Abstract
Objectives
The objective of this study was to evaluate the benefit of repeated subgingival cleaning with a low-concentrated hypochlorite/amino acid gel in subjects in maintenance care with residual pockets ≥ 5 mm.
Material and methods
Examiner masked, randomized two-arm parallel design. Thirty-two adult periodontal patients in maintenance phase, > 3 months after periodontal therapy, with at least one residual periodontal pocket ≥ 5 mm, were randomly assigned to treatment by subgingival ultrasonic debridement with the gel or ultrasonic debridement only. At months 0, 4, and 8, all sites presenting with a probing depth (PD) ≥ 5 mm were treated. Six sites were monitored on each tooth. The primary end point was the presence or absence of PD ≥ 5 mm after 12 months. Secondary clinical outcomes were oral tissue safety; patient acceptance; changes in PD; bleeding on probing; recession after 4, 8, and 12 months; and the presence or absence of six target microorganisms in treated pockets at baseline, after 7 days and 4 months.
Results
A total of 365 sites in 32 patients with PD ≥ 5 mm were treated at baseline. At the final evaluation at month 12, 47% of these sites in the test and 49% in the control group were still in this PD category. The difference between baseline and month 12 was significant in both groups (p < 0.01), whereas the difference between groups was not. Repeated short ultrasonic instrumentation with adjunctive administration of the test product resulted in a clinical attachment level (CAL) gain of 1.02 mm (p < 0.01) and led to − 0.97 mm of pocket reduction (p < 0.01) without inducing further recession. However, repeated short ultrasonic debridement without the gel led to a similar clinical outcome (p < 0.01). No adverse events were recorded.
Conclusions
Short ultrasonic instrumentation of residual pockets with PD ≥ 5 mm during maintenance visits resulted in a clinically relevant CAL gain and PD reduction in the order of 1 mm in 1 year, without inducing further recession.
Clinical relevance
This study corroborates the benefit of regular maintenance care after periodontal therapy, including short debridement of the residual pockets.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Periodontal diseases can be treated by thorough, professional, mechanical cleaning of microbially contaminated tooth surfaces [1]. If patients control the regrowth of bacterial biofilms with good oral hygiene practices and attend professional maintenance care on a regular basis, the results of therapy can be maintained over prolonged periods [2]. However, not all deep lesions always transform predictably into a sulcus with physiological probing depth (PD) after conventional periodontal therapy. Longitudinal studies have shown that two to four residual pockets can be counted per patient on average after general successful periodontal treatment [3, 4]. Those sites carry the risk of recolonization by bacteria forming an adherent biofilm, which endangers periodontal tissue homeostasis and increases the risk for tooth loss (for review, see [5]). Self-performed oral hygiene procedures including brushing and flossing have only limited effects on bacteria in the subgingival area [6,7,8,9]. Therefore, regular professional debridement may be required to avoid recurrence of disease.
Various mechanical instruments, such as specific curettes or ultrasonic tips, have been developed for the management of residual pockets. Despite these inventions, the long-term maintenance of sites with increased probing depth is challenging. Root planing in deep defects carries the risk of leaving small amounts of mineralized and non-mineralized bacterial deposits due to difficult access [10, 11]. Repeated instrumentation with steel curettes removes excessive amounts of cementum and dentin over time and may lead to recession of the gingival margin [12,13,14]. Local antibiotic therapy, although potentially effective [15], may contribute to the development of bacterial resistance if used regularly [16, 17]. The outcomes of various trials evaluating the potential benefit of lasers and antimicrobial photodynamic therapy have been heterogeneous and their effects rather limited [18]. Subgingival air-polishing has proven to be safe [19] and able to control the regrowth of non-mineralized bacterial deposits in a maintenance care setting without the unwanted effects of repeatedly scraping with steel curettes [20]. However, as much as these procedures may be able to remove newly formed biofilm between maintenance visits, their potential to eliminate sticky mineralized residues and toxins is limited.
