Abstract
Hyperhomocysteinemia has been shown to increase the incidence of osteoporosis and osteoporotic fractures. Endoplasmic reticulum (ER) stress was recently shown to be associated with apoptosis in several types of cells. In this study, we determined the effect of homocysteine (Hcy) on the apoptosis of osteoblastic cells and investigated whether ER stress participates in Hcy-induced osteoblast apoptosis. Human osteoblastic cells were incubated with Hcy. Hcy dose-dependently decreased cell viability and increased apoptosis in osteoblastic cells. Osteoblastic cells are more susceptible to Hcy-mediated cell death than other cell types. Expression of cleaved caspase-3 was significantly increased by Hcy, and pretreatment with caspase-3 inhibitor rescued the cell viability by Hcy. Hcy treatment led to an increase in release of mitochondrial cytochrome c. It also triggered ER stress by increased expression of glucose-regulated protein 78, inositol-requiring transmembrane kinase and endonuclease 1α (IRE-1α), spliced X-box binding protein, activating transcription factor 4, and C/EBP homologous protein. Silencing IRE-1α expression by small interfering RNA effectively suppressed Hcy-induced apoptosis of osteoblastic cells. Our results suggest that hyperhomocysteinemia induces apoptotic cell death in osteoblasts via ER stress.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Osteoporosis is a skeletal disease characterized by low bone mass and microarchitectural deterioration of bone tissue, which results in increased bone fragility and susceptibility to fracture [1, 2]. An imbalance between bone resorption by osteoclasts and bone formation by osteoblasts is the main mechanism leading to osteoporosis and bone fragility [2]. In postmenopausal and glucocorticoid-induced osteoporosis, increased apoptosis of osteoblasts is observed and the rate of apoptosis of osteoblasts determines, in part, the amount of bone and its microarchitecture [3, 4]. Osteoporosis is a highly prevalent disease and results in massive costs both to the individual and to society through associated fragility fractures [1, 5]. Therefore, it is important to understand the risk factors and the pathogenic mechanisms of osteoporosis and to establish a preventive strategy.
Homocysteine (Hcy) is a sulfur-containing amino acid that plays pivotal roles in the metabolism of methionine, the biosynthesis of nucleic acids, protein methylation, and the biosynthesis of neurotransmitters and phospholipids [6]. Severe hyperhomocysteinemia is found in patients with homocysteinuria, an inherited disorder of amino acid metabolism, and is associated with osteoporosis and cardiovascular disease at a very young age [7, 8]. It has been reported that elevated serum Hcy level is associated with low bone mineral density and increased risk of fracture in longitudinal observational studies [9, 10]. Hcy-lowering treatment, such as folate and vitamin B12, reduces the risk of hip fracture [11]. Animal studies have shown a shift of bone metabolism towards bone resorption and a significant reduction of bone quality in hyperhomocysteinemic animals [12, 13]. Therefore, Hcy is now considered a risk factor for osteoporosis as well as cardiovascular diseases [14].
The endoplasmic reticulum (ER) is mainly recognized as a protein-folding factory, responsible for the biosynthesis, folding, assembly and modification of numerous soluble proteins and membrane proteins. Disturbance in the normal functions of the ER (ER stress) leads to an evolutionarily conserved cell stress response, the unfolded protein response (UPR), which is aimed initially at compensating for damage but can eventually trigger cell death if ER dysfunction is severe or prolonged [15]. ER stress was shown to be involved in Hcy-induced apoptosis of endothelial cells in atherosclerosis, hepatocytes in alcoholic liver disease and neuronal cells in various neurodegenerative diseases [16–19]. Meanwhile, overexpression of C/EBP homologous protein (CHOP), which appears as a result of excessive ER stress, suppresses bone formation by attenuating the function and differentiation of osteoblasts or inducing apoptosis of osteoblasts [20, 21].
Therefore, we hypothesized that decreased bone mineral density and increased risk of fracture by hyperhomocysteinemia is due to the decline of bone formation by Hcy-induced apoptosis of osteoblasts and that ER stress is involved in that process. In this study, we investigated the ability of Hcy to induce apoptosis in osteoblastic cells in vitro and examined the functional involvement of ER stress.
Materials and methods
Reagents
The pan-caspase inhibitor, Z-VAD-fmk, was purchased from Calbiochem (La Jolla, CA, USA); Hcy was purchased from Sigma-Aldrich (St. Louis, MO, USA); antibodies against B-cell lymphoma 2 (Bcl-2), Bcl-2-associated X protein (Bax), CHOP, and activating transcription factor 4 (ATF4) were from Santa Cruz Biotechnology (Santa Cruz, CA, USA). Antibodies to cytochrome c were also from Santa Cruz Biotechnology. Antibodies against caspase-3, glucose-regulated protein 78 (GRP78), inositol-requiring transmembrane kinase and endonuclease 1α (IRE-1α) and spliced X-box binding protein (sXBP-1) were purchased from Abcam (Cambridge, UK).
Cell culture
This work was approved by the Institutional Review Committee of the Catholic Medical Center, Catholic University of Korea. Informed consent for use of the isolated cells was obtained from all patients and healthy controls.
