Abstract
The aim of this study was to compare the short-term performance of a session of single photodynamic therapy (PDT) and of a conventional ultrasonic debridement (UST) in persistent pockets of maintenance patients. In a prospective, randomized, controlled, single-blind clinical study, patients with chronic periodontitis with at least two persistent pockets (>4 mm) were enrolled. They were treated either with UST (n = 29) or PDT (n = 25). Clinical and microbiological examinations were performed at baseline and after 3 month. For UST, the mean probing depth was reduced from 5.3 to 4.5 mm (p = <0.001) and for PDT from 5.3 to 4.7 mm (p < 0.001) with no difference between the two treatment modalities. Microbial counts were significantly reduced about 30% to 40% immediately after debridement but returned to baseline values at month 3 irrespective of treatment. PDT is not superior to conventional mechanical treatment of persistent pockets, but it may be a meaningful therapeutic alternative; the clinical effects were too minor to draw a definitive conclusion.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
An important goal of periodontal therapy is the removal of the bacterial biofilm from the subgingival root surface. The success of mechanical debridement decreases with increasing probing depth and with furcation involvement [13, 30, 38]. The problems inherent to subgingival scaling result from the difficult access to the root surface and from the bizarre root morphology. Therefore, complete removal of bacterial deposits in vivo is accomplished rather seldom [8, 27, 28], and bacterial reservoirs can survive in mechanically inaccessible areas. Thus, deep pockets may persist or recur after mechanical therapy.
In order to maintain stable long-term results of persistent pockets after cause-related therapy, supportive therapy has to be performed in regular intervals. During supportive therapy, recurrent or persistent pockets can be treated either with repeated mechanical root debridement or with locally delivered antimicrobial devices. Both treatment modalities have drawbacks: repeated mechanical root debridement leads to loss of root substance and dentinal hypersensitivity, and local antimicrobial devices may increase the antibiotic resistance. Thus, alternative therapies are warranted.
One possible alternative may be photodynamic therapy (PDT). Organisms absorb a dye (photosensitizer) and by irradiation with light in the visible range of the spectrum, the dye will be excited to its triplet state, whose energy is transferred to molecular oxygen. The reaction product formed is highly reactive singlet oxygen, which induces cell damage or cell death. Despite of its short half-life time (4 µs in water), singlet oxygen exerts strong cytotoxic effects, destroying cellular constituents such as organelles, proteins, nucleic acids, cholesterol, etc. Microorganisms are killed by singlet oxygen, which include viruses, bacteria, protozoa, and fungi [24].
Even though the effects of photodynamic action have been known for a long time [16], interest in practical use only increased in the last years [9, 21, 39]. Since several studies have shown that killing of gram-positive, as well as gram-negative bacteria is possible [3, 11, 22], the Wilson group in London investigated different aspects of PDT application in dentistry in vitro and in vivo systems [42]. They studied the photosensitizing effects in lesions of endodontic, peri-implant, caries, or periodontal origin. Periodontal pathogens, e.g., Porphyromonas gingivalis, Prevotella intermedia, Fusobacterium nucleatum, and Parvimonas micra were killed by photodynamic action in vitro [19] and in vivo [41] by altering the membrane fluidity [4]. Reduction of the biological activities of the key virulence factors such as lipopolysaccharide and proteases may act as an additional benefit [19].
Despite the wealth of accumulated data, up to now, no established treatment protocols for the treatment of recurrent or persistent periodontal pockets exists. PDT may be a meaningful therapeutic approach since the biofilm on the root surface can be easily flushed with the dye and illuminated with light [24]. In this prospective, randomized, controlled clinical study on maintenance patients we investigated:
-
(1.)
whether a single PDT session can reduce probing depth in persistent periodontal pockets beyond what can be achieved with conventional mechanical debridement; and
-
(2.)
whether a single PDT session can change the microbial composition towards a healthier flora and decrease the total load of subgingival bacteria more than conventional periodontal therapy.
