevance
Seemingly, missing molars do not have to be replaced in order to prevent TMD pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Temporomandibular disorders (TMD), which comprises a heterogeneous group of conditions affecting the temporomandibular joint (TMJ), the masticatory muscles, and/or surrounding tissues [1], are the second most commonly occurring musculoskeletal disorder (after chronic low back pain) [2]. With a prevalence of about 10 % and an incidence of about 3 % in the general population, it presents a relevant public-health problem [3]. Cardinal features of TMD are pain and dysfunction [4], with pain intensity playing a major role in the decision of patients to seek care for their complaints [5]. TMD has a substantial impact in the affected individuals by significantly impairing their quality of life [6–8]. Current knowledge regarding the etiology of TMD suggests that TMD is of multifactorial origin, involving structural/anatomic, neuro-muscular, psychosocial, and genetic factors [9, 10]. Among them, occlusal variations are still controversially discussed as potential TMD risk factors [11–15].
In 1934, when Costen first published a syndrome of several symptoms comprising pain in the temples and tenderness of the TMJs that is currently referred to as TMD, he considered a reduced vertical dimension of occlusion due to loss of posterior teeth as the causative factor [16]. Since then, several studies have been performed to investigate whether missing posterior teeth, a situation named shortened dental arch (SDA) [17], are related to TMD. However, results are contradictory. While several studies reported an association between SDA and signs and symptoms of TMD [13, 18–22], others reported contrary results [23–25]. Among dentists, 50 % consider risk for development of TMD as an indication for treatment of unilateral SDA [26]. Although the number of studies that focus on the relationship between SDA and TMD is large, high-level evidence is still lacking. Many studies were conducted using either a case-control or a cross-sectional design, none were prospective or randomized, and hence, drawing inference regarding cause–effect relationship is difficult.
The identification of missing posterior support due to SDA as a risk factor for TMD is not only important from epidemiological aspects for the etiology of TMD, it also has practical relevance for diagnostics and treatment. SDA has different treatment options and, therefore, would represent a modifiable risk factor. Treatments of SDA comprise the replacement of missing teeth by removable dental prostheses (RDP), cantilever or implant-supported fixed dental prostheses (FDP), or the preservation/restoration of the premolar occlusion. The randomized shortened dental arch study (RaSDA) aimed to provide information on a variety of outcomes for two treatment options in patients with missing posterior teeth, retaining or preservation of an SDA and replacement of missing posterior teeth by RDPs, with tooth loss as the primary outcome [27, 28]. The aim of this analysis was to assess the impact of missing posterior support on the risk for TMD pain.
Methods
Subjects, study design and setting
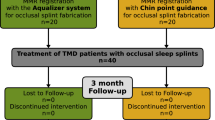
In this multi-center, randomized controlled trial (RCT), a sample of 215 patients, meeting the inclusion and exclusion criteria, was consecutively recruited in 14 prosthodontic departments of dental schools in Germany, between January 2001 and February 2004. For inclusion in the study, patients had to request prosthodontic treatment and have all molars missing in one jaw, with at least both canines and one premolar present on each side of the jaw. Patients with acute signs or symptoms of TMD or a Grade 2 or higher of the Anamnestic Helkimo Index [29] were excluded. A total of 152 patients received allocated interventions and were analyzed. Data were collected before treatment and at follow-ups after treatment (4–8 weeks, 6 months, 12 months, 24 months, 36 months, 48 months, and 60 months). For more details regarding study design, inclusion and exclusion criteria, randomized allocation of interventions, and flow of participants, see Luthardt et al. [27] and Walter et al. [30].
Sample size calculation was based on the primary outcome of the study, tooth loss [28]. This resulted in a required sample size of 70 patients per group. Results of the primary outcome were published elsewhere [28]. In this paper, the results of the secondary outcome, TMD pain, are reported.
This research was conducted in accordance with accepted ethical standards for research practice, undergoing review and approval by the Institutional Review Board at the TU Dresden, Germany (EK 260399). The study has been registered at controlled-trials.com under ISRCTN68590603 (pilot study) and ISRCTN97265367 (main study). Written informed consent was obtained from all participants prior to their enrollment.
