Abstract
Sarcopenia and osteoporosis are both significant health burdens among postmenopausal women. This study examined associations between sarcopenia and osteopenia/osteoporosis in Japanese women and evaluated the prevalence of sarcopenia in women with osteopenia and osteoporosis. A total of 2400 Japanese women aged 40–88 years underwent dual-energy x-ray absorptiometry (DXA) scans of the whole body, lumbar spine, and total hip. Osteopenia and osteoporosis were defined according to World Health Organization criteria using bone mineral density (BMD) of the lumbar spine or hip. Sarcopenia was defined as a relative skeletal muscle index (RSMI) more than 2 standard deviations below the mean for a young adult reference population, calculated as the appendicular skeletal muscle mass (ASM) obtained from whole-body DXA divided by height in meters squared (RSMI = ASM/height2). Significant and marginal/moderate positive correlations were observed between RSMI and lumbar spine/total hip BMDs (r = 0.197 and r = 0.274, respectively; p < 0.0001 each). The BMDs of the lumbar spine and total hip showed significant moderate negative correlations with age (r = −0.270 and r = −0.375, respectively; p < 0.0001 each), but RSMI showed no association with age in this population (r = 0.056). When osteopenia/osteoporosis was defined using lumbar spine BMD, prevalences of sarcopenia in subjects with normal BMD, osteopenia and osteoporosis were 10.4, 16.8, and 20.4 %, respectively. When osteopenia/osteoporosis was defined using total hip BMD, the prevalences of sarcopenia in these subjects were 9.0, 17.8, and 29.7 %, respectively. A Chi-square test for independence showed a significant association between sarcopenia and osteopenia/osteoporosis (p < 0.0001). These results indicate that sarcopenia is significantly associated with osteopenia and osteoporosis in Japanese women.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a worldwide health problem that is age-related and three times more common in women than in men [1]. The loss of bone mass is a potent risk factor for fragility fractures, and osteoporosis-induced fractures represent a major burden on society [1]. Lifetime risk for hip, vertebral and forearm (wrist) fractures has been estimated as approximately 40 %, similar to that for coronary heart disease [1].
Sarcopenia is defined as the age-associated loss of skeletal muscle mass and function [2]. Sarcopenia is very common in older individuals, with a reported prevalence in 60- to 70-year-olds of 5–13 %, and a prevalence in >80-year-olds of 11–50 % [3]. Sarcopenia increases the risk of falls [4, 5], which enhance fragility fractures including osteoporotic hip fractures. The risk of falls appears more closely related to risk of limb fracture than bone mineral density (BMD) [6]. Concomitant sarcopenia and osteopenia/osteoporosis thus represents a greater risk than osteopenia/osteoporosis alone for limb fractures.
Several factors that play important roles in causing sarcopenia also contribute to bone loss, such as age-related decreases in levels of sex steroid hormones [7, 8], impaired growth hormone and insulin-like growth factor-I signaling and activity with aging [9, 10], and changes in nutritional status, including vitamin D insufficiency [11]. Previous studies have shown a positive association between lean mass and BMD in postmenopausal women [12, 13]. Sarcopenia and osteoporosis may thus act together. The prevalence of sarcopenia has been reported as 10–52 % in the postmenopausal population, depending on the reference method used and the population examined [2]. However, the prevalence of sarcopenia in osteopenic and osteoporotic women has not been fully evaluated.
Given this background, the aims of this study were to examine associations between sarcopenia and osteopenia/osteoporosis in Japanese women ≥40 years old, and to evaluate the prevalence of sarcopenia among Japanese women with osteopenia and osteoporosis.
Materials and methods
Subjects
A total of 2400 consecutive women ≥40 years old (range, 40–88 years) who visited our orthopedic outpatient clinic and underwent whole-body and regional (lumbar spine and total hip) dual-energy X-ray absorptiometry (DXA) (QDR 4500A; Hologic, Waltham, MA, USA) were enrolled in this study. All subjects were orthopedic patients who had minor symptoms (i.e., sprain, contusion, transient joint pain, etc.) and requested examination for osteoporosis, or were examinees in a regional screening program for osteoporosis who were referred to our clinic for confirmation of whether osteoporosis was present. All subjects were informed about the objectives of DXA and consented. Subjects with a past history of medication using anti-osteoporosis drugs, malignancy, corticosteroid use, bone metabolic disorders other than osteoporosis (i.e., osteomalacia, hyperparathyroidism, etc.), paralysis or inability to walk for any reason (i.e., myelopathy, paraplegia, severe osteoarthritis, etc.) were excluded.
