Abstract
The purpose of this study was to clarify the effects of a 1-year treatment with either alendronate or risedronate on the proximal femoral geometry among Japanese women with osteoporosis by hip structure analysis. Postmenopausal women who had taken at least 90% of their prescription for alendronate (35 mg/week, 94 patients) or risedronate (17.5 mg/week, 181 patients) for 1 year were retrospectively analyzed. In the alendronate treatment group, bone mineral density (BMD), cross-sectional area (CSA), section modulus and average cortex significantly increased by 0.81, 1.35, 2.23 and 0.97% at the narrow neck and increased by 2.19, 2.28, 2.85 and 1.11% at the intertrochanteric, respectively. Buckling ratio at the intertrochanteric significantly decreased by 2.50%. The CSA, section modulus and average cortex at the shaft significantly increased at 1 year. In the risedronate treatment group, the CSA, section modulus and average cortex at the narrow neck significantly increased by 0.80, 0.95 and 0.89%, respectively. BMD, CSA, section modulus, and average cortex at the intertrochanteric significantly increased by 1.61, 0.88, 2.05 and 0.79%, respectively, and buckling ratio significantly decreased by 1.53%. BMD, CSA, section modulus, and average cortex at the shaft significantly increased. The percent change of section modulus was significantly correlated with that of BMD, CSA and average cortex and negatively correlated with that of buckling ratio at all regions in both treatment groups. Statistically significant differences between the alendronate and risedronate groups were seen for section modulus in the narrow neck and CSA in the intertrochanteric. In conclusion, Japanese osteoporotic women treated by either alendronate or risedronate showed significant improvements of geometry in proximal femur within 1 year.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
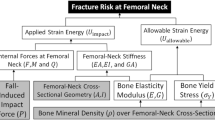
Areal bone mineral density (BMD) measured by dual energy X-ray absorptiometry (DXA) is a valuable tool for the evaluation of bone fragility, and shows significant correlation between BMD decline and risk of fracture [1–3]. However, BMD may not be the best assessment of treatment efficacy since the fracture reduction after treatment is only partially explained by increased BMD [4–6]. Strength of bone is governed by structural dimensions and tissue material properties, neither of which is directly measured by a conventional BMD measurement.
Beck and Ruff applied the hip structure analysis (HSA) method to measure proximal femur geometry and strength using conventional DXA scans of the hip [7, 8]. HSA has been used to demonstrate age trends, racial and gender differences, and treatment effects on osteoporosis in Caucasians [8–16]. In Japan, we have previously demonstrated age-related differences in structural geometry and femoral strength [17] and raloxifene had positive effects on geometry in Japanese women with osteoporosis [18]. Ito et al. [19] also reported that minodronic acid hydrate, a new bisphosphonate developed in Japan, improved bone strength indices in the proximal femoral region.
Bonnick et al. [15] reported that treatment with once-weekly alendronate or risedronate resulted in significant improvements in HSA parameters in Caucasian patients with osteoporosis; however, the doses of bisphosphonates for Japanese patients are half of those applied to Caucasians (alendronate 70 vs. 35 mg/week, risedronate 35 vs. 17.5 mg/week, in Caucasians vs. Japanese, respectively). These dosages seemed to be associated with race differences [20, 21]. The HSA for minodronic acid in Japanese women has been previously reported [19]; however, the effects of bisphosphonates are not the same. These results indicate that analysis of the geometry for the half doses of alendronate and risedronate is necessary in Japanese patients with osteoporosis.
The purpose of this study was to clarify the effects of a 1-year treatment with either alendronate (35 mg/week) or risedronate (17.5 mg/week) on the proximal femoral geometry of Japanese postmenopausal women with osteoporosis by HSA.
Materials and methods
Three hundred and sixty-seven community-dwelling, ambulatory, postmenopausal women had taken alendronate (35 mg/week, 128 patients) or risedronate (17.5 mg/week, 239 patients) from August 2007 to April 2009. Of these patients, 275 of them who had taken at least 90% of their prescribed biphosphonates for 1 year were retrospectively analyzed by HSA. The number of patients and the mean age was 94 patients and 73.2 years of age for alendronate and 181 patients and 70.6 years of age for risedronate, respectively. There was no significant difference between alendronate and risedronate in the percent of patients who dropped out and/or discontinued medication (26.6% in alendronate, 24.3% in risedronate). All of the patients in both treated groups were defined by Japanese osteoporosis diagnosis criteria [22]. These criteria included low BMD (T score <−2.5) or presence of osteoporotic fractures. Patients with a history of hip fracture or any disease or medication known to affect bone metabolism were excluded from the study. DXA scans of the hip were taken at baseline and were repeated at 6 and 12 month follow-up. Hip scans were performed using a hip positioner system (HPS; OsteoDyne, Durham, NC, USA) to ensure consistent positioning [23]. This device keeps the subject’s legs positioned in abduction and internal rotation (15°).
