Abstract
Background
Ossification of the posterior longitudinal ligaments (OPLL) causes myelopathy with progression or trauma. Most OPLL patients visit the hospital after severe symptoms occur, and surgery did not supply complete relief in severe symptoms related to OPLL. While it is necessary to diagnose OPLL early and observe carefully, the nature of symptoms and asymptomatic OPLL have been unclear. The purposes of this study were to investigate the prevalence and symptoms of ossification of the posterior longitudinal ligaments (OPLL) of the cervical spine in the general population.
Methods
The subjects were 1291 Japanese general residents. Radiographic OPLL was detected by lateral view of the cervical spine, and subjects were classified into OPLL and non-OPLL groups. Visual analog scales of neck stiffness, neck pain, arm pain, and the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire were examined. Neck and arm symptoms were compared among the presence of OPLL, and among subtypes (continuous, segmental, and mixed types) statistically.
Results
Prevalence of OPLL was 3.7 % in overall participants, 3.9 % in symptomatic participants, and 2.2 % in asymptomatic participants. While 86.7 % of participants with OPLL had symptoms, the consultation rate was only 6.7 %. The female OPLL group had higher neck pain than the non-OPLL group, and neck function of JOACMEQ in the continuous type of OPLL was significantly restricted compared to those without OPLL and with the mixed type of OPLL.
Conclusions
Prevalence of OPLL was 3.7 %, and most of them had neck and arm symptoms; however, they did not visit hospitals. Asymptomatic OPLL had the potential risk for spinal cord injury and myelopathy. Early detection and careful observation would prevent the severe symptoms induced by OPLL.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Ossification of the posterior longitudinal ligaments (OPLL) of the spine is characterized by ectopic bone formation in the spinal ligament. Ossification of this ligament usually occurs in the cervical or thoracic spine, and less frequently in the lumbar spine [1]. OPLL regions in the cervical spine damage the spinal cord slowly and cause myelopathy [2]. Various degrees of restriction of activities of daily living related to precision motion or gait disturbance eventually require surgical treatment.
Cervical OPLL has a major impact on the society and economy. In severe myelopathy for patients with OPLL, postoperative improvement is not necessarily realized, and relatively higher incidences of surgical complications are seen compared with other cervical degeneration diseases [3, 4]. Also, neck trauma can lead to cord injury and sudden bedridden conditions in OPLL patients [5]. It has been reported that 23 % of traumatic cervical spinal cord injuries and 34 % of traumatic cervical spinal cord injuries without bony injury were related to cervical OPLL [6]. In a clinical trial, early diagnosis and careful observation effectively prevented spinal cord injuries [7]. However, only a few large cohort studies have been performed, even though such cohort studies could reveal the precise background of OPLL.
OPLL has long been considered a disease of Asian origin, and more specifically of the Japanese population, but this disorder is now being recognized in Europeans and North Americans. Previous reports showed that prevalence of radiographic OPLL in Japan was 1.9–4.3 % among orthopedic patients [2, 8, 9]. Also, cohort studies suggested that the typical age at onset is 50 years, with a male/female ratio of 2:1 [9, 10]. However, there were few cohort studies that investigated the prevalence of symptomatic OPLL and asymptomatic OPLL in general populations. Furthermore, the differences of features of symptoms between people with OPLL and the general population were unclear.
A better understanding of features of symptoms in those with OPLL will aid in appropriate diagnosis and intervention such as preventive education, medication, or surgical treatment. The purpose of this study was to investigate the prevalence of OPLL with or without symptoms in the Japanese general population. Also, influences of OPLL on their symptoms were examined. We hypothesized that there are a lot of asymptomatic and untreated people with OPLL in the general population. Furthermore, people with symptomatic OPLL have discriminative pain and symptoms.
Materials and methods
Subjects
Subjects were volunteers who participated in the Iwaki Health Promotion project. This project is a community-based program to improve average life expectancy by performing general health checkups and prophylactic interventions, and details have been shown in previous reports [11, 12]. All participants provided written informed consent, and the study was conducted with the approval of the ethics committee of Hirosaki University School of Medicine.