Interventions
Patients were randomly allocated either to the SDA group or to the RDP group. SDA was considered the intervention and RDP the control.
In the SDA group, molars were not replaced [31, 32]. If the SDA was complete up to the second premolar, no dental treatment was performed in the posterior region. In cases with missing second premolars, cantilever FDP were incorporated to replace the missing tooth.
In the RDP groups, molars were replaced. Tooth replacement was carried out by means of RDPs retained with precision attachments (Mini SG No. 055 675, CMSA, Biel, Switzerland), connected to either splinted crowns or FDP abutments on the posterior-most teeth on both sides. If the second premolar was missing, it was replaced by the RDPs as well.
Any missing tooth up to the second premolar was replaced by conventional tooth-supported FDP in both groups. All patients received appropriate dental pretreatment, including oral hygiene instructions, periodontal treatments, and endodontic treatment, if necessary, to ensure adequate conditions prior to the final prosthodontic treatment phase. In cases with missing teeth in the opposite jaw, teeth were replaced up to the second premolar in the SDA group, and up to the first molar in the RDP group, to ensure adequate occlusion and posterior tooth support. All dental procedures were performed standardized in all participating study centers.
Outcome
This paper focused on the secondary outcome of the study, TMD pain, assessed using components of a German translation of the Research Diagnostic Criteria for TMD (RDC/TMD) [33]. The RDC/TMD is a well-established and internationally accepted instrument for the assessment of TMD that applies a dual approach. Axis I involves a standardized protocol for the assessment of physical symptoms of TMD, while Axis II assesses psychosocial aspects of TMD, including pain intensity and pain-related impairment using the Graded Chronic Pain Scale (GCPS) [34], depression using the SCL-90-R Depression and Vegetative Symptom Scale [35], nonspecific physical symptoms using the SCL-90-R Somatization Scale [35], and limitations related to mandibular functioning using a Jaw Disability Checklist [33]. Population-based normative data are available for both SCL-90-R scales, which allow the classification of depression and nonspecific physical symptoms as “normal,” “moderate” (above 70th percentile on population norms), and “severe” (above 90th percentile on population norms), a categorization recommended by the original English-language RDC/TMD [33].
This study did not focus on TMD diagnoses, but on the prevalence and intensity of TMD pain, hence the complete RDC/TMD Axis I was not applied. The major outcome for this analysis was the patient’s report of pain using the RDC/TMD pain question: “Have you had pain in the face, jaw, temple, in front of the ear or in the ear in the past month?” This anamnestic self-report was verified by clinical signs of pain in the physical examination consisting of bilateral palpation of the masticatory muscles (Temporalis and Masseter) and the lateral pole of the TMJ, and pain in the TMJ during jaw movements (mouth opening or closing) in both sides, which were adapted from the examination procedures of the RDC/TMD Axis I [33]. TMD pain was considered clinically verified when at least one sign of pain occurred in any of the examined regions on either side. Additionally, characteristic pain intensity was assessed using the mean of the pain intensity items of the GCPS (current pain, worst pain, average pain in the last 6 months). Possible scores of characteristic pain intensity could range from 0 (no pain) to 10 (pain as bad as could be). Patients who reported no pain in the above-mentioned RDC/TMD pain question did not complete the GCPS, hence the corresponding value for characteristic pain intensity was set to 0.
Data analyses
The analytic approach to investigate if SDA is a risk factor for TMD pain involved several steps. First, patient histories of both groups (SDA and RDP) were compared with respect to socio-demographic characteristics, behavior, and physical health, to ensure that potential confounders were equally distributed between both groups. Student’s t-test were applied for continuous data (age), Wilcoxon rank-sum test (Mann Whitney U-test) for ordinal data (level of education) and chi-squared test for categorical data (e.g., gender, martial status, professional activities) to test for statistically significant group differences.
