Abstract
Objectives
Zirconia-based restorations have been increasingly used on implant and teeth abutments, but the evidence about clinical outcomes of these restorations is limited. The aim of this study was to assess up to 7-year clinical outcomes of implant- and tooth-supported zirconia-based single crowns.
Materials and methods
In this retrospective study, 261 patients with 556 single crowns supported by either teeth (324) or implants (232) were examined during 3- to 7-year follow-up (mean observation of 60.70 months for tooth and 59.20 months for implant-supported crowns). California Dental Association (CDA) quality evaluation system was used to evaluate the restorations. Soft tissue status was assessed using plaque and gingival index scores, bleeding on probing, and pocket depth. Patient and professional satisfaction were evaluated by visual analog scale (VAS).
Results
The 5-year Kaplan–Meier survival probability was 98.3 and 97.3 for implant- and tooth-supported crowns, respectively. In regard to CDA rating, most of the crowns were ranked as either excellent or acceptable (99.5 %). The recorded failures were replacement of the crown due to porcelain chipping (3), implant failure (1), and teeth extraction (5). Soft tissue parameters were not affected by the restorations compare to control teeth. The VAS was high for both patients and clinicians.
Conclusions
Zirconia-based single crowns on both tooth and implant abutments showed promising clinical performance in this up to 7-year follow-up.
Clinical relevance
The zirconia-based single crowns can be used clinically for tooth- and implant-supported restorations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
During the last decades, metal–ceramic crowns have been the restoration of choice because of their relative esthetic quality and high success rate. Due to long-term experience, the metal–ceramic restorations showed good clinical results [1, 2]. However, the presence of the metal framework and lack of light transmission is a limiting factor for the esthetic quality of these restorations. Increasing demands for more esthetic materials and metal-free restorations have led to improvement of new dental ceramics [3, 4].
To increase the mechanical strength of all-ceramic restorations, different core materials were used. Recently, yttria-stabilized zirconia polycrystals (Y-TZP) has been made available to dentistry through the CAD/CAM technology [5]. Zirconia is an acceptable material because of favorable mechanical properties, good esthetics, and biocompatibility [6, 7]. Zirconia has been used in clinical dentistry for at least 15 years; however, the reports regarding the clinical performance and survival rates of zirconia-based single crown restorations, especially for implant-supported restorations are limited [8–13]. The survival rates of zirconia-based restorations were 70 to 100 % after 2- to 5-year follow-up [14–16]. No failure of the zirconia- based single crowns were reported after 3 years by Beuer et al. [10] and Tartaglia et al. [11]. Ortorp et al. [8] reported 88.8 % cumulative survival rates for zirconia single crowns (Procera, Nobel Biocare AB) in a 5-year retrospective study. The clinical studies on zirconia-based single crowns are limited and most of the studies were performed on fixed dental prostheses (FDPs) [17, 18]. Larsson and Wennerberg [19] calculated the 5-year cumulative survival rate of 95.9 % for tooth-supported and 97.1 % for implant-supported zirconia crowns in a systematic review. They reported that complication rate of tooth- and implant-supported zirconia-based single crowns were 5.6 and 7.5 %, respectively [19]. Takeichi et al. [20] compared the clinical outcomes of metal–ceramic and zirconia single crowns in another systematic review. Although they found similar 3-year cumulative survival percentage for metal–ceramic and zirconia crowns (95.9 % for zirconia and 95.4 % for metal–ceramic crowns), they revealed that scientific clinical data regarding zirconia crowns are limited and long-term clinical studies are needed to compare metal–ceramic and zirconia crowns [20].
One of the most frequent problems with zirconia reconstructions is chipping or cracking of the veneer ceramic. The incidence of veneer chipping was 4.5 % per 100 FDP/year (95 %CI, 1.35–15.3 %) and 79.44 % (95 %CI, 44.28–93.44 %) of restorations were free of chipping in a systematic review [14]. Heintze and Rousson [21] reported that for an observation period of 3 years, zirconia FDPs have 7 % higher veneer chipping than metal–ceramic FDPs (90 % survival rate regarding to chipping after 3 years).
Jung et al. [22] found 3.5 % chipping of ceramic veneers of implant-supported single crowns in a meta-analysis which was similar in all-ceramic and metal–ceramic restorations. Hosseini et al. [12] and Ortorp et al. [8] reported 3 % of ceramic chipping in implant-supported zirconia-based single crowns. Larsson and Wennerberg [19] showed that the most reason for failure and complication in implant-supported single crowns was veneer material fracture while in tooth-supported crowns, the most common reason for failure was endodontics/periodontics problems.
Vigolo and Mutinelli [23] found no statistically significant difference in the 5-year clinical outcomes of metal–ceramic and zirconia crowns (95 % in metal–ceramic and 79 and 85 % in two kinds of zirconia crowns) but they showed that technical problems, such as extended fracture of the veneering ceramic, tended to occur more frequently in the zirconia crowns.
