Abstract
The purpose of this in vitro study was to evaluate the effect of endodontic treatment with or without fiber-post restorations on the fracture strength of abutment teeth under fixed partial dentures (FPDs). Seventy extracted premolar and canine teeth were used. Groups of fiber-post-retained and root-filled teeth were endodontically treated. The teeth were embedded in an acrylic resin perpendicular to the horizontal plane to create fixed partial dentures. The following groups were created using different abutments: (1) sound (S) canine/S premolar, (2) S canine/endodontically treated (ET) premolar, (3) ET canine/S premolar, (4) ET canine/ET premolar, (5) S canine/fiber-post-restored (FPR) premolar, (6) FPR canine/S premolar, and (7) FPR canine/FPR premolar. Each tooth was prepared for a complete-coverage full-metal crown. Impressions were taken; metal frameworks were fabricated and cemented. The samples were exposed to 5,000 cycles of thermomechanical fatigue and loaded compressively until fracture (2 mm/min). The data were statistically analyzed using (Kruskal–Wallis test, α = 0.05). No significant difference was found among the mean fracture strengths of the groups (p = 0.696). There were distinct differences in failure patterns. All of the fracture types were horizontal, and neither vertical nor non-restorable root fractures were recorded. Premolars seemed to be a critical abutment compared to canines when they were sound under FPDs. The percentage of cervical fractures was high in endodontically treated teeth when compared to post-retained groups. In case of post-debonding, the abutment fracture did not occur. When root-filled teeth are used as abutments for FPDs, fiber-post restorations or the creation of abutments from similar structures (ET/ET or FPR/FPR) results in improved conservation of root structure under loading when compared to the abutments from different structures (S/ET, ET/S, FPR/S, S/FPR).
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The restoration of severely damaged coronal hard tissue and endodontically treated teeth (ETT) is always a challenge in reconstructive dentistry [1]. For many decades, full-coverage restorations were the only possible treatment options to overcome the assumed brittleness and the structural weakness of ETT. Improved restorative adhesive bonding techniques and materials have led some researchers to suggest that ETT can be restored in a more conservative manner than was previously considered appropriate. Recently, several restorative options have been used, such as adhesive-bonded composite restorations and fiber-reinforced composite (FRC) posts [2–5] in combination with resin cores [6], all of which have proven clinically successful [7, 8].
ETT (with or without a post) are sometimes used as abutments for fixed and removable prostheses. This situation is complex because fixed partial dentures (FPDs) can be short span, long span, or cantilevered and can be made with rigid or nonrigid connectors [9]. Sorensen and Martinoff reported a lower success rate for ETT serving as FPD abutments for 1 to 25 years when compared to single crowns [10]. The lives of ETT are shortened when functioning as an abutment for FPDs [11]. According to a review [9], ETT should be used with caution because higher failure rates can be expected when compared to those with vital abutments.
A post is sometimes required for the restoration of ETT as a result of extensive loss of natural tooth structure. Posts have often been described as a necessity to retain coronal build-up materials, as opposed to simply reinforcing ETT. Abutment teeth are subject to large horizontal and torquing forces during function, such as in FPDs and removable partial dentures, in which the abutment teeth are at higher risk for fracture [12]. Consequently, it can be speculated that posts that are bonded adhesively to the tooth structure enable active transmission of the applied load [13]. When used as crown abutments, ETT without posts perform comparably or better than those restored with post and core [14, 15].
To our current knowledge, there is still no general agreement regarding the behavior of ETT when used as abutments for FPDs. Therefore, the purpose of this study is to compare the fracture strengths failure patterns of different abutments (ETT and post core-retained ETT) for FPDs. The hypothesis tested was ETT (with or without post) would have an effect on fracture resistance and type of fracture when used as abutments for FPDs.
