Abstract
Objectives
This study aimed to compare posterior tooth root fractures in endodontically treated teeth versus nonendodontically treated teeth in the Chinese population.
Materials and methods
We investigated 500 root fractured posterior teeth in 461 Chinese patients. The clinical information (age, sex of patients, tooth type) were recorded. The fractured teeth were divided into endodontically treated root fractured (ETRF) teeth and nonendodontically treated root fractured (NETRF) teeth. The morphology of the fractured root (circular, oval, other), the orientation of fracture lines (vertical and non-vertical), the restorations performed (crown, filling, non-filling), and the position of the teeth in the dental arch (normal, misaligned) were evaluated based on cone-beam computed tomography images. These data were compared between 2015 and 2019. ETRF% was calculated as ETRF/ETRF + NETRF. Vertical% was calculated as vertical/vertical + non-vertical.
Results
There were 177 ETRF teeth and 323 NETRF teeth in this population. The total ETRF% was 29.3% in 2015 and 37.6% in 2019 (P = 0.087). The proportion of vertical root fracture in the ETRF group increased significantly in 2019 compared with that in 2015 (46.2% vs. 80.2%, P = 0.000). The ETRF% in female patients increased by 16.8%, but increased by only 1.2% in male patients in 2019 compared with that in 2015. The ETRF% of mandibular and maxillary premolars increased by 48.5% and 29.3%, respectively. The proportion of crown restoration increased by 2.4% in 2019 compared with that in 2015 in the ETRF group.
Conclusions
The proportion of NETRF teeth and non-vertical root fractures in posterior teeth is high in this Chinese population. The number of vertical root fractures in endodontically treated teeth increased significantly from 2015 to 2019.
Clinical relevance
More attention should be paid to endodontic treatment factors in the occurrence of root fractures, especially as female patients and premolars are more susceptible.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
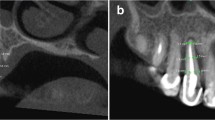
Dental root fractures are fractures that occur in the root of a tooth, with complete or incomplete fractures, extending through the tooth root [1, 2]. X-ray diagnosis is important for diagnosis, because most root fractures have no specific clinical signs and symptoms. Cone-beam computed tomography (CBCT), as a widely used noninvasive imaging technique, can provide three-dimensional visualization and evaluation of root fractures. For displaced root fractures, which have separation of fracture fragments [3], CBCT is regarded as the gold standard for diagnosis.
Root fractures can occur in both anterior teeth and posterior teeth. For anterior teeth, most root fractures are traumatized [4, 5]. However, for posterior teeth, root fractures can occur in vital teeth with intact pulp or in endodontically treated teeth [2]. For nonendodontically treated root fractures, attrited occlusal surfaces [6], damaging chewing habits or the chewing of hard foods [6, 7], excessive and repetitive masticatory force [7, 8], and morphological features (flat roots with smaller mesiodistal diameters) [9] are risk factors. For endodontically treated root fractures (ETRFs), excessive dentin removal and excessive wedging forces are important factors associated with their occurrence [10].
For the Chinese population, because of their particular diet pattern and chewing habits [6, 11], root fractures in nonendodontically treated teeth are common [6, 7, 12]. Moreover, vertical root fractures in nonendodontically treated teeth, which mainly occur in endodontically treated teeth, also comprise a proportion of root fractures in the Chinese population. The incidence of endodontically treated root fractured (ETRF) teeth and nonendodontically treated root fractured (NETRF) teeth and of vertical and non-vertical root fractures in the Chinese population is quite different from that in other populations. Moreover, as more teeth are treated endodontically and the methods of endodontic treatment have developed rapidly in recent years, it is unknown whether this has induced more ETRF teeth. Therefore, in the present study, we retrospectively reviewed displaced root fractured teeth in our hospital in 2015 and 2019, based on our CBCT database. The proportion of root fractures (endodontically treated vs. nonendodontically treated, vertical and non-vertical) was calculated, the clinical characteristics of the patients and their teeth were recorded, and the differences were compared between 2015 and 2019.