It seems that framework design [24], firing and cooling temperatures of veneering ceramics [25], and methods of veneering of zirconium oxide are critical factors in achieving better results [26].
The aim of this retrospective study was to evaluate the 3–7 year clinical performance of a large number of zirconia-based crowns, placed on both natural teeth and implant abutments. The null hypothesis was that there would be no significant difference in the clinical performance of tooth- and implant-supported zirconia-based single crowns.
Materials and methods
In this study, 261 patients (146 women and 115 men) with a mean age of 48 ± 14.6 years (range 18–62 years) who had received 556 single zirconia-based crowns (Cercon, Degudent, Hanau, Germany) between October 2007 to March 2011 were evaluated (Table 1). This research was approved by the Ethical Committee of Isfahan University of Medical Sciences (# 391045) and individuals signed written consent in the first follow-up visits.
The inclusion criteria consisted of having received a zirconia crown supported by either implants or teeth from the same private practice during the aforementioned time span. Patients had good oral health and there was no sign of periodontal disease. The abutment teeth had to be vital or state-of-the-art endodontically treated. All the inserted crowns during this period were included in the study. The studied restorations consisted of 324 crowns on natural tooth abutments and 232 on implant abutments (Table 2). Clinical treatment was performed by one prosthodontist with more than 20 years’ experience in all-ceramic restorations in a private dental clinic. The laboratory procedures were also performed by one expert dental technician.
Prosthodontic treatment procedures
Tooth-supported restorations
The abutment teeth were prepared with a circumferentially rounded shoulder (1.0 mm in width), an axial reduction of 1.5 mm, an occlusal reduction of 1.5 to 2.0 mm with approximately 10° to 20° taper, and the minimum retention height of 4 mm. The preparation margins were located at the gingival level or not more than 1 mm subgingivally. The shoulders were prepared using round-end taper fine diamond burs (850-021; Meisinger, Neuss, Germany). The preparations were modified in mandibular incisors with less reduction of teeth according to Schmitt et al. [16]. The two step putty wash (Panasil, Kettenbach, Eschenburg, Germany) and double retraction cord (Ultrapak, Ultradent, South Jordan, UT) techniques were used for making the impression. Interocclusal record was made with polyvinyl siloxane bite registration material (Futar D, Kettenbach). Following tooth preparation and making impression, interim restoration was fabricated using direct method (Protemp 3 Garant, 3M ESPE, ST. Paul, MN) and luted (Free eugenol, GC Co, Tokyo, Japan). The impressions were sent to laboratory and poured using type IV dental stone (Fuji Rock, GC, Tokyo, Japan).
Out of 324 teeth, 276 were root canal treated. Three of these teeth were restored with cast gold-alloy post and core, 39 had amalgam core, and the remaining were treated with prefabricated post (DT LIGHT-POST, Bisco Inc., Schaumburg, IL) and a composite resin core material (Build-It, Pentron LLC, Wallingford, USA).
Implant-supported restorations
The implants were non-submerged (standard plus, narrow, regular, or wide neck, Straumann Dental Implant System, Straumann AG, Basel, Switzerland). Conventional delayed loading protocol was followed after implant placement. One step putty wash (Panasil, Kettenbach) impression technique with open tray and screw-type impression cap (Straumann Dental Implant System, Straumann AG) was used for implant-supported restorations. An interocclusal record was made with polyvinyl siloxane bite registration material (Futar D, Kettenbach). The impressions with proper implant analogs attached to impression copings were sent to dental laboratory and poured using gingival mask (esthetic mask, Ettlingen, Germany) and type IV stone (Fuji Rock, GC). Appropriate cemented-type abutment (narrow-neck abutment, regular or wide-neck SynOcta abutments, Straumann Dental Implant System, Straumann AG) with 6° taper and minimum retention height of 4 mm were selected and screwed in implant analogs.
Laboratory procedures
The zirconia copings were fabricated by means of a CAD/CAM system (Cercon, DeguDent, Hanau, Germany). Master casts were scanned (Cercon Eye, DeguDent), and the zirconia copings were designed (Cercon art 3.0.1, DeguDent) with anatomical form to create homogeneous space for the veneering ceramic and made in white or colored zirconia (Cercon Base, DeguDent) by CAM machine (Cercon Brain, DeguDent) with 30-μm space for luting agent. Copings were sintered in 1350 °C for 7 h (Cercon Heat, DeguDent). The veneering of copings was performed using corresponding veneering ceramic with conventional layering technique (Cercon Ceram Kiss, DeguDent). The core was covered by even thickness of veneering ceramic, with a maximum of 2 mm of layering porcelain. Zirconia core was designed in respect of the layered ceramic. Minimum thickness of the zirconia core material at the axial walls was 0.5 mm. The zirconia frameworks were sandblasted with Al2O3 (110 μm–3 bar) and then cleaned in ultrasonic cleaner. All of the final restorations were fabricated by the same dental technician.