Materials and methods
Seventy extracted and caries-free human maxillary canines and second premolars with similar dimensions (7.56 ± 0.51 mm mesiodistally, 8.43 ± 0.56 mm bucco-lingually for canines; 6.79 ± 0.63 mm mesiodistally, 8.21 ± 0.73 mm bucco-lingually for maxillary second premolars) and similar root lengths (17.40 ± 1.83 mm for canines, 15.19 ± 1.59 mm for maxillary second premolars) were selected. The measurements were made beginning 1 mm from the cemento-enamel junction (CEJ) and from the apex to the CEJ after cleaning the root surfaces with a periodontal scaler. The teeth were divided into seven groups according to the abutment teeth to create the following groups (n = 10): group 1, sound (S) canine/S premolar; group 2, S canine/endodontically treated (ET) premolar; group 3, ET canine/S premolar; group 4, ET canine/ET premolar; group 5, S canine/fiber-post-retained (FPR) premolar; group 6, FPR canine/S premolar; and group 7, FPR canine/FPR premolar.
A statistical analysis was performed to confirm the standardization of the mesio-distal, bucco-lingual, and cervico-apical dimensions of the teeth in each group. No statistically significant difference was found in the mesio-distal dimension of canines (p = 0.549), bucco-lingual dimension of canines (p = 0.51), cervico-apical dimension of canines (p = 0.359), mesio-distal dimension of maxillary premolars (p = 0.92), bucco-lingual dimension of maxillary premolars (p = 0.987), or cervico-apical dimension of maxillary premolars (p = 0.669). The roots were covered with polyvinyl siloxane (Anti-Rutsch-Lack; Wenko-Wenselaar, Hilden, Germany) to simulate the periodontal membrane [16]. The teeth were then embedded in specimen holders perpendicular to the horizontal plane using an autopolymerizing acrylic resin (Technovit 4,000; Heraeus Kulzer, Wehrheim, Germany). To simulate the biologic width, the resin was extended to 2 mm below the CEJ.
The teeth in groups 2 to 7 were endodontically treated. Standard access cavities were made, and the canals were prepared to within 1 mm of the radiographic apex using a conventional step-back technique with an International Standardization Organization (ISO) file #35 (Dentsply Maillefer) at the apex. The canals were irrigated with 2 ml of 2.5% sodium hypochlorite solution throughout the preparation and dried with paper points (Sure-endo, Gyeonngi-do, South Korea). Each canal was obturated using a lateral condensation technique with an ISO 35 primary gutta-percha master cone (DiaDent, South Korea), gutta-percha points (DiaDent, South Korea), and root canal sealer (AH Plus, Dentsply). The access cavities in groups 2 to 4 were then filled with composite resin (Clearfil AP-X, Kuraray, Japan) in combination with a self-etch adhesive (Clearfil SE Bond, Kuraray, Japan) and cured using a light-curing unit with an intensity of minimum 700 mW/cm2 (Bluephase, Ivoclar Vivadent, MV).
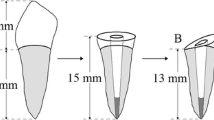
In groups 5 to 7, the crowns of the teeth were reduced under water cooling to create a 2-mm-high by 1-mm-thick ferrule. Post preparations were made with a #5 reamer (Largo; Dentsply Maillefer), keeping a minimum of 4 mm of root canal filling at the apex. The post spaces were cleaned with alcohol, and parallel-sided fiber posts with retentive grooves (Reforpost, Angelus, Londriana, Parana, BR) with a diameter of 1.5 mm were luted using a dual-curable resin cement (Clearfil SA cement, Kuraray, Tokyo, Japan) according to the directions of the manufacturer. Since this cement is a self-adhesive luting material, no additional root surface treatment was done. The length of the posts inside the roots was 13 mm for canines, 11 mm for premolars, and 3 mm for core structures. Four-millimeter-high core buildups were created using Clearfil DC Core Automix (Kuraray, Japan).
