Abstract
The availability of cone beam computed tomography (CBCT) and the numbers of CBCT scans rise constantly, increasing the radiation burden to the patient. A growing discussion is noticeable if a CBCT scan prior to the surgical removal of wisdom teeth may be indicated. We aimed to confirm non-inferiority with respect to damage of the inferior alveolar nerve in patients diagnosed by panoramic radiography compared to CBCT in a prospective randomized controlled multicentre trial. Sample size (number of required third molar removals) was calculated for the study and control groups as 183,474 comparing temporary and 649,036 comparing permanent neurosensory disturbances of the inferior alveolar nerve. Modifying parameter values resulted in sample sizes ranging from 39,584 to 245,724 respectively 140,024 to 869,250. To conduct a clinical study to prove a potential benefit from CBCT scans prior to surgical removal of lower wisdom teeth with respect to the most important parameter, i.e., nerval damage, is almost impossible due to the very large sample sizes required. This fact vice versa indicates that CBCT scans should only be performed in high risk wisdom tooth removals.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The ever increasing interest in 3D visualization and diagnostics concerns all medical fields and specialities. In oral and maxillofacial surgery, cone beam computed tomography (CBCT) in recent years has replaced classical computed tomography (CT) for typical hard-tissue diagnostics such as impacted teeth. Of course, with the increasing availability of this 3D technique, the numbers of CBCT scans rise constantly. However, every CBCT scan that replaces a panoramic radiograph, or is coming on top of that, considerably increases the radiation burden to the patient [1–5]. It would be interesting if the benefit from using 3D diagnostics will indeed outweigh the risk associated with the higher radiation dose, respecting the as low as reasonably achievable (ALARA) principle [6, 7]. Even more so, a quite inevitable side effect of the spread of CBCT machines will be a more frequent use of these techniques for various types of diagnostic questions. Accompanying this more frequent application, claims postulating CBCT as standard technology for certain medical or dental procedures will also occur more frequently. Such a standard procedure may be the removal of mandibular wisdom teeth. Indeed, a growing discussion among experts is noticeable whether a CBCT scan prior to the surgical removal may be indicated. On the other hand, modern medicine no longer believes in expert opinion; rather, it relies on “evidence” gained from studies following a highly reproducible, standardized design with low or moderate bias.
This discussion brought up the idea to initiate a prospective multicentric clinical study to investigate the potential benefit resulting from presurgical 3D visualization and planning on the outcome of the surgery. Since nerve damage is a good measure for complications, our initial approach had been to quantify a potential difference in the appearance of nerve injuries after the removal of lower third molars using 2D panoramic radiography and the 3D CBCT as presurgical diagnostics.
The injury of the inferior alveolar nerve (IAN) and the lingual nerve (LN) are typical risks and most frequent severe complications in the lower third molar (M3) removal; likewise, M3 extraction is the most frequent reason for IAN and LN injury [8–11]. The incidence reported in the literature is ranging from 0.35% [12] to 8% [13] for temporary and from 0% [14, 15] to 1% [16] for permanent IAN injury and from 0% [17] to 11% [18] for temporary and from 0% [15, 19] to 1.1% [20] for permanent LN injury [21–32]. When related to the number of cases (see Table 1), average probabilities of IAN injury of 1.85% (temporary) and 0.53% (permanent) and LN injury of 2.82% (temporary) and 0.46% (permanent) occur. The higher amount of temporary LN injuries is due to the inclusion of studies where the lingual flap technique is used. This technique increases the amount of LN disturbances extremely [9, 33, 34]. When excluding these studies, the figures for a temporary LN disturbance are 1.52% for a temporary and 0.44% for a permanent damage.
The LN traverses the region lingually completely through soft tissues and thus is not visible in either radiographic technique [35]. Hence, the IAN only could present a meaningful measure for comparison of both methods. Commonly, the bony canal is likely to be visualized in both imaging techniques.
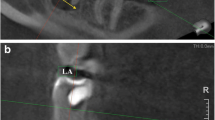
The anatomic relationship between IAN and M3 is one of the most important information to be obtained during the presurgical evaluation.
In the literature, 2D radiographic risk factors for a neurosensory disturbance of the IAN after surgical removal of M3 are specified, such as darkening of the root, diversion of the inferior alveolar canal, and interruption of the cortical white line, indicating a close relationship between tooth and IAN [36–44].