Try-in and insertion of restorations
At the try-in appointment, proximal contacts and static and dynamic occlusal contacts were checked and corrected with fine diamond burs with water cooling. Silicon disclosing medium (Fit Checker, GC Co) was used to check the fit of restorations. Manufacturer guidelines were followed for glazing of final restorations. The abutment teeth were cleaned with pumice and rubber cups before cementation and titanium abutments were cleaned with 70 % alcohol in ultrasonic cleaner (Sonorex, Bandelin Electronic, Berlin, Germany) for 5 min. Intaglio surface of crowns were treated with airborne-particle abrasion with 50-μm Al2O3 particles at 3-bar pressure and then cleaned in ultrasonic cleaner.
Zinc polycarboxylate (Poly F, Dentsply, Weybridge, England) (149, 46 %), resin (Panavia F 2.0 Kuraray Co, Kurashiki, Japan) (106, 32.7 %), or resin-modified glass ionomer (Fuji Plus, GC Co) (69, 21.3 %) cements were used for cementation of the tooth-supported crowns. Implant-supported crowns were provisionally cemented (Free eugenol, GC Co) (207, 89.3 %), or zinc polycarboxylate (Poly F, Dentsply) (17, 7.3 %) or resin (Panavia F 2.0 Kuraray Co) (8, 3.4 %) luting agents were used for their cementation. Resin and resin-modified glass ionomer cements were used for the short abutments to reduce the risk of debonding. After 5 min, excess cement was removed; the occlusion was refined as needed, and any adjusted crown surfaces were polished with pumice paste and rubber cups. For all crowns, standardized parallel periapical radiographs (Irix 70, Trophy, Kodak Spa, Cinisello Balsamo, Italy) were taken to verify the seating of the restorations.
Registrations and clinical examinations
The patients were scheduled for checkup of the crowns after 6 and 12 months from the date of insertion of the crowns and continued annually at 24-, 36-, 48-, 60-, 72-, and 84-month intervals. Patients were asked to contact the clinic whenever they had problems with their crowns. The follow-up examinations were performed by two prosthodontists other than the clinician who had placed restorations. Inter-examiner agreement for the examined characteristics was 92 %. Every finding (complication or failure) of crowns were additionally examined by the principal investigator.
For each patient, data were collected regarding the patient’s gender, age at crown delivery, number of crowns cemented, tooth or implant position, luting agent, occluding teeth in the opposite jaw, endodontic treatment before delivery, post and core material, and dynamic occlusal contacts. The California Dental Association (CDA) guidelines were used to evaluate the quality of zirconia-based crowns [27]. Variables alpha and bravo were excellent and acceptable, whereas variables charlie and delta were defined as not acceptable and remake of crown was necessary. The treatment was considered a failure when the abutment tooth was extracted or the implant failed following a biological complication (root fracture, endodontic and periodontal problems, and loss of osseointegration) or any variables scored charlie or delta. Any restoration or abutment problem which needed clinical intervention and did not require removal of the restoration was defined as complication. Survival was defined as the restoration being in situ with or without complication.
The following periodontal parameters were recorded for the studies crowns and contralateral, non-crowned teeth as the control. In addition, parallel periapical radiographs were taken to evaluate bone loss at the first, third, fifth, and seventh year follow-up. The radiographs were evaluated by researchers for any marked sign of bone loss.
Gingival index (GI) [28, 29]: GI 0 = normal healthy gingiva; GI 1 = slight inflammation, slight color change, edema, no spontaneous bleeding; GI 2 = moderate inflammation, moderate color change, edema, bleeding on probing; GI 3 = serious inflammation, serious color change, serious edema, spontaneous bleeding.
Plaque index (PI) [28]: PI 0 = no dental plaque, PI 1 = dental plaque to be pointed out only with dental plaque-revealing substances, PI 2 = dental plaque to be pointed out at a glance, PI 3 = plentiful dental plaque.
Probing pocket depth (PPD) [29] was analyzed by means of 4-point periodontal probing (mesial, buccal, distal, and palatal/lingual) in the depth of the pocket until a slight resistance was met.
Bleeding on probing (BOP) was evaluated with a yes/no score.
Tooth mobility was classified as (1) <0.2 mm in horizontal direction, (2) 0.2–1 mm horizontally, (3) >1 mm horizontally, and (4) mobility in vertical direction.
Smoking habits (more than 10 cigarettes per day as heavy smoker), presence of pain and tenderness of temporomandibular joints, and nocturnal bruxism of individuals were also asked and recorded in the examination form.
The patients were interviewed regarding their satisfaction with their crowns (regarding chewing comfort, color, esthetics, and general satisfaction) using a visual analog scale (VAS) of 100 mm with the endpoints extremely dissatisfied (0) and extremely satisfied (100).
Statistical analysis
The data were evaluated using descriptive statistics. To analyze and compare the survival probabilities of the tooth- and implant-supported single crowns, Kaplan–Meier analysis and the log-rank test were applied. The CDA score comparison between tooth- and implant-support restorations was performed by using the log-rank test. Because a patient could have received more than one crown, a general estimation equation model (GEE; binary logistic, failure yes/no, chipping yes/no, as target variable) was produced with type of restoration (implant- or tooth-supported) as covariates to support the results of the log-rank test.