Second, the impact of SDA on risk for TMD pain was computed by applying multilevel modeling [36]. Logistic random-intercept models, with intervention group as the predictor variable, and prevalence of self-reported TMD pain at each follow-up as the criterion variable, were developed using the subject as the grouping variable to account for inter-correlation of the scores within a subject. This analysis was adjusted for gender, since gender is known to be a major risk factor for TMD pain [37], by including this variable as covariate in a multivariate model. Furthermore, the prevalence of oral parafunctions was included as a covariate in the model. Self-report of clenching or grinding during daytime was considered as an indicator for awake bruxism, and nocturnal clenching or grinding as an indicator for sleep bruxism [38]. This was supplemented by analyses using the additional outcomes, clinically verified TMD pain and characteristic pain intensity as criterion variables in logistic and linear random-intercept models, respectively. Multilevel models resulted in odds ratios (OR) with 95 % confidence intervals (CI) for self-reported and clinically verified TMD pain, and regression coefficients (including CI) for characteristic pain intensity. An OR of 2 or above was considered clinically relevant.
Finally, analyses were performed for each follow-up period separately to investigate whether the relationship between intervention group and TMD pain changed within the 5 years of follow-up. Logistic regression analyses were applied for self-reported and clinically verified TMD pain, linear regression analyses were applied for characteristic pain intensity, and analyses were controlled for gender, sleep bruxism, and awake bruxism as covariates. Effect sizes were calculated for the group comparison of characteristic pain intensity to determine clinical relevance of differences. According to Cohen [39], an effect size above 0.2 indicates a small effect, above 0.5 indicates a medium effect, and above 0.8 indicates a large effect. We considered an effect size of 0.5 as the threshold for clinical relevance as has been previously defined for self-reported health measures [40].
A total of 150 of the 152 participants (97 %) had data for TMD pain for at least one follow-up and were included in the analyses. Number of participants at follow-ups ranged from 150 (4–8 weeks) to 128 (48 months, Table 2) with a total of 20 participants lost to follow-up after 60 months (SDA: n = 10, RDP: n = 10). Reasons for loss to follow-up did not differ substantially between groups. For details, see Walter et al. [28]. Participants did not leave the study when the primary outcome tooth loss occurred (SDA: n = 17, RDP: n = 22, Cox regression: P > 0.05) [28]. Tooth loss and loss to follow-up were not considered to be related to the risk of TMD pain, and, therefore, this information was not included in the analyses.
All analyses were performed as intention-to-treat analyses using the statistical software package STATA (Stata Statistical Software: Release 12; StataCorp LP, College Station, TX, USA), with the probability of a type I error set at the 0.05 level.
Results
Characteristics of participants
At baseline, mean age of the participants was 59.7 years and about half of the participants were female (53.9 %) with no significant differences between intervention groups (Table 1). About two-thirds (70.8 %) were married and lived with their spouse. Participants in the SDA group were more often divorced (18.5 % vs. 2.5 %) and less often lived with their spouse (63.1 % vs. 77.2 %) than those in the RDP group (Fisher’s exact test: P = 0.027). No significant group differences occurred for level of education, professional activities, or alcohol and tobacco use.
Oral parafunctions (clenching or grinding) were reported between 19.3 % (diurnal, awake bruxism) and 26.4 % (nocturnal, sleep bruxism). However, morning jaw stiffness was experienced in only 6.3 % of the participants. Jaw clicking or popping, as well as grating or grinding noises of the jaw, was reported by about an eighth (13.6 % and 13.1 %). About a quarter of the participants (22.5 %) indicated having arthritis or rheumatism, while only 8.0 % of the participants stated having osteoporosis. There were no significant group differences in oral parafunctions or physical health conditions.
Participants’ mandibular functions were only slightly impaired at baseline with on average one out of 12 affected activities and no significant difference between groups. The amount of both depression and nonspecific physical symptoms was classified as “normal” for the majority of the participants (66.7 % and 57.6 %, respectively). There were no significant differences between groups with respect to both psychosocial measures.
