Abstract
Purpose
Ossification of the posterior longitudinal ligament (OPLL) of the cervical spine has been classified into four types by lateral plain radiographs, but the reliability of the classification and of the diagnosis of either cervical OPLL or cervical spondylotic myelopathy (CSM) was unknown. We investigated the interobserver and intraobserver reliability of the classification and diagnosis for OPLL by radiographs and computed tomography (CT) images.
Methods
A total of 16 observers classified each patient’s images into five groups; OPLL continuous, segmental, mixed, circumscribed type, or CSM. To evaluate interobserver reliability, the observers first classified only radiograph images, and next both radiographs and CT images. On another day they followed the same procedure to evaluate intraobserver reliability. We also evaluated interobserver and intraobserver reliability of the diagnosis of either cervical OPLL or CSM.
Results
Interobserver reliability of the classification with radiographs only showed moderate agreement, but interobserver reliability with both radiographs and CT images showed substantial agreement. Intraobserver of reliability the classification was also improved by additional CT images. Interobserver reliability of the diagnosis with both radiographs and CT images was almost similar to with radiographs only. Intraobserver reliability of the diagnosis was improved by additional CT images.
Conclusions
This study suggested that the reliability of the classification and diagnosis for cervical OPLL was improved by additional CT images. We propose that diagnostic criteria for OPLL include both radiographs and CT images.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Ossification of the posterior longitudinal ligament (OPLL) of the spine is characterized by ectopic bone formation in the spinal ligaments. In 1960, Tsukimoto [1] first reported OPLL in Japan and OPLL is a common disorder among Japanese and other Asian populations. The incidence of OPLL in Japan is about 3 % (1.8–4.1 %) [2], and the male/female ratio for patients diagnosed as having OPLL is 1.96 (1.1–3.0) [3]. OPLL causes compression of the spinal cord and leads to various degrees of myelopathy. Typical symptoms of OPLL are sensory and motor disturbance of the upper and lower extremities, abnormal reflexes, hyperresponsive deep reflexes, and bladder-bowel dysfunction. Various degrees of dysfunction, such as precise action and gait disturbance, lead to the restriction of activities involved in daily living and the deterioration of quality of life.
The occurrence and development of OPLL involve many environmental, systemic, and local factors. Examples of factors are diet, metabolic or endocrinological background, and mechanical stress [4]. Genetic susceptibilities to OPLL have been identified by several groups. COL11A2 [5], NPPS [6], and COL6A1 [7] have been reported as candidate genes for OPLL.
According to the report of the Investigation Committee on OPLL of the Japanese Ministry of Public Health and Welfare (now the Japanese Ministry of Health, Labour, and Welfare), OPLL of the cervical spine has been classified into four types by lateral plain radiographs [8, 9]: (1) continuous; a long lesion extending over several vertebral bodies, (2) segmental; one or several separate lesions behind the vertebral bodies, (3) mixed; a combination of the continuous and segmental types, and (4) circumscribed; mainly located posterior to a disc space (Fig. 1).
The guidelines committee of the Japan Orthopaedic Association proposed that the clinical diagnostic criteria for OPLL need the radiograph findings as well as the clinical symptoms (Table 1) [10]. A small ossification area that is not visible on radiographs but can be detected only by computed tomography (CT) images does not fulfill the diagnostic definition for OPLL. Therefore, it is sometimes difficult to differentiate OPLL from cervical spondylotic myelopathy (CSM) only by radiographs. Recently, sagittal CT images are used for diagnosis of OPLL, and we can evaluate the ossification area in detail with CT images. But CT images are not included in the clinical guidelines for OPLL. (As a proposal, the use of CT images is advised.) Accurate classification and diagnosis for cervical OPLL is important for treatment and prognosis, but the reliability of the classification has not been evaluated.
The purpose of this study was to investigate the interobserver and intraobserver reliability of the classification and diagnosis for cervical OPLL by radiographs and CT images.
Materials and methods
Observers
Because experience in clinical practice was expected to affect the reliability of the classification and diagnosis, the observers were separated into two groups by their level of experience in orthopaedic surgery. One group included eight spine surgery specialists, and the other included eight residents in the orthopaedic residency programs. A total of 16 observers classified each patient’s image into five groups: continuous, segmental, mixed, circumscribed type OPLL, or CSM.
Patients and images
Fifty-seven patients (41 males and 16 females) with a diagnosis of OPLL or CSM were included in this study. The films of radiographs and CT images were scanned by computer (radiographs; 200 dpi, CT images; 300 dpi), and each image was displayed on a computer screen. The magnification of the images depended on each observer. To differentiate the ossification area clearly, we did not use CT myelography.
Evaluation for reliability
To evaluate interobserver reliability, the observers classified images only by radiographs, and next they classified by both radiographs and CT images. To evaluate intraobserver reliability, the observers followed the same procedure on another day (more than 24 h later). We used not only radiographs but also CT images to evaluate the degree of improvement of reliability, and we also evaluated difference in reliabilities between only radiographs and both radiographs and CT images. The reliability was examined with Cohen’s kappa values. Interpretation of the strength of agreement determined with the kappa values was given by adopting the criteria of Landis and Koch [11]: >0.81; Almost perfect, 0.61–0.80; Substantial, 0.41–0.60; Moderate, 0.21–0.40; Fair, 0–0.20; Slight.
