Abstract
Introduction
To evaluate the differences in the associations of combinations of co-existent osteopenia, obesity, and/or sarcopenia with insulin resistance (IR) according to different criteria of obesity.
Materials and methods
Among 4500 Korean men and postmenopausal women who were aged ≥ 50 years and did not have diabetes mellitus, osteopenia, sarcopenia, and obesity were defined using bone mineral density, skeletal mass index, and body fat % (or BMI). Body composition groups were generated based on the combinations of these components. IR was defined using the HOMA-IR ≥ 2.5.
Results
When obesity was defined by body fat % and the relationships were adjusted for age, sex, education, and health behaviors, the odds ratios (ORs) for IR was highest in the groups with obesity and osteopenic obesity, followed by sarcopenic obesity and osteosarcopenic obesity, followed by osteopenia and sarcopenia, and followed by osteosarcopenia. When BMI was additionally adjusted, the ORs for IR were not significantly different between body composition groups except for osteopenia: those groups had higher ORs for IR compared to osteopenia. When obesity was defined by BMI, obesity co-existent groups had higher ORs for IR than the obesity non-coexistent groups. The ORs for IR were not significantly different within obesity co-existent groups or obesity non-coexistent groups.
Conclusions
Combinations of co-existent osteopenia, obesity, and/or sarcopenia had different associations with IR according to obesity classification methods and consideration of BMI adjustment. Osteosarcopenic obesity may not have a stronger association with IR compared to obesity only and obesity co-existent other conditions.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Aging is associated with a decrease in bone and muscle mass and an increase in body fat mass. These changes in body composition are due to osteosarcopenic obesity (OSO), a simultaneous deterioration of bone and muscle and excess fat [1,2,3]. The development of OSO may be linked to low-grade chronic inflammation initiated by overweight/obesity and lifestyle factors, such as inadequate dietary intake and low physical activity levels [1]. Studies have suggested that a combined body composition derangement may be associated with reduced functionality and cardiometabolic risk factors [3]. OSO was associated with poor functionality in postmenopausal women [4], with poor physical performance and frailty in Mexican women aged ≥ 50 years [5], and with hypertension and dyslipidemia in Chinese women [6, 7].
Insulin resistance (IR), which is frequently assessed using the homeostasis model assessment of insulin resistance (HOMA-IR) in population-based studies, is an underlying pathophysiological factor of the metabolic syndrome and represents an intermediate state between obesity and type 2 diabetes mellitus [8]. It has been suggested that higher upper-body fat distribution [9], both excess and lack of adipose tissue [10], a relatively low muscle mass [11], sarcopenia [12], and a high-fat mass irrespective of muscle mass [13] and bone mineral density (BMD) [14] are associated with insulin sensitivity or IR. Based on the evidence of associations of excess/low body fat, sarcopenia/low muscle mass, and low BMD with IR, the strengths of associations of co-existent osteopenia, obesity, and sarcopenia with IR may differ according to the combinations of these components. However, the differences in the associations of these combinations with clinical outcomes, such as IR, remain unclear [15]. Meanwhile, it is unclear clinical advantage of examination of body components over simple body mass index (BMI) measurement, as well as the scientific significance of component-specific effect on IR, excluding BMI variability.
Therefore, this study aimed to evaluate the associations of the combinations of osteopenia, obesity, and/or sarcopenia, such as osteopenic obesity, osteosarcopenia, sarcopenic obesity, and OSO with IR with considering for BMI variability and those association with respect to BMI-based obesity classification using the Korean National Health and Nutrition Examination Survey (KNHANES).
Materials and methods
Study participants
The participants were a representative sample of the civilian, noninstitutionalized Korean population included in the KNHANES that was conducted during 2008–2011. The survey used a multistage, stratified, systematic sampling method and a rolling survey sampling of household units [16, 17]. The current study included 2067 men and 2.433 women aged between 50 and 80 years who participated in the KNHANES and provided complete data related to body composition measures, metabolic risk factors, health behaviors, and demographic characteristics; those who had a diagnosis of diabetes mellitus and premenopausal women were excluded. Informed consent was obtained from all individual participants included in the study. The study protocol was approved by the institutional review board of Korea Centers for Disease Control and Prevention (IRB approval number: 2008-04EXP-01-C, 2009-01CON-03-2C, 2010-02CON-21-C, and 2011-02CON-06-C) [16].