Another line of investigation has recently opened up, with a new gel that is designed to aid in both the mechanical removal of hard and soft subgingival bacterial deposits and the detoxification of the root surface. The active ingredients in this gel are sodium hypochlorite (0.95%) and amino acids (glutamic acid, leucine, lysine), which create chloramines. Chloramines have a strong antimicrobial effect and can penetrate the biofilm [21, 22]. Based on studies using a similar formulation for the removal of carious dentin lesions [23], a gel mixture has been designed for subgingival use. The gel is expected to enhance the effect of scaling and root planing by softening calculus and reducing friction during instrumentation, by disrupting biofilm, by dissolving necrotic tissue, and by virtue of its antibacterial properties [24]. These effects are purportedly achieved through the chemical reaction of sodium hypochlorite with the amino acids to form N-monochloroamino acids, which, while capable of dissolving degenerated tissue, also minimize the effects of the hypochlorite on sound dentin and healthy soft tissue [25, 26]. So far, this gel has been applied exploratorily in some periodontal pockets in a limited number of patients and reported in three cases [27].
As it is customary in periodontal maintenance to clean subgingival root surfaces repeatedly, the objective of this trial was to evaluate the benefit of repeated subgingival cleaning using a gel containing sodium hypochlorite (0.95%) and amino acids (glutamic acid, leucine, lysine) as adjunct to ultrasonic debridement in maintenance therapy of periodontal sites ≥ 5 mm deep during a period of 1 year.
Material and methods
This was a single-center, examiner masked, randomized clinical trial of 12 months, with a two-arm parallel design with 1:1 allocation ratio. The Ethical Committee on human clinical research of the Canton of Geneva approved the project (#15-228). The study was conducted according to the principles outlined in the Declaration of Helsinki on human medical experimentation. Participants were informed about the procedures and signed a consent form prior to inclusion. The clinical procedures and evaluations were carried out between March 2016 and August 2018.
Subjects
Forty-four systemically healthy individuals previously treated for periodontal disease at the University Clinic of Dental Medicine, University of Geneva, Switzerland, but nevertheless with evidence for persistence of periodontal pockets, were screened for possible participation. Thirty-two of them were included based on the following criteria: in maintenance care at least 3 months after completion of comprehensive periodontal therapy, aged 20–80 years, the presence of at least one residual pocket with PD ≥ 5 mm in the area between the distal aspect of the first incisor, and the mesial aspect of the second molar. Exclusion criteria were significant illnesses or diseases that might influence or preclude subject’s participation in the study (e.g., AIDS, diabetes), therapy with any drug for at least three consecutive days within the last 28 days that might affect the outcome of the study (i.e., antibiotics, antiinflammatory medications, phenytoin), medical conditions or a history requiring prophylactic antibiotics as per the European guidelines for prophylactic and antibiotic coverage for dental treatment and systemic conditions, physical limitations or restrictions that might preclude normal oral hygiene procedures (i.e., tooth brushing), untreated dental caries, and known allergy to the test products.
Interventions
The test product (Perisolv®, Regedent AG, Zürich, Switzerland) consists of two components: (I) an uncolored gel containing amino acids (glutamic acid, leucine, lysine), carboxymethylcellulose, and ultrapure water (pH > 10) and (II) a 0.95% sodium hypochlorite solution. The two components are mixed before use to generate chloramines. The clinical procedure was as follows: Using a blunt canula, the mixed gel was dispensed into the periodontal pocket(s) until overfill as shown in Fig. 1. After 30 s, the pocket(s) were instrumented with an ultrasonic scaler (Piezon® LED, EMS Electro Medical System S.A., Nyon, Switzerland). Thereafter, the gel was applied once more to the pockets. The control treatment was subgingival ultrasonic debridement. Ultrasonic debridement was limited to 1 min per site in both groups. Treatments were carried out without local anesthesia.