Clinically, the risk of IAN injury correlates with the exposure of the neurovascular bundle in the operation situs [32, 45–48]. When there is a close relationship between the mandibular canal and the wisdom tooth, the incidence of a nerve injury increases extremely, with a reported incidence ranging between 20% and 60% of these cases [45, 48, 49].
In theory, CBCT should be superior in predicting the exposure, i.e. the contact between nerve and tooth, of the IAN compared to panoramic radiography. A possible absence of the cortical border of the canal can be determined more precisely having the third dimension [46, 50]. Obviously, having available the third dimension allows determining the position of the nerve canal relative to the tooth in all three dimensions. However, Gheaminia et al. [47] did not find a significant difference in the prediction of IAN exposure between CBCT and panoramic radiography. Moreover, several authors in general consider panoramic radiography as a useful tool to predict a contact between the third molar and the IAN [31, 42, 47, 51].
When considering all the arguments listed above, the question arises whether or not the presurgical imaging technique has an influence on the outcome of the study as assessed by an objective measure. Despite the belief of some authors that 3D diagnostic is able to reduce operating time and therefore postoperative complications, such as neurosensory disturbances, swelling, or alveolitis [52, 53], there is only low-level scientific evidence on the actual usefulness of different preoperative imaging techniques for the operative removal of wisdom teeth [49, 54]. In contrary, one study found no significant differences for postoperative complications between 3D and 2D presurgical diagnostics [11]. In intraoral radiography, the parallax technique is able to determine a lingual or buccal position of the IAN in relation to M3 [55, 56], as well as the PA cephalomatric radiography [57].
Apart from that, many studies observed a significant correlation of an IAN injury with the experience respectively skills of the operator [9, 17, 20, 24], the age of the patient [21, 23, 27, 30, 44], and the removal under general anaesthesia for LN injury [23] and for IAN and LN injury [30].
We found no published data revealing an evidence-based effectiveness of using preoperative 3D imaging on the degree of patient morbidity and the overall outcome of third molar surgery. It is unclear if the exact determination of the anatomical position of the IAN in relation to the M3 prior to surgery using 3D diagnostics is required for safe removal with a decrease in neurosensory disturbances.
We discussed how to address this open question in an adequate way. The trial design considerations comprising sample size calculations will be described in this article.
Our hypothesis was that panoramic radiography is not inferior compared to CBCT regarding the postsurgical neurosensory disturbances of the IAN. Testing the superiority of CBCT compared to panoramic radiography, which would also be a feasible way, could only present evidence if superiority is proven. However, if superiority of CBCT is not detected, this would not automatically prove the non-inferiority of panoramic radiography. For this reason, testing non-inferiority of panoramic radiography is the appropriate trial.
Materials and methods
Planned study design
The gold standard to compare treatments is the prospective randomized controlled trial (RCT). In this setting, a comparison of diagnostic imaging techniques with respect to their impact on surgical complications is aimed. The surgeon’s qualification may have a great impact on the risk of neurosensory disturbances, too. One challenge is therefore to distinguish the effects of the imaging technique and the surgical performance. As the surgical performance and other predictors for the risk of complications are expected to be on average similar between the study arms in a randomized controlled trial, an RCT is principally an adequate design.
In order to support external validity of study results, a multicentre approach was chosen [58].
Criteria for inclusion were patient age of 25 years or above, the operation difficulty, which has to be determined with the established Pederson Index, grades 4–10, and patients’ compliance [59–61]. Criteria for exclusion were germs, pregnancy, operation difficulty grade 3 of the Pederson Index, likelihood of an enlacement of the IAN nerve by the root(s), the existence of an external CBCT, and a presurgically existent neurosensory alteration. The surgeon should be experienced in removing lower third molars (a minimum of 150 removals required). The surgical procedure should be standardized by raising a buccal mucoperiostal flap. Bone removal and sectioning of the tooth should be performed when necessary. Possible study endpoints were the operation time (defined from raising the mucoperiostal flap until the finishing of the suture), with an expected average range from 8 to 15 min [62–64], and the percentage of neurosensory disturbances of the IAN. We considered the first postsurgical day to measure the neurosensory disturbance to also include short-term temporary disturbances. Since the LN traverses completely through soft tissues and is not visible in either radiographic technique, only the neurosensory disturbance of the IAN presents a meaningful measure for comparison of both methods and was therefore defined as the primary endpoint of the planned trial. We wanted to use an objective method, the sharp/blunt discrimination with a dental probe, to characterize neurosensory disturbance [65, 66]. As a secondary endpoint, we planned to consider the operation time as a continuous variable and indicator for overall operation difficulty.