Body composition measurements and categorization
Dual-energy X-ray absorptiometry (Discovery QDR4500W, Hologic Inc., Bedford, MA, USA) was used to measure BMD at the lumbar spine, femoral neck, and proximal femur, the fat percentage for the whole body (fat mass/total mass × 100), and lean masses at the four extremities. Appendicular skeletal muscle mass was calculated as the sum of the muscle masses of the four extremities that were computed as lean mass minus bone mineral content.
The skeletal mass index was calculated as the sum of the muscle mass of the four limbs divided by the height square (kg/m2). The sarcopenia was defined as a skeletal mass index < 7.0 kg/m2 for males and < 5.7 kg/m2 for females based on the Asian Working Group for Sarcopenia (AWGS) criteria [18].
Osteopenia was defined as a T score of ≤ − 1.0 standard deviation for BMD at the lumbar spine, femoral neck, or proximal femur [19]. Obesity was defined using total body fat % or BMI: total body fat ≥ 25% for men and ≥ 35% for women, based on the findings from a Mongolian study [20] or BMI ≥ 25 kg/m2 [21]. BMI was calculated using the measured bodyweight (kg) divided by the square of the height (m).
Four groups based on a number of unfavorable body composition components defined by body fat % or BMI for obesity classification were generated [22]. Accordingly, participants were divided into normal (without osteopenia, obesity, or sarcopenia), single component (having any one of these components), two components (having any two combinations of these components), and OSO groups.
Measurements of IR, demographic, and lifestyle-related factors
Antecubital venous blood samples taken after a 12-h overnight fast were used to measure glucose (calorimetry method) and insulin (immunoradiometric assay) with an automated analyzer (Automatic Chemistry Analyzer 7600, Hitachi, Tokyo, Japan). IR was defined based on HOMA-IR, which was calculated as fasting plasma glucose (mmol/L) × fasting insulin (mU/mL)/22.5) [23]. The cutoff value of HOMA-IR for IR was ≥ 2.5 [24]. Self-reported questionnaires were also used to assess educational attainment, current smoking status (smoker vs. non-smoker), physical activity (yes vs. no for engaging in high-intensity activity for > 75 min/week or moderate-intensity activity for > 150 min/week), and alcohol use (yes vs. no for the frequency of alcohol consumption ≥ 1 month during the past year).
Statistical analyses
The comparison of unfavorable body composition components, body composition groups, demographic factors, and health behaviors by HOMA-IR levels was performed using a Chi square test or t test. The association of each body composition component with IR were analyzed using logistic regression analysis after adjusting for sex, age, education level, smoking status, physical activity, alcohol use, and other body composition components. Similarly, multivariable logistic regression analyses were performed for associations between body composition groups and IR, using different reference groups. These analyses were conducted for body composition groups based on different criteria of obesity. In the analysis for body composition groups based on body fat %, all analyses were adjusted additionally for BMI to consider the potential effect of BMI variability. Sex-specific analysis was not performed due to an insufficient number of subjects in some body composition groups according to classification methods. Data were analyzed using IBM SPSS Statistics for Windows, version 25.0 (IBM Corp., Armonk, NY, USA).
Results
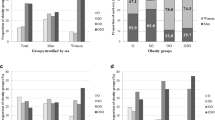
In this representative sample of the Korean men and postmenopausal women who were aged 50 years or older and did not have diabetes mellitus, the prevalence of OSO based on body fat% or BMI was respectively 5.8% and 0.4% in men and 7.2% and 0.7% in women. The prevalence of IR was 33.4%. Individuals with IR were more likely to have obesity and a higher number of unfavorable body composition components, while they are less likely to have osteopenia and sarcopenia compared to those without IR (Table 1).
Table 2 presents the associations of an individual or combined body composition components with IR. Individuals with high body fat % had a higher odds ratio (OR) of IR regardless of adjusting for other body composition components and BMI. Osteopenia had an inverse association with IR after adjusting for other body composition components, while the association was not more significant after additionally adjusting for BMI. By contrast, sarcopenia was negatively associated with IR after adjusting for other body composition components, while the association was changed to be positive with adjustment for BMI. Individuals with OSO based on body fat % had higher OR of IR than those without any unfavorable body composition components or only one such component, after adjusting for confounding factors and BMI (Table 2).