The human osteosarcoma cell line, U2OS, and the human normal osteoblast cell line, HNOst, were purchased from the Korean Cell Line Bank (Seoul, Korea) and LONZA (Basel, Switzerland), respectively. These cell lines were cultured in RPMI 1640 medium containing 10% fetal calf serum (FCS) at 37°C in a humidified chamber of 5% carbon dioxide (CO2).
The human umbilical vein endothelial cells (HUVECs) were isolated from normal-term umbilical cord vein by collagenase digestion, and then grown to confluence in 75 cm2 flasks containing M199 medium (Life Technologies) supplemented with 20% FCS, 100 U/ml penicillin, 100 μg/ml streptomycin, and 2 mM l-glutamine. Cultures were kept at 37°C in a CO2 incubator, and the medium was changed every 2–3 days until confluence was reached. HUVECs were passed with 0.2% collagenase and 0.02% ethylenediaminetetraacetic acid (EDTA) (Life Technologies); cells from passages 2–3 were used in this study.
The fibroblast-like synoviocytes (FLS) were prepared from the synovial tissues of patients with knee osteoarthritis who had undergone total joint replacement surgery. The isolation of the FLS from the synovial tissues was performed according to a procedure described previously [22]. The purity of the cells was confirmed by flow cytometry analysis (>95% CD90, <2% CD14, <1% CD3, and <1% CD19 positive). FLS, from passages 3 through to 8, were used for each experiment.
Dermal fibroblasts were obtained from three healthy controls during plastic surgery. Fibroblasts were grown from explants in Dulbecco’s modified Eagle’s medium (DMEM) at 37°C in 5% CO2. The cells were then centrifuged at 500g, resuspended in DMEM supplemented with 10% FCS, 2 mM glutamine, penicillin (100 U/ml) and streptomycin (100 μg/ml), and plated in 25-cm2 flasks. The culture medium was replaced every 3 days. When cells approached confluence, they were detached with trypsin, passed after dilution 1:3 with fresh medium, and recultured until use. Cells were housed at 37°C in a humidified incubator with 5% CO2.
Cell viability assay
Cell viability was determined by the crystal violet staining method, as described previously with minor modification [23]. In brief, osteoblastic cells (3.5 × 104 cells/well) were plated onto 24-well plates in 1 ml of RPMI 1640 containing 10% fetal bovine serum (FBS) until cell density reached 70–80% confluence. Each type of cell was cultured with serum-free medium for 6 h and switched to 0.5% FBS RPMI 1640 medium containing Hcy (0, 0.5, 1.0, 2.5, and 5 mM). The concentration of 0 mM Hcy was used as control. After 24 h, viable cells were stained by the crystal violet staining method. Plates were washed four times with tap water. After drying, cells were lysed with 1% sodium dodecyl sulfate (SDS) solution, and dye uptake was measured at 550 nm using a 96-well plate reader. Cell viability was calculated from relative dye intensity compared with untreated samples.
Apoptosis assessment
Hoechst 33342 assay
The assay was performed as described previously [24]. Cells were cultured in a 24-well plate. After incubation with Hcy (0, 0.5, 1.0, 2.5, and 5 mM), the cells were treated with Hoechst 33342 (5 μg/ml) for 10 min at 37°C in the dark. The samples were then analyzed by fluorescence microscopy (excitation wavelength in the range of 450–500 nm).
TdT-mediated dUTP nick-end labeling (TUNEL) assay
The assay was performed using a Cell Death Detection ELISAplus kit (Roche Applied Science, Indianapolis, IN, USA). The assay was performed as described previously with minor modification [19]. Osteoblastic cells (1.5 × 104 cells) grown in a chamber slide and treated with 0.5% FBS media containing 5 mM Hcy for 24 h were fixed with 4% formaldehyde in phosphate-buffered saline (PBS), washed in PBS, and permeabilized by 0.2% Triton X-100. The 3′-nick ends were then labeled with fluorescein-12-dUTP by incubating in terminal deoxynucleotidyl transferase buffer. Specimens in which terminal deoxynucleotidyl transferase was omitted served as a negative control, and a DNase-treated specimen served as a positive control. Propidium iodide (1 μg/ml) was used to counterstain the nuclei. At least 600 cells from three different fields were examined in each experiment, and the cell death was expressed as a percentage of TUNEL-positive cells.
Assay for cytochrome c release
Release of cytochrome c from the mitochondria of osteoblastic cells into the cytosol was measured by immunoblotting as described previously with minor modifications [25]. Briefly, following incubation with 2.5 mM Hcy for various times, the cells were harvested by centrifugation and lysed, and the soluble cytosolic fractions were obtained by centrifugation. Aliquots of the cytosolic fractions containing equal amounts of proteins were separated by 15% SDS-polyacrylamide electrophoresis gel (SDS-PAGE) and cytochrome c release was measured by immunoblotting with specific antibody.
Small interfering RNA (siRNA)-mediated silencing
The 21-nucleotide siRNA duplexes used in this study (IRE1a siRNA(h), sc-40705; Santa Cruz Biotechnology) were transfected with siRNA oligonucleotides using Lipofectamine™ 2000 (Invitrogen, Carlsbad, CA, USA) according to the manufacturer’s recommendations. U2OS were seeded at 2 × 104 cells/well with antibiotic-free normal growth medium supplemented with FBS in 24-well plates and allowed to reach approximately 50% confluence on the day of transfection. Cells were transfected with 50–100 nM siRNA in Opti-MEM medium (Santa Cruz Biotechnology) using Lipofectamine™ reagent (Invitrogen) according to the manufacturer’s transfection protocol. Twenty-four hours after transfection, the cells were treated with or without Hcy for the indicated time point (as described in figure legends). Efficiency of siRNA was measured by Western blot analysis.