Material and methods
Patients
Sixty patients with moderate to advanced chronic periodontitis (age > 35 years, mean age, 48 ± 8 years) were selected from the maintenance pool of the Unit of Periodontology, School of Dentistry, Greifswald, Germany. The protocol of the study was approved by the Ethics Committee of the Ernst-Moritz-Arndt-University of Greifswald. Patients gave their informed consent after the study was carefully explained to them. A screening session of the patients was implemented prior to the actual recruitment, and potential pockets were identified. In order to qualify, the patients had to have at least two teeth with probing depths of >4 mm and at least ten remaining teeth. The selected teeth had to have at least one site with a probing depth >4 mm without furcation involvment. The patients in the UST control group had 3.4 ± 1.2 and in the PDT test group 3.4 ± 0.9 teeth >4 mm probing depth. The distribution of sites according to the initial probing depth and treatment group (PDT/UST) was for sites <4 mm, 330/396; 4–4.9 mm, 91/84; 5–5.9 mm, 50/67; 6–6.9 mm, 29/24; and ≥7 mm, 18/17. Initial periodontal treatment had to be completed at least 1 year previously, and patients had to receive regular supportive periodontal treatment at a 3-month interval. Patients with any of the following conditions were excluded from the study: systemic disease, use of systemic or local antibiotic therapy in the previous 6 months, pregnancy, lactation, and current smoking.
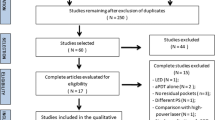
A computer-generated randomization list assigned 30 patients to the UST control group and 30 to the PDT test group. From the initially included 60 patients, six had to be excluded because five received antibiotic therapy and one developed an abscess during the observation period. Thus, we report on 25 subjects in the PDT group (eight men) and 29 subjects in the control group (seven men).
Clinical protocol
After assessment of the clinical variables during the initial examination, the patients were assigned to the test or to the control group according to the randomization list. Clinical examination was performed by a blinded investigator. During treatment, patients did not receive a detailed information on which instrument was actually used. The observation period spanned over one maintenance interval of 3 months. Clinical examination was performed at baseline and in an identical manner, 3 months later. Proper oral hygiene was reinforced in the baseline session after the clinical examination prior to instrumentation in both groups. There was no further session between baseline and the 3 months examination.
The patients of the control group (UST) were treated with Slimline® inserts (Cavitron® SPS Ultrasonic, power setting 1/4 [end of Blue zone], tips FSI-SLI and FSI-10 [Dentsply, Konstanz, Germany]; tips were chosen according to operator’s preference). Subgingival instrumentation was performed on selected teeth, irrespective of bleeding on probing; the time needed was up to the operator. The patients were motivated at each appointment to perform oral hygiene regularly. Prior to subgingival instrumentation, the supragingival plaque was dyed with a disclosing agent and removed by polishing.
In the test group, treatment was performed on selected teeth with PDT (SaveDent® Dental Laser System, Asclepion-Meditec Ltd., Fife, UK; diode laser, wavelengths 635 nm; this system has been further developed by and is now sold by Cumdente, Tübingen, Germany). The pockets were rinsed with the photosensitizer (5% tolonium chloride, Asclepion-Meditec, Fife, UK) with a blunt cannula guided along the bottom of the pocket by continuous horizontal movements to achieve a complete flushing of the pocket and root surface. Flushing with the photosensitizer was restricted to 30 s on each site. A ball-shaped laser probe (SaveDent®) was used to activate the photosensitizer. The laser was guided, like an ultrasonic probe, from the pocket bottom to the gingival margin under continuous horizontal movements in order to ensure that all areas of the pocket are irradiated. Each test surface was irradiated with a light dose of 100 mW for 1 min.
Clinical parameters
Plaque index
Plaque deposits were stained with a disclosing solution and assessed as present or absent on all teeth on six sites per tooth.
Probing depth and relative attachment level
Measurements of the probing depth (PD) and the relative attachment level (RAL) were taken at the selected teeth with a computerized probe (Florida Probe Corporation, Gainsville, Florida, USA) at six sites per tooth (mesio-, mid-, and distobuccal, and mesio-, mid-, and distolingual) by an operator experienced in the use of the probe, who was blinded for the treatment modalities. PD was measured from the free gingival margin to the base of the pocket, and RAL was measured with Florida Disc Probe® (Florida Probe Corporation), taking cusps or incisal edges as reference point. PD and RAL measurements were duplicated and averaged, respectively. Deviations in the values exceeding 0.5 mm were verified by a third measurement. If three measurements had to be conducted, the one with the highest deviation was excluded.