In Table 3, the associations with IR are compared among groups with one or more adverse body composition components. Obesity and osteopenic obesity based on body fat % were associated with higher ORs of IR compared to other groups including OSO, while the OR of IR in osteopenic obesity was not significantly different than that in obesity. Sarcopenic obesity based on body fat % was associated with higher OR of IR compared to osteosarcopenia. There was no significant difference in OR of IR between osteopenia and sarcopenia when those groups did not have co-existent obesity. However, osteopenia with obesity was associated with higher OR of IR compared to sarcopenia with obesity. Therefore, IR was most related to obesity or osteopenic obesity, followed by sarcopenic obesity or OSO, followed by osteopenia or sarcopenia, and followed by osteosarcopenia, before adjusting for BMI.
After additionally adjusting for BMI, the ORs of IR in obesity co-existent groups were attenuated, while those ORs in sarcopenia co-existent groups increased. Then, the strengths of association with IR were similar between the groups with unfavorable body composition components except for osteopenia. However, those groups (except for sarcopenic obesity) were associated with higher ORs of IR compared to osteopenia.
When obesity was defined based on BMI, the groups with co-existent obesity were associated with higher ORs of IR compared to the groups without co-existent obesity. However, there were no significant differences in ORs with IR within obesity co-existent groups or obesity non-coexistent groups (Table 3).
Discussion
In this representative sampling of Korean men and postmenopausal women who were aged 50 years or older and did not have diabetes mellitus, IR was most related to obesity or osteopenic obesity, followed by sarcopenic obesity or OSO, followed by osteopenia or sarcopenia, and followed by osteosarcopenia, when obesity was defined by body fat % and the relationships were not adjusted for BMI. When BMI was additionally adjusted, the strengths of association with IR were similar between body composition groups except for osteopenia and those groups had stronger associations with IR than osteopenia. When obesity was defined by BMI, obesity co-existent groups had stronger associations with IR compared to the groups without co-existed obesity. However, the strengths of association were not different within groups with co-existent obesity or groups without co-existent obesity.
The current findings considering BMI variability suggested that adjustment of BMI may attenuate the associations between obesity co-existent groups and IR, while it may increase the associations between sarcopenia co-existent groups and IR. The findings from BMI-based obesity criteria suggested that osteopenia and sarcopenia may increase the strength of association with IR when co-existent with obesity. However, regardless of both obesity classification methods, the current study did not demonstrate OSO may have a stronger association with IR than other obesity co-existent groups or obesity only group.
Although numerous studies have reported the associations of fat mass, muscle mass, or BMD with IR [9,10,11,12,13,14], the current study is unique in terms of presenting a comparison of the associations of the combinations of co-existent osteopenia, obesity, or sarcopenia with IR. Considering the paucity of previous studies on associations between OSO and clinical outcomes, the current observation appears to provide evidence that an individual with OSO would not be at a higher risk of IR than those with obesity, osteopenic obesity, or sarcopenic obesity. These findings are of value as there is limited evidence on the health impact of osteoporosis co-morbid with obesity and sarcopenia [15].
Consensus for the criteria of OSO may be critical for comparing studies regarding the prevalence of OSO and the relationship between OSO and clinical/functional outcomes [15, 19].Although the definition of osteopenia is widely accepted, substantial debate still exists regarding the definition of sarcopenia and even obesity [25, 26]. Therefore, the low prevalence of OSO in the current study (0.4–5.8% in men and 0.7–7.2% in women) compared to that in a previous Korean study (13.5% in men and 25.0% in women) [27] may be explained by the inconsistent criteria for defining sarcopenia and obesity between the studies. At least, the current study revealed that the prevalence of OSO based on body fat % for obesity definition may be higher than that prevalence based on BMI. The criteria used to define these conditions may influence the association strengths between the various body composition groups and IR due to the effects on statistical power by changing the number of participants in the body composition groups. Although specific cut-off points for each component have yet to be determined, the current findings demonstrated the concurrent obesity is likely associated with a worse risk of IR than the risk induced by osteopenia, sarcopenia, or osteosarcopenia in the absence of obesity.
Despite growing evidence of shared mechanisms among excess adiposity and decreased bone mass and skeletal muscle mass [3, 15], the current study revealed discrepancies in the associations between each of these components and IR: a positive association for obesity, a positive or a neutral association for sarcopenia, and a neutral association for osteopenia according to obesity classification methods when other body composition groups or BMI were adjusted. These differences in the associations with IR among those components may explain the findings that individuals with any one component did not have with a greater risk of IR than those without any of these components in body composition groups based on body fat %. However, the current study also demonstrated that individuals with any combination of two or three components had a greater risk of IR than those with any one of these components. These findings suggested the possibility of additive or synergic effects of co-existing components on the strength of the associations with IR.
