Abstract
This in vitro study compared the marginal adaptation of all-ceramic MOD-inlays luted to human molars with four self-adhesive resin cements. Thirty-two human third molars were randomly assigned to four test groups (n = 8 per group). MOD cavities were prepared with approximal finishing lines in dentin and enamel. All-ceramic Empress 2 inlays were luted with four self-adhesive cements (Clearfil SA, iCEM, Bifix SE, seT). Oral stress was simulated by 90 day storage in water as well as by thermal and mechanical loading (TCML, 1.2 × 106 × 50 N, 6,000× 5°/55°, 1.6 Hz). The marginal fit was evaluated by scanning electron microscopy (SEM) and dye penetration. Data were analyzed with the ANOVA/Tukey's test (α = 0.05). The SEM investigation of the gingival cement margins (cement–tooth interface) showed values of perfect margin [percent] (means ± SD) after simulated aging between 84 ± 9% and 95 ± 5% for enamel and 80 ± 9% and 92 ± 3% for dentin. In enamel, seT showed significantly higher marginal integrity than iCEM after water storage and TCML (post hoc; p = 0.011). Furthermore, the marginal adaptation of iCEM in enamel deteriorated by simulated aging (p = 0.014, ANOVA). Mean values of dye penetration (percentage of dye entry into dentin) at the investigated restorations margins ranged between 3% and 8% for enamel and 12% and 22% for dentin. Clearfil SA, iCEM, and seT showed lower dye penetration in enamel than in dentin (Clearfil SA: p = 0.013, iCEM: p = 0.044, seT: p = 0.003). The results suggest that the four self-adhesive luting agents investigated seem to successfully bond to dentin-restricted as well as to enamel-restricted cavities, predicting good clinical performance.
Similar content being viewed by others

Avoid common mistakes on your manuscript.
Introduction
All-ceramic restorations have become widely accepted within the past decades because of increasing aesthetic demand and improved materials. Depending on the type of ceramic or restoration, practitioners may either want to use conventional cementation with, for example, glass-ionomers or adhesive cementation with resin cements [1]. Adhesive cementation increases the stability of glass ceramic restorations (inlays, veneers, partial crowns, crowns) and assures the fixation of a restoration on the abutment in case an abutment tooth is not retentively prepared.
This study investigated the marginal integrity of cemented ceramic inlays during simulated oral and practice-like conditions. Testing marginal adaptation allowed the investigation of critical interfaces (cement–tooth, cement–restoration) and the evaluation of the possible impacts of saliva and chewing processes on the margins of dental restorations [2]. Microleakage may be detected, leading to bacterial ingress, secondary caries at the tooth or restoration interface, and hypersensitivity of the restored tooth [3–5]. Gap-free continuous cement margins are considered important for the longevity of dental restorations [3], even though no luting material is able to achieve a perfect marginal seal [6]. Scanning electron microscopy (SEM) is a generally accepted test method to visually observe the adaptation of restorative materials to cavity margins and to detect microleakage on surfaces [3]. However, SEM only enables the observation of exposed margin sections [7]. Dyes provide a sensitive method for discovering “functional” leakage by showing visible penetration into the tooth substance [3].
Conventional resin cements (e.g., Panavia F 2.0 (Kuraray, Osaka, Japan), Variolink II (Ivoclar Vivadent, Schaan, Liechtenstein) have been proven not only to effectively bond to the tooth substance but to show good marginal adaptation [8–12]. Achieving a micro-retentive bond between cement and tooth substance requires several steps [13]: etching (selective or total etch), priming, and bonding can be done in different ways depending on the adhesive system used. Literature reports have described the clinical success of adhesive bonding to enamel and dentin when performed in three steps [13, 14]. However, this process is time-consuming and sensitive to handling errors: problems arise, for example, because of excessive drying of the cavity surfaces [15–17] or because of residual water on the enamel or dentin surface, inhibiting a proper micro-retentive bond [18].
Cements were developed that avoid the complex bonding procedures by reducing the number of application steps while obtaining results comparable to conventional resin cements [13]. In 2001, a self-adhesive luting agent was introduced to the market (RelyX Unicem, 3M ESPE, Seefeld, G) claiming that the adhesive luting procedure would become as simple as the luting procedure of conventional cements, such as glass-ionomers, and did not require special surface treatment [7, 19]. RelyX Unicem consists of a matrix with components of composites (monomers, (acidic) methacrylates) as well as of glass-ionomers (reactive glass fillers) [20–23]. The first clinical data after over 3 years and many in vitro data show that this cement is indeed successful [8, 9, 24, 25]. However, this material also requires improvement: both the marginal adaptation [12, 24, 26] and the bonding effectiveness [27] of RelyX Unicem were found to be lower in enamel than in dentin, as known from all-in-one adhesives [28]. Also, the bond strength of RelyX Unicem showed inferior results on dentin surfaces than conventional resin cements [29].