Bleeding upon probing
Bleeding upon probing was assessed after charting the probing depth. The percentage of sites, which bled upon probing was calculated.
Microbiology
Prior to probing at baseline and at 3 months, bacterial samples were taken from the sites, which had been identified at the screening visit. Before taking the microbiological sample, the supragingival plaque was removed with a curette, and the site was held dry using cotton rolls. Then, sterile paper tips (ISO #40, Carpgen, Münster, Germany) were inserted into the identified site of each selected tooth for 10 s and pooled for each patient. The pooled sample was analyzed for the quantitative assessment of six periodontal pathogens (Aggregatibacter actinomycetemcomitans, P. gingivalis, Tannerella forsythia, Treponema denticola, F. nucleatum, and P. intermedia), as well as for the registration of the total load of microbiota. A commercial real-time PCR test (Meridol Paro-Diagnostik, Gaba, Lörrach, Germany) was performed.
Data and statistical analysis
The power calculation was based on patient means and revealed that when the sample size is 60, there is 80% power to detect a difference in means of 0.40 mm. Additional analyses were performed in order to assess upper limits for sample size varying in standard deviation between 0.50 and 1.00 and variance of means between 0.15 (e.g., means of 1.50, 1.75, 2.20, and 2.50) and 0.40.
As a main variable, we selected probing depth; explorative analyses were performed on bleeding, probing, attachment level, and microbiology. A paired or unpaired t test was used for the analysis of probing depth, attachment level, plaque and bleeding indices. Based on initial probing depth, categories were generated for each patient: shallow sites with a PD value of 3–3.9 mm, moderate sites with 4–5 mm and 5–5.9 mm, deep sites with 6–6.9 mm, and advanced sites with ≥7 mm. All periodontal variables were averaged per patient. For the microbiological analyses, we used the Friedman test within a study group. And if this test showed a high significance, the paired comparisons were made by means of a Wilcoxon test. The analysis between the treatment modalities was performed with the Mann–Whitney U test. A significance level of p < 0.05 was assumed for all analyses (SPSS, version 11, USA).
Results
In the UST group, no adverse events or side effects (e.g., redness, swelling, or abscesses) were observed; in the PDT group, one abscess developed.
Plaque index and bleeding upon probing
The plaque index decreased from 30.5% to 24.0% in the UST group and from 33.0% to 23.8% in the PDT group (Table 1). In both groups, bleeding upon probing (BOP) did not change significantly from baseline to the re-examination (UST, baseline 4.7 to 5.7% and PDT, from 5.7 to 3.3%).
Probing depth and relative attachment level
The mean probing depth was significantly reduced from 3.3 to 3.1 mm by the ultrasonic treatment and from 3.5 to 3.3 mm by the photodynamic therapy (Table 1). The percentage of pockets >4 mm decreased from 30 to 23% in the UST group and from 33 to 29% in the PDT group; there was no significant difference between PDT and UST. In both groups, the mean probing depth of sites >4 mm was significantly reduced (UST, from 5.3 to 4.5 mm and PDT, from 5.3 to 4.7 mm). No significant difference was found between the two therapy groups both at baseline and in the final recording.
According to the baseline categories of the initial probing depths, Fig. 1 displays the mean probing depth and change of the attachment level after 3 months for the two therapy methods. In the probing depth category of 4–4.9 mm, a reduction was achieved from 4.5 to 4.0 mm (UST) and from 4.4 to 4.1 mm (PDT); in the probing depth category of 5–5.9 mm from 5.3 to 4.6 mm (UST) and from 5.3 to 4.7 mm (PDT); in the probing depth category of 6–6.9 mm from 6.4 to 5.2 mm (UST) and from 6.3 to 5.5 mm (PDT); and in the category ≥7 mm from 7.9 to 6.3 mm (UST) and from 8.0 to 6.8 mm (PDT).
Change of probing depth during the 3-month observation period split according to initial probing depth category and treatment group (PDT/UST). The distribution of sites according to the initial probing depth category and treatment group (PDT/UST) was for sites <4 mm, 396/330; ≥4–4.9 mm, 91/84; ≥5–6 mm, 50/67; ≥6–7 mm, 29/24; and ≥7 mm, 18/17
The UST sites tended to lose attachment and to have more recession than the PDT sites. Ultrasonic scaling caused an attachment loss of 0.2 mm in the pocket category 5–5.9 mm and of 0.6 mm in the pocket category 6–6.9 mm. With PDT therapy, pockets of category 5–5.9 mm gained 0.4 mm attachment.