Prevalence of TMD pain
Prevalence of self-reported TMD at follow-ups ranged from 11.7 % (48 months) to 18.1 % (24 months, Table 2). More than a third (36.2 %) of the participants reported having TMD pain on at least one follow-up. TMD pain was clinically verified in 3.3 % (48 months) to 5.4 % (36 months) of the participants, with a prevalence of 12 % of clinically verified TMD pain at any follow-up. Characteristic pain intensity ranged from 0 to 10 with means between 0.33 (48 months) and 0.43 (4–8 weeks). The overall mean pain intensity for the complete study period was 0.39 (Table 2).
Risk of TMD pain
Tooth replacement (RDP group) did not change the risk for self-reported TMD pain significantly compared to no tooth replacement (SDA group). The OR was close to 1 with 0.9 in the unadjusted and 1.1 in the adjusted analyses, indicating no effect (Table 3). However, the CI was wide (0.3–2.9 and 0.4–3.4, respectively). Although tooth replacement (RDP group) slightly decreased the risk for clinically verified TMD pain compared to no tooth replacement (SDA group; both OR: 0.7), the effect was not statistically significant in either model. Mean characteristic pain intensity was virtually identical in both groups (coefficients: −0.02 and 0.01, respectively).
When analyzing the effect of tooth replacement on TMD pain at each follow-up separately, only one of the regression analyses revealed a statistically significant effect (Table 4). OR for the effect of tooth replacement (RDP group) on self-reported TMD pain were all around 1, indicating no effect. While at 6 months after treatment the prevalence of self-reported TMD pain was higher in the RDP group (20.5 % vs. 14.9 %), at 36 months, prevalence was higher in the SDA group (21.3 % vs. 13.9 %). Results were similar for clinically verified TMD pain (Table 4). Differences in mean characteristic pain intensity between SDA and RDP group were close to 0, expect for the 6- and 60-month follow-up with small effect sizes. While pain intensity at 6 months was higher in the RDP group (0.48 vs. 0.21), results were contrary at 60 months with higher values in the SDA group (0.62 vs. 0.21), with a statistically significant difference in the adjusted analysis. However, the absolute value of the difference was still low. All three analyzed outcomes indicated no effect by the time between treatment and follow-up on risk for TMD pain.
Discussion
This RCT assessed the impact of missing posterior support on the risk for TMD by comparing patients with either SDA or molar replacement by RDP. The study’s findings provide no evidence that replacement of missing posterior teeth with RDPs decreases the risk for TMD pain in patients with SDA.
SDA and TMD pain
Only one of the analyses revealed a statistically significant difference in risk for TMD pain between the intervention and the control group. Furthermore, the OR for the analyses, including the data of all follow-ups, were close to 1, indicating no effect, and not reaching the threshold for clinical relevance. The effect on characteristic pain intensity was virtually zero with only one statistically significant difference between both groups of a small extent. However, CIs were wide, and thus, prevented from the definite exclusion of an effect of the intervention on the study outcome compared to the control. Even though equality of the intervention and the control could not be clearly proven, a difference in the impact on TMD pain is quite unlikely. This is supported by the separate analyses for each follow-up. We found a consistent pattern in all three outcome measures, neither favoring the SDA or the RDP group. Therefore, the retention or preservation of an SDA is most likely not a significant risk factor for TMD pain.
The comparison of the study’s findings with the literature reveals contradictory results. Some studies found no association between SDA and TMD [23–25], but others reported an association [13, 18–22]. However, none of the studies was randomized or even prospective. Studies that found an association were case-control [13, 18, 22] or cross-sectional studies [19–21], and, therefore, could not provide evidence regarding cause–effect relationship. Other methodological differences might also explain differences in study findings. While the case-control and cross-sectional studies compared the number of existing posterior teeth and, therefore, if the loss of posterior teeth is associated with TMD, this is not possible in an RCT. Tooth loss cannot be randomly assigned to the patients by ethical reasons. We assessed whether replacement or non-replacement of the missing posterior teeth affects the risk for TMD pain. From a clinical point of view, the effect of tooth replacement is much more relevant than the effect of tooth loss. Teeth will be removed mainly based on their survival probability, initiated by complaints of the patients. The decisions for extractions will mainly be driven because of periodontal or carious destructions of the teeth, and, therefore, a possible prevention of TMD by keeping the molars plays certainly only a negligible role. However, when it comes to the decision whether or not the tooth should be replaced, the issue of prevention of TMD becomes particularly important [26]. Based on our study design, the findings regarding the risk of TMD pain can be generalized to patients with already existing SDA, but not to the new occurrence of SDA.