This study had some limitations. The causal relationships between co-existent adverse body composition components and IR remain to be determined. Potential confounding factors, such as medications for osteoporosis and dietary habits related to body composition and/or IR, were not fully adjusted in current statistical analyses. In addition, sex-specific associations were not examined due to insufficient sample size in the OSO group. Nevertheless, this study had strengths in terms of demonstrating differences in associations with IR through a comparison of the combinations of concurrent osteopenia, obesity, and sarcopenia in a representative population. Another strength of this study may be presenting changes in the associations of body composition groups with IR after adjustment with BMI variability.
In conclusion, in Korean men and postmenopausal women who were aged 50 years or older and did not have diabetes mellitus, obesity and osteopenic obesity may have stronger associations with IR compared to OSO, sarcopenic obesity, or osteosarcopenia when obesity was defined by body fat %. Those differences in strengths of association with IR between body composition groups were not more significant with adjustment for BMI. When obesity was defined by BMI, the strengths of association with IR were not significantly different within groups with co-existent obesity or groups without co-existent obesity, although IR had stronger associations with obesity co-existent groups than the groups without co-existent obesity. Therefore, combinations of co-existent osteopenia, obesity, and/or sarcopenia had different associations with IR according to obesity classification methods and consideration of BMI adjustment. Further prospective studies are warranted to elucidate long-term clinical outcomes associated with unfavorable body composition groups.
References
Ilich JZ, Kelly OJ, Inglis JE (2016) Osteosarcopenic obesity syndrome: what is it and how can it be identified and diagnosed? Curr Gerontol Geriatr Res 2016:7325973
Ilich JZ, Kelly OJ, Inglis JE, Panton LB, Duque G, Ormsbee MJ (2014) Interrelationship among muscle, fat, and bone: connecting the dots on cellular, hormonal, and whole body levels. Ageing Res Rev 15:51–60
Kelly OJ, Gilman JC, Boschiero D, Ilich JZ (2019) Osteosarcopenic obesity: Current knowledge, revised identification criteria and treatment principles. Nutrients. https://doi.org/10.3390/nu11040747
Ilich JZ, Inglis JE, Kelly OJ, McGee DL (2015) Osteosarcopenic obesity is associated with reduced handgrip strength, walking abilities, and balance in postmenopausal women. Osteoporos Int 26:2587–2595
Szlejf C, Parra-Rodriguez L, Rosas-Carrasco O (2017) Osteosarcopenic obesity: prevalence and relation with frailty and physical performance in middle-aged and older women. J Am Med Dir Assoc 18:733.e1–733.e5
Chen X, Kong C, Yu H, Gong J, Lan L, Zhou L, Gong J, Liu P, Xu L, Deng Q (2019) Association between osteosarcopenic obesity and hypertension among four minority populations in china: a cross-sectional study. BMJ Open 9:2018–026818
Mo D, Hsieh P, Yu H, Zhou L, Gong J, Xu L, Liu P, Chen G, Chen Z, Deng Q (2018) Osteosarcopenic obesity and its relationship with dyslipidemia in women from different ethnic groups of China. Arch Osteoporos 13:65018-0481-1
Shanik MH, Xu Y, Skrha J, Dankner R, Zick Y, Roth J (2008) Insulin resistance and hyperinsulinemia: is hyperinsulinemia the cart or the horse? Diabetes Care 31:S262–S268
Karpe F, Pinnick KE (2015) Biology of upper-body and lower-body adipose tissue–link to whole-body phenotypes. Nat Rev Endocrinol 11:90–100
Goossens GH (2017) The metabolic phenotype in obesity: fat mass, body fat distribution, and adipose tissue function. Obes Facts 10:207–215
Srikanthan P, Karlamangla AS (2011) Relative muscle mass is inversely associated with insulin resistance and prediabetes findings from the third national health and nutrition examination survey. J Clin Endocrinol Metab. 96:2898–2903
Mesinovic J, Zengin A, De Courten B, Ebeling PR, Scott D (2019) Sarcopenia and type 2 diabetes mellitus: a bidirectional relationship. Diabetes Metab Syndr Obes 12:1057–1072