Microbiology
The total bacterial load was reduced in the UST group from 7.5 × 107 to 6.8 × 107 directly after the treatment (p < 0.001); 3 months later, the initial microbial load was reached again (7.5 × 107, p < 0.001). In the PDT group, the total bacterial count decreased from 7.6 × 107 to 7.3 × 107 directly after the treatment (p < 0.001) and reached the baseline value of 7.6 × 107 (p < 0.004) after 3 months. The differences between the UST group and the PDT group did not vary significantly (Fig. 2). Three members of the red complex (P. gingivalis, T. forsythia, and T. denticola), according to Socransky et al. [34], was reduced more slightly with the ultrasound therapy than with the photodynamic therapy. Two members of orange complex (F. nucleatum and P. intermedia) showed a significant difference (p < 0.011) between PDT and UST at baseline, but not after treatment and after 3 months. In the UST group, the microbiota of the orange complex was reduced more slightly than in the PDT group. A. actinomycetemcomitans was only detectable in very low counts and did not show any change no matter which therapy was applied.
Log number of subgingival bacteria. Samples were taken before and directly after photodynamic treatment (PDT) or ultrasonic treatment (UST) and after 3 months of observation time. Aa Aggregatibacter actinomycetemcomitans, Pg Porphyromonas gingivalis, Tf Tannerella forsythia, Td Treponema denticola, Fn Fusobacterium nucleatum, Pi Prevotella intermedia, total total load
Discussion
The aim of this randomized, controlled single-blind pilot study was to compare the clinical and microbiological effects of PDT treatment with conventional subgingival instrumentation (UST) in persistent pockets of chronic periodontitis patients. Our hypothesis that PDT is superior to mechanical periodontal therapy was rejected. We hypothesized that flushing and insertion of the fiber-optic applicator should allow an easier access into deep pockets and thus, would lead to a significant decrease of microbial load with a concomitant improved clinical healing. We had on our mind that new devices or treatment options should be superior to conventional treatment options as long as they are more expensive. Our results correspond, however, to those of de Oliveira et al. [10] who showed in patients with aggressive periodontitis that nonsurgical treatment with PDT alone resulted in a similar pocket depth reduction as conventional scaling in cause-related phase. Considering the clinical results, both treatment groups presented a small reduction in the percentage of sites >4 mm (5–7%) and a mean PD reduction of about 0.7 mm after 3 months in sites >4 mm. If we just regard the mean change of probing depth >4 mm in nonmolars (data not shown), an improvement of about 1 mm occurred in both treatment groups. These results correspond to those found by Kocher et al. [18] where a Vector® ultrasonic device was compared with a conventional ultrasonic for the treatment of persistent pockets during the maintenance therapy. Both units achieved a 1 mm reduction of the probing depths from 5.4 to 4.4 mm. A very similar experiment was performed by Tomasi et al. [40] who treated maintenance patients with persistent pockets either with an Er:YAG laser or with an ultrasonic instrument. Both instrumentation modalities reduced the probing depth from about 6.0 to about 5.0 mm after 4 months. In a study of Chondros et al. [7], patients receiving supportive therapy were treated either with subgingival scaling followed by PDT or scaling and root planing alone. They found no difference between the test and control group in terms of PD reduction or attachment change at 3 and 6 months, but a higher improvement of BOP in the test group.
Eickholz et al. [14] investigated the effect of either scaling or exclusive subgingival application of a doxycycline gel in subjects with persistent pockets >4 mm. Six months after the treatment, both groups exhibited statistically significant reductions of probing depths (doxycycline gel, 1.4 mm and scaling, 1.1 mm). However, there were no statistically significant differences between both therapies. In a study of McColl et al. [23], sites with residual pocket probing depths ≥5 mm were repeatedly treated with minocycline gel at baseline and 3, 6, and 9 months or with scaling and root planing only at baseline as well. In both groups, a persistent reduction in the probing depths of approximately 10% to 15% was measured.