Definitions of osteopenia and osteoporosis
Osteopenia and osteoporosis were diagnosed using the criteria of the World Health Organization (WHO) [1]. Osteopenia was defined as a BMD more than 1.0 standard deviation (SD) below the young adult mean, but less than 2.5 SDs below this value (T-score < –1 and > –2.5), and osteoporosis was defined as a BMD 2.5 SDs or more below the young adult mean (T-score ≤ –2.5). The BMDs were measured from DXA of the lumbar spine (L2–L4) and total hip.
Sarcopenia definition
From the whole-body composition data obtained using DXA, appendicular skeletal muscle mass was calculated as the sum of skeletal muscle mass in the arms and legs, assuming that all non-fat and non-bone tissue is skeletal muscle [14, 15]. The DXA measurement methods and validation have been reported elsewhere [16, 17]. Relative skeletal mass index (RSMI) was derived from the appendicular skeletal muscle mass in kilograms divided by the square of the height in meters [14, 18]. Sarcopenia was considered present for an RSMI more than 2 SDs below the mean in young women [14]. In this study, the cut-off value for sarcopenia (<5.46 kg/m2 for women) was referenced from normative data from the Japanese population using the same DXA device (QDR 4500A; Hologic) [19].
Prevalences of sarcopenia, osteopenia, and osteoporosis
The 2400 subjects were divided into five groups according to age decade: 40–49 (n = 105); 50–59 (n = 459); 60–69 (n = 825); 70–79 (n = 874); and 80–89 (n = 137) years. Prevalences of sarcopenia, osteopenia, and osteoporosis in each age group were then estimated. Prevalences of sarcopenia in subjects with osteopenia or osteoporosis in the total study population and in each age group were further calculated.
Statistical analyses
The correlation between estimated variables was analyzed using Pearson’s correlation coefficient and simple regression analysis. Further analyses using multiple regression were conducted to evaluate the impact of RSMI on BMD. The association between sarcopenia and osteopenia/osteoporosis was investigated using the Chi-square test for independence. Values of p < 0.05 were considered statistically significant.
Results
Characteristics of the 2400 participants in this study are shown in Table 1. The correlations between variables are listed in Table 2. Significant and marginal/moderate positive correlations were observed among RSMI and lumbar spine/total hip BMDs. The RSMI showed a strong positive correlation with BMI. Age showed a significant, marginal positive correlation with BMI and a significant, marginal/moderate negative correlations with lumbar spine/total hip BMDs.
Multiple regression analysis on lumbar spine BMD using age, BMI, and RSMI as independent variables identified age and BMI as significant contributors for lumbar spine BMD, but RSMI did not reach the level of statistical significance (Table 3). Multiple regression analysis for total hip BMD revealed that in addition to age and BMI, RSMI was also selected as a significant contributor to total hip BMD (Table 4).
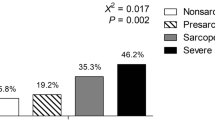
A Chi-square test for independence showed a significant association between sarcopenia defined using RSMI and osteopenia/osteoporosis defined using both lumbar spine BMD and total hip BMD (p < 0.0001).
When osteopenia and osteoporosis were defined using lumbar spine BMD, the prevalence of osteopenia increased after the 50s and the prevalence of osteoporosis gradually increased with age (Fig. 1). When osteopenia and osteoporosis were defined by total hip BMD, prevalence of osteopenia increased with age decade, but decreased slightly in the 80s , while the prevalence of osteoporosis increased exponentially with age group (Fig. 2). Prevalence of sarcopenia as defined using RSMI in this population was higher in the 40s compared to other age groups, and after the 50s , the prevalence appeared to almost plateau (Fig. 3).