Materials and methods
Root fractured teeth inclusion
We carried out a retrospective search of CBCT reports from 21,480 patients who were referred to the Affiliated Stomatology Hospital of Medical School, Nanjing University, China, in 2015 and 2019, who required a CBCT examination as part of their dental treatment. We identified 461 patients whose CBCT images provided a definitive diagnosis of root fractures and enrolled them in this study. The inclusion criteria were as follows: (1) All patients were examined by CBCT and were definitively diagnosed as having root fractures (hypodense (radiolucent) fracture line presented clearly on the CBCT images); (2) posterior teeth present (the tooth type included the first premolar, the second premolar, the first molar, and the second molar); (3) no post insertion; (4) no trauma history; and (5) CBCT images were of good quality, without motion artifacts and foreign body artifacts.
Collection of clinical information and the evaluation of CBCT images
The following clinical information was recorded: age and sex of each patient and the tooth type of each fractured tooth. The fractured teeth were divided into four types: maxillary premolars, maxillary molars, mandibular premolars, and mandibular molars.
On the CBCT images, the orientations of the root fractures were evaluated and classified into vertical and non-vertical types. If the fracture line was parallel to the long axis of the root, the fractured tooth was recorded as vertical; otherwise, the fractured tooth was recorded as non-vertical. The morphology of the root canal of the fractured root was classified as circular, oval, or other (C-shaped, fused, and irregular). The restorations performed in these fractured teeth were classified into crown, filling, and non-filling. The position of the teeth in the dental arch was divided into normal and misaligned. Evaluation of the CBCT images was performed by two oral radiologists, separately. If a consensus could not be reached between the two evaluators, a senior radiologist performed the final classification. Before the evaluation, all three evaluators were trained on the classification criteria.
Statistics
In both 2015 and 2019, the root fractured teeth were divided into endodontically treated root fractured (ETRF) teeth and nonendodontically treated root fractured (NETRF) teeth. The proportion of ETRF teeth among the total root fractures was calculated as total ETRF% = ETRF/(ETRF + NETRF), and the NETRF% was calculated as NETRF% = NETRF/(ETRF + NETRF).
In both 2015 and 2019, for the ETRF and NETRF groups, the proportion of vertical root fracture was calculated as vertical% = vertical/(vertical + non-vertical).
In both 2015 and 2019, for the ETRF and NETRF groups, average age of each group of patients was calculated, and then, the ETRF% and NETRF% were calculated for males and females. Female ETRF% = female ETRF/(female ETRF + female NETRF), and male ETRF% = male ETRF/(male ETRF + male NETRF). Then, the ETRF% and NETRF% were calculated for the four tooth types. For example, maxillary premolar ETRF% = maxillary premolar ETRF/(maxillary premolar ETRF + maxillary premolar NETRF). The calculations were similar for the other three tooth types. The ETRF% and NETRF% were also calculated for the three root shapes. For example, circular-shaped ETRF% = circular-shaped ETRF/(circular-shaped ETRF + circular-shaped NETRF). The calculations were similar for the other two root shapes. For the ETRF and NETRF groups, the proportion of crown restoration was calculated as crown% = crown/(crown + filling + non-filling), and the calculations were similar for the other two restoration types. For the ETRF and NETRF groups, the proportion of misaligned teeth was calculated as misaligned% = misaligned/(normal + misaligned).
SPSS23.0 software (IBM Corp., Armonk, NY, USA) was used for the statistical analysis. For the quantitative data, values were presented as the mean ± standard deviation. The Kolmogorov–Smirnov test was used to inspect the normality and homogeneity of variance of the data. An independent t test was used to compare the differences between 2015 and 2019. For categorical variables, proportion (%) was calculated, and the chi-squared test was used to compare the differences between 2015 and 2019. P < 0.05 was considered statistically significant.
Results
A total of 500 root fractured teeth from 461 Chinese patients were analyzed in this study. The number and proportion of ETRF and NETRF teeth are shown in Table 1. Total ETRF% increased from 29.3% in 2015 to 37.6% in 2019 (Fig. 1); however, the difference was not statistically significant between the two years (P = 0.087).
The distributions of vertical and non-vertical ETRF and NETRF teeth in 2015 and 2019 are shown in Table 2. In the ETRF group, vertical root fractures increased significantly from 46.2 to 80.4% (P = 0.000) between 2015 and 2019 (Fig. 2).
The average ages of ETRF and NETRF patients are shown in Table 3. There were no statistically significant differences between 2015 and 2019 for both ETRF and NETRF patients.
Table 4 shows the ETRF% and NETRF% for male and female patients in 2015 and 2019. The total number of male patients was approximately 2.1-fold higher than the number of female patients (79 vs. 38) in 2015, but was only 1.3-fold higher (193 vs. 151) in 2019. From 2015 to 2019, the male ETRF% increased by 1.2% (P = 0.843), while the female ETRF% increased by 16.8% (P = 0.062) (Fig. 3).