The great success of RelyX Unicem has prompted many dental companies to develop a self-adhesive luting agent. Obviously, clinical studies are necessary but sufficient clinical data may only be available in 3 to 4 years' time. Meanwhile, the marginal adaptation of new cements in comparison to well-established and investigated materials has to be evaluated by in vitro studies.
A previous study [24] compared the marginal adaptation of three self-adhesive cements (RelyX Unicem, Maxcem (Kerr Hawe, Orange, CA, USA), Multilink Sprint (Ivoclar Vivadent, Schaan, Liechtenstein)) with the multi-step system Panavia F 2.0 (Kuraray, Osaka, Japan) after aging using the well-tried adhesive system Panavia F 2.0 as control [8, 9, 29, 30]. The results of scanning electron microscopy and the dye penetration test showed that only the marginal adaptation of RelyX Unicem was comparable to the control group Panavia [24]. The performance of Maxcem and Multilink Sprint was inferior. Therefore, we decided to investigate other self-adhesive resin cements currently available on the dental market. To promptly receive results, a limited number of cements were tested in the present experiments.
The objective of this in vitro study was to compare the marginal adaptation of all-ceramic MOD-inlays luted to human molars with four different self-adhesive resin cements. All specimens underwent an aging procedure in a chewing simulator that simulated 5 years of oral stress to show the possible effects of oral exposure [28, 31–37]. The quality of the proximal restorations' margins in enamel and dentin was evaluated by SEM and dye penetration test [3, 38, 39]. The self-adhesive luting agents were compared with each other with regard to marginal adaptation. The null hypothesis was that the four self-adhesive cements do not show any different marginal adaptation after the aging process.
Materials and methods
This in vitro study was designed to simulate actual dental practice: all-ceramic MOD-inlays were luted to extracted human molars with different self-adhesive resin cements. Oral conditions were simulated by water storage as well as thermal and mechanical loading (TCML). Models were created that allow mechanical loading and tests for leakage. Replicas of test specimens were made after cementation and after TCML (thermocycling and mechanical loading) for SEM analysis. Marginal adaptation was measured with common methods: scanning electron microscopy (SEM) and dye penetration tests [3, 38, 39].
Preparation of the test specimens
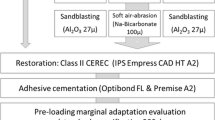
As test specimens, 32 human molars were used in this study stored in 0.5% chloramine aqueous solution for up to 6 weeks. The apices of the teeth roots were covered (closed) with wax before a thin (approximately 1 mm in thickness) layer of polyether (Impregum, 3M ESPE, Seefeld, Germany) was applied to the root surface. Then, the teeth roots were axially inserted in polymethylmethacrylate (PMMA) resin (Palapress Vario, Heraeus-Kulzer, Wehrheim, Germany). Considering the polyether layer as an artificial periodontium, physiological tooth movement could be simulated [31]. The inserted teeth were randomly assigned into four subgroups of eight teeth each. Obviously, a low number of test specimens may be more affected by variables, such as dimension, age, and history of the teeth or structure of the hydroxyapatite, leading to higher standard deviations in statistical analysis [39]. The extraction procedure may result in cracks that allow microorganisms to enter the tooth substance [40]. To limit consequences of such tooth-related facts, macroscopically crack-free and caries-free human third molars were chosen, and cavities of similar dimensions were prepared. The inlay cavities (Class II MOD) were prepared with diamond burs (Cerinlay Set, Intensiv, Viganello Lugano, Switzerland) in a high-speed handpiece with sufficient water cooling. The preparation corresponded with the criteria of ceramic inlays [41]: occlusal cavity depth 1.5 to 2 mm, cavity isthmus width ∼1/3 of the intercuspal width (about 2 mm), total occlusal convergence angle (TOC) about 20°, and rounded internal line angles. Proximal margins were mesially placed 1 mm below the cemento-enamel junction in dentin and distally 1 mm above in enamel. Impressions were taken from the prepared teeth (Permadyne-Penta, 3 M ESPE, Seefeld, Germany), and gypsum casts were made. On the casts, Empress 2 all-ceramic inlays were manufactured by a dental technician. Spacer (Clear Spacer (transparent), Yeti Dental, Engen, Germany; Cergo Die Spacer, Degudent, Hanau, Germany) was applied in a reproducible way to achieve similar cement margin thickness. The occlusal contact area was constructed in correspondence to a human molar antagonist (three-point occlusal contact). These antagonists were later used for applying the occlusal load during the simulation of oral stress.