Hip structure analysis (HSA)
The archived DXA images were analyzed using the HSA method which is described in detail in earlier publications [7, 8]. Briefly, using an automated program, DXA scan files were first converted into bone mass images in which pixel values represent bone mass in grams per square centimeter. The underlying principle of the method is that a line of pixels traversing the bone axis is a projection of the corresponding cross-section from which certain geometric properties can be derived. Three measured sites were defined as: (1) narrow neck, traversing the narrowest width of the femoral neck, (2) intertrochanteric, along the bisector of the shaft and femoral neck axes, and (3) shaft, at a distance of 1.5 times minimum neck width, distal to the intersection of the neck and shaft axes. HSA was performed by a radiological engineer who did not know about the treatment of the patients.
The structural parameters used in this paper were as follows [24, 25].
-
Areal BMD (g/cm2): mean values of BMD from the narrow neck region are on the average about 14% higher than the conventional Hologic neck region of interest (ROI) values on the same subjects, although age trends are similar in previous reports [10].
-
Outer diameter (cm): the distance between (blur corrected) outer margins of the cross-section.
-
Cross-sectional area (CSA, cm2): this is defined as the surface area of bone tissue in the cross-section after excluding soft tissue (marrow) spaces. CSA is an index of resistance to forces directed along the long axis of the bone.
-
Section modulus (cm3): this is an index of resistance to bending forces and is calculated as CSMI/d max where CSMI is the cross-sectional moment of inertia and d max is the maximum distance from either bone edge to the centroid of the profile.
-
Average cortex (cm): this is an estimate of the mean cortical thickness assuming a circular (narrow-neck or shaft) or elliptical (intertrochanteric) annulus model of the cross-section for use in the estimated buckling ratio. The model assumes that 60, 70 and 100% of the measured bone mass is in the cortex for narrow-neck, intertrochanteric and shaft, respectively.
-
Buckling ratio: this describes stable configurations of thin-walled tubes subjected to compressive loads and is estimated as the ratio of d max to the estimated mean cortical thickness. Buckling ratio is presented only for the narrow neck and intertrochanteric regions, because this parameter is not important in the shaft.
Based on a preceding study, precision error (%CV) for HSA parameters at the neck, intertrochanteric and shaft ranges from 0.8 to 4.7%, with an average of 2.2% [17, 26].
Statistical analysis
All parameters are presented as mean (standard deviations, SD) at baseline, and percent differences from baseline (95% confidence interval, CI). Differences were regarded as statistically significant when the 95% CI did not include zero. The correlations between HSA parameters were analyzed by Pearson’s R and considered statistically significant at P < 0.05. P values from two-sample t tests were used to compare group means and considered statistically significant at P < 0.05.
Results
Percent changes from baseline in HSA parameters
Alendronate treatment group
Narrow neck: BMD significantly increased by 0.81% (95% CI 0.16, 1.45) at 1 year, and section modulus significantly increased by 0.86% (95% CI 0.16, 1.56) and 2.23% (95% CI 1.47, 2.99) compared to baseline at 6 months and 1 year, respectively. Compared to baseline, the mean difference in CSA and average cortex significantly increased at 1 year; however, changes in the outer diameter and buckling ratio did not reach significance (Table 1a).
Intertrochanteric: BMD and section modulus significantly increased by 1.20% (95% CI 0.58, 1.81) and 1.24% (95% CI 0.62, 1.85) at 6 months, by 2.19% (95% CI 1.38, 3.01) and 2.85% (95% CI 1.98, 3.72) at 1 year, respectively. The buckling ratio significantly decreased by 1.30% (95% CI −2.12, −0.49) and 2.50% (95% CI −3.40, −1.59) at 6 months and 1 year, respectively. The other parameters, CSA and average cortex significantly increased at 1 year; however, changes in the outer diameter did not show significant change (Table 1b).