In both definitions of osteopenia/osteoporosis by BMD measurement of the lumbar spine and total hip, the prevalence of sarcopenia defined with RSMI in subjects with osteopenia (16.8 or 17.8 %) was higher than the prevalence of sarcopenia in subjects with normal BMD (10.4 or 9.0 %), and the prevalence of sarcopenia in subjects with osteoporosis (20.4 or 29.7 %) was higher than the prevalence of sarcopenia in subjects with osteopenia. This relationship (lowest prevalence of sarcopenia in subjects with normal BMD and highest in osteoporotic subjects) was observed in all age groups (Figs. 4, 5).
Discussion
Sarcopenia and osteoporosis represent significant health burdens among postmenopausal women [5]. Associations with sarcopenia and osteopenia/osteoporosis in women have been reported in several studies. Gillette-Guyonnet et al. [20] reported that among 129 healthy French women, appendicular skeletal muscle mass was significantly lower in osteoporotic women than in age- and sex-matched non-osteoporotic controls. Walsh et al. [18] investigated the prevalence of sarcopenia defined using RSMI in 213 healthy pre- and postmenopausal volunteers in the United States (97 % Caucasian) and reported that the prevalence of sarcopenia in that sample was 11.7 %, with prevalences of 12.5 % in premenopausal osteopenic women, 25 % in postmenopausal women with osteopenia, and 50 % in postmenopausal women with osteoporosis. Di Monaco et al. [4] recently assessed the prevalence of sarcopenia evaluated with RSMI and associations with osteoporosis in 313 hip-fracture women, and reported that 58 % of subjects were sarcopenic, whereas 74 % were osteoporotic. They concluded that the high prevalence of sarcopenia and its significant association with osteoporosis was present in a sample of hip-fracture women [4]. The present study with a larger number of Japanese women demonstrated significant associations of lumbar spine/total hip BMD and RSMI, and the prevalence of sarcopenia was highest in osteoporotic subjects, followed by osteopenic subjects, and lowest in normal BMD subjects in all age decade groups from the 40 s to 80 s.
A study from the Third National Health and Nutrition Examination Survey (NHANES III) in the United States showed that prevalence of sarcopenia in women as estimated using bioelectrical impedance analysis (BIA) increased with age [21]. In the present study, osteopenia and osteoporosis were significantly associated with age, as with the wider literature including a report from the WHO [1]; however, RSMI and sarcopenia showed no significant association with age. Although the evaluation method in this study (RSMI) differed from that used in NHANES III (BIA), this discrepancy warrants closer attention. Study samples in the present study may have been biased compared to the normal population, because all participants in this study were subjects visiting an orthopedic clinic. Thus, the study participants might have had several underlying diseases/conditions modifying muscle mass and thus affecting the results. However, a cohort survey in Japan with a sample size of 2419 participants aged in their 40–80s showed that muscle strength (grip and knee extensor) decreased significantly with age in both men (n = 1200) and women (n = 1219), although age-related declines in the prevalence of sarcopenia as evaluated using RSMI were observed only in men, not in women [22]. Kirchengast et al. [23] also reported that significant age-related declines in lean body mass as evaluated with RSMI were observed only in men, not in women, among 282 healthy Austrian subjects aged 60–92 years. The reasons why these studies did not show age-related increases in sarcopenia among women remain unclear, but sex-specific differences may exist when sarcopenia is evaluated using RSMI.
In the present study, significant positive correlations between lumbar spine BMD and total hip BMD were observed, as previously reported [24]. However, multiple regression analysis showed that a significant impact of RSMI on BMD was only seen for total hip BMD, and not for lumbar spine BMD. We speculated that this discrepancy between total hip and lumbar spine BMDs might have been primarily attributable to the existence of spondylosis, which affects lumbar spine BMD. Although we could not evaluate the degree of spondylosis because spine X-rays were not available for many participants in this study population, previous studies have shown that lumbar osteophyte formation and intervertebral disc degeneration correlate positively with BMD [24]. In addition, from the perspective of muscle and bone interactions, RSMI of the arms and legs is considered to have a more significant relationship with BMD from an extremity (total hip BMD) rather than spine BMD.