Western blot analysis
Osteoblastic cells were incubated for various times and in different concentrations of Hcy. After incubation, the cells were harvested and lysed in 50 μl lysis buffer [20 mM Tris(hydroxymethyl)aminomethane hydrochloride pH 7.5; 0.5 M sodium chloride; 1 mM EDTA; 1 mM ethylene glycol tetraacetic acid (EGTA); 0.25% Triton X-100; protease inhibitor cocktail; 2 mM phenylmethylsulphonic fluoride; 1 mM dithiothreitol] and the resulting lysate was cleared by centrifugation. Protein concentrations were then determined with the Bradford method (Bio-Rad, Hercules, CA, USA). Fifty μg of proteins were resolved on SDS-PAGE (12% for Bcl-2, Bax, and CHOP, 10% for GRP78 and ATF4, 14% for caspase-3) and transferred onto a nitrocellulose membrane. The membrane was blocked by 1 h incubation at room temperature with PBS containing 5% skimmed milk and 0.1% Tween-20, and then incubated for 2 h at room temperature with primary antibodies specific for Bcl-2, Bax, GRP78, CHOP, ATF4, and cleaved caspase-3 in the blocking buffer. The membrane was incubated subsequently with horseradish peroxidase (HRP)-conjugated anti-rabbit IgG (1:2,500 dilution) and HRP-conjugated anti-mouse IgG (1:5,000) visualized by a chemiluminescence system (ECL; Amersham, Freiburg, Germany). Fuji X-ray film (Fuji Co.) with cassette closure times was used to obtain adequate exposure and to visualize bands.
Statistics
Statistical comparisons were performed with Student’s t test or Mann–Whitney U test to compare non-parametric data for statistical significance. Percentage comparisons were performed using the chi-squared test. A p-value <0.05 was considered significant.
Results
Effect of Hcy on apoptosis of osteoblastic cells
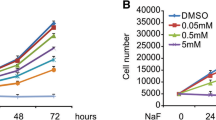
U2OS cells treated with Hcy for 24 h disclosed a concentration-dependent reduction of cell viability. To examine the effect of Hcy on apoptotic death of osteoblastic cells, we performed the Hoechst 33342 staining assay of Hcy-treated U2OS cells. Hcy induced the appearance of Hoechst staining-positive cells, which exhibited the morphological features of decreased size with highly condensed and fragmented nuclei (Fig. 1a). In contrast, very few Hoechst staining-positive cells were observed in the control cells. This result was confirmed with TUNEL assay and experiments using HNOst cells produced equivalent results (Fig. 1a). Osteoblastic cells were cultured with different concentrations of Hcy. There was a significant tendency that the rate of apoptotic cell death of osteoblastic cells increased with the higher concentration of Hcy (Fig. 1b). Apoptosis of osteoblastic cells also increased with longer exposure to Hcy (Fig. 1c). These data demonstrate that Hcy induced apoptosis in osteoblastic cells in dose- and time-dependent manner.
Effect of homocysteine (Hcy) on apoptosis of osteoblastic cells. A U2OS cells were cultured in the absence (a) or presence (b) of 2.5 mM Hcy for 24 h, and assayed by the Hoechst 33342 staining method. The arrow indicates Hoechst 33342 staining-positive cells with nuclei condensation and fragmentation. This result was confirmed with TUNEL assay (c, d). Experiments using HNOst cells under the same conditions produced equivalent results (e, f). B HNOst cells were cultured in the presence of Hcy (0, 2.5 or 5 mM) for 24 h, and apoptotic cells were quantified. The apoptosis by Hcy was statistically significant (*p < 0.05 vs 0 mM). C HNOst cells were cultured in the presence of Hcy 0.5 mM for 12, 24, 48 and 72 h, and apoptotic cells were measured at the indicated time. The apoptosis by Hcy was statistically significant (*p < 0.05 vs control). Data shown in B and C are the mean ± SD percentages
Susceptibility of osteoblastic cells to Hcy
We compared the susceptibility of osteoblastic cells to Hcy with other cells. HNOst cells, HUVECs, human dermal fibroblasts, and human FLS were cultured in the presence of Hcy for 24 h. The viability of HNOst cells and HUVECs declined depending on Hcy concentration (Fig. 2a, b), while human dermal fibroblasts and human FLS survived the toxic effect of Hcy with little change of viability (Fig. 2c, d). Viability of HNOst and HUVEC decreased from 2.5 mM Hcy. (Fig. 2a, b). These data suggest that osteoblastic cells are more susceptible to Hcy-mediated cell death than other cell types.