Our hypothesis is that 2D imaging is not inferior to the 3D diagnostic with respect to the risk of temporary neurosensory disturbances of the IAN (primary endpoint). We decided to define a relative non-inferiority bound of 10% and so allowing the rate of nerve damage in the panoramic radiography group to be up to 10% higher relative to the CBCT group. Methodological and ethical considerations substantiate the need for a sample size calculation. If an assumed effect cannot be demonstrated within a study due to an insufficient number of patients, study participants would be exposed to unnecessary radiation. On the other hand, if an effect could have been demonstrated even with a lower number of patients, more patients than necessary have been exposed to the inferior treatment, and more time was needed to assess the question of interest [58, 67–69].
Sample size calculation
Basing on the in-depth analysis of data from the literature, we calculated the required sample sizes, i.e., the number of third molar removals, under the following assumptions:
Temporary neurosensory disturbance rates of the IAN are assumed to be 1.85% for both CBCT and panoramic radiography patients. A power of 80% is required and a one-sided type I error of 2.5% is allowed. For the panoramic radiography group, disturbance rates up to 10% higher relative to the CBCT group are considered non-inferior. Sample sizes should be equal in both trial arms.
To illustrate the effects of single parameters on required sample sizes, the relative non-inferiority margin and type I and II error were modified. Besides permanent neurosensory disturbance rates of the IAN were considered.
The same calculations were performed for permanent neurosensory disturbance rates assuming 0.53% for both CBCT and panoramic radiography.
Sample sizes were calculated by means of PASS 2002 (Number Cruncher Statistical Systems, Kaysville, UT, USA).
Results
The required sample size, i.e., the number of third molar removals, for temporary IAN injury is 183,474 under the assumptions considered most adequate (power 80%, type I error 2.5%, relative non-equivalence margin 10%). Modifying these parameters in different ways (power, 90%; type I error, 5%; relative non-equivalence margin, 20%) changes the required numbers of third molar removals considerably yielding a range from 39,584 to 245,724 (Table 2, Fig. 1). For the permanent IAN injury, the corresponding sample size was 649,036 ranging from 140,024 to 869,250 (Table 3, Fig. 2).
Discussion
The results of the sample size calculation show that proving non-inferiority of panoramic radiography compared to CBCT with respect to neurosensory disturbance rates would be a definite challenge. Huge sample sizes are mainly a consequence of the rare event rates in both trial arms. Many patients must be allocated to the trial until the first neurosensory disturbance is observed. To show that rare event rates do not diverge in terms of a relative difference definition, very precise estimates are necessary. For example, 10% relative difference implies 5% allowed absolute difference if event rates are assumed to be 50%. If the expected event rate is 1%, 0.1% is the maximum allowed absolute difference.
Even if it was possible to conduct the trial, it would be difficult to get robust estimates for the surgeon effects. Assuming an event rate of 1.85%, a surgeon would have to remove 54 third molars until the first neurosensory disturbance is expected to occur. Therefore, it would be desirable not to allow for too many participating surgeons, which would, on the other hand, limit external validity.
It should be noted that proving superiority of CBCT would require high sample sizes as well in this situation—for the same reasons as described above. The negative outcome of our initial approach also bears some significance for the question that was standing at the beginning of all planning: Is CBCT superior with respect to the (measurable) clinical outcome of lower third molar surgery? Consequently, the aim of this report was to provide some insight into the sample size necessary to answer this particular question and on the conclusions, which may be drawn from these purely theoretical considerations.
The injury of the IAN is a typical but rare complication of third molar surgery, particularly when a permanent disturbance is regarded. We do not believe that the low incidence of IAN and LN injury could be reduced using CBCT. The risk of damage is predetermined by the anatomy. When IAN penetrates through the root, 67% injuries occurred although CBCT was performed [70]. Panoramic radiography occasionally overestimates the risk of IAN injury compared with 3D imaging [48, 71].