Each tooth was prepared for a complete-coverage full-metal FPD using a silicone index. An occlusal reduction of 1.8 to 2.0 mm was prepared, followed by a circular 1.2-mm-wide accentuated chamfer preparation using a diamond bur (Mani, Tochigi, Japan). The final preparation resulted in a taper of 4° to 6° and an approximate abutment height of 4.5 mm. All sharp line angles were rounded, and all margins were finished 0.5 mm apical to the CEJ using fine diamond burs ((Mani, Tochigi, Japan). Impressions of the prepared abutments were made using a putty-wash technique. A vinyl polysiloxane impression material (Monopren; Kettenbach, Eschenburg, Germany) was syringed around the abutments, and putty material (Twinduo; Picodent, Wipperfurth, Germany) was used in the custom-made impression tray. Dies were fabricated using dental stone (Fujirock II; GC Europe, Leuven, Belgium). The metal frameworks were fabricated. Each core had a thickness of 0.5 mm, except at the occlusal surface, where the core material was 0.7 mm thick. After verification of the framework dimensions with a caliper (SU metal caliper; SchulerDental, Ulm, Germany), a FPD was performed. The intaglio surfaces of the FPDs were airborne-particle abraded with 50 mm Al2O3 particles at an air pressure of 2.5 bar and cleaned ultrasonically in 96% isopropyl alcohol. All FPDs were cemented using zinc phosphate cement (Harvard Dental, Berlin, Germany). During the cementation, the crowns were secured in place with finger pressure for 5 min. All specimens were stored in 100% humid conditions for 24 h and then exposed to 5,000 cycles of thermal fatigue before testing (5°C to 55°C, with a 10-s dwelling time).
Each FPD was positioned in a universal testing machine (Instron, Canton, MA, USA) so that the steel sphere with a 4-mm-diameter ball contacted the two cuspal inclines of the pontic simultaneously and loaded until fracture (2 mm/min). The load necessary to fracture each FPD was recorded as newtons (N). The test of homogeneity of variance significance was p = 0.05. Therefore, the data were statistically analyzed using the Kruskal–Wallis test (α = 0.05). The fracture patterns of FPDs and abutment teeth were classified after the fracture test as follows:
-
Type 1
Horizontal cervical root fracture of canine/no fracture for premolar
-
Type 2
No fracture of canine/horizontal cervical root fracture of premolar (Fig. 1)
-
Type 3
Horizontal cervical root fracture of canine and premolar (Fig. 2)
-
Type 4
Vertical root fracture of one or two abutments
-
Type 5
Horizontal and vertical root fractures of one or two abutments
Results
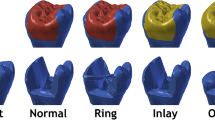
The fracture strength values (median, maximum, minimum) and fracture modes are given in Tables 1 and 2. Figure 3 represents box plots for fracture strength values. No statistically significant difference was found among the test groups using the Kruskal–Wallis test (p = 0.696). Due to the large variation of our data, the power was only 0.29. Table 2 shows the failure patterns of the tested samples. All of the fracture types were horizontal, and no vertical root fractures were recorded. In group 1, teeth showed 50% type 2 fractures, while 50% were type 3 fractures; 90% of the teeth in group 2 showed type 3 fractures. In group 3, 100% of the abutments showed type 3 failure patterns. In group 4, 70% showed type 3 fractures, while group 5 showed mostly (60%) type 3 failures. In group 6, 80% showed type 3 failures. Finally, in group 7, 40% showed type 3 failures. Figures 1 and 2 show that sound and ETT abutment fracture lines are horizontal and placed below the ferrule structure. All of the post-restored groups showed debonded failure of the FRC post after the test. Figure 4 shows that in case of post-debonding, the abutment fracture does not occur.