Methodological aspects of the study
The study has some strengths and limitations. At the time of study initiation, the validated German version of the RDC/TMD [41] was not available yet. Therefore, a German translation of the original English version [33] had to be prepared, applying a forward–back approach involving both German and English native speakers. The original and the retranslated English versions were compared, and the German version was adapted until both English versions were congruent. Therefore, the accuracy of the translation process had been confirmed. Even though validity and reliability of the translated version have not been assessed, this seems not to be a major drawback. The translated version was not substantially different from the later published validated version, supporting the use of the initial translation in this study.
The major outcome for this analysis was TMD pain. Pain-free signs or symptoms of TMD such as joint noises were not considered as important outcomes. They result in low impairments in everyday life and are in general considered as conditions without treatment need. Pain intensity plays a major role for quality of life impairment [8] and the decision of patients to seek care for their complaints [5]; pain-associated TMD diagnoses (e.g., myofascial pain) have the highest impact on quality of life whereas patients with disc displacement only showed lowest impairment [7]. TMD pain was defined as a secondary outcome in the main study, as well as oral health-related quality of life with results reported elsewhere [42]. These measures were selected to assess patients’ perceptions of treatment results and, therefore, represent patient-reported outcomes. Accordingly, TMD pain was assessed through the patients’ self-reports, using a single question contained in the RDC/TMD [33]. A single question regarding orofacial pain has already been used as an effective diagnostic test for pain-associated TMD diagnoses with a sensitivity of 96 % and a specificity of 95 % [43]. This was complemented by not only including the presence of TMD pain in our analyses, but also including the responses from the pain intensity items of the GCPS [34]. Patients’ self-reports were verified by evidence of pain symptoms in the masticatory muscles or the TMJ in the clinical examination. As expected, prevalence of clinically verified TMD pain was lower than that of self-reported pain. The data of the TMD examination did not allow for allocation of TMD diagnoses according to the RDC since the examination protocol had to be somewhat shortened to ensure feasibility of the study (e.g., no distinction between the three parts of the temporal muscle and no intraoral palpations). Therefore, clinically verified TMD pain does not represent the presence of a pain-associated TMD diagnosis according to the RDC/TMD [33], limiting the comparability to findings of other studies. However, this is not considered a major drawback since this study did not focus on TMD diagnoses, but on the patients’ perceptions of TMD pain, which were appropriately ascertained.
Several factors that were not included in the presented analyses can potentially affect pain perception such as medication intake or anxiety. Since the presence of psychiatric disorders was an exclusion criterion [27], the proportion of patients taking psychotropic drugs should have been negligible. Even though pain medication probably decreases the level of pain, we are convinced that the patients would still perceive some pain (of lower intensity) and would consequently report the pain in the clinical examination. Accordingly, only characteristic pain intensity would be affected, but the effect on anamnestic or clinically verified pain was expected to be low, not having an impact on the study findings. Anxiety is known to be strongly related to depression [44]. Given the finding of almost identical levels of depression and vegetative symptoms at baseline in both study groups, substantial differences in the levels of anxiety are not very likely. Furthermore, pain prevalence was low in both groups and pain intensity was almost negligible in our study, making substantial impact of different anxiety levels or medication intake on study findings unexpected.