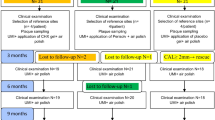
The sponsor allocated the treatments using a simple computer-generated randomization list. The clinical part of the trial was executed by two independently working dentists. Initially, the operator (AMg) enrolled the patients and selected the study sites. Next, the examiner (AZe) made the clinical measurements and took microbiological samples. Then, the operator delivered therapy to the designated sites according to protocol and randomization code. At baseline, months 4 and 8, he treated all sites with a PD ≥ 5 mm. The final evaluation was made at month 12. While the examiner was blinded with regard to all aspects of therapy, notably group allocation, the operator was not involved in the assessments.
Clinical protocol
In the areas between the distal aspect of the first incisors and the mesial aspect of the second molars, the tooth with the deepest pocket was selected as study tooth, i.e., there was one study tooth per participant. The site with the highest PD at this site was designated as the study site, i.e., there was one study tooth per participant. Root hypersensitivity (RH) was assessed, and microbiological samples were taken at this site.
On six sites of all teeth, except third molars, the following clinical parameters were recorded: Plaque Index (PI) [28], PD, bleeding upon probing (BOP), and recession (REC; positive if gingival margin located apical, negative if located coronal to the cemento-enamel junction).
A visual analogue scale (VAS) was used to assess RH as described previously [20]: Air from the three-way syringe was blown towards the tooth surface close to the gingival margin during 2 s. Then, the participants placed a mark on a horizontal line, 100 mm long, labeled with “no pain” at one end and with “worst pain” at the other. A similar VAS was used at the end of each treatment session to rate pain caused by the intervention. An examination of the oral hard and soft tissues was carried out at each visit to monitor for safety. The examination of the oral cavity included lips, tongue, gingivae, sublingual area, inner surfaces of the cheeks, mucobuccal folds, hard and soft palate, and pharyngeal area and cervical areas of all teeth. Changes in color, texture, abrasion, and any other irregularities of the soft tissue and changes of the hard tissues and dental restorations were registered.
A total of six visits were required for completion of the study:
In the first visit (day -1), the examiner measured RH at the study site; collected a subgingival plaque sample from that site; and recorded PI, PD, BOP, and REC at six sites of every tooth.
In visit 2 (day 0), the operator removed supragingival plaque, calculus, and stain from the crowns of all teeth as per the established protocol of the Division of Periodontology. He spent 5 to 10 min per person for reviewing and explaining the oral hygiene procedures including brushing and interdental cleaning. Next, he opened the randomization envelope for the subject number to reveal the treatment assignment. In the test group, all pockets ≥ 5 mm were treated with the test procedure and in the control group only with ultrasonic debridement. At the end of the session, the operator noted the total time needed for treatment and asked the patient to rate pain on a VAS.
On visit 3 (day 7 ± 1), the examiner reviewed health, oral tissue safety, and concomitant medication. She collected a subgingival plaque sample from the study site with one sterile paper point as described below.
On visit 4 (month 4, i.e., day 120 ± 4), the examiner reviewed health, oral tissue safety, and concomitant medication; collected a subgingival plaque sample from the study site; and recorded the clinical parameters. On the same day, the operator gave oral hygiene instructions in case improvement was needed. He then treated all pockets ≥ 5 mm with the allocated procedure. Time and pain were recorded as described for visit 2.
On visit 5 (month 8, i.e., day 240 ± 6), the examiner again reviewed health, oral tissue safety, and concomitant medication and recorded the clinical parameters. On the same day, the operator reviewed oral hygiene instructions if needed. He then treated all pockets ≥ 5 mm with the allocated procedure. Time and pain were recorded as described for visit 2.
On visit 6 (month 12, i.e., day 365 ± 8), the examiner again reviewed health, oral tissue safety, and concomitant medication and recorded the clinical parameters.