Subjects were recruited by calls from public health nurses and advertisements in the mass media. A total of 1305 volunteers (483 males and 822 females) from approximately 12000 residents participated in 2008 (first survey) or 2010 (second survey). Among them, 14 patients (7 males and 7 females) after neck surgery were excluded in this study to investigate features of preoperative symptoms of people with OPLL. The number of participants without neck surgery was 804 volunteers in the first survey, and 918 in the second survey. A total of 1291 (476 males and 815 females) volunteers participated in the first or second surveys, and were included for a cross-sectional statistical analysis. As a longitudinal observation, 431 participants (148 males and 283 females) were followed up in both the first and second surveys, and the follow up rate from the first survey was 53.7 %. In these 431 participants, their symptomatic data for the first survey were adopted for overall cross sectional analysis. Their mean age was 57.2 ± 14.1 (21–87) years old in males and 57.7 ± 12.9 (21–87) years old in females. All participants completed a questionnaire regarding age, gender, neck and arm symptoms, hospital visit due to those symptoms, and lifestyle habits such as smoking, drinking, and physical fitness.
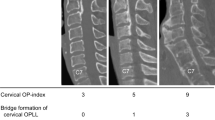
Radiographic OPLL
Plain lateral radiography of the cervical spine was taken in all participants. OPLL of the cervical spine was detected by the presence of ossification located in the region posterior to the vertebral body [13] (Fig. 1a–c). Furthermore, detected OPLL was classified into three types: continuous, segmental, and mixed. While there are four types of OPLL, there has been a concern that the circumscribed type of OPLL may be confused with degenerative spurs by radiography [14]. So, this study did not consider the circumscribed type of OPLL in order not to overestimate the prevalence of OPLL. All radiography was graded by two senior spine surgeons (A.O. and K.W.), and if their findings differed, they came to a conclusion after mutual consultation. A senior spine surgeon (A.O.) graded 100 radiographs again after a month, and the intraobserver reliability by intraclass correlation coefficient (1, 1) was 0.801.
Symptoms with OPLL
Symptoms with OPLL were evaluated by self-completed questionnaires. As the common symptoms related to cervical spine, presence and intensity of shoulder stiffness, neck pain, and arm pain, theywere measured by visual analog scales (VAS) by mm. Also, the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) was used to evaluate myelopathy related symptoms and quality of life (QOL) [15]. JOACMEQ is a valid and reliable patient-based outcome score, and consists of five subscales: neck function, upper extremity function, lower extremity function, bladder disturbance, and QOL [16]. Each subscale is converted into 0–100 points, and a higher value means good condition of their respective function.
Statistical analysis
Prevalence of OPLL was calculated in overall participants, participants with symptoms, and asymptomatic participants. Furthermore, the prevalence of OPLL among age groups [under 50 (<50), 50–59, 60–69, and 70 and older (70+)] in males and females was calculated in the overall participants. Consultation rate among OPLL subtypes was compared by the χ 2 test. Prevalence of shoulder stiffness, neck pain, and arm pain between OPLL and non-OPLL groups were compared by the χ 2 test. Furthermore, VAS between OPLL and non-OPLL groups, and VAS and JOACMEQ among the three OPLL types were compared by analysis of covariance. These values were adjusted by age, BMI, lifestyle habits (smoking, drinking, and fitness habits), and compared by the Bonferroni method. Data input and calculation were performed with the SPSS ver. 12.0J (SPSS Inc., Chicago, IL, USA). A p value of <0.05 was considered to be statistically significant.
Results
Prevalence and development of OPLL
In the cross-sectional analysis, 45 people with OPLL were detected in the overall 1291 participants, and the prevalence was 3.7 % (3.5 % in the first survey and 3.3 % in the second survey) (Table 1). Also, prevalence of OPLL in 1005 participants with neck and arm symptoms was 3.9 %. Corresponding prevalence in 286 asymptomatic participants was 2.2 %. Prevalence of OPLL in the general population increased with aging, and males from 60 to 69 years old showed the highest prevalence among age and gender groups (Fig. 2). A total of 431 participants, including 13 participants with OPLL, were followed up in both first and second surveys, and there was no evidence of new development or progression of OPLL in a 2-year longitudinal observation. In the 45 participants with OPLL, only 3 participants with OPLL (6.7 %) were treated in a hospital (Table 2).
Comparison of symptoms between non-OPLL and OPLL groups
In the OPLL group, 89.3 % of males and 82.4 % of female participants had pain between neck and arm, while 75.2 % of males and 78.8 % of female participants had corresponding pain in the non-OPLL group. Prevalence of shoulder stiffness was more than 65 % in non-OPLL and OPLL groups of both genders. There were significant differences in ratio of participants with neck pain in male OPLL group (p = 0.034) (Table 3). Furthermore, the female OPLL group showed significant strong neck pain in VAS (p = 0.021).