Cox regression was used to evaluate hazard ratio of the effect of bruxism, position of the restorations, and antagonist occlusion. Comparison between GI, PI, and PPD of studied teeth/implants and control teeth was made using Wilcoxon signed-rank test for paired samples and comparison between GI, PI, and PPD of tooth- and implant-supported crowns was made using Mann–Whitney U test. McNemar’s test was used for comparing BOP of studied teeth/implants and control teeth. The agreement between VAS score of clinicians’ and patients’ satisfactions was evaluated using the Spearman correlation test. The level of significance was set at 0.05. The statistical analysis was performed by using IBM SPSS (version 20, IBM Corp, Armonk, NY) statistical software.
Results
A total of 556 single crowns were installed in 261 patients (146 women and 115 men). Of these, 324 tooth-supported single crowns in 139 patients (81 women and 58 men, mean age of 46 ± 14 years), and 232 implant-supported single crowns were installed in 122 patients (65 women and 57 men, mean age of 50 ± 13 years). For tooth-supported crowns, there were an average 2.4 crowns cemented per patient (maximum of 17 in a 58-year-old patient) and for implant-supported crowns, there were an average 1.8 crowns cemented per patient (maximum of 8 in a 66-year-old patient). The distribution of restored teeth and location of implants are presented in Table 2. There was no information on five patients (2 % drop-out) with 5 crowns (1 implant-supported crown, and 4 tooth-supported crowns) because they did not come back to the clinic after the insertion of the crowns. The mean observation times were 60.70 months for the tooth-supported and 59.20 months for the implant-supported single crowns (range 36–84 months).
Among the participants, 4.6 % was heavy smokers; 98.3 % of the implant-supported and 95.7 % of tooth-supported patients did not have pain in temporomandibular joints and 15.7 % of patients had nocturnal bruxism.
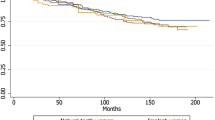
Table 3 presents all failures occurred during the observation time. During the follow-up period no core material fracture was occurred. Nineteen veneer material fractures (8.2 %) in implant-supported group (12 in molar, 7 in anterior teeth) and 26 veneer fractures (8.1 %) in tooth-supported group (14 in molar, 2 in premolar, and 10 in anterior teeth) were recorded. Among these veneer fractures 17 implant- supported crowns and 25 tooth-supported crowns were not considered failed and after polishing, the chippings were not considered to interfere with function and esthetics. The major porcelain chipping in 2 implant-supported and 1 tooth-supported crown were considered failed and the crowns were remade. There was no significant difference between the two groups regarding to fracture (χ 2 = 0.55, P = 0.46) (Table 4). The GEE model estimated that the risk of chipping was not significantly different in the implant- and tooth-supported groups (Exp (B) = 0.32, P = 0.55) that supported the result of the log-rank test. Figure 1 shows the cumulative fracture rate of studied single crowns according Kaplan–Meier survival probability including minor and major fractures (Kaplan–Meier fracture free probability of 91.0 % (95 % CI, 87.7–94.3 %) and 91.4 % (95 % CI, 86.9–95.9 %) for tooth- and implant-supported single crowns, respectively). The rate of porcelain chipping was significantly higher in patients with bruxism (χ 2 = 27.94, P < 0.001, hazard ratio (HR) = 4.50, 95 % CI, 2.44–8.29). The veneer chipping was significantly less in premolars than in molar and anterior crowns (χ 2 = 10.56, P = 0.004, HR = 0.18, 95 % CI, 0.05–0.58).
Five abutment teeth were extracted (1.6 %; 3 root fractures, 1 endodontic, and 1 periodontal problems) and 20 (6.3 %) crowns were deboned which all of them could be recemented. No secondary caries of the natural abutment teeth was recorded. In total, 6 tooth-supported restorations (1.9 %; in 6 patients) were recorded as failures: 5 abutment teeth were extracted and 1 veneer fractured. One implant failure was recorded due to loss of osseointegration. In total, 3 implant-supported restorations (1.3 %; in 3 patients) were recorded as failures: 1 implant failure and 2 veneer fracture.
The restorations were occluded against natural teeth (53.7 % in tooth-supported and 43.8 in implant-supported crowns), fixed dental prosthesis (44.9 % in tooth-supported and 51.6 % in implant-supported crowns), or removable prosthesis (1.4 % in tooth-supported and 4.6 % in implant-supported crowns). In tooth-supported group, the type of antagonist had no significant effect on failure (χ 2 = 0.30, P = 0.58, HR = 1.07 (95 % CI, 0.85–1.34) and fracture (χ 2 = 2.05, P = 0.15, HR = 1.19 (95 % CI, 0.94–1.52). In implant-supported group, the failure and fracture were also not affected by the type of antagonist (χ 2 = 2.32, P = 0.13, HR = 0.81 (95 % CI, 0.62–1.06) and χ 2 = 2.86, P = 0.09, HR = 0.79 (95 % CI, 0.60–1.04), respectively).