Microbiological procedures
Subgingival microbial samples were obtained with the paper point method. A sterile paper point was inserted to the bottom of the pocket of each study site and withdrawn after 10 s. Six periodontal microorganisms were assessed using quantitative real-time polymerase chain reaction (PCR) as previously described [29]: The genomic DNA was extracted using the GenElute Bacterial Genomic DNA Kit (Sigma-Aldrich Co., St. Louis, MO, USA) and stained with SYBR Green (Life Technologies, Carlsbad, CA, USA). Real-time PCR was carried out in a fully automated system (ABI Prism® 7900HT Sequence detection system, Applied Biosystems, Foster City, CA, USA) with the following species-specific primers [30, 31]: Aggregatibacter actinomycetemcomitans (forward: GGGGATGTACTGACGCTGAT, reverse: ACCAGGGCTAAACCCCAATC), Parvimonas micra (forward: TCG AAC GTG ATT TTT GTG GAA A, reverse: GGT AGG TTG CTC ACG TGT TAC TCA), Porphyromonas gingivalis (forward: GAGGGGCAGCATGATCTTAG, reverse: GTCCGTCTTTCAACGGGTTA), Prevotella intermedia (forward: CAAGTAGCGTGCAGGATTGA, reverse: CCGGTCCTTATTCGAAGGGTA), Tannerella forsythia (forward: GGGTGAGTAACGCGTATGTAACCT, reverse: GCCCATCCGCAACCAATAAA), and Treponema denticola (forward: CGTTCCTGGGCCTTGTACA, reverse: TTCACCCTCCTTACCAAACG). Bacterial counts were calculated by comparison with homologous reference. The detection limit was set at 1000 cells/ml.
Statistical analysis
Sites with PD ≥ 5 mm after periodontal therapy have an increased risk for tooth loss [4] and are therefore commonly considered in need for further therapy. Thus, the primary end point was the absence of PD ≥ 5 mm at the last examination (visit 6, month 12). Secondary clinical outcomes included changes in PD, BOP, REC (clinical attachment level CAL = PD + REC), and the presence of six microbial marker organisms at levels > 1000, > 10,000, and > 100,000 cells/ml, before treatment, at day 7 and month 4. The sample size for the study was chosen considering that mean PD changes in the order of 0.4 mm may be expected in 12 months of supportive periodontal care with subgingival debridement [32].
For the variables recorded at several sites in one patient, either an individual mean and standard deviation (PI, PD, REC) or the frequency and percentage (BOP) was calculated. Differences between test and control at each time point were tested for significance using the Mann–Whitney U test; longitudinal changes were analyzed using the Wilcoxon matched pairs signed rank test. Adverse events and observations concerning oral hard and soft tissues were summarized by treatment group for all evaluable subjects. Statistical software (IBM SPSS Statistics 24.0, IBM Corporation, Somers, NY, USA) was used for the analysis. p values < 0.05 were accepted for statistical significance.
Results
Thirty-two persons gave informed consent, were enrolled in the study, and were treated as allocated. All participants completed the study. Table 1 displays the baseline characteristics of the participants. There were no significant differences between the groups. A total of 4404 sites (6 per tooth at 734 teeth) were clinically monitored. Three hundred and sixty-five sites, 174 in the test, and 191 in the control group had an initial PD ≥ 5 mm and were therefore treated in the first treatment session (day 0). Table 2 shows the clinical status of the study sites (one of these sites in each participant) at baseline and after 1 year. The PD of the study sites ranged from 5 to 8 mm and was 5.78 on average. Eighty-eight percent of them showed bleeding upon probing. After 12 months of maintenance therapy, the PD of the study sites was reduced by 0.44 ± 0.73 and 0.88 ± 1.15 mm in the test and control groups, respectively. However, these improvements, as well as differences between groups, did not reach a level of statistical significance. Eighty-eight percent test and 69% control sites still showed a PD ≥ 5 mm, and the difference was not significant.
Table 3 shows the microbiological results, expressed as numbers of samples positive for six microorganisms at three thresholds (> 1000; > 10,000; > 100,000 cells/ml). There were no significant differences between groups at any threshold level. There were significant longitudinal reductions for T. forsythia in the test group from baseline to day 7 and for T. denticola from baseline to month 4.