The inner surfaces of the ceramic inlays were etched for 60 s with 5% hydrofluoric acid (IPS Ceramic etching gel, Ivoclar-Vivadent, Schaan, Liechtenstein). After rinsing (1 min) and drying, a silane coupling agent (Monobond S, Ivoclar-Vivadent) was applied to the etched ceramic surface with an applicator brush. The silane was left undisturbed for 60 s and was then gently dried with air to assure complete evaporation. Teeth were rinsed off with water (15 s) and carefully dried to prevent a collapse of the collagen network. The inlays were cemented with four different self-adhesive luting agents in accordance to the manufacturers' instructions: the tested cements were dispensed directly from an automix syringe or applied after activation and mixing of a capsule (Table 1). Both cavity and silanated ceramic surfaces were covered with cement. Inlays were inserted, fixed with a ball plugger, and light cured for 2 s each side (sdi radii plus, SDI, Victoria, Australia). Large excess was removed with hand instruments (PF-3 DE Carver, GK 7 Black's SE Gold Knife (HuFriedy, Chicago, USA)). Finally, the restorations were light cured for 20 to 30 s each side. The cement gap and the restorations' margins of the proximal box were then gently polished with Sof-Lex discs (3M ESPE) (low speed, water cooling). The cemented restorations were investigated with a laboratory microscope to detect macroscopic cement excess on the margins and then polished with a finishing bur (Shofu One Gloss, Shofu Dental). The cemented Empress inlays were finished and restorations' margins were polished with Sof-Lex discs (3 M ESPE, St Paul, USA) and polishing burs (Shofu One Gloss, Shofu Dental, Ratingen, Germany). Then, impressions were taken with a polyether material (Permadyne-Penta, 3 M ESPE, Seefeld, Germany), copying the cervical–proximal margins (dentin and enamel) of the MOD inlays. The impressions were poured with an epoxy-resin (Rencast CW 2215, Huntsman, Everberg, Belgium) to get marginal analysis replicas for the scanning electron microscope (SEM). After the drying process (24 h), the back sides of the replicas were finished with a bur, fixed on special metallic beams with carbon cement glue, and coated with a gold film using a sputter coater (BAL-TEC SCD005 Sputter Coater, BAL-TEC AG, Liechtenstein). All inlays were stored in distilled water at 37°C for 90 days [28], followed by thermal cycling and mechanical loading (TCML) for 8.3 days; 6,000 × 5/55°C, changing every 2 min, 1.2 × 106 × 50 N, 1.66 Hz. These parameters are considered to represent a 5-year period of oral stress [31, 42].
The load of 50 N was applied by the same antagonists (third human molars) used for forming the occlusal contact area of the inlays. The cemented inlays were stressed by axial load with a three-point support. After water storage and TCML, impressions were taken again from the marginal areas to construct the epoxy resin replicas.
SEM
The gold-coated replicas were examined with scanning electron microscopy (Stereoscan 240, Cambridge Instruments, Nussloch, Germany). SEM images were analyzed with an image analysis system (Optimas 6.0, Orange, USA).
The following interfaces were examined, i.e., restoration-to-cement and cement-to-enamel and dentin, and the following assessment criteria (Fig. 1) were defined [38]:
-
1.
Perfect margin. The two adjoining surfaces (cement–ceramic, cement–tooth) show no interruption of the continuous margin and merge into each other without any difference in level.
-
2.
Marginal gap. The two adjoining surfaces show gap formation due to loss of cohesion or adhesion.
-
3.
Non-assessable areas. All adjoining areas that do not fit criteria 1 or 2:
-
Defects in material and processing irregularities: The interfaces show level differences due to, for instance, cement excess or cement deficits. Yet, marginal integrity (continuous margins) is provided.
-
Non-evaluable areas: Imperfections of the polyether impression, improper epoxy resin effusion, or areas with bullous overlays inhibit evaluation of the critical interfaces.
-
Small drop-outs of the cement layer after TCML due to mechanical loading (rarely).