Susceptibility of several types of cells to Hcy. HNOst cells (a), HUVECs (b), human dermal fibroblasts (c), and human FLS (d) were cultured in various concentration of Hcy (0, 0.5, 1.0, 2.5, and 5 mM) in fixed exposure time of 24 h. Cell viability was measured by the crystal violet staining method. Data shown are the mean ± SD percentages. *p < 0.05 vs untreated control
Activation of caspase-3 in Hcy-induced apoptosis of osteoblastic cells
The caspase family of cysteine proteases is implicated in the programmed cell death of numerous cell types. Caspase-3 is a final component of the caspase cascade leading to cell death [26]. Thus, we examined active caspase-3 in Hcy-treated osteoblastic cells. Hcy increased the cleaved active form of caspase-3 (Fig. 3a). Pretreatment of U2OS cells with z-DEVD-fmk, a caspase-3 inhibitor, efficiently suppressed the Hcy-induced cell death (Fig. 3b). These data indicate that Hcy induced apoptotic cell death in osteoblastic cells, and activation of caspase-3 is involved in the process.
Activation of caspase-3 in Hcy-induced apoptosis of osteoblastic cells. a U2OS cells incubated with various concentration of Hcy (0, 0.5, 1.0, 2.5, and 5 mM) for 24 h (left panel) and 2.5 mM for indicated times (5, 10, 24, and 48 h) (right panel). Whole-cell extracts from U2OS cells were separated on 14% SDS-PAGE and immunoblotted using monoclonal antibody against anti-procaspase 3 and anti-cleaved caspase-3. b U2OS cells preincubated with the 5 μM zVAD-fmk for 1 h were treated with 2.5 mM Hcy for 24 h. Cell death was assayed by the Hoechst 33342 fluorescent staining method. Data shown are the mean ± SD percentages. *p < 0.01 vs 2.5 mM Hcy-treated control
Apoptosis via mitochondrial pathway
Cytochrome c, an apoptogenic protein, is released from activated mitochondria into the cytosol and is crucial for activating the caspase cascades of cell degradation [27]. To determine whether Hcy-induced apoptosis occurred via the mitochondrial pathway, we examined cytochrome c release in U2OS cells. Release of cytochrome c was observed, which was dependent on Hcy concentration (Fig. 4a). Cytochrome c release was observed as early as 5 h after treatment with Hcy and peaked at 24 h and then decreased (Fig. 4a). Cytochrome c release from mitochondria into cytosol is controlled by Bcl-2 family members [28]. Bax, the pro-apoptotic members, can form pores or interact with pore-forming proteins at the level of the mitochondrial membrane, a function that is antagonized by Bcl-2 [28, 29]. We investigated the expression of Bax and Bcl-2 protein by Western blot analysis in Hcy-treated U2OS cells. The expressions of Bcl-2 were down-regulated and the levels of Bax were up-regulated to the Hcy concentration of 2.5 mM and the ratio of Bax and Bcl-2 expression indicates a shift toward pro-apoptosis (Fig. 4b). These results suggest Hcy induces apoptotic cell death in osteoblastic cells via mitochondrial pathway.
Hcy-induced apoptosis via mitochondrial pathway. a U2OS cells were incubated with various concentration of Hcy (0, 0.5, 1.0, 2.5, and 5 mM) for 24 h (left panel) and 2.5 mM for indicated times (5, 10, 24, and 48 h) (right panel) and their cytosolic fractions were isolated. Cytochrome c content of each was measured by immunoblotting. Band intensity determined by densitometry and presented as the ratio after Hcy treatment relative to that at baseline. b U2OS cells were incubated with various concentration of Hcy (0, 0.5, 1.0, 2.5, and 5 mM) for 24 h and Bcl-2 and Bax expression were measured by Western blot analysis. The data represent the mean of three independent experiments with an SD bar
Involvement of ER stress of Hcy-induced apoptosis
Hcy activated ER stress in hepatocyte, neuron, and vascular endothelial cells and excessive ER stress could induce apoptosis [16, 19, 30]. To investigate the involvement of ER stress in Hcy-induced cell death in osteoblastic cells, we examined the expression of ER stress-associated molecules. Hcy induced the expression of GRP78, IRE-1α, sXBP-1, ATF4 and CHOP monitored by Western blot analysis (Fig. 5a).
Involvement of ER stress of Hcy-induced apoptosis. a U2OS cells incubated with various concentration of Hcy (0, 0.5, 1.0, 2.5, and 5 mM) for 24 h (left panel) and 2.5 mM for indicated times (5, 10, 24, and 48 h) (right panel). Whole-cell extracts from U2OS cells were separated on SDS-PAGE for Western blot analysis using antibodies specific to GRP78, IRE-1α, sXBP-1, ATF4, and CHOP. b U2OS cells were transfected with control siRNA or a specific IRE-1α siRNA. Twenty-four hours later, the cells were treated with 2.5 mM Hcy for 24 h. Whole-cell lysates were then subjected to Western blot analysis. c Apoptotic cell death was determined by TUNEL assay. Data shown are the mean ± SD percentages. *p < 0.05 vs 2.5 mM Hcy-treated control
The IRE-1α branch of the UPR has an essential role in defending cells and tissues against the lethal consequences of ER stress [31, 32]. Thus, when the IRE-1α branch is silenced in these organisms, they become more sensitive to agents that perturb protein folding in the ER [32]. To examine the functional significance of Hcy-induced IRE-1α upregulation, we employed the siRNA duplex against IRE-1α mRNA. U2OS cells were transfected with the indicated siRNA and treated with or without Hcy. Immunoblot analysis demonstrated that transfection of siRNA against IRE-1α resulted in a suppression of Hcy-induced IRE-1α expression in U2OS cells as compared to cells transfected with control siRNA (Fig. 5b). We then examined the effect of inhibiting IRE-1α on Hcy-induced apoptosis of osteoblastic cells by TUNEL assay. Silencing IRE-1α expression by siRNA effectively suppressed Hcy-induced cell death of osteoblastic cells (Fig. 5c). These results together suggest that Hcy activated the ER stress, which leads to apoptotic cell death in osteoblastic cells and Hcy-induced cell death is mediated by a signal transduction pathway involving ER-resident kinase IRE-1α.