Shaft: CSA, section modulus and average cortex significantly increased at 1 year; however, changes in BMD and the outer diameter did not show significant change (Table 1c).
Percent changes from baseline in HSA parameters
Risedronate treatment group
Narrow neck: the section modulus significantly increased by 0.95% (95% CI 0.19, 1.70) compared to baseline at 1 year. Compared to baseline, CSA and average cortex significantly increased at 1 year; however, changes in BMD, the outer diameter and buckling ratio did not reach significance (Table 2a).
Intertrochanteric: BMD and section modulus significantly increased by 0.90% (95% CI 0.48, 1.31) and 1.00% (95% CI 0.52, 1.49) at 6 months, by 1.61% (95% CI 1.05, 2.17) and 2.05% (95% CI 1.29, 2.80) at 1 year, respectively. The buckling ratio significantly decreased by 0.57% (95% CI −1.10, −0.04) and 1.53% (95% CI −2.25, −0.81) at 6 months and 1 year, respectively. The other parameters, CSA and average cortex significantly increased at 1 year; however, changes in the outer diameter did not show significant change (Table 2b).
Shaft: BMD, CSA, section modulus and average cortex significantly increased at 1 year; however, changes in the outer diameter did not show significant change (Table 2c).
Correlations among the percent changes of parameters
Tables 3 and 4 show correlations (Pearson’s R) among the percent changes of HSA parameters in the narrow neck, intertrochanteric and shaft regions. The percent change of the section modulus is significantly correlated with the percent change of BMD, CSA, and average cortex and negatively correlated with the percent change of the buckling ratio in all regions in both treatment groups. As expected, the percent changes of BMD had a positive relationship with the percent change of CSA, but negative relationship with the percent change of the outer diameter in all regions.
Comparisons of percent changes of the parameters between the alendronate and risedronate treatment groups
The comparisons of percent changes of the parameters between the alendronate and risedronate treatment groups are shown in Fig. 1. Statistically significant differences between alendronate and risedronate were seen for section modulus in the narrow neck and CSA in the intertrochanteric. The other parameters did not show a significant difference; however, alendronate showed a greater improvement in several parameters compared with risedronate.
Discussion
One of the problems with the use of BMD as a monitor for osteoporosis treatment is that it does not completely capture the mechanical factors that lead to fragility [4–6]. Beck and Ruff applied the HSA method to measure proximal femur geometry and strength using conventional DXA scans of the hip [7, 8]. In this study, we are the first to report that Japanese women with either alendronate or risedronate treatment over a 1-year period had significant improvements of geometry in proximal femur.
HSA has been demonstrated in the effects of alendronate and risedronate in the post hoc analysis of a large clinical trial (Fosamax Actonel Comparison Trial, FACT) in Caucasians [15]. Two years of treatment with either alendronate or risedronate resulted in statistically significant improvements from baseline in most geometric parameters at the narrow neck, intertrochanteric and shaft; however, these data are mainly based on Caucasian patients. It is not fully understood whether the geometric effects of bisphosphonate upon Japanese patients are the same on Caucasians, because the dosage used to treat osteoporosis in Japan (alendronate 35 mg/week, risedronate 17.5 mg/week) is half of that applied to Caucasians (alendronate 70 mg/week, risedronate 35 mg/week) [20, 21]. The HSA data for minodronic acid in Japanese women have been previously reported [19]; however, the effects of bisphosphonates are not the same. In addition, the changing trends of HSA parameters are not the same as those of BMD, so that the analysis of the half dosage of bisphosphonates to influence hip geometry is important.
It is worth noting that the percent change of section modulus was higher than that of BMD in all three regions (Tables 1, 2). These results might suggest that the reduction of fracture rate is not fully explained by increased BMD in the clinical outcomes. The baseline values of section modulus at all regions are greater than that of BMD, and the percent changes of section modulus are also greater than that of BMD; therefore, a small increase of absolute value in section modulus did not lead to a greater increase of percent changes.