Discussion
In the present study, the use of ETT and/or FPR-ETT as abutments for FPDs was evaluated. To avoid unexpected failure of ceramic and to facilitate easy observation of the damaging effects on the abutments, the FPDs were fabricated with Ni–Cr alloy; Ni–Cr has a high modulus of elasticity that transfers stress to the restoring systems, resulting in a more damaging effect [17]. The incorporation of a ferrule is reported to be an important factor when using a post core [18, 19], and it enhances fracture resistance [20, 21]. A 2-mm-high [22] and 1-mm-thick ferrule is created in the post groups.
The resulting data partly support the hypothesis. No significant difference was found among the mean fracture strength values of the test groups (p > 0.05); however, the fracture patterns after failure were different in all of the groups. The failure modes showed 100% failure of the sound premolars in the first group. The higher failure rates of premolars were previously explained by their smaller sizes and, therefore, lower fracture strengths [23]. According to the results of this study, premolars seem to be a critical abutment when compared to the canines if they kept sound under FPDs (group 1).
The loss of structural tooth integrity associated with endodontic access preparation is reported as a possible factor for the higher occurrence of fractures in ETT [24]. Irrigation solutions have adverse effects on the physical properties of root canal dentin, which might increase the risk for root fractures [25–27]. Various obturation materials and obturation techniques are reported to have different effects on fracture strengths of teeth [12]. All of these studies indicate that root canal treatment has an effect on the fracture strength of teeth. Wu et al. compared mandibular premolars and canines and reported that the force required to fracture the instrumented premolars was 30% lower than that required to fracture their non-instrumented counterparts, whereas the force required for the instrumented canines was 2% lower than for their non-instrumented counterparts [28]. In the present study, although there was no significant difference among the mean fracture strength values, the fracture pattern analysis showed that endodontic treatment has an effect on fracture lines. If one of the abutments was root-filled (groups 2 and 3), the number of cervical fractures increased (Table 1). Group 2 had an interesting finding in which 90% of the abutments had cervical failure. Considering the sudden drop in the recorded applied load, we speculate that, in these samples, root-filled premolars might have broken first and were then followed by the sound canines. High torque due to the FPD might have caused failure of the sound canines [12]. It is possible to observe which abutment was broken first using a high-speed video recorder [29]; however, in this study, the fracture strength values and the fracture pattern of the test samples could be evaluated at the end of every test ending in failure. Therefore, these details were not evaluated. Further studies can be performed to evaluate behaviors of abutments individually using a high-speed video recorder.
The 100% failure rate in both abutments recorded in the third group shows that root canal treatment reduced the strength of the canines. When the two abutments were root-filled (group 4), the number of cervical fractures was decreased, showing that homogeneity among the abutments results in stress that can be forwarded toward the abutments homogenously. Stress concentrates where non-homogeneous material distributions are present, just like interfaces. Interfaces of materials with different moduli of elasticity represent the weak link of restorative systems, as the toughness/stiffness mismatch influences the stress distribution [30–32].
Fiber-reinforced composite (FRC) posts helped to improve stress distribution because of their elastic moduli being similar to that of dentin [33–36]. Recent studies suggest that FRC posts also contribute to the reinforcement and strengthening of endodontically treated teeth under full-coverage crown restorations [4, 37]. In the present study, all of the post-restored groups showed debonding failure of the FRC post after the test (Fig. 3), confirming the results of previous studies indicating that the weakest point in adhesively cemented post core restorations is the interface between the post and the resin-based cement [34, 38, 39]. When the fracture modes in the post groups were evaluated, neither vertical nor non-restorable fracture patterns were observed. When both abutments were treated with a fiber post, the distribution of the cervical fractures was homogenous among the abutments (30% canines, 30% premolars, and 40% both), and the percentage of the cervical fractures of the two abutments was decreased to the same as in the ETT group. When one of the abutment teeth was restored with a fiber post, the percentage of failure of the two abutments increased at the same time. Post restoration of either canine or premolar also changed the failure modes. When the canine was restored with a post, the fracture rate was 50%, which is lower than that of the sound canine. Post restoration of the premolar also decreased the percentage of cervical fractures within premolars (from 60% to 50%). The results of this study showed that post restoration of the abutment teeth changes the fracture pattern and seems to have a positive effect on premolars. Normally, the use of an adhesive post can contribute to the reinforcement of the tooth by changing the distribution of the stresses along the roots under loading [40] and can be protective for the remaining tooth structure [41]. The results of the in vitro study discussed in this paper confirm these previous studies.