Table 4 shows the results for all 365 sites that were treated at baseline. Per participant, there were 10.9 ± 8.3 such sites in the test and 11.9 ± 14.3 in the control group. The PD of these sites ranged from 5 to 9 mm and was 5.35 mm in mean, and 89% bled after probing. It took 372 ± 174 s per patient in the test and 238 ± 176 s in the control group to deliver the allocated treatments (p = 0.015). The perception of pain, as assessed after treatment on a VAS from 1 to 100 mm, was 19.8 ± 13.6 mm for the test and 27.6 ± 26.1 mm for the control treatment (difference non-significant). Upon questioning, the most frequent comment of participants in the test group was smelling chlorine after treatment. At month 4, periodontal probing by the examiner revealed 209 of the previously treated sites to be still in the PD ≥ 5 mm category. Consequently, 108 of them were again treated with the test and 101 with the control procedure. At month 8, the examiner revealed 196 of the same sites with a PD ≥ 5 mm. One hundred of them were once more treated with the test procedure and 96 with ultrasonic instrumentation. Figures 2 and 3 are scatterplots showing the individual PD at baseline and 12 months later of all these sites in the test and control group, respectively. At the final evaluation at 12 months, 47% of the test and 49% of the control sites displayed still a PD ≥ 5 mm (difference non-significant). Nevertheless, as Table 4 shows, a protocol of repeated short ultrasonic instrumentation with adjunctive administration of the test product resulted in a CAL gain of 1.02 mm and led to − 0.97 mm of pocket reduction without inducing further recession. However, repeated short ultrasonic debridement without the gel led to a similar clinical outcome with non-significant difference between the test and control procedures.
Discussion
The aim of this study was to evaluate the benefit of repeated short subgingival ultrasonic debridement with or without adjunctive low-concentrated hypochlorite/amino acid gel in residual pockets ≥ 5 mm over a period of 1 year. The final evaluation revealed that 47% of the test and 49% of the control sites initially ≥ 5 mm deep were still in this category. Nevertheless, repeated short ultrasonic instrumentation during periodontal maintenance, with or without adjunctive administration of the test product, resulted in a clinically relevant CAL gain and PD reduction in the order of 1 mm, without inducing further recession. It is worth noting that the participants perceived less pain after the test than after the control treatment, although this difference did not reach a level of statistical significance due to considerable inter-individual variability.
Discussing these results, it is important to keep in mind that the participants of this study presented with residual periodontal pockets despite the fact that in the past they had been treated with deep scaling and root planing. The underlying assumption of this trial was that this may have been due to persistence of microbial deposits that were not removed properly. However, there may be other reasons for non-response or re-emergence of periodontal pockets than incomplete elimination of deposits on root surfaces. Anatomical variability of subjects’ teeth, including root morphology, tilted teeth, furcation involvement, and the presence of residual infra-bony defects with complex configuration can increase the difficulty to treat residual pockets [10, 11, 33]. It is well established that good oral hygiene is required after therapy to control gingival inflammation and prevent the microbial recontamination of treated sites. Hence, one needs to distinguish refractory disease due to failure of subgingival instrumentation from re-infection due to insufficient secondary prophylaxis. As shown by the PI scores in this study, some of the persisting periodontal problems in the participants of this trial may have been due to suboptimal personal oral hygiene. In addition to good plaque control, being a non-smoker is an important factor for a successful outcome of periodontal therapy [34,35,36]. In the current study, 13% and 31% of participants were smokers in the test and control groups, respectively.
The clinically relevant CAL gains and PD reductions in the order of 1 mm, without inducing further recession, compare favorably with those obtained in other similar studies, for example, after repeated subgingival air-polishing with erythritol powder [20] or repeated antimicrobial photodynamic therapy as adjunct to ultrasonic debridement in residual periodontal pockets [37].