The changing trends of HSA parameters in this study were generally consistent with the FACT study in mostly Caucasians, the minodronic acid study, and the raloxifene study in Japan (Table 5). These changes were particularly evident at the intertrochanteric region, i.e., BMD, CSA, section modulus, average cortex and buckling ratio showed significant improvements in the bisphosphonate and raloxifene treatments. CSA and section modulus at the narrow neck and average cortex at the shaft also showed a significant increase in all of the treatment groups. The tendency to change in the other parameters is approximately similar in the bisphosphonate and raloxifene treatment groups. In addition, the comparison of the percent changes of parameters between alendronate and risedronate showed that statistically significant differences were seen for section modulus in the narrow neck and CSA in the intertrochanteric. The other parameters did not show a significant difference; however, alendronate showed a greater improvement in several parameters compared with risedronate. Both alendronate and risedronate treatment over 1 year resulted in an improvement in HSA parameters with consistently greater effects seen with alendronate than risedronate. These consistent trends of efficacy in this study are approximately similar to the FACT study.
There are methodological limitations to our study. First, DXA scanners are not designed or optimized to measure structural dimensions. Precision in 3D was relatively poor in 2D. Second, use of 2D DXA scans means that the section modulus is assessed only in the scan plane; effects of treatment may be different for bending directions out of the image plane. Third, alendronate and risedronate significantly improved geometric parameters in Caucasians and Japanese; however, the magnitude of change in any of these parameters necessary to reduce hip fracture risk is unknown. Finally, the model assumes that 60, 70 and 100% of the measured bone mass is in the cortex for the narrow neck, intertrochanteric and shaft, respectively. These methods have the possibility of overestimating the cortical thickness in cases with increased trabecular bone, especially in the narrow neck and intertrochanteric regions.
Although there were some limitations, this study also has significant strengths. This is the first study employing the HSA method to examine whether geometric strength-related parameters in elderly Japanese women on either alendronate (35 mg/week) or risedronate (17.5 mg/week) alter femoral geometry in a positive direction within a 1 year period. Although these women maintained their hip BMD, there were statistically significant changes in the underlying geometry that has not previously been reported in Japanese women with osteoporosis. If geometric parameters better explain osteoporotic fragility than BMD, then alendronate and risedronate clearly change geometry toward improved strength at the femoral neck and intertrochanteric regions of Japanese women.
We conclude that Japanese women treated with either alendronate or risedronate for 1 year showed positive structural changes in proximal regions of the femur that suggest improved bending and axial strength.
References
Kanis JA (2002) Diagnosis of osteoporosis and assessment of fracture risk. Lancet 359:1929–1936
Miller PD (2003) Bone mass measurements. Clin Geriatr Med 19:281–297
Schott AM, Cormier C, Hans D, Favier F, Hausherr E, Dargent-Molina P, Delmas PD, Ribot C, Sebert JL, Breart G, Meunier PJ, for EPIDOS Group (1998) How hip and whole-body bone mineral density predict hip fracture in elderly women: the EPIDOS Prospective Study. Osteoporos Int 8:247–254
Li Z, Meredith MP, Hoseyni MS (2001) A method to assess the proportion of treatment effect explained by a surrogate endpoint. Stat Med 20:3175–3188
Cummings SR, Karpf DB, Harris F, Genant HK, Ensrud K, LaCroix AZ, Dennis M, Black DM (2002) Improvement in spine bone density and reduction in risk of vertebral fractures during treatment with antiresorptive drugs. Am J Med 112:281–289
Sarkar S, Mitlak BH, Wong M, Stock JL, Black DM, Harper KD (2002) Relationships between bone mineral density and incident vertebral fracture risk with raloxifene therapy. J Bone Miner Res 17:1–10
Beck TJ, Ruff CB, Warden KE, Scott WW Jr, Rao GU (1990) Predicting femoral neck strength from bone mineral data: a structural approach. Invest Rad 25:6–18
Beck TJ, Ruff CB, Scott WW Jr, Plato CC, Tobin JD, Quan CA (1992) Sex differences in geometry of the femoral neck with aging: a structural analysis of bone mineral data. Calcif Tissue Int 50:24–29