Patients were consecutively recruited in 14 prosthodontic departments of dental schools in Germany. Although these departments represent centers of primary, secondary, and tertiary prosthodontic care, most participants were either long-term patients or sought initial treatment for their situation in these departments. Study participants can therefore be considered a representative sample of typical prosthodontic patients with SDA. Most of the participants required appropriate dental pre-treatment prior to the final prosthodontic treatment to ensure absence of caries and adequate periodontal conditions [27]. Nevertheless, the necessary strict inclusion and exclusion criteria of an RCT limit the generalizability of our study results. Due to the recruitment in several centers across Germany, the impact of regional differences regarding possible socio-economic or psychosocial confounders on study outcomes could be delimited. However, only 152 patients of the initial sample of 215 patients received the allocated treatment and were included in the study. A total of 63 were excluded after randomization, mostly due to refusal of the randomization result and preference of an alternative restoration (n = 24), or high costs and non-approval by health insurance (n = 10) [30]. The number of participants who withdrew for particular reasons before treatment was comparable between both groups, and should not have influenced the study’s findings.
Sample size calculation was based on the primary outcome of the study, tooth loss [28], and not TMD pain. This may have resulted in insufficient statistical power of the presented analysis to detect meaningful effects of the interventions on TMD pain. However, even though more participants would have increased statistical power and probably increased precision of the estimates by decreasing the width of the CI, we observed no clinically relevant effect and the pattern of the observed differences between both groups supported the conclusion of a lack of significant effect. Therefore, we do not think that low statistical power would be an important limitation of our study or would affect our study findings.
Teeth were replaced in the control group by RDP; no implants were provided. However, the rigid connection of the RDP to the teeth due to precious attachments and the regular maintenance (e.g., relining) of the RDP should have ensured sufficient posterior support in the RDP group during the complete course of the study [45]. While the impact of RDP on quality of life is lower than in cases with replacement by implant-supported FDP or preservation of SDA [46], the impact of implant-supported FDP compared to RDP on TMD signs and symptoms is less clear. Therefore, the study’s findings cannot be generalized to the replacement of missing molars with implant-supported FDP.
Clinical implications
The study’s findings do not necessarily imply that missing molars should not be replaced, they just deny the belief that risk for development of TMD is an indication for treatment of SDA, which is quite common among dentists [26]. Other reasons for tooth replacement might be present in the individual case, e.g., risk of supraeruption of antagonist unopposed teeth [47] or impaired quality of life [48]. In patients with SDA, chewing complaints are a significant predictor of prosthodontic treatment for replacing missing teeth [49, 50]. However, when in patients with SDA quality of life is not impaired and risk or impact of tooth supraeruption is negligible, seemingly, missing molars do not have to be replaced.
Conclusion
With the limitations of this study it can be concluded that retention or preservation of SDA is not a major risk factor for TMD pain over the course of 5 years when compared to molar replacement with RPDs.
References
Okeson JP (1996) Orofacial pain: guidelines for assessment, diagnosis, and management. Quintessence, Carol Stream
NIDCR — National Institut of Dental and Craniofacial Research. Facial Pain. 2010 [updated 2010; cited 2010]; Available from: http://www.nidcr.nih.gov/DataStatistics/FindDataByTopic/FacialPain/
LeResche L (1997) Epidemiology of temporomandibular disorders: implications for the investigation of etiologic factors. Crit Rev Oral Biol Med 8:291–305