Comparison of symptoms among OPLL subtypes
Seven participants had a continuous type of OPLL, twenty-two had segmental type, and sixteen had the mixed type in overall participants (Table 1). While degree of VAS of shoulder stiffness in the mixed type was 36.7 mm, and was higher than the 11.3 mm in the continuous type and 19.2 mm in the segmental type, there was no significant difference (Fig. 3). On the other hand, the neck function of JOACMEQ in those with continuous type OPLL was significantly lower than those without OPLL (p = 0.011) and those with mixed type OPLL (p = 0.003) (Fig. 4). There were no differences in upper and lower extremity function, urinary function, and QOL of JOACMEQ among OPLL subtypes.
Comparison of the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire among OPLL subtypes. Values were means and standard deviations of subscales of the Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire. U/E function upper extremity function, L/E function lower extremity function, QOL quality of life
Discussion
This cohort study was focused on the symptoms with cervical OPLL in a Japanese general population, and revealed that prevalence was 3.9 % in symptomatic participants and 2.2 % in asymptomatic participants. Almost all people with OPLL had symptoms between the neck and arm; however, there were a number of non-treated people with OPLL in the Japanese general population. This study suggested that there are many people at a potential risk for cervical cord injury and possibility for prevention of this severe injury.
This study revealed that prevalence of OPLL was higher in Japan than in other countries, as has been previously reported [17, 18]. Izawa et al. [17] reported the comparative data that prevalence was 2.1 % in Japan, 1.0 % in Korea, 0.1 % in the US, and 0.1 % in Germany. Also, it is known that the prevalence of OPLL reaches a peak in the 50s to 60s in males [9, 10]. Though it appears that much cervical OPLL has occurred in this decade, it has been unclear how OPLL develops. Also, the mechanism of OPLL formation has been unclear, while previous reports suggested associations with genetic factors, and the aging process. Present results showed the increasing prevalence of OPLL with aging. Taiwan’s national registration showed the prevalence and occurrence of OPLL in a large sample analysis; however, the diagnosis and symptoms were obscure and not accurate due to the large number of patients [10]. A large, longitudinal and extensive cohort study is needed to include the development imaging and examine the risk factors.
This study showed the features of participants with symptomatic and asymptomatic OPLL. Prevalence of symptoms related to myelopathy by the presence of OPLL was not significantly high. It was considerable likelihood that myelopathy would occur only after progression of the OPLL region or in combination with dynamic factors. Neck function was restricted in those with the continuous type of OPLL. On the contrary, there were no significant differences in degree of shoulder stiffness, arm pain, upper and lower extremities function, and QOL among OPLL subtypes. A large ossified region would affect symptoms since occupation rates in mixed and continuous types are higher than in the segmental type [19]. Also, Iwasaki et al. [20] suggested that a larger ossified region leads to poorer outcome after surgical treatment. However, symptoms induced by the segmental type of OPLL are the most severe, despite its low occupation rate. A dynamic factor of the cervical spine is considered to be a potential risk factor for this dissociation. It is reported that a dynamic factor had a major impact on clinical outcome especially in the segmental and mixed type [7].
It is controversial how to detect OPLL in order to estimate its prevalence in a cohort study. There is consensus regarding the accuracy of OPLL detection by CT and images of spinal cord damage by MRI [21]. In this study, diagnosis of OPLL was performed only by radiography. Kudo et al. [14] showed the reliability of radiography by comparing with CT, and suggested their correlation was not so strong. Intraobserver reliability by intraclass correlation coefficients was 0.516 by radiographs, and 0.665 by CT and radiographs. Also, interobserver reliability was 0.817 by radiographs, and 0.832 by CT and radiographs. Analysis of OPLL regions by CT scan would increase the prevalence of OPLL; however, it is not practical or reasonable in a large sample cohort study. Also, presence of a vertebral spur makes it difficult to distinguish from the circumscribed type of OPLL [14]. This study did not consider the circumscribed type, which made it possible to prevent an overestimation of OPLL prevalence.
Even in the participants with symptomatic OPLL, the consultation rate was very low. One considerable reason was that intensity of pain was not so high. Previous study showed that OPLL patients who undergo neck surgery had strong pain (VAS ≥40 mm) or neurological symptoms from myelopathy related to cervical OPLL regions [22]. However, it is considered that postoperative symptoms of severe myelopathy remain, and even in mild myelopathy, postoperative outcome would be worse than in spondylotic myelopathy [23]. Matsunaga et al. [24] reported that 19 % of asymptomatic OPLL patients incurred myelopathy by trauma, and 64 % of OPLL patients with myelopathy had a worse progression of symptoms. Since prognosis of moderate or severe OPLL is not excellent, it is necessary to diagnose OPLL at an early stage, educate patients to avoid trauma, and continue careful observation [7].