Summarizing these clinical studies with maintenance patients, we have to conclude that retreatment in sites with a residual probing depth >4 mm usually ensures only a slight clinical probing depth reduction and attachment gain [18, 23, 40]. Explanations for this observation may be that major healing effects were obtained during the cause-related phase and that such sites represent a negative selection of inaccessible sites for instruments to remove and to influence the biofilm.
The contradicting microbial results in our study and those reported in in vitro and animal studies pinpoint the problematic transfer of in vitro and animal results into clinical reality. Various in vitro studies have shown that periopathogens can effectively be killed with PDT procedures [29, 32, 35–37, 42]. These in vitro results, however, are not reflected in our clinical results. There may be different reasons for these results. Other combinations of sensitizers and light sources might be more powerful than the combination used. Sigusch et al. [33] pointed out that the success of PDT depends on the photosensitizer used. They could show in an animal study with gingivitis that chlorine e6 was more effective than BLC1010 in suppressing P. gingivalis and F. nucleatum. Another explanation is that photodestruction of plaque-residing bacteria effects less in biofilms than in a culture broth [43]. An uptake of photosensitizers into the plaque may be impeded in the same way as the uptake of antibiotic drugs. Recently, Müller et al. [25] presented a study about the efficacy of photodynamic therapy on a multispecies biofilm in vitro. In this study, PDT had a minimal effect on the viability of microorganisms organized in a biofilm.
In contrast to findings in rat and dog models [20, 33], we could not show any bactericidal efficacy to periodontal bacteria. Chondros et al. [7], who treated maintenance patients either with scaling and root planing plus PDT or root planing alone (control group), found 3 months after therapy a statistically significant reduction of F. nucleatum and Eubacterium nodatum in the PDT test group; but at 6 months, statistically higher significant numbers of Eikenella corrodens and Capnocytophaga species were detected in the test group.
In the present study, PDT treatment had no long-lasting impact on the microbial counts of periopathogens after 3 months. In both treatment groups, microbiota returned to baseline values. Similar results were reported in pharmacomechanical studies in maintenance patients. Wong et al. [44] compared scaling with the additional use of subgingival tetracycline fibers and detected a recolonization after 3 months to baseline values. McColl et al. [23] compared the short-term performance of subgingival local delivery of 2% minocycline gel and conventional subgingival debridement in maintenance patients with probing depths ≥5 mm. The prevalence of periodontal microbiota remained at levels >105 in the majority of patients and sites in both groups. To cite another study, Bogren et al. [5] evaluated the 3-year long-term effects of annual locally delivered doxycycline in maintenance patients. They reported no clinical or microbiological effects beyond those observed with mechanical debridement alone.
Since we took the microbial samples immediately after the treatment, we can exclude that the microbiota stemmed from the recolonization of the ecological niches other than the treated periodontal pocket. That means that the operator was not able to mechanically remove the bacterial load beyond 90%. This corresponds to Petersilka et al. [28] who reported that mechanical scaling reduced the cultured bacterial load of one log step in maintenance patients. Another explanation may be that bacteria have been flushed in from “healthy” not treated neighboring sites of the same tooth. Real-time PCR assays provide a better detection tool for oral pathogens than culturing [6, 17], but it do not differentiate between living and dead microbiota and PDT. Since PDT may not physically remove but only kill bacteria, it is feasible that the microbial test may not have been completely appropriate to investigate the effect of PDT on microbiota. Probably, a life/dead staining or culturing method may have better reflected the action of PDT.
This explanation is supported by findings of Dörtbudak et al. [12] who took bacterial samples before and after PDT treatment in peri-implantitis sites and cultured A. actinomycetemcomitans, P. gingivalis, and P. intermedia. PDT treatment reduced the bacterial counts by two log steps on average; complete elimination of bacteria, however, was not achieved. Rhemrev et al. [31] investigated the reduction in the number of microorganisms obtained directly after subgingival debridement by culture. Significant reductions were found for T. forsythia, P. micra, F. nucleatum, and spirochaetes. No reductions were observed for A. actinomycetemcomitans, P. gingivalis, P. intermedia, and C. rectus.