Discussion
The careful balance between bone deposition and resorption is crucial for the proper maintenance of bone mass [4]. Bone loss occurs when osteoblastic bone formation uncouples from osteoclastic bone resorption. This imbalance results in part from accelerated apoptosis and dysfunction of osteoblasts which are influenced by various signals, and inverse relationship between osteoblast apoptosis and bone formation was confirmed in an animal study [33]. This phenomenon is also observed clinically in the main causes of osteoporosis—aging, postmenopause and glucocorticoid treatment. In rheumatoid arthritis (RA), bone loss is caused in part by impairing bone formation via induction of osteoblast apoptosis, which is mediated by pathogenic key cytokines, interleukin-1 and tumor necrosis factor alpha (TNF-α) [34].
Hyperhomocysteinemia is known to be associated with osteoporosis and is a predictive factor for osteoporotic fracture [9, 10]. To date, the mechanism of Hcy in bone metabolism remains not fully understood. Our data showed Hcy induced apoptotic cell death in osteoblastic cells and was signaled through cytochrome c and caspase-3. This effect was dependent on Hcy concentration and exposure time and was inhibited by caspase-3-specific inhibitor. This result is consistent with previous reports using endothelial cells and bone marrow stromal cells [19, 25]. Subsequently, we demonstrated that osteoblastic cells and endothelial cells were more susceptible to Hcy-mediated cell death than other cell types in vitro, which is compatible with the clinical observation that homocysteinuria, a genetically inherited disease caused by a deficiency of cystathionine β-synthase (CBS), manifests characteristic clinical features of osteoporosis and premature atherosclerosis [7].
Not only could Hcy enhance endothelial apoptosis via upregulation of Fas-mediated pathway or stimulating mitochondrial pathway by oxidative stress [25, 35] but Hcy also induces apoptotic cell death in endothelial cells through activation of the ER stress response [19]. In effect, Hcy induced ER stress in hepatocytes, as well as neuronal cells, leading to apoptosis [16, 18] and a mouse model of CBS deficiency exhibited strong biological phenotypes, ER stress in the liver and kidney as well as osteoporosis [13]. We showed that along with apoptosis induction, increased expression of ER stress-associated molecules like IRE-1α, sXBP-1, GRP78 and ATF4 was observed in Hcy-treated osteoblastic cells in a dose- and time-dependent manner, which suggests activation of UPR in Hcy-treated osteoblastic cells. Severe and prolonged ER dysfunction in osteoblasts stirred by Hcy could initiate apoptosis [36]. Three known proapoptotic pathways emanating from the ER are mediated by IRE-1α, caspase-12, and protein kinase RNA-like ER-associated kinase (PERK)/CHOP, respectively.
Under ER stress, activated IRE-1α can bind c-Jun-N-terminal kinase (JNK) and recruit cytosolic adapter TNF receptor-associated factor 2 protein (TRAF2) to the ER membrane. TRAF2 activates the apoptosis-signaling kinase 1 (ASK1), a mitogen activated protein kinase kinase kinase. Activated ASK1 leads to activation of the JNK protein kinase and mitochondria/Apaf1-dependent caspase activation [37]. In addition, caspase-12 may be activated by IRE-1α, which may recruit caspase-12 through TRAF2 [38]. We showed that Hcy-enhanced expression of IRE-1α and inhibition of IRE-1α expression by siRNA resulted in an effective suppression of apoptotic cell death by Hcy. This result demonstrated that Hcy-induced apoptosis of osteoblastic cells is mediated by a signal transduction pathway through ER-resident kinase IRE-1α. Although activity of JNK was not examined in our study, it has been reported that Hcy-induced IRE-1α activation causes a rapid and sustained activation of JNK protein kinases in endothelial cells [39] and that activation of JNK protein kinases were not induced by knockdown of IRE-1α [40]. Considering persistent JNK activation is associated with apoptotic cell death [41], it is speculated that the protective effect of IRE-1α silencing from Hcy-induced apoptotic cell death of osteoblastic cells is attributable partly to interruption of IRE-1α-mediated JNK activation.
Another main signaling pathway is that activation of PERK leads to the phosphorylation of eukaryotic initiation factor 2 alpha, which suppresses translation initiation of most cellular proteins but promotes translation initiation of ATF4, leading to transcription of the ATF4 downstream target CHOP [42]. Expression of CHOP is highly sensitive to ER stress condition [43]. CHOP was expressed significantly after 24-h exposure time in Hcy-treated osteoteoblastic cells. CHOP, also known as growth-arrest- and DNA-damage-inducible gene 153, contributes to apoptosis induction by down-regulating anti-apoptotic factor, Bcl-2. We also confirmed decreased expression of Bcl-2 together with upregulation of Bax, a pro-apoptotic factor (Fig. 4b). In the study of CHOP knockout mice, the epithelial cells of kidney resisted apoptotic cell death in spite of functional impairment under ER stress [43], confirming that induction of CHOP is an important element of the switch from pro-survival to pro-death signaling.