M3 removal is recommended to be carried out until the 25th birthday to minimize postsurgical complications [72]; however, the sensitivity to radiation is significantly higher in younger ages [73]. Hence, for this age group, the ALARA principle should be followed with extra caution. No matter how low the dose, it is excessive if it is unlikely to improve the outcome of the treatment provided [6].
The effective doses (ICRP 2007) of the different imaging techniques are reported as follows: CBCT, 13–1,073 μSv [3, 5, 74]; Panoramic radiography, 8.6–24.3 μSv [4, 75, 76]; PA cephalometric radiography, 2.3–5.1 μSv [4, 77]; intraoral radiography, 0.3–5.5 μSv [4, 75]; and head CT, 470–4,000 μSv [73, 74, 76, 78] (Table 4).
In one study, the vertical position of the root tip relative to the mandibular canal could not be correctly determined in both CBCT and PA cephalometric radiography in combination with panoramic radiography for 1% of the cases [57]. The horizontal relation could not be identified exactly in 9.0% for panoramic radiography and PA cephalomatric radiography versus 2.8% for CBCT [57]. 3D diagnostics were not able to detect the relationship between IAN and M3 in every case of the investigation [48, 50, 57, 70]. Hence, CBCT does not guarantee for an exact 3D location of the IAN in relation to the M3.
The increasing information in CBCT datasets in comparison to panoramic radiographs is undisputed, but it cannot be an indication for its own sake because of the increasing radiation dose, yet without any proof of benefit for the patient. Removal of M3 seems to be a highly effective procedure when done by experienced surgeons, with a very low rate of permanent nerve injuries, even when using panoramic radiography as presurgical imaging technique. A use as routine diagnostic cannot be justified for CBCT because of the absence of evident benefit [7].
In conclusion, from our theoretical calculations based on data published in the literature, we cannot recommend CBCT scans prior to surgical removal of lower wisdom teeth. The major negative outcome, a (temporary or permanent) damage of the alveolar nerve, is such a rare event even when 2D imaging is the basis for the procedure, which the sample sizes required to prove a difference would be exceedingly large. The low rate of complications when experienced surgeons perform the surgery does not warrant the currently approximately tenfold radiation dose imposed by CBCT when compared to panoramic radiography. This is of particular importance, since the majority of patients with lower third molar surgery are under 25 years of age.
A remaining indication for CBCT are the so-called high risk extractions, for example, when the parallax technique and the PA cephalomatric radiography could not determine the location of the mandibular canal properly or an enlacement of the IAN nerve by the root(s) can be expected to be very likely.
References
Ludlow JB, Davies-Ludlow LE, Brooks SL (2003) Dosimetry of two extraoral direct digital imaging devices: NewTom cone beam CT and Orthophos Plus DS panoramic unit. Dentomaxillofac Radiol 32:229–234
Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB (2006) Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Radiol 35:219–226
Ludlow JB, Ivanovic M (2008) Comparative dosimetry of dental CBCT devices and 64-slice CT for oral and maxillofacial radiology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 106:106–114
Ludlow JB, Davies-Ludlow LE, White SC (2008) Patient risk related to common dental radiographic examinations: the impact of 2007 international commission on radiological protection recommendations regarding dose calculation. J Am Dent Assoc 139:1237–1243
Roberts JA, Drage NA, Davis J, Thomas DW (2009) Effective dose from cone beam CT examinations in dentistry. Br J Radiol 82:35–40
Farman AG (2005) ALARA still applies. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 100:395–397
Assael LA (2002) The presurgical workup: how much is enough? J Oral Maxillofac Surg 60:977–978
Hillerup S (2007) Iatrogenic injury to oral branches of the trigeminal nerve: records of 449 cases. Clin Oral Investig 11:133–142
Bataineh AB (2001) Sensory nerve impairment following mandibular third molar surgery. J Oral Maxillofac Surg 59:1012–1017