Four tooth types of ETRF% and NETRF% in 2015 and 2019 are shown in Table 5. The proportion of root fracture was found to be highest in mandibular molars in both ETRF and NETRF groups. From 2015 to 2019, the ETRF% of mandibular premolars increased the most (from 33.3 to 81.8%), followed by maxillary premolars; however, the ETRF%s of maxillary molars and mandibular molars were almost the same (Fig. 4).
Table 6 shows the ETRF% and NETRF% of three root morphologies in 2015 and 2019. Oval roots were more susceptible to root fractures. The ETRF% for both circular and oval root increased in 2019 compared with that in 2015; however, the difference was not significant.
The distribution of different dental restoration methods in the ETRF and NETRF groups in 2015 and 2019 is shown in Table 7. In the ETRF group, the proportion of crown restoration was 23.1% and 21.7%, respectively.
The position of the teeth in the dental arch was divided into normal and misaligned groups. In the ETRF group, two teeth were misaligned in 2015 (2/39) and four in 2019 (4/138). In the NETRF group, four teeth were misaligned in 2015 (4/94) and 20 in 2019 (20/229).
Discussion
Dental root fractures occur at the root of the tooth [13]. The site of fracture is hidden; therefore, it cannot be directly observed by clinical examination. CBCT diagnosis of root fracture is based on the presence of a hypodense (radiolucent) fracture line on the CBCT image. Displaced root fractures, which have displacement of root segments, can be demonstrated clearly on CBCT images and can be definitively diagnosed using CBCT. Moreover, the position and the orientation of root fractures and the shape of the fractured root can be evaluated on CBCT images. In this study, a retrospective cross-sectional investigation of root fractures in posterior teeth was performed based on our CBCT database.
We observed that the proportions of NETRF teeth and vertical root fractures (VRFs) were much higher than in a previous study [6], probably because of different sample sizes, different data sources, and different populations. VRFs occur more often in teeth that have undergone complex restorative procedures, i.e., root canal treatment and intraradicular post-retention [1, 6, 12]. Mizuhashi et al.’s [4] study reported that only 9 of 51 fractured teeth (17.6%) were vital teeth, and 8 of them were traumatized anterior teeth. For the Chinese population, NETRF teeth were reported to account for a certain proportion of root fractures. In our study, of 500 root fractured teeth, 323 were NETRF teeth (64.6%); of the 282 vertical root fractured teeth, 153 were NETRF teeth (54.3%). Liao et al. [10] reported that 13.8% of 65 VRF teeth were nonendodontically treated; Chan et al. [6] showed that 40% of 315 VRF teeth were nonendodontically treated. NETRF teeth are reported to occur mainly in the Chinese population [11]. This might be related to damaging chewing habits (chewing of hard foods, such as meat bones, sugar canes, and betel nuts), which are common in the Chinese population [7, 11]. In addition, it was reported that the distinctive chewing habits of the Chinese population will produce heavy, repeated, and prolonged stress and might initiate a large number of non-vertical root fractures [2, 14].
In the present study, all the CBCT images in our hospital in 2015 and 2019 were screened retrospectively, and many root fractured teeth were diagnosed as non-chief complaint teeth; thus, the proportion of NETRF teeth among total root fractures and in VRFs was high. This also suggested that the incidence of NETRF teeth in the Chinese population is higher than previously assumed.
In this study, the total ETRF% increased from 29.3% in 2015 to 37.6% in 2019; the proportion of VRFs in all root fractures increased from 42.1 to 61.6%; for ETRF teeth, the proportion of VRF teeth increased from 46.2 to 80.2%. We consider that the bite force and dietary factors related to the occurrence of root fractures would not have changed in such a short time [15]. However, more patients have their teeth endodontically treated, and endodontic treatment techniques have developed rapidly [16]. Therefore, the ETRF% increased, and VRFs among ETRF teeth increased significantly. This also suggested endodontically treated root fractures are more likely to be vertical.