-
Dye penetration
After TCML, the polyether layers were removed from each tooth root. We completely coated all teeth with nail varnish, except for areas within 1 mm from the proximal restoration margins, thus preventing dye penetration elsewhere [39]. The coated teeth were stored in 0.5% basic fuchsine solution (pH = 10.2) with distilled water. After 16 h storage at 37°C, we rinsed off the fuchsine solution with water and removed the nail varnish. Teeth were embedded in PMMA resin (Palapress Vario, Kulzer, Wehrheim, Germany), fixed on a special tray of a low-speed diamond saw (Innenlochsäge Leitz 1600, Leitz, Germany) and then cut longitudinally in 600 μm sections (seven per tooth, mean value) in a mesio-distal direction. Dye penetration was measured with a microscope (12.5×; Leica Zeiss, Oberkochen, Germany). Digital images of the sections were recorded. The amount of dye entry into dentin at the cement–tooth interface of the proximal restoration margin was measured metrically (Corel Draw 7.0) and set as a percentage of the whole depth of the proximal box (100%) (Fig. 2).
Because of its tubule system, dentin is permeable to dyes and other solutes. Limiting factors of dye penetration result from the nature of the extracted teeth. Aged teeth, for example, show lowered permeability of the dentin because of mineral deposits in the tubule system and hypermineralized peritubular dentin. Furthermore, long-time carious lesions may provoke pathological reactions of the pulp–dentin system (stained tubules towards the pulp) to lower the permeability for bacterial toxins [39]. However, basic fuchsine has shown to bind preferentially with carious dentin [3]. All natural teeth used were macroscopically caries-free, but even microscopically hypomineralized dentin may facilitate the entry of a tracer into superficial dentin.
Statistics
Means and 95% confidence intervals of means were calculated. Statistical differences were analyzed with ANOVA and the Tukey test, and the level of significance was set at α = 0.05.
SEM analysis
Areas with “perfect margin” (PM), “marginal gap” (G), as well as “non-evaluable” (NE) areas were calculated per proximal tooth side in relation to the overall length of the proximal gingival restorations' margin for dentin vs. enamel. To clearly arrange the results, a statistical analysis of the criteria “marginal gap” and “non-assessable areas” were rejected, since the criterion “perfect margin” sufficiently describes the quality of the marginal adaptation.
Statistics of dye penetration tests
Means of dye penetration per proximal tooth side (dentin/enamel) were defined. Only specimens with dye entry into dentin were included in the statistics.
Results
Scanning electron microscopy
Regarding enamel margins, aging significantly impaired the marginal adaptation of iCEM on the cement–tooth interface (p = 0.014, ANOVA). The 95% confidence interval of means showed the lowest values of perfect margin integrity after aging for iCEM and Clearfil SA. Only seT showed a significantly higher percentage of perfect margin on the cement–tooth interface after TCML than iCEM (post hoc; p = 0.011) (Fig. 3a; Table 2).
For dentin margins, Bifix SE and iCEM showed the lowest values of perfect margin areas and had the widest distribution of values, particularly on the cement–dentin interface.
Before artificial aging, Bifix SE, seT and Clearfil SA showed higher values of “perfect margin” than iCEM with a significant difference between Bifix SE and iCEM on the cement–inlay interface in dentin (post hoc; p = 0.029) and a significant difference between seT and iCEM on the cement–dentin interface (post hoc; p = 0.044).
After TCML, values for Bifix SE (post hoc; p = 0.03) and seT (post hoc; p = 0.023) were significantly higher than those for iCEM on the cement–inlay interface. The marginal adaptation of Clearfil SA on the cement–dentin interface was significantly better after aging than after initial cementation (p = 0.003, ANOVA).
Dye penetration
For proximal enamel margins, all four groups of self-adhesive cements showed values of dye penetration of less than 15%. We found the lowest values for seT, iCEM, and Clearfil SA; however, the differences between the tested materials were not statistically significant (Fig. 3b; Table 2).
For dentin margins, seT showed the lowest mean values of dye penetration followed by iCEM, Bifix SE, and Clearfil SA. The values for Clearfil SA were widely distributed, but no significant deterioration was found when comparing the performance of the four resin cements in dentin.
Clearfil SA, iCEM, and seT showed significant lower dye penetration in enamel than in dentin (Clearfil SA, p = 0.013, iCEM, p = 0.044, seT, p = 0.003).