It has been reported that ER stress-associated molecules might have a significant role in function and differentiation of osteoblasts. ATF4, one of the major ER stress markers has been reported to regulate the onset of osteoblast differentiation, type I collagen synthesis, osteoblast-specific gene expression, and osteoblast terminal differentiation, and ATF4 knockout mice have reduced bone mass throughout life [44]. PERK knockout mice exhibited skeletal defects including deficient mineralization, osteoporosis, and abnormal compact bone development, which are associated with defects in the rough endoplasmic reticulum [45]. In contrast, osteoporosis and deficient bone mineralization occur during osteogenesis imperfecta, which is a disease where misfolded mutant procollagen binds to GRP78 and activates the UPR [46]. Therefore, a proper balance of UPR activation may be required for optimal osteoblast function and modulation of ER stress would be beneficial to prevent bone loss in some conditions.
High plasma levels of Hcy are commonly observed in patients with RA [47] and Hcy was also present in synovial fluid, with a mean concentration significantly higher in RA patients [48]. Hcy upregulates expression of GRP78 in endothelial cells [49]. GRP78, an ER molecular chaperone, was overexpressed in cells in the hypervascular synovium of patients with RA, which indicates that rheumatoid synovium is under condition of ER stress [50]. The probability is that increased Hcy in the synovial fluid induces ER stress or exacerbates the process in the synovial tissue and surrounding bone tissue. The ER-associated degradation system is an important processing system for ER homeostasis by eliminating unfolded proteins through the ubiquitin–proteasome system [51]. Synoviolin, an E3 ubiquitin ligase, was highly expressed in the rheumatoid synovial cells and that makes synovial cells resist the excessive ER stress by eliminating unfolded proteins and acquire the aggressive activity [52]. On the other hand, osteoblasts are susceptible to ER stress leading to apoptosis, which could eventually contribute to the development of periarticular osteoporosis.
Our data demonstrated the ability of Hcy to induce apoptosis in osteoblastic cells and the functional involvement of ER stress in that process. It is especially notable that osteoblasts are more susceptible to Hcy-induced apoptotic cell death, unlike other cell types. This result suggests that Hcy induces ER stress in osteoblastic cells, which are vulnerable to ER stress, leading to apoptotic cell death. These findings help understanding the mechanisms that Hcy reduces bone formation and subsequently increases the risk of fracture and establishing the therapeutic strategy of attenuating Hcy-induced ER stress.
Abbreviations
- IRE-1α:
-
Inositol-requiring transmembrane kinase and endonuclease 1α
- sXBP-1:
-
Spliced X-box binding protein
- ATF4:
-
Activating transcription factor 4
- Bax:
-
Bcl-2-associated X protein
- Bcl-2:
-
B-cell lymphoma 2
- CHOP:
-
C/EBP homologous protein
- ER:
-
Endoplasmic reticulum
- FLS:
-
Fibroblast-like synoviocytes
- GRP78:
-
Glucose-regulated protein 78
- Hcy:
-
Homocysteine
- HUVECs:
-
Human umbilical vein endothelial cells
- PERK:
-
PKR-like ER-associated kinase
- UPR:
-
Unfolded protein response
References
Kanis JA, McCloskey EV, Johansson H, Oden A (2009) Approaches to the targeting of treatment for osteoporosis. Nat Rev Rheumatol 5:425–431
Seeman E (2002) Pathogenesis of bone fragility in women and men. Lancet 359:1841–1850
Manolagas SC (1998) Cellular and molecular mechanisms of osteoporosis. Aging (Milano) 10:182–190
Weinstein RS, Manolagas SC (2000) Apoptosis and osteoporosis. Am J Med 108:153–164
Harvey N, Dennison E, Cooper C (2010) Osteoporosis: impact on health and economics. Nat Rev Rheumatol 6:99–105
Levasseur R (2009) Bone tissue and hyperhomocysteinemia. Jt Bone Spine 76:234–240
Yap S, Naughten E (1998) Homocystinuria due to cystathionine beta-synthase deficiency in Ireland: 25 years’ experience of a newborn screened and treated population with reference to clinical outcome and biochemical control. J Inherit Metab Dis 21:738–747
Testai FD, Gorelick PB (2010) Inherited metabolic disorders and stroke part 2: homocystinuria, organic acidurias, and urea cycle disorders. Arch Neurol 67:148–153
van Meurs JB, Dhonukshe-Rutten RA, Pluijm SM et al (2004) Homocysteine levels and the risk of osteoporotic fracture. N Engl J Med 350:2033–2041