One hypothesis for a potential beneficial effect of the gel is that it may be able to penetrate areas difficult to access by mechanical means alone. It has been shown in the past that the difficulty to reach complete debridement of root surfaces increases with PD [10]. Therefore, the adjunctive use of the gel may be specifically useful in deep lesions. Figures 2 and 3 show the distribution of pocket depths after 12 months as a function of initial pocket depth. The slope of the regression line in Fig. 2 (test) is lower than in Fig. 3 (control), indicating a higher PD reduction in the test group especially in deep residual pockets. In addition, only one very deep pocket (PD ≥ 7 mm) persisted in the test group, while six such sites persisted in the control group. However, due to its primary objective, this study did not include a sufficiently high number of initially very deep pockets to allow a subgroup analysis for this PD range. Further studies elucidating a potentially beneficial effect in very deep residual pockets would be of clinical interest, since teeth with such residual defects have a highly increased risk for being lost in the maintenance phase [4].
As is seen in Table 3, the bacterial counts of most monitored microorganisms were generally low throughout this study. In fact, only very few sites presented with bacterial counts above > 100,000 cells/ml at baseline. Counts of a single species in the range of a few 1000 cells/ml may not be relevant for disease progression, and a further decrease may not be clinically relevant. In addition, if the counts were already low at baseline, the specific antimicrobial potential of the test product could not be evaluated. T. forsythia was a notable exception, as this microorganism was present at elevated counts in a sufficiently large number of sites to allow a meaningful comparison of the antimicrobial effects. Interestingly, in this case, a significant reduction of sites with elevated bacterial counts from baseline to day 7 was observed in the test but not in the control group. A significant reduction was also observed for T. denticola, however, in a smaller number of sites. The finding that the effect on T. forsythia was no longer significant at month 4 may be related to the fact that the hypochlorite/amino acid gel has an immediate effect and other processes may overrule this effect over time. Other studies have shown that treated sites are subject to recolonization, especially if personal oral hygiene measures are inadequate [5]. Our results indicate that the adjunctive use of the gel may be beneficial in pockets with elevated bacterial counts at least for a short time and thus provide a basis for further maintenance care. Further studies should perhaps focus on patients with residual pockets that are heavily recolonized due to lack of regular maintenance care.
Significant longitudinal reductions for T. forsythia in the test group from baseline to day 7 and for T. denticola from baseline to month 4 further reinforce the benefit of repeated intervention in residual pockets. It makes sense to clean residual pockets regularly. That does not need to be root planing with sharp steel curettes. Within the limitations of this study, our results show that even short interventions involving ultrasonic cleaning, with or without low-concentrated hypochlorite/amino acid gel, during periodontal maintenance are efficient.
References
van der Weijden GA, Timmerman FA (2002) A systematic review on the clinical efficacy of subgingival debridement in the treatment of chronic periodontitis. J Clin Periodontol 29(Suppl 3):55–71
Axelsson P, Nystrom B, Lindhe J (2004) The long-term effect of a plaque control program on tooth mortality, caries and periodontal disease in adults. Results after 30 years of maintenance. J Clin Periodontol 31(9):749–757
Mombelli A, Almaghlouth A, Cionca N, Courvoisier DS, Giannopoulou C (2015) Differential benefits of amoxicillin-metronidazole in different phases of periodontal therapy in a randomized controlled crossover clinical trial. J Periodontol 86:367–375. https://doi.org/10.1902/jop.2014.140478