Discussion
Cement margins of indirect restorations are commonly investigated by in vitro studies on human teeth. To preliminarily predict the clinical performance of adhesively luted restorations oral conditions have to be simulated. A certain tooth movement inside the alveole was permitted by a thin polyether layer covering the roots. Literature reports describe that ceramic restorations are sensible to the physiological tooth movements because of their low bending strength: Rosentritt et al. found that an artificial periodontium (next to thermal cycling, mechanical loading and human antagonist) reduced the fracture resistance of fixed partial dentures [31]. Since literature reports use different values of assumable tooth movements, the thickness of the polyether layer was set arbitrarily (1 mm). Furthermore, all samples underwent an aging procedure. In their review, Manhart et al. showed that oral stress influences the marginal integrity of indirect restorations [36]. Our chosen parameters of TCML should simulate a 5-year period of oral stress (6,000 cycles, 5°/55°, 8.3 days) [31]. Long-term water storage (90 days) and thermocycling may show effects of hydrolysis, such as degradation of the resin matrix, which may result in a loss of sealing and gap formation [32–35]. Thus, clinical failure might be expected. In 2007, Blunck and Zaslansky compared resin cement margins after different periods of water storage. The authors found that different materials have different deterioration rates after initial vs. long-term water storage and that one-bottle all-in-one adhesives seem to be significantly affected by water storage on enamel margins [28]. For this reason, the impact of long-term water storage and chewing processes were incorporated into this study.
The marginal fit of the tested self-adhesive resin cements was investigated with common laboratory methods using semi-quantitative marginal analysis (SEM) and dye penetration test [3, 38, 39]. SEM investigation allows the observation of the quality of cement margins at the critical interfaces. The dye penetration test is intended to find failures undetected in SEM analysis. However, the limitations of both methods need to be discussed.
Dye penetration tests use the characteristic of dentin to be permeable to dyes and other solutes because of its tubule system. It is described in literature that the permeability of dentin is higher in laboratory tests than in vivo [39]. This observation may preclude the interpretation of any dye entry in in vitro studies as a lack of sealing. The non-existence of pulpal pressure and dentinal fluid in non-vital teeth seems to increase permeability in laboratory conditions [39]. Further limiting factors result from the nature of the extracted teeth. Aged teeth, for example, show lower permeability of the dentin because of mineral deposits in the tubule system and hypermineralized peritubular dentin. Additionally, long-time carious lesions may provoke pathological reactions of the pulp–dentin system (stained tubules towards the pulp) to lower the permeability for bacterial toxins [39]. However, basic fuchsine has shown to preferentially bind with carious dentin [3]. All natural teeth used were macroscopically caries-free, but even microscopically hypomineralized dentin may facilitate the entry of a tracer into superficial dentin.
Also, the results of dye penetration may vary significantly within different operators, since samples were evaluated subjectively [3]. Dye penetration simply gives an indication whether there is leakage or not. The actual extent of dye penetration is less valuable for comparing the sealing ability of different materials. A limited amount of dye penetration may be tolerable in dentin permeability testings for evaluating the marginal seal. But microleakage must be suspected to be above a certain amount of tracer entry. In vivo, microleakage may lead to secondary caries and pulpal inflammation through bacterial ingress as well as to hypersensitivity or staining at the restorations' margins [3, 37, 39].
Dye penetration into the dentin tubules shows insufficient sealing between the cement layer and the tooth substance [39]. Solitary penetration into the cement layer was not considered in the present results because of the initially low pH value of the cement matrix and the basic pH value of the fuchsine dye. As described in the literature, one-step self-etch adhesives contain acidic monomers to demineralize and infiltrate the tooth substrate, establishing self-adhesion to calcium ions in the hydroxyapatite [13, 14]. This process was also expected for self-adhesive cements [20–22]. The acidic monomers may not be totally neutralized and therefore react with the basic fuchsine dye. Such chemical reaction would explain the coloration of the cement. Therefore, the operative point was assumed to be good sealing of the tooth surface proven by the lack of dye penetration into the dentin structure.