The importance of BMD measurement for osteopenia/osteoporosis screening is widely accepted [1]. Screening for sarcopenia should also now be considered, because sarcopenia represents a major cause of disability and increased health costs, particularly among older individuals [2]. In this study, BMD and RSMI were simultaneously examined by DXA. As suggested by Walsh et al. [18], simultaneous screening for sarcopenia during BMD examinations by DXA may be of value in identifying osteopenic/osteoporotic women with sarcopenia, a group that may be most in need of exercise interventions to increase muscle and BMD.
Several limitations should be addressed. First, the definition of sarcopenia in this study only referred to RSMI, because the majority of diagnostic thresholds for sarcopenia have been developed based on this method [2, 5, 14, 18, 19, 25]. However, muscle mass does not correlate directly with muscle strength [5], and the European Working Group on Sarcopenia in Older People (EWGSOP) recommends the diagnosis of sarcopenia based on documentation of low muscle mass plus low muscle function (strength or performance) [25]. If we could have evaluated muscle function in addition to muscle mass in this study, age-related associations between sarcopenia and osteopenia/osteoporosis might have become more apparent. In future studies, for example, walking velocity should be included as a functional parameter in the definition of sarcopenia. Second, although the sample size was considered large, the present data cannot be generalized to the overall population, because the subject cohort may have suffered selection bias in that all subjects had visited orthopedic clinics. Further community-based studies with normal populations to evaluate both muscle mass and function are required to confirm the present findings.
In conclusion, this study examined associations between sarcopenia and osteopenia/osteoporosis in a total of 2400 Japanese women. The RSMI showed significant positive correlations with BMDs of the lumbar spine and total hip. Prevalence of sarcopenia defined with RSMI was highest in subjects with osteoporosis, followed by subjects with osteopenia, and lowest in subjects with normal BMD. These results suggest that sarcopenia is significantly associated with osteopenia and osteoporosis in Japanese women. However, the results should be interpreted with care, as the subject cohort may have suffered selection bias in that all subjects had visited orthopedic clinics.
References
WHO Scientific Group (2003) Prevention and management of osteoporosis. World Health Organ Tech Rep Ser 921:1–164
Fielding RA, Vellas B, Evans WJ, Bhasin S, Morley JE et al (2011) Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. International working group on sarcopenia. J Am Med Dir Assoc 12:249–256
Morley JE (2008) Sarcopenia: diagnosis and treatment. J Nutr Health Aging 12:452–456
Di Monaco M, Vallero F, Di Monaco R, Tappero R (2011) Prevalence of sarcopenia and its association with osteoporosis in 313 older women following a hip fracture. Arch Gerontol Geriatr 52:71–74
Sirola J, Kröger H (2011) Similarities in acquired factors related to postmenopausal osteoporosis and sarcopenia. J Osteoporos 2011:536735
Kaptoge S, Benevolenskaya LI, Bhalla AK, Cannata JB, Boonen S et al (2005) Low BMD is less predictive than reported falls for future limb fractures in women across Europe: results from the European Prospective Osteoporosis Study. Bone 36:387–398
Douchi T, Yamamoto S, Nakamura S, Ijuin T, Oki T, Maruta K, Nagata Y (1998) The effect of menopause on regional and total body lean mass. Maturitas 29:247–252
Messier V, Rabasa-Lhoret R, Barbat-Artigas S, Elisha B, Karelis AD, Aubertin-Leheudre M (2011) Menopause and sarcopenia: a potential role for sex hormones. Maturitas 68:331–336
Kasukawa Y, Miyakoshi N, Mohan S (2004) The anabolic effects of GH/IGF system on bone. Curr Pharm Des 10:2577–2592