Table 4 demonstrates the CDA scores and comparison of tooth- and implant-supported restorations.
Table 5 presents the soft tissue status of the studied zirconia-based crowns. No significant differences were found concerning plaque index, gingival index (Wilcoxon signed-rank test for paired samples; P = 0.07 and P = 0.06), and bleeding on probing (McNemar’s test; P = 0.07), between abutment teeth/implant and the control teeth. There were no significant differences in PI and GI of the two groups (Mann–Whitney U test; P = 0.64 and P = 0.95).
Probing pocket depth was 1 to 3 mm in 318 (99.4 %) of tooth-supported group and 217 (93.9 %) of implant-supported group. Two teeth and 14 implants had more than 4-mm pockets (Table 6). There were significant differences in pocket depth between implant- and tooth-supported crowns (Mann–Whitney U test; P < 0.001). The radiographic evidences of bone loss were not observed in the studied patients.
The patient and clinician satisfaction in both tooth-supported and implant-supported groups regarding chewing comfort, color, esthetics, and general satisfaction were high. Spearman correlation test showed a strong relation between patient’s and clinician’s satisfaction in both tooth-supported and implant-supported groups regarding general satisfaction (r = 0.66, P < 0.001) (Table 7).
According to Kaplan–Meier analysis, the 5-year survival rate of tooth- and implant-supported crowns were 97.3 (95 % CI, 94.9–99.6) and 98.3 (95 % CI, 98.3–99.5) respectively (χ 2 = 0.19, P = 0.66, GEE model estimate: Exp (B) = 0.41, P = 0.58) (Fig. 2).
Discussion
The hypothesis of the study for some of the CDA rating criteria was rejected. But the present study could not prove significant difference in failure between tooth- and implant-supported zirconia-based single crowns (χ 2 = 0.19, P = 0.66). There are few studies about the clinical outcomes of zirconia-based single crowns [8–13, 16, 19, 20, 23]. In the present study, 556 zirconia-based crowns supported either by teeth or implants were assessed in a 3- to 7-year follow-up. During the follow-up, only 2 % of the restorations have been registered as drop-out. The 5-year survival rate of tooth- and implant-supported crowns were 97.3 and 98.3, respectively. The 5-year cumulative survival rate of 95.9 % for tooth-supported and 97.1 % for implant-supported zirconia crowns were calculated in Larsson and Wennerberg [19] systematic review. The 3-year cumulative survival rate of 95.9 % was reported by Takeichi et al. [20] for zirconia single crowns. However, Ortorp et al. [8] suggested 88.8 % and Vigolo and Mutinelli [23] reported 79 and 85 % cumulative survival rate for two types of tooth-supported zirconia crowns after a 5-year of follow-up. The survival was estimated at 98 % over 24 months by Groten and Huttig [30]. Rinke and coworkers [31] found 100 % survival rate for Cercon single crowns with a prolonged cooling period of the veneering porcelain. In a 1-year randomized clinical trial (RCT) study, the survival rate of the zirconia-based and metal–ceramic single implant-supported crowns were 97.8 and 97.1 %, respectively [12]. Zembic et al. [13] reported 88.9 % survival rate for implant-supported all-ceramic single crowns with zirconia abutments. Salinas and Eckert [32] found survival rate of 91.2 % (CI 86.6–94.2 %) for all-ceramic implant-supported single crowns. The different results may be explained by different materials and follow-up time.
In regard to technical complications, no core material was fractured. This is in line with previous studies [8, 10–12, 30]. But, Cehreli et al.[9] reported one restoration with fracture in both core and veneering porcelain in a patient with severe nocturnal bruxism. Forty five (8.1 %) out of 556 crowns had chipping of veneering porcelain in which 3 (0.5 %) of them were major and needed replacement and 42 (7.6 %) were minor and polished. There was no significant difference between tooth- and implant-supported crowns regarding porcelain chipping (χ 2 = 0.55, P = 0.46). This is in contrast to previous studies that found implant-supported restorations have more technical complications and veneering material fracture [8, 33]. This can be explained by difference in resiliency of periodontal ligament of natural teeth and osseointegrated implant and limited proprioception of implants [19]. Zirconia-based implant-supported fixed partial dentures had significantly higher frequency of veneering material fractures than tooth-supported restorations [21, 34]. This was not confirmed in the present study. The reason is probably due to less complicated design, load, and strains of single-tooth restoration compare with fixed partial dentures [19].