Posts can reduce maximal dentin stress by as much as 20% when the teeth are loaded vertically [42]. However, teeth in a natural, oral environment will be exposed to more than just vertical forces; therefore, the functional and para-functional forces must be applied to estimate the prognosis of the tooth [43]. Schmitter et al. [44] demonstrated that different loading vectors of the glass fiber-reinforced posts can influence the fracture strength. Fracture resistance of non-vital teeth depends on the angle of the applied load, with axial forces being less detrimental than oblique forces [45, 46]. Clinically, anterior teeth are placed at an angle to the occlusal plane; consequently, the forces are not directed along their long axes [47]. In the present study, to provide a detailed examination of the destructive effect of FPDs on abutment teeth, the pontics of the FPDs were loaded to simulate a three-bending effect, although this kind of loading does not completely simulate the clinical conditions.
In in vitro studies, it is difficult to achieve standardization with regard to functional age of teeth, morphologic variations of the pulp, and abnormalities in dentin composition before extraction [48, 49]. Although the variations were tried to be controlled in this study (the teeth were carefully selected, the dimensions were measured, the teeth were distributed into the subgroups according to their measured dimensions, etc.) because of the uncontrolled variations listed above, the fracture strength values might have been affected. This is one of the limitations of this in vitro study.
Conclusions
Within the limitations of this in vitro study, it was concluded that when ET teeth are used as abutments for FPDs subject to loading, fiber-post restoration of the abutment tooth or the creation of abutments from similar structures (ET/ET or FPR/FPR) results in improved conservation of root structure.
References
Chang CY, Kuo JS, Lin YS, Chang YH (2009) Fracture resistance and failure modes of CEREC endo-crowns and conventional post and core-supported CEREC crowns. J Dent Sci 4:110–117
Fokkinga WA, Kreulen CM, Vallittu PK, Creugers NH (2004) A structured analysis of in vitro failure loads and failure modes of fiber, metal, and ceramic post-and-core systems. Int J Prosthodont 17:476–482
Rosentritt M, Sikora M, Behr M, Handel G (2004) In vitro fracture resistance and marginal adaptation of metallic and tooth-coloured post systems. J Oral Rehabil 31:675–681
Salameh Z, Sorrentino R, Ounsi HF, Goracci C, Tashkandi E, Tay FR, Ferrari M (2007) Effect of different all-ceramic crown system on fracture resistance and failure pattern of endodontically treated maxillary premolars restored with and without glass fiber posts. J Endod 33:848–851
Goncalves LA, Vansan LP, Paulino SM, Sousa Neto MD (2006) Fracture resistance of weakened roots restored with a transilluminating post and adhesive restorative materials. J Prosthet Dent 96:339–344
Dietschi D, Duc O, Krejci I, Sadan A (2008) Biomechanical considerations for the restoration of endodontically treated teeth: a systematic review of the literature, part II (evaluation of fatigue behavior, interfaces, and in vivo studies). Quintessence Int 39:117–129
D’Arcangelo C, De Angelis F, Vadini M, Zazzeroni S, Ciampoli C, D’Amario M (2008) In vitro fracture resistance and deflection of pulpless teeth restored with fiber posts and prepared for veneers. J Endod 34:838–841
Ellis SG, Macfarlane TV, McCord JF (1999) Influence of patient age on the nature of tooth fracture. J Prosthet Dent 82:226–230