McLean RR, Jacques PF, Selhub J, Tucker KL, Samelson EJ, Broe KE, Hannan MT, Cupples LA, Kiel DP (2004) Homocysteine as a predictive factor for hip fracture in older persons. N Engl J Med 350:2042–2049
Gjesdal CG, Vollset SE, Ueland PM, Refsum H, Meyer HE, Tell GS (2007) Plasma homocysteine, folate, and vitamin B 12 and the risk of hip fracture: the hordaland homocysteine study. J Bone Miner Res 22:747–756
Herrmann M, Wildemann B, Claes L, Klohs S, Ohnmacht M, Taban-Shomal O, Hubner U, Pexa A, Umanskaya N, Herrmann W (2007) Experimental hyperhomocysteinemia reduces bone quality in rats. Clin Chem 53:1455–1461
Gupta S, Kuhnisch J, Mustafa A, Lhotak S, Schlachterman A, Slifker MJ, Klein-Szanto A, High KA, Austin RC, Kruger WD (2009) Mouse models of cystathionine beta-synthase deficiency reveal significant threshold effects of hyperhomocysteinemia. FASEB J 23:883–893
Anagnostis P, Karagiannis A, Kakafika AI, Tziomalos K, Athyros VG, Mikhailidis DP (2009) Atherosclerosis and osteoporosis: age-dependent degenerative processes or related entities? Osteoporos Int 20:197–207
Zhang K, Kaufman RJ (2008) From endoplasmic-reticulum stress to the inflammatory response. Nature 454:455–462
Ji C, Kaplowitz N (2003) Betaine decreases hyperhomocysteinemia, endoplasmic reticulum stress, and liver injury in alcohol-fed mice. Gastroenterology 124:1488–1499
Kim HJ, Cho HK, Kwon YH (2008) Synergistic induction of ER stress by homocysteine and beta-amyloid in SH-SY5Y cells. J Nutr Biochem 19:754–761
Chigurupati S, Wei Z, Belal C, Vandermey M, Kyriazis GA, Arumugam TV, Chan SL (2009) The homocysteine-inducible endoplasmic reticulum stress protein counteracts calcium store depletion and induction of CCAAT enhancer-binding protein homologous protein in a neurotoxin model of Parkinson disease. J Biol Chem 284:18323–18333
Zhang C, Cai Y, Adachi MT, Oshiro S, Aso T, Kaufman RJ, Kitajima S (2001) Homocysteine induces programmed cell death in human vascular endothelial cells through activation of the unfolded protein response. J Biol Chem 276:35867–35874
Shirakawa K, Maeda S, Gotoh T et al (2006) CCAAT/enhancer-binding protein homologous protein (CHOP) regulates osteoblast differentiation. Mol Cell Biol 26:6105–6116
Pereira RC, Stadmeyer LE, Smith DL, Rydziel S, Canalis E (2007) CCAAT/enhancer-binding protein homologous protein (CHOP) decreases bone formation and causes osteopenia. Bone 40:619–626
Yoo SA, Park BH, Park GS, Koh HS, Lee MS, Ryu SH, Miyazawa K, Park SH, Cho CS, Kim WU (2006) Calcineurin is expressed and plays a critical role in inflammatory arthritis. J Immunol 177:2681–2690
Lee SJ, Kim KM, Namkoong S et al (2005) Nitric oxide inhibition of homocysteine-induced human endothelial cell apoptosis by down-regulation of p53-dependent Noxa expression through the formation of S-nitrosohomocysteine. J Biol Chem 280:5781–5788
Yuan Q, Jiang DJ, Chen QQ, Wang S, Xin HY, Deng HW, Li YJ (2007) Role of asymmetric dimethylarginine in homocysteine-induced apoptosis of vascular smooth muscle cells. Biochem Biophys Res Commun 356:880–885
Kim DJ, Koh JM, Lee O, Kim NJ, Lee YS, Kim YS, Park JY, Lee KU, Kim GS (2006) Homocysteine enhances apoptosis in human bone marrow stromal cells. Bone 39:582–590
Orrenius S, Zhivotovsky B, Nicotera P (2003) Regulation of cell death: the calcium-apoptosis link. Nat Rev Mol Cell Biol 4:552–565
Degli Esposti M (2004) Mitochondria in apoptosis: past, present and future. Biochem Soc Trans 32:493–495
Cotter TG (2009) Apoptosis and cancer: the genesis of a research field. Nat Rev Cancer 9:501–507
Hengartner MO (2000) The biochemistry of apoptosis. Nature 407:770–776
Althausen S, Paschen W (2000) Homocysteine-induced changes in mRNA levels of genes coding for cytoplasmic- and endoplasmic reticulum-resident stress proteins in neuronal cell cultures. Brain Res Mol Brain Res 84:32–40
Shen X, Ellis RE, Lee K et al (2001) Complementary signaling pathways regulate the unfolded protein response and are required for C. elegans development. Cell 107:893–903
Cox JS, Shamu CE, Walter P (1993) Transcriptional induction of genes encoding endoplasmic reticulum resident proteins requires a transmembrane protein kinase. Cell 73:1197–1206
Bellido T, Ali AA, Plotkin LI, Fu Q, Gubrij I, Roberson PK, Weinstein RS, O’Brien CA, Manolagas SC, Jilka RL (2003) Proteasomal degradation of Runx2 shortens parathyroid hormone-induced anti-apoptotic signaling in osteoblasts. A putative explanation for why intermittent administration is needed for bone anabolism. J Biol Chem 278:50259–50272