Results
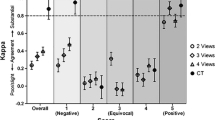
Interobserver and intraobserver reliability of the classification for cervical OPLL (Tables 2, 3)
In the first round, interobserver reliability was 0.528 with radiographs only (specialists 0.565, residents 0.476) and 0.633 using both radiographs and CT images (specialists 0.667, residents 0.623). In the second round, interobserver reliability was 0.574 with radiographs only (specialists 0.630, residents 0.526) and 0.658 using both radiographs and CT images (specialists 0.733, residents 0.622).
In the first round, interobserver reliability with radiographs only showed moderate agreement, but interobserver reliability using both radiographs and CT images showed substantial agreement. In the second round, interobserver reliability was improved in comparison with the first round.
Intraobserver reliability was 0.477 with radiographs only (specialists 0.561, residents 0.392) and 0.605 using both radiographs and CT images (specialists 0.665, residents 0.544). Intraobserver reliability of residents with radiographs only was fair. Intraobserver reliability was improved by additional CT images.
Interobserver and intraobserver reliability of the diagnosis of either cervical OPLL or CSM (Tables 4, 5)
We also evaluated interobserver and intraobserver reliability of the diagnosis of either cervical OPLL or CSM. In the first round, interobserver reliability was 0.743 with radiographs only (specialists 0.758, residents 0.812) and 0.833 using both radiographs and CT images (specialists 0.710, residents 0.753). In the second round, interobserver reliability was 0.787 with radiographs only (specialists 0.817, residents 0.878) and 0.853 using both radiographs and CT images (specialists 0.832, residents 0.823). If the observers are separated into specialists and residents, interobserver reliability obtained using both radiographs and CT images was lower than that with radiographs only in each observer group. But interobserver reliability in all observers using both radiographs and CT images improved in comparison with radiographs only. By additional CT images, interobserver reliability of the diagnosis showed almost perfect agreement.
Intraobserver reliability of the diagnosis was 0.613 (specialists 0.690, residents 0.537) with radiographs only and 0.802 (specialists 0.795, residents 0.808) using radiographs and CT images. Intraobserver reliability was improved by additional CT images.
Case presentation (Fig. 2)
Case 1
Using only radiograph, ten observers classified this case as CSM. Although the ossification area was unclear by radiograph, 15 observers classified it as cervical OPLL by additional CT image.
Case 2
All 16 observers classified this case as circumscribed cervical OPLL by additional CT image.
Case 3
By radiograph, eight observers classified this case as mixed cervical OPLL and the other eight observers classified it as continuous cervical OPLL. By additional CT image, 13 observers classified it as mixed cervical OPLL and the other three observers classified it as continuous cervical OPLL.
Discussion
In Clinical Guidelines for OPLL (Table 1) [10], diagnostic criteria for OPLL include requirements of radiographic images and clinical findings. According to the requirements of radiographic images, the ossification area must be visible in lateral plain radiograph, and a small ossification area that is visible in only CT images is not included in OPLL. If the lower cervical spine is not visible adequately by lateral plain radiograph, CT images are advised.
Chang et al. [12] reported inter- and intra-observer variability of cervical OPLL classification using reconstructed CT images. In their study, the inter- and intra-observer kappa values were 0.51 and 0.67 by the lateral radiograph, 0.70 and 0.85 by 2-D CT images. The reliability of their study was higher than that of our study.
In our study, interobserver and intraobserver reliability of classification for the cervical OPLL was improved by additional CT images. In lateral plain radiographs, facet joints of the cervical spine may overlap with the ossification area. Intervertebral bone spurs may also overlap with circumscribed OPLL. In contrast, we could not observe such overlaps in CT images. Interobserver reliability of specialists was higher than that of residents, and the reliability of residents was remarkably improved in comparison with that of spine surgery specialists by additional CT images. It seems that experience in clinical practice affects the interobserver and intraobserver reliability. The influence of experience in clinical practice may be reduced by CT images.
Interobserver reliability of the diagnosis for cervical OPLL was improved by additional CT images, and intraobserver reliability was improved remarkably. The criteria for OPLL seemed to affect the results. According to the current criteria for OPLL, it is difficult to evaluate an ossification area that is visible on CT image clearly but difficult to identify on plain radiograph.
It is well known that the ossification area is often progressive during the natural course of the disease. Shindo et al. [13] reported the long-term natural course of OPLL. Progression of the ossification was detected in 38 % of segmental OPLL, 75 % of continuous OPLL, and 55 % of mixed OPLL, but it was not related to aggravation of the myelopathy. OPLL often progresses after surgery, which may cause late-onset neurological deterioration. Kawaguchi et al. [14] reported the relationship between the progression of ossification of the OPLL and the clinical results following en bloc cervical laminoplasty. Young patients with mixed and continuous types OPLL had the greatest risk for progression. Some patients had neurological deterioration following an increase in the thickness of the ossification. Hori et al. [15] reported on 55 patients after cervical laminoplasty who were available for serial radiographs for more than 5 years. The patients were divided into three groups according to the pattern of OPLL progression. OPLL progression related to patient age or OPLL type. In genetic study, it was reported that mixed or continuous type OPLL had higher osteogenic differentiation potency than segmental or circumscribed type OPLL [16]. As above, patients with mixed or continuous OPLL had the greatest risk for progression of the ossification area. It is important for prognosis and diagnosis that reliability of the classification for cervical OPLL has high agreement. We will work out the new classification for cervical OPLL by advanced CT images.