Goga R, Purton DG (2007) The use of endodontically treated teeth as abutments for crowns, fixed partial dentures, or removable partial dentures: a literature review. Quintessence Int 38:41–46
Sorensen JA, Martinoff JT (1985) Endodontically treated teeth as abutments. J Prosthet Dent 53:631–636
Caplan DJ, Weintraub JA (1997) Factors related to loss of root canal filled teeth. J Public Health Dent 57:31–39
Tang W, Wu Y, Smales RJ (2010) Identifying and reducing risks for potential fractures in endodontically treated teeth. J Endod 36:609–617
Sorrentino R, Aversa R, Ferro V, Auriemma T, Zarone F, Ferrari M, Apicella A (2007) Three-dimensional finite element analysis of strain and stress distributions in endodontically treated maxillary central incisors restored with different post, core and crown materials. Dent Mater 23:983–993
Assif D, Bitenski A, Pilo R, Oren E (1993) Effect of post design on resistance to fracture of endodontically treated teeth with complete crowns. J Prosthet Dent 69:36–40
Sidoli GE, King PA, Setchell DJ (1997) An in vitro evaluation of a carbon fiber-based post and core system. J Prosthet Dent 78:5–9
Soares CJ, Pizi EC, Fonseca RB, Martins LR (2005) Influence of root embedment material and periodontal ligament simulation on fracture resistance tests. Braz Oral Res 19:11–16
Arunpraditkul S, Saengsanon S, Pakviwat W (2009) Fracture resistance of endodontically treated teeth: three walls versus four walls of remaining coronal tooth structure. J Prosthodont 18:49–53
Gegauff AG (2000) Effect of crown lengthening and ferrule placement on static load failure of cemented cast post-cores and crowns. J Prosthet Dent 84:169–179
Pereira JR, de Ornelas F, Conti PC, do Valle AL (2006) Effect of a crown ferrule on the fracture resistance of endodontically treated teeth restored with prefabricated posts. J Prosthet Dent 95:50–54
Rosen H, Patida-Rivera M (1986) Iatrogenic fracture of roots reinforced with a cervical collar. Oper Dent 11:46–50
Barkhordar RA, Radke R, Abbasi J (1989) Effect of metal collars on resistance of endodontically treated teeth to root fracture. J Prosthet Dent 61:676–678
Naumann M, Sterzenbach G, Rosentritt M, Beuer F, Frankenberger R (2008) Is adhesive cementation of endodontic posts necessary? J Endod 34:1006–1010
Wegner PK, Freitag S, Kern M (2006) Survival rate of endodontically treated teeth with posts after prosthetic restoration. J Endod 32:928–931
Zhi-Yue L, Yu-Xing Z (2003) Effect of post-core design and ferrule on fracture resistance of endodontically-treated maxillary central incisors. J Prosthet Dent 89:368–373
Saleh AA, Ettman WM (1999) Effect of endodontic irrigation solutions on microhardness of root canal dentine. J Dent 27:43–46
Grigoratos D, Knowles J, Ng YL et al (2001) Effect of exposing dentine to sodium hypochlorite and calcium hydroxide on its flexural strength and elastic modulus. Int Endod J 34:113–119
Yasuda G, Inage H, Kawamoto R, Shimamura Y, Takubo C, Tamura Y, Koga K, Miyazaki M (2008) Changes in elastic modulus of adhesive and adhesive-infiltrated dentin during storage in water. J Oral Sci 50:481–486
Wu MK, van der Sluis LW, Wesselink PR (2004) Comparison of mandibular premolars and canines with respect to their resistance to vertical root fracture. J Dent 32:265–268
Olson J (2007) Fracture aperture, length and pattern geometry development under biaxial loading: a numerical study with applications to natural, cross-jointed systems. In the relationship between damage and localization. Geol Soc Lond 289:123–142
Otto T (2004) Computer-aided direct all-ceramic crowns: preliminary 1-year results of a prospective clinical study. Int J Periodontics Restorative Dent 24:446–455