Since clinical periodontal treatment protocols have not yet been established for PDT when we started our study, we took a fiber-optic, which was developed for endodontic treatment, and followed the manufacturer's recommendations for flushing, power setting, etc. for endodontic treatment. In the meantime, systems have been introduced in the market, which are designed for periodontal use with other fiber-optic systems [10]. These new devices and adapted treatment protocols might produce better clinical outcomes. A further explanation may be that the operator did not flush the complete pocket area or did not move the laser over the complete pocket surface. It can be questioned whether pockets inaccessible to mechanical treatment devices should offer better accessibility to a laser device. Nosal et al. [26] showed that the coolant of an ultrasonic instrument does not spread lateral to the insert. Thus, if the operator was not able to rinse and stain the complete biofilm with the canule and to move the laser in regular overlapping strokes over the complete pocket area, there would still be left some microbiota without PDT treatment. Therefore, it may not be the fault of the PDT procedure itself that it did not work to our expectations; it may be the inherent problems of mechanical obstructions for devices to get access to all parts of the pocket.
As in most studies with maintenance patients [2, 18, 23, 40], in our study, no negative control subjects were included who perform only supragingival plaque control. Thus, it is not possible to estimate if the treatment effect observed had been influenced by a Hawthorne effect [1]. The trial situation presumably caused the operator and/or patient to take considerably greater effort in supra- and subgingival plaque control than it would have been the case in routine sessions. Furthermore, we did not include a control group with only irrigation or only irradiation. However, neither pocket irrigation alone [15] nor a soft-laser treatment with a low-power application alone [33, 45] has shown any clinical benefit.
This study reported similar results after retreatment of persistent pockets with UST and PDT during SPT. UST is likely to remove dental hard tissue, whereas, PDT is unlikely to do so. Thus, there are two competing therapies resulting in the same clinical effect. However, PDT is less harmful to teeth, particularly, if one considers the need of repeated retreatment over years. The sample size of this study was too small to show equivalence of UST and PDT because the power calculation was based on the assumption to detect a difference in means of 0.40 mm between UST and PDT. Future studies with more test power may confirm the equivalence of this two treatment approaches, and they should use as a secondary outcome questionnaire to assess quality of life with respect to pain
In conclusion: In our study in maintenance patients, we did not find any additional significant improvement with photodynamic therapy in terms of PD or RAL. Microbial counts reduced about 30% to 40% immediately after debridement but returned to baseline values at month 3 irrespective of treatment. Because of the pilot nature of this study, the results are too inconsistent to detect clinically relevant differences. Satisfying treatment solutions for persistent pockets sites still remain a problem. Until today, it seems that no new device or therapeutic regimen could overcome this problem and proved to have really superior clinical effects to conventional scaling devices. However, the concept of PDT is plausible and could foster new therapeutic concepts in the treatment of periodontal diseases. The knowledge available so far justifies the devotion of more research efforts to this method.
References
Adair G (1984) The Hawthorne effect: a reconsideration of the methodological artifact. J Appl Psychol 69:334–345
Bardet P, Suvan J, Lang N (1999) Clinical effects of root instrumentation using conventional steel or non-tooth substance removing plastic curettes during supportive periodontal therapy (SPT). J Clin Periodontol 26:742–747