Kim K, Park SM (2018) Association of muscle mass and fat mass with insulin resistance and the prevalence of metabolic syndrome in korean adults: a cross-sectional study. Sci Rep 8:2703018-21168-5
Conte C, Epstein S, Napoli N (2018) Insulin resistance and bone: a biological partnership. Acta Diabetol 55:305–314
Bauer JM, Cruz-Jentoft AJ, Fielding RA, Kanis JA, Reginster JY, Bruyere O, Cesari M, Chapurlat R, Al-Daghri N, Dennison E, Kaufman JM, Landi F, Laslop A, Locquet M, Maggi S, McCloskey E, Perna S, Rizzoli R, Rolland Y, Rondanelli M, Szulc P, Vellas B, Vlaskovska M, Cooper C (2019) Is there enough evidence for osteosarcopenic obesity as a distinct entity? A critical literature review. Calcif Tissue Int 105:109–124
Korea centers for disease control and prevention. Guidelines for using the fifth national healthy and nutition examination survey (KNHANES V-3), 2012. In, osong, chungcheong buk-do, Republic of Korea
Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K (2014) Data resource profile: the Korea National Health and Nutrition Examination Survey (KNHANES). Int J Epidemiol 43:69–77
Chen LK, Liu LK, Woo J, Assantachai P, Auyeung TW, Bahyah KS, Chou MY, Chen LY, Hsu PS, Krairit O, Lee JS, Lee WJ, Lee Y, Liang CK, Limpawattana P, Lin CS, Peng LN, Satake S, Suzuki T, Won CW, Wu CH, Wu SN, Zhang T, Zeng P, Akishita M, Arai H (2014) Sarcopenia in Asia: consensus report of the asian working group for sarcopenia. J Am Med Dir Assoc 15:95–101
Kelly OJ, Gilman JC, Boschiero D, Ilich JZ (2019) Osteosarcopenic obesity: current knowledge, revised identification criteria and treatment principles. Nutrients. https://doi.org/10.3390/nu11040747
Li Y, Wang H, Wang K, Wang W, Dong F, Qian Y, Gong H, Xu G, Li G, Pan L, Zhu G, Shan G (2017) Optimal body fat percentage cut-off values for identifying cardiovascular risk factors in mongolian and han adults: a population-based cross-sectional study in inner Mongolia. China. BMJ Open 7:e014675
The international association for the study of obesity and the international obesity task force. the asia-pacific perspective: Redefining obesity and its treatment. australia: IASO and IOTF, 2000
Chen X, Kong C, Yu H, Gong J, Lan L, Zhou L, Gong J, Liu P, Xu L, Deng Q (2019) Association between osteosarcopenic obesity and hypertension among four minority populations in china: a cross-sectional study. BMJ Open 9:e026818
Matthews DR, Hosker JP, Rudenski AS, Naylor BA, Treacher DF, Turner RC (1985) Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28:412–419
Lee YH, Kim SU, Song K, Park JY, Kim DY, Ahn SH, Lee BW, Kang ES, Cha BS, Han KH (2016) Sarcopenia is associated with significant liver fibrosis independently of obesity and insulin resistance in nonalcoholic fatty liver disease: nationwide surveys (KNHANES 2008–2011). Hepatology 63:776–786
Prado CM, Wells JC, Smith SR, Stephan BC, Siervo M (2012) Sarcopenic obesity: a critical appraisal of the current evidence. Clin Nutr 31:583–601
Ormsbee MJ, Prado CM, Ilich JZ, Purcell S, Siervo M, Folsom A, Panton L (2014) Osteosarcopenic obesity: the role of bone, muscle, and fat on health. J Cachexia Sarcopenia Muscle 5:183–192
Kim J, Lee Y, Kye S, Chung YS, Kim JH, Chon D, Lee KE (2017) Diet quality and osteosarcopenic obesity in community-dwelling adults 50 years and older. Maturitas 104:73–79
Acknowledgements
This work was funded by the National Research Foundation of Korea Grant funded by the Korean Government (NRF-2017S1A5B8066096).
Author information
Authors and Affiliations
Contributions
Author contributed to design this study, analyze the data, and write the manuscript.
Corresponding author
Ethics declarations
Conflict of interest
There are no conflicts of interest to declare.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
About this article
Cite this article
Lee, K. Association of osteosarcopenic obesity and its components: osteoporosis, sarcopenia and obesity with insulin resistance. J Bone Miner Metab 38, 695–701 (2020). https://doi.org/10.1007/s00774-020-01104-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-020-01104-2