Carmichael FA, McGowan DA (1992) Incidences of nerve damage following third molar removal: a West of Scotland Oral Surgery Research Group study. Br J Oral Maxillofac Surg 30:78–82
Better H, Abramowitz I, Shlomi B, Kahn A, Levy Y, Shaham A, Chaushu G (2004) The presurgical workup before third molar surgery: how much is enough? J Oral Maxillofac Surg 62:689–692
Cheung LK, Leung YY, Chow LK, Wong MC, Chan EK, Fok YH (2010) Incidence of neurosensory deficits and recovery after lower third molar surgery: a prospective clinical study of 4338 cases. Int J Oral Maxillofac Surg 39:320–326
Genu PR, Vasconcelos BC (2008) Influence of the tooth section technique in alveolar nerve damage after surgery of impacted lower third molars. Int J Oral Maxillofac Surg 37:923–928
Blondeau F (1994) Paresthesia: incidence following the extraction of 455 mandibular impacted third molars. J Can Dent Assoc 60:991–994
Visintini E, Angerame D, Costantinides F, Maglione M (2007) Peripheral neurological damage following lower third molar removal. A preliminary clinical study. Minerva Stomatol 56:319–326
Swanson AE (1991) Incidence of inferior alveolar nerve injury in mandibular third molar surgery. J Cand Dent Assoc 57:327–328
Blondeau F, Daniel NG (2007) Extraction of impacted mandibular third molars: postoperative complications and their risk factors. J Cand Dent Assoc 73:325
Blackburn CW, Bramley PA (1989) Lingual nerve damage associated with the removal of lower third molars. Br Dent J 167:103–107
Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C (2000) Lingual nerve damage after third lower molar surgical extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 90:567–573
Jerjes W, Upile T, Shah P, Nhembe F, Gudka D, Kafas P et al (2010) Risk factors associated with injury to the inferior alveolar and lingual nerves following third molar surgery-revisited. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:335–345
Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C (2001) Inferior alveolar nerve damage after lower third molar surgical extraction: a prospective study of 1117 surgical extractions. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 92:377–383
Alling CC 3rd (1986) Dysesthesia of the lingual and inferior alveolar nerves following third molar surgery. J Oral Maxillofac Surg 44:454–457
Gühlicher D, Gerlach KL (2001) Sensory impairment of the lingual and inferior alveolar nerves following removal of impacted mandibular third molars. Int J Oral Maxillofac Surg 30:306–312
Jerjes W, Swinson B, Moles DR, El-Maaytah M, Banu B, Upile T et al (2006) Permanent sensory nerve impairment following third molar surgery: a prospective study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 102:1–7
Akadiri OA, Fasola AO, Arotiba JT (2009) Incidence and risk factors for nerve injuries in mandibular third molar surgery. Niger J Med 18:402–408
Black CG (1997) Sensory impairment following lower third molar surgery: a prospective study in New Zealand. N Z Dent J 93:68–71
Queral-Godoy E, Valmaseda-Castellon E, Berini-Aytes L, Gay-Escoda C (2005) Incidence and evolution of inferior alveolar nerve lesions following lower third molar extraction. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 99:259–264
Robert RC, Bacchetti P, Pogrel MA (2005) Frequency of trigeminal nerve injuries following third molar removal. J Oral Maxillofac Surg 63:732–735
Renton T, McGurk M (2001) Evaluation of factors predictive of lingual nerve injury in third molar surgery. Br J Oral Maxillofac Surg 39:423–428
Brann CR, Brickley MR, Shepherd JP (1999) Factors influencing nerve damage during lower third molar surgery. Br Dent J 186:514–516
Smith AC, Barry SE, Chiong AY, Hadzakis D, Kha SL, Mok SC et al (1997) Inferior alveolar nerve damage following removal of mandibular third molar teeth. A prospective study using panoramic radiography. Aust Dent J 42:149–152
Kipp DP, Goldstein BH, Weiss WW (1980) Dysesthesia after mandibular third molar surgery: a retrospective study and analysis of 1377 surgical procedures. J Am Dent Assoc 100:185–192
Robinson P, Smith KG (1996) Lingual nerve damage during lower third molar removal: a comparison of two surgical methods. Br Dent J 180:456–461
Pichler JW, Beirne OR (2001) Lingual flap retraction and prevention of lingual nerve damage associated with third molar surgery: a systematic review of the literature. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 91:395–401