In our study, nonendodontically treated root fractures were more frequent in male patients than in females (by about 1.7-fold). This was consistent with previous studies. In two studies by Chan et al., males had 2.2 times [7] and 3.6 times [6] more nonendodontically treated VRFs than females. Liao et al. [10] reported that among nine patients with nonendodontically treated VRFs, eight were male, and only one was female. Males have more nonendodontically treated root fractures, which might be related to factors such as stronger masticatory force and habitual chewing of hard foods [17]. However, for endodontically treated VRFs, the results for the sex distribution of Chan et al.’s and Liao et al.’s studies were opposite. Liao et al. [10] reported that 67.35% of endodontically treated VRFs occurred in females and 32.65% occurred in males, whereas Chan et al. [6] reported that 42% occurred in females and 58% occurred in males. In this study, males had more endodontically treated root fractures in 2015 (male:female = 24:11), but slightly fewer in 2019 (male:female = 61:69). Notably, the female ETRF% increased by 16.8% and male ETRF% increased by only 1.2% in 2019 compared with that in 2015. A change in the tooth structure is the main reason for endodontically treated root fractures [10]. Therefore, based on our data, we believe that endodontic treatment has a higher impact on female patients.
In this study, for nonendodontically treated root fractures, the proportion of maxillary and mandibular molars was very high (92.6% in 2015 and 87.8% in 2019), which was consistent with the results of Chan et al. [7] (87.5%). This might be related to the heavier masticatory force associated with molars or to the habitual use of molars in the chewing of hard foods. However, for endodontically treated root fractures, the proportion of maxillary and mandibular premolars changed markedly between 2015 and 2019. The mandibular premolar ETRF% increased from 33.3% in 2015 to 81.8% in 2019; and the maxillary premolar ETRF% increased from 28.6% in 2015 to 57.9% in 2019. The sample of mandibular premolars was small in 2015, and this might introduce some bias to our results; however, the increase in the maxillary premolar ETRF% was statistically sound. This was also consistent with the results reported by Liao et al. [10]. This result suggested that endodontic treatment has more impact on premolars.
In this study, the morphology of the fractured root was also investigated. The results showed that oval roots were more prone to fracture than other types of roots in both ETRF and NETRF teeth. This was consistent with the results reported by Chan et al. [6], in which the mesiobuccal roots of maxillary molars and mesial roots of mandibular molars were more prone to fractures. The oval root canal, with a smaller mesiodistal dimension, is more prone to root fractures [9]. The ETRF% for both oval and circular roots increased from 2015 to 2019; however, there were no significant differences for both of them.
The restoration performed in root fractured teeth was also investigated. ETRF teeth without crown restorations accounted for 76.9% in 2015 and 78.3% in 2019. Almost 80% of ETRF teeth were only composite or amalgam filled. Compared with those treated with crown restoration, endodontically treated teeth seemed to be more susceptible to fracture if they were restored with a composite or amalgam filling, which might have aggravated the risk of fracture. Therefore, dental practitioners have an important responsibility regarding their decision about the final restoration delivered to these teeth, and post-treatment instructions also play an important role in the prevention of root fractures. The position of the teeth in the dental arch (e.g., orthodontic anomalies and misalignment) results in them being subjected to different masticatory forces. Therefore, we also evaluated the position of the teeth in the dental arch. The results showed that only a small number of root fractured teeth were misaligned in the ETRF and NETRF groups. Thus, misalignment of teeth did not seem to be a risk factor for root fractures in this study.
Conclusion
In summary, the proportion of NETRF teeth and non-vertical root fractured posterior teeth in the Chinese population is high. The proportion of vertical root fractures in endodontically treated teeth increased significantly from 2015 to 2019, which suggested we should pay more attention to the endodontic treatment factors in the occurrence of root fractures. In addition, endodontic treatment has higher impact on female patients and premolars.