CT images were very valuable on the classification and diagnosis for cervical OPLL; however, there were some problems. One problem was the cost. CT images of cervical spine cost about three times more than radiographs of cervical spine in Japan. Another problem was the radiation dosage to the patients. The radiation dose of CT images of cervical spine was about 17 times higher than that of radiographs of cervical spine in our institute (The radiation dosage of CT images of cervical spine was 61.8 mGy and that of radiographs of cervical spine was 3.6 mGy). In terms of the cost and the radiation dosage, CT images were not repeatable test.
This study suggested that interoberver and intraobserver reliability of the classification for cervical OPLL was improved by additional CT images, which also improved intraobserver reliability of the diagnosis for cervical OPLL. We propose that diagnostic criteria for OPLL include both radiographs and CT images.
References
Tsukimoto H (1960) A case report-autopsy of syndrome of compression of spinal cord owing to ossification within spinal canal of cervical spines. Arch Jpn Chir 29:1003–1007
Sakou T, Matsunaga S (1996) Ossification of the posterior longitudinal ligament. J Jpn Spine Res Soc 7:437–448 (in Japanese)
Terayama K, Kurokawa T, Seki H (1975) National survey of ossification of the posterior longitudinal ligament. In: Investigation Committee 1975 report on the ossification of the spinal ligaments of the Japanese Ministry of Public Health and Welfare, pp 8–33 (in Japanese)
Furukawa K-I (2008) Pharmacological aspect of ectopic ossification in spinal ligament tissues. Pharmacol Ther 118:352–358
Koga H, Sakou T, Taketomi E et al (1998) Genetic mapping of ossification of the posterior longitudinal ligament of the spine. Am J Hum Genet 62:1460–1467
Nakamura I, Ikegawa S, Okawa A et al (1999) Association of the human NPPS gene with ossification of the posterior longitudinal ligament of the spine (OPLL). Hum Genet 104:492–497
Tanaka T, Ikari K, Inoue I et al (2003) Genomewide linkage and linkage disequilibrium analyses identify COL6A1, on chromosome 21, as the locus for ossification of the posterior longitudinal ligament of the spine. Am J Hum Genet 73:812–822
Investigation Committee on OPLL of the Japanese Ministry of Public Health and Welfare (1981) The ossification of the longitudinal ligament of the spine (OPLL). J Jpn Orthop Assoc 55:425–440
Yonenobu K, Nakamura K, Toyama Y (eds) (2006) OPLL ossification of the posterior longitudinal ligament. Springer, Japan
Nakamura K, Shinomiya K, Yonenobu K et al (2005) Clinical guidelines for ossification of the posterior longitudinal ligament (in Japanese). Nankodo, Tokyo
Landis JR, Koch GG (1977) The measurement of observer agreement for categorical data. Biometrics 33:159–174
Chang H, Kong C-G, Park J-B et al (2010) Inter- and intra-observer variability of a cervical OPLL classification using reconstructed CT images. Clin Orthop Surg 2:8–12
Shindo S, Yamaura I et al (2004) Long-term clinical course of ossification the posterior longitudinal ligament in the cervical region. Rinsyo Seikeigeka 39:445–452 (in Japanese)
Kawaguchi Y, Kanamori M, Ishihara H et al (2001) Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am 83:1798–1802
Hori T, Kawaguchi Y, Kimura T et al (2006) How does the ossification area of the posterior longitudinal ligament progress after cervical laminoplasty. Spine 31:2807–2812
Kudo H, Furukawa K-I, Toh S et al (2011) Genetic differences in the ostenogenic differentiation potency according to the classification of ossification of the posterior longitudinal ligament of the cervical spine. Spine 36:951–957
Acknowledgments
We thank the Spine Surgery group in the Department of Orthopaedic Surgery of Hirosaki University Graduate School of Medicine and Drs. Taisuke Nitobe and Naoki Echigoya for providing film samples, and Drs. Takashi Tomita, Syuichi Aburakawa, Takeuchi Kazunari, Akira Saito, Masaki Kishiya, Ryoko Uesato, Takuya Naraoka, Yoshimitsu Hayashi, Kozo Kato, and Yuka Kimura for classifying and making a diagnosis for OPLL.
Conflict of interest
None of the authors has any potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kudo, H., Yokoyama, T., Tsushima, E. et al. Interobserver and intraobserver reliability of the classification and diagnosis for ossification of the posterior longitudinal ligament of the cervical spine. Eur Spine J 22, 205–210 (2013). https://doi.org/10.1007/s00586-012-2573-8
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00586-012-2573-8