Dodson TB (2005) Role of computerized tomography in management of impacted mandibular third molars. NY State Dent J 71:32–35
Rood JP, Shehab BBA (1990) The radiological prediction of inferior alveolar nerve injury during third molar surgery. Br J Oral Maxillofac Surg 28:20–25
Blaeser BF, August MA, Donoff RB, Kaban LB, Dodson TB (2003) Panoramic radiographic risk factors for inferior alveolar nerve injury after third molar extraction. J Oral Maxillofac Surg 61:417–421
Bell GW (2004) Use of dental panoramic tomographs to predict the relation between mandibular third molar teeth and the inferior alveolar nerve. Radiological and surgical findings and clinical outcome. Br J Oral Maxillofac Surg 42:21–27
Sedaghatfar M, August MA, Dodson TB (2005) Panoramic radiographic findings as predictors of inferior alveolar nerve exposure following third molar extraction. J Oral Maxillofac Surg 63:3–7
Tantanapornkul W, Okochi K, Bhakdinaronk A, Ohbayashi N, Kurabayashi T (2009) Correlation of darkening of impacted mandibular third molar root on digital panoramic images with cone beam computed tomography findings. Dentomaxillofac Radiol 38:11–16
Friedland B, Donoff B, Dodson TB (2008) The use of 3-dimensional reconstructions to evaluate the anatomic relationship of the mandibular canal and impacted mandibular third molars. J Oral Maxillofac Surg 66:1678–1685
Atieh MA (2010) Diagnostic accuracy of panoramic radiography in determining relationship between inferior alveolar nerve and mandibular third molar. J Oral Maxillofac Surg 68:74–82
Monaco G, Montevecchi M, Sonetti GA, Gatto MRA, Checchi L (2004) Reliability of panoramic radiography in evaluating the topographic relationship between the mandibular canal and impacted third molars. J Am Dent Assoc 135:312–318
Szalma J, Lempel E, Jeges S, Szabo G, Olasz L (2010) The prognostic value of panoramic radiography of inferior alveolar nerve damage after mandibular third molar removal: retrospective study of 400 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 109:294–302
Tay AB, Go WS (2004) Effect of exposed inferior alveolar neurovascular bundle during surgical removal of impacted lower third molars. J Oral Maxillofac Surg 62:592–600
Tantanapornkul W, Okouchi K, Fujiwara Y, Yamashiro M, Maruoka Y, Ohbayashi N et al (2007) A comparative study of cone-beam computed tomography and conventional panoramic radiography in assessing the topographic relationship between the mandibular canal and impacted third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 103:253–259
Ghaeminia H, Meijer GJ, Soehardi A, Borstlap WA, Mulder J, Berge SJ (2009) Position of the impacted third molar in relation to the mandibular canal. Diagnostic accuracy of cone beam computed tomography compared with panoramic radiography. Int J Oral Maxillofac Surg 38:964–971
Nakayama K, Nonoyama M, Takaki Y, Kagawa T, Yuasa K, Izumi K et al (2009) Assessment of the relationship between impacted mandibular third molars and inferior alveolar nerve with dental 3-dimensional computed tomography. J Oral Maxillofac Surg 67:2587–2591
Flygare L, Öhman A (2008) Preoperative imaging procedures for lower wisdom teeth removal. Clin Oral Investig 12:291–302
Pawelzik J, Cohnen M, Willers R, Becker J (2002) A comparison of conventional panoramic radiographs with volumetric computed tomography images in the preoperative assessment of impacted mandibular third molars. J Oral Maxillofac Surg 60:979–984
Nakagawa Y, Ishii H, Nomura Y, Watanabe NY, Hoshiba D, Kobayashi K et al (2007) Third molar position: reliability of panoramic radiography. J Oral Maxillofac Surg 65:1303–1308
Feifel H, Riediger D, Gustorf-Aeckerle R, Claus C (1991) High-resolution computerized tomography in the diagnosis of impacted third molars and its implications in terms of irradiation exposure. Dtsch Z Mund Kiefer Gesichtschir 15:226–231
Feifel H, Riediger D, Gustorf-Aeckerle R (1994) High resolution computed tomography of the inferior alveolar and lingual nerves. Neuroradiology 36:236–238
Koong B, Pharoah MJ, Bulsara M, Tennant M (2006) Methods of determining the relationship of the mandibular canal and third molars: a survey of Australian oral and maxillofacial surgeons. Aust Dent J 51:64–68
Richards AG (1952) Roentgenographic localization of the mandibular canal. J Oral Surg 10:325–329