References
Mora MA, Mol A, Tyndall DA, Rivera EM (2007) In vitro assessment of local computed tomography for the detection of longitudinal tooth fractures. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103:825–829. https://doi.org/10.1016/j.tripleo.2006.09.009
Wang P, Yan XB, Lui DG, Zhang WL, Zhang Y, Ma XC (2011) Detection of dental root fractures by using cone-beam computed tomography. Dentomaxillofac Radiol 40:290–298. https://doi.org/10.1259/dmfr/84907460
Gao A, Cao D, Lin Z (2021) Diagnosis of cracked teeth using cone-beam computed tomography: literature review and clinical experience. Dentomaxillofac Radiol 50:20200407. https://doi.org/10.1259/dmfr.20200407
Mizuhashi F, Ogura I, Sugawara Y, Oohashi M, Mizuhashi R, Saegusa H (2021) Diagnosis of root fractures using cone-beam computed tomography: difference of vertical and horizontal root fracture. Oral Radiol 37:305–310. https://doi.org/10.1007/s11282-020-00453-y
Wang P, Lv H, Sun H, Lin Y, He W (2011) Horizontal root fractures in posterior teeth: a case series. Dent Traumatol 27:152–155. https://doi.org/10.1111/j.1600-9657.2010.00962.x
Chan CP, Lin CP, Tseng SC, Jeng JH (1999) Vertical root fracture in endodontically versus nonendodontically treated teeth: a survey of 315 cases in Chinese patients. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 87:504–507. https://doi.org/10.1016/s1079-2104(99)70252-0
Chan CP, Tseng SC, Lin CP, Huang CC, Tsai TP, Chen CC (1998) Vertical root fracture in nonendodontically treated teeth–a clinical report of 64 cases in Chinese patients. J Endod 24:678–681. https://doi.org/10.1016/s0099-2399(98)80154-4
Yeh CJ (1997) Fatigue root fracture: a spontaneous root fracture in non-endodontically treated teeth. Br Dent J 182:261–266. https://doi.org/10.1038/sj.bdj.4809363
Hsiao LT, Ho JC, Huang CF, Hung WC, Chang CW (2020) Analysis of clinical associated factors of vertical root fracture cases found in endodontic surgery. J Dent Sci 15:200–206. https://doi.org/10.1016/j.jds.2019.09.003
Liao WC, Tsai YL, Wang CY, Chang MC, Huang WL, Lin HJ, Liu HC, Chan CP, Chang SH, Jeng JH (2017) Clinical and radiographic characteristics of vertical root fractures in endodontically and nonendodontically treated teeth. J Endod 43:687–693. https://doi.org/10.1016/j.joen.2016.12.009
Yang SF, Rivera EM, Walton RE (1995) Vertical root fracture in nonendodontically treated teeth. J Endod 21:337–339. https://doi.org/10.1016/s0099-2399(06)81013-7
Rivera EM, Walton RE (2007) Longitudinal tooth fractures: findings that contribute to complex endodontic diagnoses. Endod Top 16:82–111. https://doi.org/10.1111/j.1601-1546.2009.00243.x
Lin ZT, Zhu M, Liu S, Wang TM (2013) Clinic study and radiographic features on CBCT images of root fractures of posterior teeth. J Oral Sci Res 29:929-931+935. https://doi.org/10.13701/j.cnki.kqyxyj.2013.10.003
Tsai YL, Liao WC, Wang CY, Chang MC, Chang SH, Chang SF, Chang CW, Huang YD, Chan CP, Jeng JH (2017) Horizontal root fractures in posterior teeth without dental trauma: tooth/root distribution and clinical characteristics. Int Endod J 50:830–835. https://doi.org/10.1111/iej.12704
Wang P, Su L (2009) Clinical observation in 2 representative cases of vertical root fracture in nonendodontically treated teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 107:e39-42. https://doi.org/10.1016/j.tripleo.2008.12.014
Gavini G, Santos MD, Caldeira CL, Machado MEL, Freire LG, Iglecias EF, Peters OA, Candeiro GTM (2018) Nickel-titanium instruments in endodontics: a concise review of the state of the art. Braz Oral Res 32:e67. https://doi.org/10.1590/1807-3107bor-2018.vol32.0067
Lim MJ, Kim JA, Choi Y, Hong CU, Min KS (2017) Differentiating spontaneous vertical root fracture in endodontically treated tooth. Eur J Dent 11:122–125. https://doi.org/10.4103/ejd.ejd_160_16
Funding
This work was supported by the General Project of Jiangsu Provincial Health Commission (M2021077), scientific research fund of Jiangsu Medical Association (SYH-3201150–0007(2021002)), and Nanjing Clinical Research Center for Oral Diseases (no. 2019060009).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Ethics approval
This study was approved by the Ethics Committee of Nanjing Stomatological Hospital (ethics approval number: 2018NL-044(KS)).
Consent to participate
For this type of study, formal consent is not required.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Pan, X., Tang, R., Gao, A. et al. Cross-sectional study of posterior tooth root fractures in 2015 and 2019 in a Chinese population. Clin Oral Invest 26, 6151–6157 (2022). https://doi.org/10.1007/s00784-022-04564-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-022-04564-0