Matuliene G, Pjetursson BE, Salvi GE, Schmidlin K, Brägger U, Zwahlen M, Lang NP (2008) Influence of residual pockets on progression of periodontitis and tooth loss: results after 11 years of maintenance. J Clin Periodontol 35(8):685–695. https://doi.org/10.1111/j.1600-051X.2008.01245.x
Mombelli A (2018) Microbial colonization of the periodontal pocket and its significance for periodontal therapy. Periodontol 2000 76:85–96. https://doi.org/10.1111/prd.12147
Kho P, Smales FC, Hardie JM (1985) The effect of supragingival plaque control on the subgingival microflora. J Clin Periodontol 12:676–686
Beltrami M, Bickel M, Baehni PC (1987) The effect of supragingival plaque control on the composition of the subgingival microflora in human periodontitis. J Clin Periodontol 14:161–164
Loos B, Claffey N, Crigger M (1988) Effects of oral hygiene measures on clinical and microbiological parameters of periodontal disease. J Clin Periodontol 15:211–216
McNabb H, Mombelli A, Lang NP (1992) Supragingival cleaning three times a week: the microbiological effects in moderately deep pockets. J Clin Periodontol 19:348–356
Rabbani GM, Ash MM Jr, Caffesse RG (1981) The effectiveness of subgingival scaling and root planing in calculus removal. J Periodontol 52(3):119–123
Caffesse RG, Sweeney PL, Smith BA (1986) Scaling and root planing with and without periodontal flap surgery. J Clin Periodontol 13(3):205–210
Zappa U, Smith B, Simona C, Graf H, Case D, Kim W (1991) Root substance removal by scaling and root planing. J Periodontol 62:750–754
Schmidlin PR, Beuchat M, Busslinger A, Lehmann B, Lutz F (2001) Tooth substance loss resulting from mechanical, sonic and ultrasonic root instrumentation assessed by liquid scintillation. J Clin Periodontol 28(11):1058–1066
Obeid P, Bercy P (2005) Loss of tooth substance during root planing with various periodontal instruments: an in vitro study. Clin Oral Investig 9(2):118–123. https://doi.org/10.1007/s00784-005-0309-4
Matesanz-Perez P, Garcia-Gargallo M, Figuero E, Bascones-Martinez A, Sanz M, Herrera D (2013) A systematic review on the effects of local antimicrobials as adjuncts to subgingival debridement, compared with subgingival debridement alone, in the treatment of chronic periodontitis. J Clin Periodontol 40(3):227–241. https://doi.org/10.1111/jcpe.12026
Carter GP, Schultz MB, Baines SL, Goncalves da Silva A, Heffernan H, Tiong A, Pham PH, Monk IR, Stinear TP, Howden BP, Williamson DA (2018) Topical antibiotic use coselects for the carriage of mobile genetic elements conferring resistance to unrelated antimicrobials in Staphylococcus aureus. Antimicrob Agents Chemother 62(2). https://doi.org/10.1128/AAC.02000-17
Williamson DA, Carter GP, Howden BP (2017) Current and emerging topical antibacterials and antiseptics: agents, action, and resistance patterns. Clin Microbiol Rev 30(3):827–860. https://doi.org/10.1128/CMR.00112-16
Azaripour A, Dittrich S, Van Noorden CJF, Willershausen B (2018) Efficacy of photodynamic therapy as adjunct treatment of chronic periodontitis: a systematic review and meta-analysis. Lasers Med Sci 33(2):407–423. https://doi.org/10.1007/s10103-017-2383-7
Moëne R, Décaillet F, Andersen E, Mombelli A (2010) Subgingival plaque removal using a new air-polishing device. J Periodontol 81(1):79–88. https://doi.org/10.1902/jop.2009.090394
Müller N, Moëne R, Cancela J, Mombelli A (2014) Subgingival air-polishing with erythritol during periodontal maintenance. Randomized clinical trial of twelve months. J Clin Periodontol 41(9):883–889. https://doi.org/10.1111/jcpe.12289
Gottardi W, Debabov D, Nagl M (2013) N-chloramines, a promising class of well-tolerated topical anti-infectives. Antimicrob Agents Chemother 57(3):1107–1114. https://doi.org/10.1128/AAC.02132-12
Gottardi W, Nagl M (2010) N-chlorotaurine, a natural antiseptic with outstanding tolerability. J Antimicrob Chemother 65(3):399–409. https://doi.org/10.1093/jac/dkp466
Nadanovsky P, Cohen Carneiro F, Souza de Mello F (2001) Removal of caries using only hand instruments: a comparison of mechanical and chemo-mechanical methods. Caries Res 35(5):384–389. https://doi.org/10.1159/000047478