Beck TJ, Ruff CB, Bissessur K (1993) Age-related changes in female femoral neck geometry: implications for bone strength. Calcif Tissue Int 53(Suppl 1):S41–S46
Beck TJ, Looker AC, Ruff CB (2000) Structural trends in the aging femoral neck and proximal shaft: analysis of the Third National Health and Nutrition Examination Survey dual-energy X-ray absorptiometry data. J Bone Miner Res 15:2297–2304
Wang XF, Duan Y, Beck TJ, Seeman E (2005) Varying contributions of growth and ageing to racial and sex differences in femoral neck structure and strength in old age. Bone 36:978–986
Uusi-Rasi K, Beck TJ, Semanick LM, Daphtary MM, Crans GG, Desaiah D, Harper KD (2006) Structural effects of raloxifene on the proximal femur: results from the multiple outcomes of raloxifene evaluation trial. Osteoporos Int 17:575–586
Greenspan SL, Beck TJ, Resnick NM, Bhattacharya R, Parker RA (2005) Effect of hormone replacement, alendronate, or combination therapy on hip structure geometry: a 3-year, double blind, placebo-controlled clinical trial. J Bone Miner Res 20:1525–1532
Uusi-Rasi K, Semanick LM, Zanchetta JR, Bogado CE, Eriksen EF, Sato M, Beck TJ (2005) Effects of teriparatide [rh PTH (1–34)] treatment on structural geometry of the proximal femur in elderly osteoporotic women. Bone 36:948–958
Bonnick SL, Beck TJ, Cosman F, Hochberg MC, Wang H, de Papp AE (2009) DXA-based hip structural analysis of once-weekly bisphosphonate-treated postmenopausal women with low bone mass. Osteoporos Int 20:911–921
Beck TJ, Lewiecki EM, Miller PD, Felsenberg D, Liu Y, Ding B, Libanati C (2008) Effects of denosumab on the geometry of the proximal femur in postmenopausal women in comparison with alendronate. J Clin Densitom 11:351–359
Takada J, Beck TJ, Iba K, Yamashita T (2007) Structural trends in the aging proximal femur in Japanese postmenopausal women. Bone 41:97–102
Takada J, Miki T, Imanishi Y, Nakatsuka K, Wada H, Naka H, Yoshizaki T, Iba K, Beck TJ, Yamashita T (2010) Effects of raloxifene treatment on structural geometry of the proximal femur in Japanese women with osteoporosis. J Bone Miner Metab 28:561–567
Ito M, Sone T, Fukunaga M (2010) Effect of minodronic acid hydrate on hip geometry in Japanese women with postmenopausal osteoporosis. J Bone Miner Metab 28:334–341
Uchida S, Taniguchi T, Shimizu T, Kakikawa T, Okuyama K, Okaniwa M, Arizono H, Nagata K, Santora AC, Shiraki M, Fukunaga M, Tomomitsu T, Ohashi Y, Nakamura T (2005) Therapeutic effects of alendronate 35 mg once weekly and 5 mg once daily in Japanese patients with osteoporosis: a double-blind, randomized study. J Bone Miner Metab 23:382–388
Kishimoto H, Fukunaga M, Kushida K, Shiraki M, Itabashi A, Nawata H, Nakamura T, Ohta H, Takaoka K, Ohashi Y, for the Risedronate Phase III Research Group (2006) Efficacy and tolerability of once-weekly administration of 17.5 mg risedronate in Japanese patients with involutional osteoporosis: a comparison with 2.5-mg once-daily dosage regimen. J Bone Miner Metab 24:405–413
Osteoporosis diagnostic criteria review committee: Japanese society for bone, mineral research (2001) Diagnostic criteria for primary osteoporosis: year 2000 revision. J Bone Miner Metab 19:331–337
Hans D, Duboeuf F, Schott AM, Horn S, Avioli LV, Drezner MK, Meunier PJ (1997) Effects of a new positioner on the precision of hip bone mineral density measurements. J Bone Miner Res 12:1289–1294
Ruff CB, Hayes WC (1983) Cross-sectional geometry of Pecos Pueblo femora and tibiae––a biomechanical investigation. I. Method and general patterns of variation. Am J Phys Anthropol 60:359–381
Melton LJ III, Beck TJ, Amin S, Khosla S, Achenbach SJ, Oberg AL, Riggs BL (2005) Contributions of bone density and structure to fracture risk assessment in men and women. Osteoporos Int 16:460–467
Nelson DA, Barondess DA, Hendrix SL, Beck TJ (2000) Cross-sectional geometry, bone strength, and bone mass in the proximal femur in black and white postmenopausal women. J Bone Miner Res 15:1992–1997
Acknowledgments
The authors wish to acknowledge Dr. Thomas J. Beck for his assistance.
Author information
Authors and Affiliations
Corresponding author
About this article
Cite this article
Takada, J., Katahira, G., Iba, K. et al. Hip structure analysis of bisphosphonate-treated Japanese postmenopausal women with osteoporosis. J Bone Miner Metab 29, 458–465 (2011). https://doi.org/10.1007/s00774-010-0242-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00774-010-0242-8