There were several limitations in this study. First, this study did not observe the development of OPLL over a 2-year period. Though it is known that OPLL regions rarely progress, it has been unclear how these regions develop. This longitudinal study is currently being continued to overcome the limitation of the short period of observation and relative small sample size. Second, objective evaluation was limited to radiographic analysis. Examination by CT scan or extensive examination such as specific motion or deep tendon reflex would reveal symptoms in those with OPLL. Third, possible risk factors of genetic expression were not investigated. Tsuyama et al. [2] reported 23 % of OPLL patients had familial OPLL regions. Fourth, selection bias had to be considerable. Recruited volunteers are only a part of the general population, even if the participation levels were high. Also, presence and prevalence of younger population would affect these results. Fifth, how the OPLL regions affect the spinal cord was not investigated. Evaluating the signal changes in the spinal cord by MRI would help to clarify the relationship between intensity of symptoms and OPLL regions. Also, while common symptoms in neck and arm, and JOACMEQ were evaluated in this study, these symptoms would have a relationship with other musculoskeletal disorders. Less physical and functional data for myelopathy were one of the limitations of this study. On the other hand, it could be that one of the reasons for a very low consultation rate in those with OPLL that were the recruited subjects for this study was relative health, and few people had severe symptoms due to cervical myelopathy.
Despite these limitations, the prevalence of symptomatic OPLL and asymptomatic OPLL was revealed. Since early diagnosis and a preventive approach have advantages, it is important to find and observe asymptomatic OPLL patients. While many participants with OPLL were untreated in this study, this result indicated the potential decrease of spinal cord injury related to OPLL and influential information for preventive checkup.
Conclusion
Prevalence of OPLL in overall participants was 3.7 %, 3.9 % in symptomatic participants, and 2.2 % in asymptomatic participants. While most of the people with OPLL had pain between the neck and arm, there were a number of non-treated people with OPLL. This study suggested a potential risk of cervical cord injury by asymptomatic cervical OPLL and the possibility for prevention of this severe injury.
References
Schmidt MH, Quinones-Hinojosa A, Rosenberg WS. Cervical myelopathy associated with degenerative spine disease and ossification of the posterior longitudinal ligament. Semin Neurol. 2002;22:143–8.
Tsuyama N. Ossification of the posterior longitudinal ligament of the spine. Clin Orthop Relat Res. 1984;184:71–84.
Li H, Dai LY. A systematic review of complications in cervical spine surgery for ossification of the posterior longitudinal ligament. Spine J. 2011;11:1049–57.
Uchida K, Nakajima H, Sato R, Kokubo Y, Yayama T, Kobayashi S, Baba H. Multivariate analysis of the neurological outcome of surgery for cervical compressive myelopathy. J Orthop Sci. 2005;10:564–73.
Onishi E, Sakamoto A, Murata S, Matsushita M. Risk factors for acute cervical spinal cord injury associated with ossification of the posterior longitudinal ligament. Spine. 2012;37:660–6.
Chikuda H, Seichi A, Takeshita K, Matsunaga S, Watanabe M, Nakagawa Y, Oshima K, Sasao Y, Tokuhashi Y, Nakahara S, Endo K, Uchida K, Takahata M, Yokoyama T, Yamada K, Nohara Y, Imagama S, Hosoe H, Ohtsu H, Kawaguchi H, Toyama Y, Nakamura K. Acute cervical spinal cord injury complicated by preexisting ossification of the posterior longitudinal ligament: a multicenter study. Spine. 2011;36:1453–8.
Matsunaga S, Sakou T, Hayashi K, Ishidou Y, Hirotsu M, Komiya S. Trauma-induced myelopathy in patients with ossification of the posterior longitudinal ligament. J Neurosurg. 2002;97:172–5.
Shingyouchi Y, Nagahama A, Niida M. Ligamentous ossification of the cervical spine in the late middle-aged Japanese men. Its relation to body mass index and glucose metabolism. Spine. 1996;21:2474–8.
Inamasu J, Guiot BH, Sachs DC. Ossification of the posterior longitudinal ligament: an update on its biology, epidemiology, and natural history. Neurosurgery. 2006;58:1027–39.
Wu JC, Liu L, Chen YC, Huang WC, Chen TJ, Cheng H. Ossification of the posterior longitudinal ligament in the cervical spine: an 11-year comprehensive national epidemiology study. Neurosurg Focus. 2011;30:E5.