Tsuboi M, Kawakami A, Nakashima T et al (1999) Tumor necrosis factor-alpha and interleukin-1beta increase the Fas-mediated apoptosis of human osteoblasts. J Lab Clin Med 134:222–231
Suhara T, Fukuo K, Yasuda O, Tsubakimoto M, Takemura Y, Kawamoto H, Yokoi T, Mogi M, Kaimoto T, Ogihara T (2004) Homocysteine enhances endothelial apoptosis via upregulation of Fas-mediated pathways. Hypertension 43:1208–1213
Szegezdi E, Logue SE, Gorman AM, Samali A (2006) Mediators of endoplasmic reticulum stress-induced apoptosis. EMBO Rep 7:880–885
Zhang K, Kaufman RJ (2006) The unfolded protein response: a stress signaling pathway critical for health and disease. Neurology 66:S102–S109
Morishima N, Nakanishi K, Takenouchi H, Shibata T, Yasuhiko Y (2002) An endoplasmic reticulum stress-specific caspase cascade in apoptosis. Cytochrome c-independent activation of caspase-9 by caspase-12. J Biol Chem 277:34287–34294
Cai Y, Zhang C, Nawa T, Aso T, Tanaka M, Oshiro S, Ichijo H, Kitajima S (2000) Homocysteine-responsive ATF3 gene expression in human vascular endothelial cells: activation of c-Jun NH(2)-terminal kinase and promoter response element. Blood 96:2140–2148
Zhang C, Kawauchi J, Adachi MT, Hashimoto Y, Oshiro S, Aso T, Kitajima S (2001) Activation of JNK and transcriptional repressor ATF3/LRF1 through the IRE1/TRAF2 pathway is implicated in human vascular endothelial cell death by homocysteine. Biochem Biophys Res Commun 289:718–724
Chen YR, Meyer CF, Tan TH (1996) Persistent activation of c-Jun N-terminal kinase 1 (JNK1) in gamma radiation-induced apoptosis. J Biol Chem 271:631–634
Ron D, Walter P (2007) Signal integration in the endoplasmic reticulum unfolded protein response. Nat Rev Mol Cell Biol 8:519–529
Zinszner H, Kuroda M, Wang X, Batchvarova N, Lightfoot RT, Remotti H, Stevens JL, Ron D (1998) CHOP is implicated in programmed cell death in response to impaired function of the endoplasmic reticulum. Genes Dev 12:982–995
Yang X, Matsuda K, Bialek P et al (2004) ATF4 is a substrate of RSK2 and an essential regulator of osteoblast biology; implication for Coffin–Lowry syndrome. Cell 117:387–398
Zhang P, McGrath B, Li S, Frank A, Zambito F, Reinert J, Gannon M, Ma K, McNaughton K, Cavener DR (2002) The PERK eukaryotic initiation factor 2 alpha kinase is required for the development of the skeletal system, postnatal growth, and the function and viability of the pancreas. Mol Cell Biol 22:3864–3874
Lisse TS, Thiele F, Fuchs H et al (2008) ER stress-mediated apoptosis in a new mouse model of osteogenesis imperfecta. PLoS Genet 4:e7
Berglund S, Sodergren A, Wallberg Jonsson S, Rantapaa Dahlqvist S (2009) Atherothrombotic events in rheumatoid arthritis are predicted by homocysteine—a six-year follow-up study. Clin Exp Rheumatol 27:822–825
Lazzerini PE, Selvi E, Lorenzini S, Capecchi PL, Ghittoni R, Bisogno S, Catenaccio M, Marcolongo R, Galeazzi M, Laghi-Pasini F (2006) Homocysteine enhances cytokine production in cultured synoviocytes from rheumatoid arthritis patients. Clin Exp Rheumatol 24:387–393
Kokame K, Kato H, Miyata T (1996) Homocysteine-respondent genes in vascular endothelial cells identified by differential display analysis. GRP78/BiP and novel genes. J Biol Chem 271:29659–29665
Blass S, Union A, Raymackers J, Schumann F, Ungethum U, Muller-Steinbach S, De Keyser F, Engel JM, Burmester GR (2001) The stress protein BiP is overexpressed and is a major B and T cell target in rheumatoid arthritis. Arthritis Rheum 44:761–771
Hampton RY (2002) ER-associated degradation in protein quality control and cellular regulation. Curr Opin Cell Biol 14:476–482
Amano T, Yamasaki S, Yagishita N et al (2003) Synoviolin/Hrd1, an E3 ubiquitin ligase, as a novel pathogenic factor for arthropathy. Genes Dev 17:2436–2449
Acknowlegment
This work was supported by grants from the Korea Health 21R&D Project, Ministry of Health & Welfare, Republic of Korea (No. A040018), and the Korea Healthcare Technology R&D Project, Ministry for Health, Welfare and Family Affairs (No. A092258 and A084948), and National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (No. 314-2008-1-E00113).
Conflict of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
S.-J. Park and K.-J. Kim contributed equally to this work.
About this article
Cite this article
Park, SJ., Kim, KJ., Kim, WU. et al. Involvement of endoplasmic reticulum stress in homocysteine-induced apoptosis of osteoblastic cells. J Bone Miner Metab 30, 474–484 (2012). https://doi.org/10.1007/s00774-011-0346-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-011-0346-9