Perrini S, Laviola L, Carreira MC, Cignarelli A, Natalicchio A, Giorgino F (2010) The GH/IGF1 axis and signaling pathways in the muscle and bone: mechanisms underlying age-related skeletal muscle wasting and osteoporosis. J Endocrinol 205:201–210
Visser M, Deeg DJ, Lips P (2003) Low vitamin D and high parathyroid hormone levels as determinants of loss of muscle strength and muscle mass (sarcopenia): the Longitudinal Aging Study Amsterdam. J Clin Endocrinol Metab 88:5766–5772
Blain H, Vuillemin A, Teissier A, Hanesse B, Guillemin F, Jeandel C (2001) Influence of muscle strength and body weight and composition on regional bone mineral density in healthy women aged 60 years and over. Gerontology 47:207–212
Douchi T, Oki T, Nakamura S, Ijuin H, Yamamoto S, Nagata Y (1997) The effect of body composition on bone density in pre- and postmenopausal women. Maturitas 27:55–60
Baumgartner RN, Koehler KM, Gallagher D, Romero L, Heymsfield SB, Ross RR, Garry PJ, Lindeman RD (1998) Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 147:755–763
Delmonico MJ, Harris TB, Lee JS, Visser M, Nevitt M, Kritchevsky SB, Tylavsky FA, Newman AB (2007) Alternative definitions of sarcopenia, lower extremity performance, and functional impairment with aging in older men and women. J Am Geriatr Soc 55:769–774
Visser M, Fuerst T, Lang T, Salamone L, Harris TB (1999) Validity of fan-beam dual-energy X-ray absorptiometry for measuring fat-free mass and leg muscle mass. Health, aging, and body composition study–dual-energy X-ray absorptiometry and body composition working group. J Appl Physiol 87:1513–1520
Salamone LM, Fuerst T, Visser M, Kern M, Lang T, Dockrell M, Cauley JA, Nevitt M, Tylavsky F, Lohman TG (2000) Measurement of fat mass using DEXA: a validation study in elderly adults. J Appl Physiol 89:345–352
Walsh MC, Hunter GR, Livingstone MB (2006) Sarcopenia in premenopausal and postmenopausal women with osteopenia, osteoporosis and normal bone mineral density. Osteoporos Int 17:61–67
Sanada K, Miyachi M, Tanimoto M, Yamamoto K, Murakami H, Okumura S, Gando Y, Suzuki K, Tabata I, Higuchi M (2010) A cross-sectional study of sarcopenia in Japanese men and women: reference values and association with cardiovascular risk factors. Eur J Appl Physiol 110:57–65
Gillette-Guyonnet S, Nourhashemi F, Lauque S, Grandjean H, Vellas B (2000) Body composition and osteoporosis in elderly women. Gerontology 46:189–193
Janssen I, Heymsfield SB, Ross R (2002) Low relative skeletal muscle mass (sarcopenia) in older persons is associated with functional impairment and physical disability. J Am Geriatr Soc 50:889–896
Shimokata H, Ando F (2011) Epidemiology of sarcopenia (in Japanese). Mod Physician 31:1283–1287
Kirchengast S, Huber J (2012) Sex-specific associations between soft tissue body composition and bone mineral density among older adults. Ann Hum Biol 39:206–213
Miyakoshi N, Itoi E, Murai H, Wakabayashi I, Ito H, Minato T (2003) Inverse relation between osteoporosis and spondylosis in postmenopausal women as evaluated by bone mineral density and semiquantitative scoring of spinal degeneration. Spine (Phila Pa 1976) 28:492–495
Cruz-Jentoft AJ, Baeyens JP, Bauer JM, Boirie Y, Cederholm T, Landi F, Martin FC, Michel JP, Rolland Y, Schneider SM, Topinková E, Vandewoude M, Zamboni M (2010) Sarcopenia: European consensus on definition and diagnosis: report of the European working group on sarcopenia in older people. Age Ageing 39:412–423
Acknowledgments
This study was supported by the 2011 Research Encouragement Award from the Japan Osteoporosis Society.
Conflict of interest
None of the authors have any conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Miyakoshi, N., Hongo, M., Mizutani, Y. et al. Prevalence of sarcopenia in Japanese women with osteopenia and osteoporosis. J Bone Miner Metab 31, 556–561 (2013). https://doi.org/10.1007/s00774-013-0443-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-013-0443-z