Bertoloni G, Rossi F, Valduga G, Jori G, Ali H, van Lier JE (1992) Photosensitizing activity of water- and lipid-soluble phthalocyanines on prokaryotic and eukaryotic microbial cells. Microbios 71:33–46
Bhatti M, Mac Robert A, Henderson B, Wilson M (2002) Exposure of Porphyromonas gingivalis to red light in the presence of the light-activated antimicrobial agent toluidine blue decreases membrane fluidity. Curr Microbiol 45:118–122
Bogren A, Teles RP, Torresyap G, Haffajee AD, Socransky SS, Wennström JL (2008) Locally delivered doxycycline during supportive periodontal therapy: a 3-year study. J Periodontol 79:827–835
Boutaga K, van Winkelhoff AJ, Vandenbroucke-Grauls CM, Savelkoul PH (2006) The additional value of real-time PCR in the quantitative detection of periodontal pathogens. J Clin Periodontol 33:427–433
Chondros P, Nikolidakis D, Christodoulides N, Rössler R, Gutknecht N, Sculean A (2009) Photodynamic therapy as adjunct to non-surgical periodontal treatment in patients on periodontal maintenance: a randomized controlled clinical trial. Lasers Med Sci 24:681–688
Cugini M, Haffajee AD, Smith C, Kent RL Jr, Socransky SS (2000) The effect of scaling and root planing on the clinical and microbiological parameters of periodontal diseases: 12-month results. J Clin Periodontol 27:30–36
de Almeida JM, Theodoro LH, Bosco AF, Mj N, Oshiiwa M, Garcia VG (2008) In vivo effect of photodynamic therapy on periodontal bone loss in dental furcations. J Periodontol 79:1081–1088
De Oliveira RR, Schwartz-Filho HO, Novaes AB Jr, Taba M Jr (2007) Antimicrobial photodynamic therapy in the non-surgical treatment of aggressive periodontitis: a preliminary randomized controlled clinical study. J Periodontol 78:965–973
Dobson J, Wilson M (1992) Sensitization of oral bacteria in biofilms to killing by light from a low-power laser. Arch Oral Biol 37:883–887
Dörtbudak O, Haas R, Bernhart T, Mailath-Pokorny G (2001) Lethal photosensitization for decontamination of implant surfaces in the treatment of peri-implantitis. Clin Oral Implants Res 12:104–108
Dragoo MR (1992) Clinical evaluation of hand and ultrasonic instruments on subgingival debridement with unmodified and modified ultrasonic inserts. Int J Periodontics Restor Dent 12:310–323
Eickholz P, Kim TS, Schacher B, Reitmeir P, Burklin T, Ratka-Krüger P (2005) Subgingival topical doxycycline versus mechanical debridement for supportive periodontal therapy: a single blind randomized controlled two-center study. Am J Dent 18:341–346
Greenstein G (2005) Position paper: the role of supra- and subgingival irrigation in the treatment of periodontal diseases. J Periodontol 76:2015–2027
Henderson BW (1992) Historical perspective. In: Henderson WH, Dougherty TJ (eds) Photodynaymic therapy. Basic principles and clinical applications. Marcel Dekker, New York, pp 1–15
Jervøe-Storm PM, Koltzscher M, Falk W, Dörfler A, Jepsen S (2005) Comparison of culture and real-time PCR for detection and quantification of five putative periodontopathogenic bacteria in subgingival plaque samples. J Clin Periodontol 32:778–783
Kocher T, Fanghänel J, Schwahn C, Rühling A (2005) A new ultrasonic device in maintenance therapy: perception of pain and clinical efficacy. J Clin Periodontol 32:425–429
Kömerik N, Wilson M, Poole S (2000) The effect of photodynamic action on two virulence factors of gram-negative bacteria. Photochem Photobiol 72:676–680
Kömerik N, Curnow A, Mac Robert AJ, Hopper C, Speight PM, Wilson M (2002) Fluorescence biodistribution and photosensitising activity of toluidine blue o on rat buccal mucosa. Lasers Med Sci 17:86–92
Malik Z, Hanania J, Nitzan Y (1990) Bactericidal effects of photoactivated porphyrins—an alternative approach to antimicrobial drugs. J Photochem Photobiol B 5:281–293
Malik Z, Ladan H, Nitzan Y, Ehrenberg B (1990) The bactericidal activity of a deuteroporphyrin-hemin mixture on gram-positive bacteria. A microbiological and spectroscopic study. J Photochem Photobiol B 6:419–430
McColl E, Patel K, Dahlen G, Tonetti M, Graziani F, Suvan J, Laurell L (2006) Supportive periodontal therapy using mechanical instrumentation or 2% minocycline gel: a 12-month randomized, controlled, single masked pilot study. J Clin Periodontol 33:141–150