Clark CA (1910) A method of ascertaining the relative position of unerupted teeth by means of film radiographs. Proc R Soc Med 3:87–90
Neugebauer J, Shirani R, Mischkowski RA, Ritter L, Scheer M, Keeve E et al (2008) Comparison of cone-beam volumetric imaging and combined plain radiographs for localization of the mandibular canal before removal of impacted lower third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 105:633–642
ICH E9: statistical principles for clinical trials. International Conference on Harmonization, London, 1998, adopted by CPMP July 1998 (CPMP/ICH/363/96)
Pederson GW (1988) Oral surgery. Surgical removal of teeth. WB Saunders, Philadelphia, p 63
Yuasa H, Kawai T, Sugiura M (2002) Classification of surgical difficulty in extracting impacted third molars. Br J Oral Maxillofac Surg 40:26–31
Akadiri OA, Obiechina AE, Arotiba JT, Fasola AO (2008) Relative impact of patient characteristics and radiographic variables on the difficulty of removing impacted mandibular third molars. J Contemp Dent Pract 9:51–58
Renton T, Smeeton N, McGurk M (2001) Factors predictive of difficulty of mandibular third molar surgery. Br Dent J 190:607–610
Santamaria J, Arteagoitia I (1997) Radiologic variables of clinical significance in the extraction of impacted mandibular third molars. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 84:469–473
Gbotolorun OM, Arotiba GT, Ladeinde AL (2007) Assessment of factors associated with surgical difficulty in impacted mandibular third molar extraction. J Oral Maxillofac Surg 65:1977–1983
Leonhardt H, Meinecke D, Gerlach KL (2005) Quantitative evaluation of thermosensitivity in patients with mandibular fractures. Mund Kiefer Gesichtschir 9:312–316
Leonhardt H, Meinecke D, Gerlach KL (2006) Quantitative determination of thermosensitivity after mandibular sagittal split osteotomy. Mund Kiefer Gesichtschir 10:162–167
Eng J (2003) Sample size estimation: how many individuals should be studied? Radiology 227:309–313
Halpern SD, Karlawish JHT, Berlin JA (2002) The continuing unethical conduct of underpowered clinical trials. JAMA 288:358–362
Altman DG (1991) Practical statistics for medical research. Chapman and Hall, London
Heurich T, Ziegler C, Steveling H, Wörtche R, Mühling J, Hassfeld S (2002) Digital volume tomography—an extension to the diagnostic procedures available for application before surgical removal of third molars. Mund Kiefer Gesichtschir 6:427–432
Susarla SM, Dodson TB (2007) Preoperative computed tomography imaging in the management of impacted mandibular third molars. J Oral Maxillofac Surg 65:83–88
Strietzel FP, Reichart PA (2002) Wound healing after removal of mandibuler third molars. An evidence-based analysis. Mund Kiefer Gesichtschir 6:74–84
Smith-Bindman R, Lipson J, Marcus R, Kim KP, Mahesh M, Gould R et al (2009) Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med 169:2078–2086
Loubele M, Bogaerts R, van Dijck E, Pauwels R, Vanheusden S, Suetens P et al (2009) Comparison between effective radiation dose of CBCT and MSCT scanners for dentomaxillofacial applications. Eur J Radiol 71:461–468
Looe HK, Eenboom F, Chofor N, Pfaffenberger A, Steinhoff M, Rühmann A et al (2008) Conversion coefficients for the estimation of effective doses in intraoral and panoramic dental radiology from dose-area product values. Radiat Prot Dosim 131:365–373
Öhman A, Kull L, Andersson J, Flygare L (2008) Radiation doses in examination of lower third molars with computed tomography and conventional radiography. Dentomaxillofac Radiol 37:445–452
Looe HK, Eenboom F, Chofor N, Pfaffenberger A, Sering M, Rühmann A et al (2007) Dose–area product measurements and determination of conversion coefficients for the estimation of effective dose in dental lateral cephalometric radiology. Radiat Prot Dosim 124:181–186
Fayngersh V, Passero M (2009) Estimating radiation risk from computer tomography scanning. Lung 187:143–148
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roeder, F., Wachtlin, D. & Schulze, R. Necessity of 3D visualization for the removal of lower wisdom teeth: required sample size to prove non-inferiority of panoramic radiography compared to CBCT. Clin Oral Invest 16, 699–706 (2012). https://doi.org/10.1007/s00784-011-0553-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-011-0553-8