Numasawa T, Ono A, Wada K, Yamasaki Y, Yokoyama T, Aburakawa S, Takeuchi K, Kumagai G, Kudo H, Umeda T, Nakaji S, Toh S. Simple foot tapping test as a quantitative objective assessment of cervical myelopathy. Spine. 2012;37:108–13.
Sasaki E, Ishibashi Y, Tsuda E, Ono A, Yamamoto Y, Inoue R, Takahashi I, Umeda T, Nakaji S. Evaluation of locomotive disability using loco-check: a cross-sectional study in the Japanese general population. J Orthop Sci. 2013;18:121–9.
Nakamura K, Shinomiya K, Yonenobu K, Iwasaki M, Satomi K, Taguchi T, Yanaka M, Toyama Y, Matsunaga S. Clinical guidelines for ossification of the posterior longitudinal ligament (in Japanese). Tokyo: Nankodo; 2011.
Kudo H, Yokoyama T, Tsushima E, Ono A, Numasawa T, Wada K, Tanaka S, Toh S. Interobserver and intraobserver reliability of the classification and diagnosis for ossification of the posterior longitudinal ligament of the cervical spine. Eur Spine J. 2013;22:205–10.
Fukui M, Chiba K, Kawakami M, Kikuchi S, Konno S, Miyamoto M, Seichi A, Shimamura T, Shirado O, Taguchi T, Takahashi K, Takeshita K, Tani T, Toyama Y, Wada E, Yonenobu K, Tanaka T, Hirota Y, Subcommittee on Low Back Pain and Cervical Myelopathy Evaluation of the Clinical Outcome Committee of the Japanese Orthopaedic Association. An outcome measure for patients with cervical myelopathy: Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 1. J Orthop Sci. 2007;12:227–40.
Nikaido T, Kikuchi S, Yabuki S, Otani K, Konno S. Surgical treatment assessment using the Japanese orthopedic association cervical myelopathy evaluation questionnaire in patients with cervical myelopathy: a new outcome measure for cervical myelopathy. Spine. 2009;34:2568–72.
Izawa K. Comparative roentgenographical study on the incidence of ossification of the posterior longitudinal ligament and other degenerative changes of the cervical spine among Japanese, Koreans, Americans and Germans. Nippon Seikeigeka Gakkai Zasshi. 1980;54:461–74.
Matsunaga S. Updates on ossification of posterior longitudinal ligament. Epidemiology and pathogenesis of OPLL (article in Japanese). Clin Calcium. 2009;19:1415–20.
Fujimura Y, Nakamura M, Toyama Y. Influence of minor trauma on surgical results in patients with cervical OPLL. J Spinal Disord. 1998;11:16–20.
Iwasaki M, Okuda S, Miyauchi A, Sakaura H, Mukai Y, Yonenobu K, Yoshikawa H. Surgical strategy for cervical myelopathy due to ossification of the posterior longitudinal ligament: part 1: clinical results and limitations of laminoplasty. Spine. 2007;32:647–53.
Kawaguchi Y, Urushisaki A, Seki S, Hori T, Asanuma Y, Kimura T. Evaluation of ossification of the posterior longitudinal ligament by three-dimensional computed tomography and magnetic resonance imaging. Spine J. 2011;11:927–32.
Meyer SA, Wu JC, Mummaneni PV. Laminoplasty outcomes: is there a difference between patients with degenerative stenosis and those with ossification of the posterior longitudinal ligament? Neurosurg Focus. 2011;30:E9.
Sumi M. Updates on ossification of posterior longitudinal ligament. Conservative treatments for OPLL (article in Japanese). Clin Calcium. 2009;19:1480–5.
Matsunaga S, Sakou T, Taketomi E, Komiya S. Clinical course of patients with ossification of the posterior longitudinal ligament: a minimum 10-year cohort study. J Neurosurg. 2004;100:245–8.
Acknowledgments
This study was supported in part by a Grant-in-Aid from the Ministry of Education, Culture, Sports, Science and Technology of Japan (No. 18200044), Japanese Society for the Promotion of Science (No. 21500676), Health Labour Sciences Research Grant, and the JOA-Subsidized Science Project Research from the Japanese Orthopaedic Association.
Conflict of interest
The authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Sasaki, E., Ono, A., Yokoyama, T. et al. Prevalence and symptom of ossification of posterior longitudinal ligaments in the Japanese general population. J Orthop Sci 19, 405–411 (2014). https://doi.org/10.1007/s00776-014-0552-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00776-014-0552-0