Meisel P, Kocher T (2005) Photodynamic therapy for periodontal diseases: state of the art. J Photochem Photobiol B 79:159–170
Müller P, Guggenheim B, Schmidlin PR (2007) Efficacy of gasiform ozone and photodynamic therapy on a multispecies oral biofilm in vitro. Eur J Oral Sci 115:77–80
Nosal G, Scheidt MJ, O’Neal R, van Dyke TE (1991) The penetration of lavage solution into the periodontal pocket during ultrasonic instrumentation. J Periodontol 62:554–557
Petersilka GJ, Tunkel J, Barakos K, Heinecke A, Häberlein I, Flemmig TF (2003) Subgingival plaque removal at interdental sites using a low-abrasive air polishing powder. J Periodontol 74:307–311
Petersilka GJ, Draenert M, Mehl A, Hickel R, Flemmig TF (2003) Safety and efficiency of novel sonic scaler tips in vitro. J Clin Periodontol 30:551–555
Pfitzner A, Sigusch BW, Albrecht V, Glockmann E (2004) Killing of periodontopathogenic bacteria by photodynamic therapy. J Periodontol 75:1343–1349
Rabbani GM, Ash MM Jr, Caffesse RG (1981) The effectiveness of subgingival scaling and root planning in calculus removal. J Periodontol 52:119–123
Rhemrev GE, Timmerman MF, Veldkamp I, van Winkelhoff AJ, van der Velden U (2006) Immediate effect of instrumentation on the subgingival microflora in deep inflamed pockets under strict plaque control. J Clin Periodontol 33:42–48
Sharkey SM, Wilson BC, Moorehead R, Singh G (1993) Mitochondrial alterations in photodynamic therapy-resistant cells. Cancer Res 52:4994–4999
Sigusch BW, Pfitzner A, Albrecht V, Glockmann E (2005) Efficacy of photodynamic therapy on inflammatory signs and two selected periodontopathogenic species in a beagle dog model. J Periodontol 76:1100–1105
Socransky SS, Haffajee AD, Smith C, Martin L, Haffajee JA, Uzel NG, Goodson JM (2004) Use of checkerboard DNA-DNA hybridization to study complex microbial ecosystems. Oral Microbiol Immunol 19:352–362
Soukos NS, Ximenez-Fyvie LA, Hamblin MR, Socransky SS, Hasan T (1998) Targeted antimicrobial photochemotherapy. Antimicrob Agents Chemother 42:2595–2601
Soukos NS, Socransky SS, Mullholland SE, Lee S, Doukas AG (2000) Photomechanical drug delivery into bacterial biofilms. Pharm Res 17:405–409
Soukos NS, Mulholland SE, Socransky SS, Doukas AG (2003) Photodestruction of human dental plaque bacteria: enhancement of the photodynamic effect by photomechanical waves in an oral biofilm model. Lasers Surg Mes 33:161–168
Stambaugh RV, Dragoo M, Smith DM, Carasali L (1981) The limits of subgingival scaling. Int J Periodontic Restor 1:30–41
Stojiljkovic I, Evavold BD, Kumar V (2001) Antimicrobial properties of porphyrins. Expert Opin Investig Drugs 10:309–320
Tomasi C, Schander K, Dahlen G, Wennström JL (2006) Short-term clinical and microbiologic effects of pocket debridement with an Er:YAG laser during periodontal maintenance. J Periodontol 77:111–118
Williams JA, Pearson GJ, Colles MJ (2006) Antibacterial action of photoactivated disinfection PAD used on endodontic bacteria in planktonic suspension and in artificial and human root canals. J Dentistry 34:363–371
Wilson M, Dobson J, Harvey W (1992) Sensitization of oral bacteria to killing by low-power laser radiation. Curr Microbiol 25:77–81
Wilson M, Pratten J (1995) Lethal photosensitisation of Staphylococcus aureus in vitro: effect of growth phase, serum, and pre-irradiation time. Lasers Surg Med 16:272–276
Wong MY, Lu CL, Liu CM, Hou L (1999) Microbiological response of localized sites with recurrent periodontitis in maintenance patients treated with tetracycline fibers. J Periodontol 70:861–868
Yilmaz S, Kuru B, Kuru L, Noyan U, Argun D, Kadir T (2002) Effect of gallium arsenide diode laser on human periodontal disease: a microbiological and clinical study. Lasers Surg Med 30:60–66
Acknowledgments
This study was, in part supported, by Sirona, Bensheim/Germany. Mandy Rothenburg treated the patients.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rühling, A., Fanghänel, J., Houshmand, M. et al. Photodynamic therapy of persistent pockets in maintenance patients—a clinical study. Clin Oral Invest 14, 637–644 (2010). https://doi.org/10.1007/s00784-009-0347-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-009-0347-4