The rate of porcelain chipping was significantly higher in patients with bruxism (χ 2 = 27.94, P < 0.001). The veneer chipping was also significantly less in premolars than in molar and anterior crowns (χ 2 = 10.56, P = 0.004). This can be the result of more occlusal force in molars and less favorable force direction in anterior teeth. Ortorp et al. [8] reported 6 veneer fractures of 143 zirconia crowns and Beuer et al. [10] suggested no fracture in 50 single crowns after a 3-year follow-up. In a 3-year prospective study comparing zirconia versus metal–ceramic implant-supported single crowns, chipping of veneering porcelain was recorded at one metal–ceramic (out of 46) and one all-ceramic crown (out of 52) [12]. Groten and Huttig [30] reported 2 ceramic veneering material chippings of 54 single crowns after 28 months which needed replacement. Nothdurft and Pospiech [35] showed 10 % and Schwarz et al. [36] reported 24.5 % porcelain chipping in Cercon single crowns on implant abutments. In the study conducted by Schwarz et al. [36], 11.3 % of fractures led to failure. Vigolo and Mutinelli [23] concluded that even if there was no significant difference between clinical outcomes of posterior metal–ceramic and zirconia crowns, the zirconia ceramic FDP groups tended to have more frequent extended fracture of the veneering ceramic. In the systematic review by Larsson and Wennerberg [19], 26 out of 615 single zirconia crowns (4.2 %) on teeth or implants showed veneer fracture. Although a large number of chip fractures can be simply polished, chipping fractures is disappointing to both the clinician and patient, and sometimes the replacement of restorations was required because of major chipping [8, 17]. There are several suggested reasons for chipping of zirconia veneering material including: mismatch of coefficient thermal expansion of zirconia and veneering material, improper support by zirconia framework, and low thermal conductivity of zirconia [25]. In the current study, most of the frameworks were designed to provide appropriate support for the veneering material and the manufacturer recommended ceramic (Cercon Ceram Kiss, DeguDent) was used for veneering. In addition, reduced cooling rate after the final firing or glazing procedure can reduce the risk of veneer chipping. [25] The veneering ceramics, zirconia framework material and design, and fabrication techniques were different in each study and might affect the result of clinical studies [20]. Improvements in porcelain materials and technology can resolve this problem and enhance the bond strength between the porcelain and a zirconia framework [37].
In the present study, 6.3 % of tooth-supported and 1.3 % of implant-supported single crowns were deboned which all of them were recemented. In the Ortorp’s et al. study [8], 12 tooth-supported zirconia crowns (7 %) lost retention in which 8 of them could be recemented. Similar results have been reported by Schwarz et al. [36] in implant-supported Cercon crowns (7.5 % of debonding). Larsson et al. [19] reported 2 % of loss of retention among tooth-supported crowns. The relatively high rate of debonding in tooth-supported single crowns in present study could probably be related to taper of preparation, and short abutments. It has been shown that using resin-based luting agents and surface treatments of abutment and intaglio surface of restorations can increase the retention of implant-supported copings [38–40]. The implant abutment with less taper can be the reason for less debonding of implant-supported crowns in spite of temporary cementation.
The marginal accuracy was considered excellent in 98.7 % of implant-supported and 86.9 % of tooth-supported and considered acceptable in 1.3 % of implant-supported and 13.1 % of tooth-supported crowns. In the study by Cehreli et al. [9], 80 % of the single crowns had excellent marginal fit, while 13 % of the crowns were acceptable and 6 % scored not acceptable. Hosseini et al. [12] found no marginal misfit in zirconia single implant-supported crowns after 3 years. The different results of the studies can be explained by different manufacturers and fabrication techniques. The significantly better margins of implant-supported single crowns in this study can be the result of prefabricated margins of the implant analogs which can be distinguished easily.
There was no secondary caries in tooth-supported crowns. It was reported in a systematic review that the annual rate of secondary caries in all-ceramic and metal–ceramic crowns were 0.37 and 0.64 %, respectively [41].
During the follow-up period, the color and surface texture were rated excellent in most of the tooth-supported and implant-supported single crowns (Table 4).
In regard to soft tissue status, the results of present study showed that 27.9 % of patients had mild to moderate inflammation (GI 1 and 2) and 24.3 % have PI scores of 1 and 2 (Table 5). On the other hand, 26.3 % of them have positive BOP. These findings showed that oral hygiene of the participants should be improved. High plaque and gingival indices and pocket depth may be lead to peri-implantitis in the future. The periodontal parameters of the crowned teeth/implants and control teeth were not significantly different. These results were in agreement with the previous studies on zirconia restorations, indicating good biologic reactions between the periodontal tissues and zirconia [18, 42–44].
The professional’s and patient’s satisfaction with the zirconia single crowns was generally high, which was consistent with the previous studies [45].
One of the limitations of present study was the high range of observation period (36–84 months) and examinations were not performed for all of the single crowns after 7 years. The Kaplan–Meier statistical analysis of survival and log-rank test were used to compensate this limitation. Another limitation was the retrospective nature of the current study. On the other hand, the results of this study were obtained from one practitioner in a private clinic and cannot be generalized.
Conclusion
Within the limitations of this study, it can be concluded that zirconia- based single crowns supported either by tooth or implant revealed favorable clinical survival rates (5-year Kaplan–Meier survival rates of 97.3 and 98.3 %, respectively) and this treatment modality is a promising prosthodontic management.