Regarding the evaluated surfaces (cement-dentin, cement-enamel), seT performed best, though differences between the tested materials were not significant. Literature reports have shown that the marginal adaptation of self-adhesive cements (RelyX Unicem, 3M Espe) differs on the observed surfaces (inlay, dentin, enamel) with a better performance in dentin than in enamel [12, 26, 27]. In previous studies, adhesion of RelyX Unicem to enamel was lower than adhesion to approved more-step resin cements (such as Panavia F or Syntac/Variolink II) but higher than adhesion to glass ionomers [7, 27]. Since in our investigation, we found lowest rates of dye entry in enamel, the marginal fit appeared to be better in enamel than in dentin (significant for seT, iCEM, and Clearfil SA). Enhanced chemical interaction with enamel, presumably due to variations in the pH value of the new cements [23], may be an explanation for this astonishing result. The literature has postulated that lower pH values of self-adhesive cements as well as additional selective etching of the enamel margins enhance adhesion to enamel [7]. However, the data show that improved sealing to enamel does not implicate comparable adhesion to dentin. Finding the right balance to achieve similar bonding to dentin and enamel still seems to be difficult.
Scanning electron microscopy (SEM) is a high-resolution technique for examining the marginal morphology of dental restorations and for easily detecting marginal defects. Its great advantage over other methods, such as light microscopy, is excellent detail reproduction, high depth of field, and marked accuracy [3, 38]. The high level of detail is needed for analyzing margins of resin cements, since “perfect margins” can be achieved with adhesive materials [38, 43]. Furthermore, SEM represents a non-destructive method and allows the evaluation of the same margins at different times, which is particularly useful for testing the effects of oral stress or water storage on the same specimens. For this investigation, we used epoxy-resin replicas, which are considered to precisely reproduce surfaces and allow high SEM magnification [38]. Criteria were defined to precisely evaluate the critical interfaces (perfect margin, gap formation, non-evaluable areas). However, SEM replicas were subjectively investigated by a human operator. This fact definitely constitutes a potential for errors because of the likelihood of deficiencies or variations in the definition of the applied criteria. However, errors in rating the morphology of restoration margins can be diminished if specimens are evaluated by the same operator. Roulet et al. found that the difference between two measurements conducted by the same researcher 3 weeks apart was only 3% (± 2.6%) when five criteria were used to characterize the marginal quality of direct MOD composite restorations [38]. Therefore, in this study, the same operator evaluated the cement gap morphology before and after TCML. Another shortcoming of this method is that only surfaces can be observed. Thus, a complete picture of marginal quality necessitates invasive techniques [44].
The results of the SEM analysis show that artificial aging has an impact on the marginal integrity of Bifix SE and iCEM, showing lower rates of perfect margins after TCML.
In previous studies, similar deterioration after TCML was found for RelyX Unicem [9, 24] in enamel and for Maxcem (Kerr Hawe, Orange, CA, USA) in dentin [24]. A possible explanation may be given by the composition of the cement matrix. Even though manufacturers provide only vague information about the composition and chemical reactions to achieve adhesion to either tooth substance or restoration, a chemical mechanism similar to RelyX Unicem can be presumed. The matrix of RelyX Unicem contains components of composites (monomers, methacrylates) as well as of glass ionomers (reactive glass fillers) [22]. Course glass fillers might lower the cohesion of the cement. A glass ionomer-related matrix might therefore be susceptible for outbreaks of course filler particles on the cement margins under mechanical load, explaining the lower rates of “perfect margin” (SEM) after TCML.
Enhanced marginal adaptation after the aging process was found for seT on all interfaces evaluated and for Clearfil SA on dentin. Water absorption by cement components presumably affects the volume and dimension of the cement matrix [32, 34, 35], pretending enhanced marginal fit. Glass ionomer components of self-adhesive resin cements might absorb water during artificial aging, which would limit the indications for self-adhesive resin cements.
Furthermore, the application of stress may affect the cement gap: occlusal load during chewing simulation apparently leads to compression of the cement gap. Furthermore, rolling motion may occur depending on the elasticity modulus of the fundament (dentin).
Comparing the results of dye penetration and SEM analysis, the latter was expected to show a higher percentage of perfect margins. It may be explained by the subtle evaluation of the gingival cement margins in scanning electron microscopy (high number of possible criteria). The dye penetration test only distinguishes between two possible events: penetration or not. Furthermore, after luting the ceramic inlays to the cavities, excess cement was removed after a few seconds of light curing with hand instruments. Because of this procedure, small marginal cement outbreaks were (rarely) detected in the gap with the microscope, resulting in lower values of perfect margins in SEM analysis. In this study, (excessive) dye entry was not found. In summary, the quality of the marginal adaptation to the tooth substance was promising.