Suvinen TI, Reade PC, Kemppainen P, Kononen M, Dworkin SF (2005) Review of aetiological concepts of temporomandibular pain disorders: towards a biopsychosocial model for integration of physical disorder factors with psychological and psychosocial illness impact factors. Eur J Pain 9:613–633
Rollman A, Visscher CM, Gorter RC, Naeije M (2012) Care seeking for orofacial pain. J Orofac Pain 26:206–214
Reisine ST, Fertig J, Weber J, Leder S (1989) Impact of dental conditions on patients' quality of life. Community Dent Oral Epidemiol 17:7–10
Reissmann DR, John MT, Schierz O, Wassell RW (2007) Functional and psychosocial impact related to specific temporomandibular disorder diagnoses. J Dent 35:643–650
Zheng J, Wong MC, Lam CL (2011) Key factors associated with oral health-related quality of life (OHRQOL) in Hong Kong Chinese adults with orofacial pain. J Dent 39:564–571
Rollman GB, Gillespie JM (2000) The role of psychosocial factors in temporomandibular disorders. Curr Rev Pain 4:71–81
Smith SB, Maixner DW, Greenspan JD et al (2011) Potential genetic risk factors for chronic TMD: genetic associations from the OPPERA case control study. J Pain 12:T92–101
Becker IM (1995) Occlusion as a causative factor in TMD. Scientific basis to occlusal therapy. N Y State Dent J 61:54–57
Greene CS (2001) The etiology of temporomandibular disorders: implications for treatment. J Orofac Pain 15:93–116
Pullinger AG, Seligman DA, Gornbein JA (1993) A multiple logistic regression analysis of the risk and relative odds of temporomandibular disorders as a function of common occlusal features. J Dent Res 72:968–979
Cooper BC, International College of Cranio-Mandibular Orthopedics (2011) Temporomandibular disorders: A position paper of the International College of Cranio-Mandibular Orthopedics (ICCMO). Cranio 29:237–244
Türp JC, Schindler H (2012) The dental occlusion as a suspected cause for TMDs: epidemiological and etiological considerations. J Oral Rehabil 39:502–512
Costen JB (1934) A syndrome of ear and sinus symptoms dependent upon disturbed function of the temporomandibular joint. Ann Otol Rhinol Laryngol 43:1–15
Käyser AF (1981) Shortened dental arches and oral function. J Oral Rehabil 8:457–462
Tallents RH, Macher DJ, Kyrkanides S, Katzberg RW, Moss ME (2002) Prevalence of missing posterior teeth and intraarticular temporomandibular disorders. J Prosthet Dent 87:45–50
Schmitter M, Balke Z, Hassel A, Ohlmann B, Rammelsberg P (2007) The prevalence of myofascial pain and its association with occlusal factors in a threshold country non-patient population. Clin Oral Investig 11:277–281
Mundt T, Mack F, Schwahn C et al (2005) Gender differences in associations between occlusal support and signs of temporomandibular disorders: results of the population-based Study of Health in Pomerania (SHIP). Int J Prosthodont 18:232–239
Dulcic N, Panduric J, Kraljevic S, Badel T, Celic R (2003) Incidence of temporomandibular disorders at tooth loss in the supporting zones. Coll Antropol 27(Suppl 2):61–67
Wang MQ, Xue F, He JJ, Chen JH, Chen CS, Raustia A (2009) Missing posterior teeth and risk of temporomandibular disorders. J Dent Res 88:942–945
Takayama Y, Miura E, Yuasa M, Kobayashi K, Hosoi T (2008) Comparison of occlusal condition and prevalence of bone change in the condyle of patients with and without temporomandibular disorders. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:104–112
Gesch D, Bernhardt O, Kirbschus A (2004) Association of malocclusion and functional occlusion with temporomandibular disorders (TMD) in adults: a systematic review of population-based studies. Quintessence Int 35:211–221
De Boever JA, Carlsson GE, Klineberg IJ (2000) Need for occlusal therapy and prosthodontic treatment in the management of temporomandibular disorders: Part II. Tooth loss and prosthodontic treatment. J Oral Rehabil 27:647–659
Lyka I, Carlsson GE, Wedel A, Kiliaridis S (2001) Dentists' perception of risks for molars without antagonists. A questionnaire study of dentists in Sweden. Swed Dent J 25:67–73
Luthardt RG, Marre B, Heinecke A et al (2010) The Randomized Shortened Dental Arch study (RaSDA): design and protocol. Trials 11:15
Walter MH, Hannak W, Kern M et al (2013) The randomized shortened dental arch study: tooth loss over five years. Clin Oral Investig 17:877–886