References
Walton TR (2002) An up to 15-year longitudinal study of 515 metal-ceramic FPDs: part 1. Outcome. Int J Prosthodont 15:439–445
Burke FJ, Lucarotti PS (2009) Ten-year outcome of crowns placed within the general dental services in England and Wales. J Dent 37:12–24
Raigrodski AJ (2004) Contemporary materials and technologies for all-ceramic fixed partial dentures: a review of the literature. J Prosthet Dent 92:557–562
Jung RE, Holderegger C, Sailer I, Khraisat A, Suter A, Hammerle CH (2008) The effect of all-ceramic and porcelain-fused-to-metal restorations on marginal peri-implant soft tissue color: a randomized controlled clinical trial. Int J Periodontics Restorative Dent 28:357–365
Denry I, Kelly JR (2008) State of the art of zirconia for dental applications. Dent Mater 24:299–307
Tinschert J, Natt G, Mautsch W, Augthun M, Spiekermann H (2001) Fracture resistance of lithium disilicate-, alumina-, and zirconia-based three-unit fixed partial dentures: a laboratory study. Int J Prosthodont 14:231–238
Sundh A, Molin M, Sjogren G (2005) Fracture resistance of yttrium oxide partially-stabilized zirconia all-ceramic bridges after veneering and mechanical fatigue testing. Dent Mater 21:476–482
Ortorp A, Kihl ML, Carlsson GE (2012) A 5-year retrospective study of survival of zirconia single crowns fitted in a private clinical setting. J Dent 40:527–530
Cehreli MC, Kokat AM, Akca K (2009) CAD/CAM Zirconia vs. slip-cast glass-infiltrated Alumina/Zirconia all-ceramic crowns: 2-year results of a randomized controlled clinical trial. J Appl Oral Sci 17:49–55
Beuer F, Stimmelmayr M, Gernet W, Edelhoff D, Guh JF, Naumann M (2010) Prospective study of zirconia-based restorations: 3-year clinical results. Quintessence Int 41:631–637
Tartaglia GM, Sidoti E, Sforza C (2014) Seven-year prospective clinical study on zirconia-based single crowns and fixed dental prostheses. Clin Oral Investig
Hosseini M, Worsaae N, Schiodt M, Gotfredsen K (2013) A 3-year prospective study of implant-supported, single-tooth restorations of all-ceramic and metal-ceramic materials in patients with tooth agenesis. Clin Oral Implants Res 24:1078–1087
Zembic A, Bosch A, Jung RE, Hammerle CH, Sailer I (2013) Five-year results of a randomized controlled clinical trial comparing zirconia and titanium abutments supporting single-implant crowns in canine and posterior regions. Clin Oral Implants Res 24:384–390
Schley JS, Heussen N, Reich S, Fischer J, Haselhuhn K, Wolfart S (2010) Survival probability of zirconia-based fixed dental prostheses up to 5 yr: a systematic review of the literature. Eur J Oral Sci 118:443–450
Raigrodski AJ, Hillstead MB, Meng GK, Chung KH (2012) Survival and complications of zirconia-based fixed dental prostheses: a systematic review. J Prosthet Dent 107:170–177
Schmitt J, Wichmann M, Holst S, Reich S (2010) Restoring severely compromised anterior teeth with zirconia crowns and feather-edged margin preparations: a 3-year follow-up of a prospective clinical trial. Int J Prosthodont 23:107–109
Sax C, Hammerle CH, Sailer I (2011) 10-year clinical outcomes of fixed dental prostheses with zirconia frameworks. Int J Comput Dent 14:183–202
Raigrodski AJ, Chiche GJ, Potiket N, Hochstedler JL, Mohamed SE, Billiot S et al (2006) The efficacy of posterior three-unit zirconium-oxide-based ceramic fixed partial dental prostheses: a prospective clinical pilot study. J Prosthet Dent 96:237–244
Larsson C, Wennerberg A (2014) The clinical success of zirconia-based crowns: a systematic review. Int J Prosthodont 27:33–43
Takeichi T, Katsoulis J, Blatz MB (2013) Clinical outcome of single porcelain-fused-to-zirconium dioxide crowns: a systematic review. J Prosthet Dent 110:455–461
Heintze SD, Rousson V (2010) Survival of zirconia- and metal-supported fixed dental prostheses: a systematic review. Int J Prosthodont 23:493–502
Jung RE, Zembic A, Pjetursson BE, Zwahlen M, Thoma DS (2012) Systematic review of the survival rate and the incidence of biological, technical, and aesthetic complications of single crowns on implants reported in longitudinal studies with a mean follow-up of 5 years. Clin Oral Implants Res 23(Suppl 6):2–21
Vigolo P, Mutinelli S (2012) Evaluation of zirconium-oxide-based ceramic single-unit posterior fixed dental prostheses (FDPs) generated with two CAD/CAM systems compared to porcelain-fused-to-metal single-unit posterior FDPs: a 5-year clinical prospective study. J Prosthodont 21:265–269
Rosentritt M, Steiger D, Behr M, Handel G, Kolbeck C (2009) Influence of substructure design and spacer settings on the in vitro performance of molar zirconia crowns. J Dent 37:978–983