Comparisons to the results of other published studies are rather restricted and should be made only cautiously because no control was included. However, an enhanced adhesion to enamel may increase long-term clinical success and should be a focus in future research. Controlled clinical studies are necessary to determine the clinical performance of the different self-adhesive cements available on the market. Also, the bond strength of materials should be investigated in in vitro studies. Dental practitioners require material that are easy and comfortable to handle; however, the handling of the cements tested varied (worst for iCEM), thus leaving room for improvement by the manufacturers.
Conclusion
Within the limits of the present experiments, the following can be concluded: the null-hypothesis was rejected, since the SEM analysis showed that aging significantly impaired the marginal adaptation of iCEM on the cement–enamel interface (p = 0.014, ANOVA). seT seemed to work best on all investigated interfaces, showing the lowest values for dye penetration and a significantly higher percentage of “perfect margins” than iCEM, both for enamel (after TCML post hoc; p = 0.011) and dentin (before TCML post hoc; p = 0.044). For Clearfil SA, iCEM, and seT, the marginal integrity was significantly lower in enamel than in dentin. The self-adhesive luting agents investigated seemed to successfully bond to both dentin- and enamel-restricted cavities, promising good clinical performance.
References
Rosenstiel SF, Land MF, Crispin BJ (1998) Dental luting agents: a review of the current literature. J Prosthet Dent 80:280–301
Mota CS, Demarco FF, Camacho GB, Powers JM (2003) Microleakage in ceramic inlays luted with different resin cements. J Adhes Dent 5:63–70
Alani AH, Toh CG (1997) Detection of microleakage around dental restorations: a review. Oper Dent 22:173–185
Kidd EAM (1976) Microleakage: a review. J Dent 4:199–206
Going RE (1972) Microleakage around dental restorations: a summarizing review. J Am Dent Assoc 84:1349–1357
Gladys S, van Meerbeek B, Lambrechts P, Vanherle G (2001) Microleakage of adhesive restorative materials. Am J Dent 14:170–176
De Munck J, Vargas M, Van Landuyt K, Hikita K, Lambrechts P, Van Meerbeek B (2004) Bonding of an auto-adhesive luting material to enamel and dentin. Dent Mater 20:963–971
Abo-Hamar SE, Hiller KA, Jung H, Federlin M, Friedl KH, Schmalz G (2005) Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin Oral Investig 9:161–167
Behr M, Rosentritt M, Regnet T, Lang R, Handel G (2004) Marginal adaptation of a self-adhesive universal resin cement compared with well-tried systems. Dent Mater 20:191–197
De Kanter RJ, Creugers NH, Verziden CW, Vanthof MA (1998) A five year multi-practice clinical study on posterior resin bonded bridges. J Dent Res 77:609–614
Krämer N, Lohbauer U, Frankenberger R (2000) Adhesive luting of indirect restorations. Am J Dent 13:60D–76D, Spec No
Schenke F, Hiller KA, Schmalz G, Federlin M (2008) Marginal integrity partial ceramic crowns within dentin with different techniques and materials. Oper Dent 33:516–525
Van Meerbeek B, De Munck J, Yoshida Y, Inoue S, Vargas M, Vijay P, Van Landuyt K, Lambrechts P, Vanherle G (2003) Buonocore memorial lecture. Adhesion to enamel and dentin: current status and future challenges. Oper Dent 28:215–235
De Munck J, Van Landuyt K, Peumans M, Poitevin A, Lambrechts P, Braem M, Van Meerbeek B (2005) A critical review of the durability of adhesion to tooth tissue: methods and results. J Dent Res 84:118–132
Gwinnett AJ (1992) Moist versus dry dentin: its effect on shear bond strength. Am J Dent 5:127–129
Kanca J 3rd (1992) Resin bonding to wet substrate. I. Bonding to dentin. Quintessence Int 23:39–41
Saunders WP, Saunders EM (1996) Microleakage of bonding agents with wet and dry bonding techniques. Am J Dent 9:34–36
Prati C (1998) In vitro and in vivo adhesion in operative dentistry: a review and evaluation. Pract Periodontics Aesthet Dent 10:319–327
Technical product profile (2007) RelyX Unicem. 3M ESPE
Van Landuyt KL, Snauwaert J, De Munck J, Peumans M, Yoshida Y, Poitevin A, Coutinho E, Suzuki K, Lambrechts P, Van Meerbeek B (2007) Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 28:3757–3785