Ausiello P, Gee AJ, Rengo S, Davidson CL (1997) Fracture resistance of endodontically treated premolars adhesively restored. Am J Dent 10:237–241
Assif D, Gorfil C (1994) Biomechanical considerations in restoring endodontically treated teeth. J Prosthet Dent 71:565–567
Ferrari M, Vicchi A, Manocci F, Mason PN (2000) Retrospective study of the clinical performance of fiber posts. Am J Dent 13:9B–13B
Cagidiaco MC, Radovic I, Simonetti M, Tay F, Ferrari M (2007) Clinical performance of fiber post restorations in endodontically treated teeth: 2-year results. Int J Prosthodont 20:293–298
Monticelli F, Goracci C, Ferrari M (2004) Micromorphology of the fiber post-resin core unit: a scanning electron microscopy evaluation. Dent Mater 20:176–183
Akkayan B, Gulmetz T (2002) Resistance to fracture of endodontically treated teeth restored with different post systems. J Prosthet Dent 87:431–437
Akkayan B, Caniklioglu B (1998) Resistance to fracture of crowned teeth restored with different post systems. Eur J Prosthodont Restor Dent 6:13–18
Ferrari M, Cagidiaco MC, Grandini S, De Sanctis M, Goracci C (2007) Post placement affects survival of endodontically treated premolars. J Dent Res 86:729–734
Monticelli F, Grandini S, Goracci C, Ferrari M (2003) Clinical behavior of translucent-fiber posts: a 2-year prospective study. Int J Prosthodont 16:593–596
Saupe WA, Gluskin AH, Radke RA Jr (1996) A comparative study of fracture resistance between morphologic dowel and cores and a resin-reinforced dowel system in the intraradicular restoration of structurally compromised roots. Quintessence Int 27:483–491
Newman MP, Yaman P, Dennison J, Rafter M, Billy E (2003) Fracture resistance of endodontically treated teeth restored with composite posts. J Prosthet Dent 89:360–367
Ko CC, Chu CS, Chung KH, Lee MC (1992) Effects of posts on dentin stress distribution in pulpless teeth. J Prosthet Dent 68:621–627
Fernandes AS, Dessa GS (2001) Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont 14:355–363
Schmitter M, Huy C, Ohlmann B, Gabbert O, Gilde H, Rammelsberg P (2006) Fracture resistance of upper and lower incisors restored with glass fiber reinforced posts. J Endod 32:328–330
Loney RW, Moulding MB, Ritsco RG (1995) The effect of a load angulation on fracture resistance of teeth restored with cast post and cores and crowns. Int J Prosthodont 8:247–251
Krejci I, Duc O, Dietschi D, de Campos E (2003) Marginal adaptation, retention and fracture resistance of adhesive composite restorations on devital teeth with and without posts. Oper Dent 28:127–135
Mentink AG, Meeuwissen R, Kayser AF, Mulder J (1993) Survival rate and failure characteristics of the all metal post and core restoration. J Oral Rehabil 20:455–461
Fernandes AS, Dessai GS (2001) Factors affecting the fracture resistance of post-core reconstructed teeth: a review. Int J Prosthodont 14(4):355–363
Massa F, Dias C, Blos CE (2010) Resistance to fracture of mandibular premolars restored using post and core systems. Quint Int 41:49–57
Conflict of interest
This study is funded by the Research Projects Council of University of Selcuk. The authors declare that they have no financial, professional, or other personal interest that could influence the position presented in the paper.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Akman, S., Akman, M., Eskitaşcıoğlu, G. et al. The use of endodontically treated and/or fiber post-retained teeth as abutments for fixed partial dentures. Clin Oral Invest 16, 1485–1491 (2012). https://doi.org/10.1007/s00784-011-0635-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-011-0635-7