Swain MV (2009) Unstable cracking (chipping) of veneering porcelain on all-ceramic dental crowns and fixed partial dentures. Acta Biomater 5:1668–1677
Christensen RP, Ploeger BJ (2010) A clinical comparison of zirconia, metal and alumina fixed-prosthesis frameworks veneered with layered or pressed ceramic: a three-year report. J Am Dent Assoc 141:1317–1329
California Dental Association (1977) Quality evaluation for dental care. Guidelines for assessment of clinical quality and professional performance. California Dental Association, Los Angeles
Loe H (1967) The gingival index, the plaque index and the retention index systems. J Periodontol 38(Suppl):610–616
Esposito M, Hirsch JM, Lekholm U, Thomsen P (1997) Failure patterns of four osseointegrated oral implant systems. J Mater Sci Mater Med 8:843–847
Groten M, Huttig F (2010) The performance of zirconium dioxide crowns: a clinical follow-up. Int J Prosthodont 23:429–431
Rinke S, Schafer S, Roediger M (2011) Complication rate of molar crowns: a practice-based clinical evaluation. Int J Comput Dent 14:203–218
Salinas T, Eckert S (2012) Implant-supported single crowns predictably survive to five years with limited complications. J Evid Based Dent Pract 12:213–214
Pjetursson BE, Bragger U, Lang NP, Zwahlen M (2007) Comparison of survival and complication rates of tooth-supported fixed dental prostheses (FDPs) and implant-supported FDPs and single crowns (SCs). Clin Oral Implants Res 18(Suppl 3):97–113
Guess PC, Att W, Strub JR (2012) Zirconia in fixed implant prosthodontics. Clin Implant Dent Relat Res 14:633–645
Nothdurft F, Pospiech P (2010) Prefabricated zirconium dioxide implant abutments for single-tooth replacement in the posterior region: evaluation of peri-implant tissues and superstructures after 12 months of function. Clin Oral Implants Res 21:857–865
Schwarz S, Schroder C, Hassel A, Bomicke W, Rammelsberg P (2012) Survival and chipping of zirconia-based and metal-ceramic implant-supported single crowns. Clin Implant Dent Relat Res 14(Suppl 1):e119–e125
Blatz MB, Bergler M, Ozer F, Holst S, Phark JH, Chiche GJ (2010) Bond strength of different veneering ceramics to zirconia and their susceptibility to thermocycling. Am J Dent 23:213–216
Shahin R, Kern M (2010) Effect of air-abrasion on the retention of zirconia ceramic crowns luted with different cements before and after artificial aging. Dent Mater 26:922–928
Nejatidanesh F, Savabi O, Shahtoosi M (2013) Retention of implant-supported zirconium oxide ceramic restorations using different luting agents. Clin Oral Implants Res 24(Suppl A100):20–24
Nejatidanesh F, Savabi O, Jabbari E (2014) Effect of surface treatment on the retention of implant-supported zirconia restorations over short abutments. J Prosthet Dent 112:38–44
Pjetursson BE, Sailer I, Zwahlen M, Hammerle CH (2007) A systematic review of the survival and complication rates of all-ceramic and metal-ceramic reconstructions after an observation period of at least 3 years. Part I: single crowns. Clin Oral Implants Res 18(Suppl 3):73–85
Vult von Steyern P, Carlson P, Nilner K (2005) All-ceramic fixed partial dentures designed according to the DC-Zirkon technique. A 2-year clinical study. J Oral Rehabil 32:180–187
Tinschert J, Schulze KA, Natt G, Latzke P, Heussen N, Spiekermann H (2008) Clinical behavior of zirconia-based fixed partial dentures made of DC-Zirkon: 3-year results. Int J Prosthodont 21:217–222
Molin MK, Karlsson SL (2008) Five-year clinical prospective evaluation of zirconia-based Denzir 3-unit FPDs. Int J Prosthodont 21:223–227
Beuer F, Edelhoff D, Gernet W, Sorensen JA (2009) Three-year clinical prospective evaluation of zirconia-based posterior fixed dental prostheses (FDPs). Clin Oral Investig 13:445–451
Acknowledgments
This study was approved by the Ethics Committee of Isfahan University of Medical Sciences and supported by Isfahan University of Medical Sciences (research grant # 391045) and based on a thesis submitted to the postgraduate school of Isfahan University of Medical Sciences in partial fulfillment of the requirement for the Master of Science Degree.
Author information
Authors and Affiliations
Corresponding author
Additional information
This study was presented as a poster presentation in ITI World Symposium 2014 Geneva.
Rights and permissions
About this article
Cite this article
Nejatidanesh, F., Moradpoor, H. & Savabi, O. Clinical outcomes of zirconia-based implant- and tooth-supported single crowns. Clin Oral Invest 20, 169–178 (2016). https://doi.org/10.1007/s00784-015-1479-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-015-1479-3