Tay FR, Pashley DH, Peters MC (2003) Adhesive permeability affects composite coupling to dentin treated with a self-etch adhesive. Oper Dent 28:610–621
Gerth HU, Dammaschke T, Züchner H, Schäfer E (2006) Chemical analysis and bonding reaction of RelyX Unicem and Bifix composites—a comparative study. Dent Mater 22:934–941
Han L, Okamoto A, Fukushima M, Okiji T (2007) Evaluation of physical properties and surface degradation of self-adhesive resin cements. Dent Mater 26:906–914
Behr M, Hansmann M, Rosentritt M, Handel G (2009) Marginal adaptation of three self-adhesive resin cements vs. a well-tried adhesive luting agent. Clin Oral Investig 13:459–464
Kadam P, Zadeh R, Cakir D, Preston B, Ramp LC, Burgess J (2008) Shear bond strength of self-adhesive cements to enamel and dentin. J Dent Res 87(Spec Iss B):0385
Ibarra G, Johnson GH, Geurtsen W, Vargas MA (2007) Microleakage of porcelain veneer restorations bonded to enamel and dentin with a new self-adhesive resin-based dental cement. Dent Mater 23:218–225
Hikita K, Van Meerbeck B, De Munck J, Ikeda T, Van Landuyt K, Maida T, Lambrechts P, Peumanns M (2007) Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent Mater 23:71–80
Blunck U, Zaslansky P (2007) Effectiveness of all-in-one adhesive systems tested by thermocycling following short and long-term water storage. J Adhes Dent 9:231–240
Lührs AK, Guhr S, Günay H, Geurtsen W (2010) Shear bond strength of self-adhesive resins compared to resin cements with etch and rinse adhesives to enamel and dentin in vitro. Clin Oral Investig 14:193–199
Kern M (2005) Clinical long-term survival of two-retainer and single retainer all-ceramic resin-bonded fixed partial dentures. Quintessence Int 36:141–147
Rosentritt M, Behr M, Gebhard R, Handel G (2006) Influence of stress simulation parameters on the fracture strength of all-ceramic fixed-partial dentures. Dent Mater 22:176–182
Inoue S, Yoshida Y, De Munck J, Nagakane K, Suzuki K, Sano H, Van Meerbeek B (2005) Hydrolytic stability of self-etch adhesives bonded to dentin. J Dent Res 84:1160–1164
Krämer N, Frankenberger R, Pelka M, Petschelt A (1999) IPS Empress inlays and onlays after four years—a clinical study. J Dent 27:325–331
Ferracane JL (2006) Hygroscopic and hydrolytic effects in dental polymer networks. Dent Mater 22:211–222
Bagheri R, Tyas M, Burrow MF (2007) Subsurface degradation of resin-based composites. Dent Mater 23:944–951
Manhart J, Chen H, Hamm G, Hickel R (2004) Buonocore memorial lecture. Review of the clinical survival of direct and indirect restorations in posterior teeth of the permanent dentition. Oper Dent 29:481–508
Brännström M (1986) The cause of post-restorative sensitivity and its prevention. J Endodont 12:475–481
Roulet JF, Reich T, Blunck U, Noack MJ (1989) Quantitative margin analysis in the scanning electron microscope. Scanning Microscopy 3:147–159
Gale MS, Darwell BW (1999) Dentine permeability and tracer tests. J Dent 27:1–11
Phair CB, Fuller JL (1985) Microleakage of composite resin restorations with cementum margins. J Prosthet Dent 53:361–364
Thompson MC, Thompson KM, Swain M (2010) The all-ceramic, inlay supported fixed partial denture. Part 1. Ceramic inlay preparation design: a literature review. Aust Dent J 55:120–127
Nothdurft FP, Schmitt T, Motter PJ, Pospiech PR (2008) Influence of fatigue testing and cementation mode on the load-bearing capability of bovine incisors restored with crowns and zirconium dioxide posts. Clin Oral Investig 12:331–336
Blunck U, Roulet JF (1989) In vitro marginal quality of dentin-bonded composite resins in Class V cavities. Quintessence Int 20:407–412
van Dijken JWF, Hörstedt P (1996) Marginal breakdown of 5-year-old direct composite inlays. J Dent 24:389–394
Acknowledgments
We thank the company Kuraray for providing the cement system Clearfil SA (Kuraray, Osaka, Japan).
Conflict of interests
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Aschenbrenner, C.M., Lang, R., Handel, G. et al. Analysis of marginal adaptation and sealing to enamel and dentin of four self-adhesive resin cements. Clin Oral Invest 16, 191–200 (2012). https://doi.org/10.1007/s00784-010-0501-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-010-0501-z