Helkimo M (1974) Studies on function and dysfunction of the masticatory system: II. Index for anamnestic and clinical dysfunction and occlusal state. Swed Dent J 67:101–119
Walter MH, Weber A, Marre B et al (2010) The Randomized Shortened Dental Arch Study: Tooth Loss. J Dent Res 89:818–822
Witter DJ, van Palenstein Helderman WH, Creugers NH, Kayser AF (1999) The shortened dental arch concept and its implications for oral health care. Community Dent Oral Epidemiol 27:249–258
Kanno T, Carlsson GE (2006) A review of the shortened dental arch concept focusing on the work by the Kayser/Nijmegen group. J Oral Rehabil 33:850–862
Dworkin SF, LeResche L (1992) Research diagnostic criteria for temporomandibular disorders: review, criteria, examinations and specifications, critique. J Craniomandib Disord 6:301–355
Von Korff M, Ormel J, Keefe FJ, Dworkin SF (1992) Grading the severity of chronic pain. Pain 50:133–149
Derogatis LR (1999) SCL-90-R: Administration, scoring and procedures manual-II for the revised version. Clinical Psychometric Research, Towson
Rabe-Hesketh S, Skrondal A (2008) Multilevel and longitudinal modeling using Stata. Stata Press, College Station
List T, Dworkin SF (1996) Comparing TMD diagnoses and clinical findings at Swedish and US TMD centers using research diagnostic criteria for temporomandibular disorders. J Orofac Pain 10:240–253
Lobbezoo F, Ahlberg J, Glaros AG et al (2013) Bruxism defined and graded: an international consensus. J Oral Rehabil 40:2–4
Cohen J (1988) Statistical power analysis for the behavioral sciences, 2nd edn. Lawrence Earlbaum Associates, Hillsdale
Norman GR, Sloan JA, Wyrwich KW (2003) Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care 41:582–592
John MT, Hirsch C, Reiber T, Dworkin S (2006) Translating the research diagnostic criteria for temporomandibular disorders into German: evaluation of content and process. J Orofac Pain 20:43–52
Wolfart S, Muller F, Gerss J et al (2013) The randomized shortened dental arch study: oral health-related quality of life. Clin Oral Investig. doi:10.1007/s00784-00013-00991-00786
Reissmann DR, John MT, Schierz O, Hirsch C (2009) An abbreviated version of RDC/TMD. Schmerz 23:618–627
Pandey M, Devi N, Thomas BC, Kumar SV, Krishnan R, Ramdas K (2007) Distress overlaps with anxiety and depression in patients with head and neck cancer. Psychooncology 16:582–586
Wolfart S, Marre B, Wostmann B et al (2012) The randomized shortened dental arch study: 5-year maintenance. J Dent Res 91:65S–71S
Kuboki T, Okamoto S, Suzuki H et al (1999) Quality of life assessment of bone-anchored fixed partial denture patients with unilateral mandibular distal-extension edentulism. J Prosthet Dent 82:182–187
Compagnon D, Woda A (1991) Supraeruption of the unopposed maxillary first molar. J Prosthet Dent 66:29–34
Baba K, Igarashi Y, Nishiyama A et al (2008) Patterns of missing occlusal units and oral health-related quality of life in SDA patients. J Oral Rehabil 35:621–628
Fueki K, Igarashi Y, Maeda Y et al (2011) Factors related to prosthetic restoration in patients with shortened dental arches: a multicentre study. J Oral Rehabil 38:525–532
Montero J, Bravo M, Hernandez LA, Dib A (2009) Effect of arch length on the functional well-being of dentate adults. J Oral Rehabil 36:338–345
Acknowledgements
This study was supported by the German Research Foundation (Deutsche Forschungsgemeinschaft, DFG), grant DFG WA 831/2-1 to 2-6 and grant DFG WO 677/2-1.1 to 2-2.1. We acknowledge the contribution of the following members of the RaSDA-study group: W. Reinhardt, F. Jahn (Department of Prosthetic Dentistry and Dental Material Science, University of Jena), W. Gernet (Department of Prosthetic Dentistry, Ludwig-Maximilians University Munich), E.-J. Richter (Department of Prosthetic Dentistry, Julius-Maximilians University of Würzburg), E. Busche (Department of Prosthetic Dentistry, Witten-Herdecke University) in study design, study implementation and data collection.
Conflict of interest
The authors report no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Reissmann, D.R., Heydecke, G., Schierz, O. et al. The randomized shortened dental arch study: temporomandibular disorder pain. Clin Oral Invest 18, 2159–2169 (2014). https://doi.org/10.1007/s00784-014-1188-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-014-1188-3