Jurczyk K, Nietzsche S, Ender C, Sculean A, Eick S (2016) In-vitro activity of sodium-hypochlorite gel on bacteria associated with periodontitis. Clin Oral Investig 20(8):2165–2173. https://doi.org/10.1007/s00784-016-1711-9
Beeley JA, Yip HK, Stevenson AG (2000) Chemochemical caries removal: a review of the techniques and latest developments. Br Dent J 188(8):427–430
Hosoya Y, Shinkawa H, Marshall GW (2005) Influence of Carisolv on resin adhesion for two different adhesive systems to sound human primary dentin and young permanent dentin. J Dent 33(4):283–291. https://doi.org/10.1016/j.jdent.2004.09.004
Guarnelli ME, Vecchiatini R, Farina R (2015) Professional local administration of a chloramine-based treatment in conjunction with ultrasonic mechanical instrumentation: clinical outcomes in patients with deep periodontal pockets persisting following active non-surgical therapy. A 3-case report. Minerva Stomatol 64(Suppl. 1 to No. 2):158–159
Silness J, Löe H (1964) Periodontal disease in pregnancy. II. Correlation between oral hygiene and periodontal condition. Acta Odontol Scand 22:121–135
Mombelli A, Almaghlouth A, Cionca N, Cancela J, Courvoisier DS, Giannopoulou C (2017) Microbiologic response to periodontal therapy and multivariable prediction of clinical outcome. J Periodontol 88(12):1253–1262. https://doi.org/10.1902/jop.2017.170286
Kozarov E, Sweier D, Shelburne C, Progulske-Fox A, Lopatin D (2006) Detection of bacterial DNA in atheromatous plaques by quantitative PCR. Microbes Infect 8(3):687–693. https://doi.org/10.1016/j.micinf.2005.09.004
Shelburne CE, Prabhu A, Gleason RM, Mullally BH, Coulter WA (2000) Quantitation of Bacteroides forsythus in subgingival plaque comparison of immunoassay and quantitative polymerase chain reaction. J Microbiol Methods 39(2):97–107
Heasman PA, McCracken GI, Steen N (2002) Supportive periodontal care: the effect of periodic subgingival debridement compared with supragingival prophylaxis with respect to clinical outcomes. J Clin Periodontol 29(Suppl 3):163–172; discussion 195-166
Bower RC (1979) Furcation morphology relative to periodontal treatment. Furcation root surface anatomy. J Periodontol 50:366–374
Kotsakis GA, Javed F, Hinrichs JE, Karoussis IK, Romanos GE (2015) Impact of cigarette smoking on clinical outcomes of periodontal flap surgical procedures: a systematic review and meta-analysis. J Periodontol 86(2):254–263. https://doi.org/10.1902/jop.2014.140452
Patel RA, Wilson RF, Palmer RM (2012) The effect of smoking on periodontal bone regeneration: a systematic review and meta-analysis. J Periodontol 83(2):143–155. https://doi.org/10.1902/jop.2011.110130
Labriola A, Needleman I, Moles DR (2005) Systematic review of the effect of smoking on nonsurgical periodontal therapy. Periodontol 2000 37:124–137
Müller Campanile VS, Giannopoulou C, Campanile G, Cancela JA, Mombelli A (2015) Single or repeated antimicrobial photodynamic therapy as adjunct to ultrasonic debridement in residual periodontal pockets: clinical, microbiological, and local biological effects. Lasers Med Sci 30(1):27–34. https://doi.org/10.1007/s10103-013-1337-y
Funding
The work was supported by a research grant from Regedent AG, Zürich, Switzerland, the distributor of the test product.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
The Ethical Committee on human clinical research of the Canton of Geneva approved the project (#15-228).
Conflict of interest
AMo has been asked to lecture for the sponsor. The other authors report no conflict of interest related to this study.
Ethical approval
All procedures performed in this study were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
About this article
Cite this article
Megally, A., Zekeridou, A., Cancela, J. et al. Short ultrasonic debridement with adjunctive low-concentrated hypochlorite/amino acid gel during periodontal maintenance: randomized clinical trial of 12 months. Clin Oral Invest 24, 201–209 (2020). https://doi.org/10.1007/s00784-019-02949-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00784-019-02949-2