Abstract
A mother’s response towards her infant’s distress is important for the mother–infant relationship and infant development. There is evidence that maternal responses are impaired in depressed mothers. Further understanding of how depression disrupts maternal responses is important to direct treatment strategies. There is evidence that maternal responses develop during pregnancy. Further understanding of the relationship between depression and maternal responses during pregnancy is therefore important. We have previously found that depression during pregnancy is associated with reduced attentional engagement with infant distress but is unclear whether this is an insensitive or avoidance response. In the current study, we investigated the impact of anhedonic symptoms of depression on pregnant women’s autonomic response towards infant distress. We found that women experiencing anhedonic depressive symptoms during pregnancy had significantly larger systolic blood pressure responses towards infant distress (β, 1.6 mmHg, 95 % CI 0.5 to 2.6, p = 0.004) than non-depressed pregnant women. These results suggest that anhedonic symptoms during pregnancy may be associated with increased sympathetic sensitivity. This suggests that depression is not, at a sympathetic level at least, associated with insensitivity to infant distress and rather depression may be associated with an abnormally sensitive response.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Infants of depressed mothers are more likely to show attachment, behavioural, emotional and cognitive disturbances as they grow up (Kim-Cohen et al. 2005; Mantymaa et al. 2003; Murray et al. 1996b; O’Brien et al. 2004). There is evidence to suggest that this may be a result of depressed mothers’ impaired sensitivity towards their infants (Field et al. 2006; Murray et al. 1996a, b). For example, during observed interactions with their infants, depressed mothers are less engaged, show less eye contact and show more negating behaviour to signals of distress from their infant (Murray et al. 1996a, b; Field 2010). Response to infant distress may be particularly disrupted. For example, depression is associated with reduced ability to distinguish between different types of infant distress (Donovan et al. 1998). In addition, some studies have found that depression disrupts responses to distressed but not responses to non-distressed infant signals (Shaw et al. 2006) and that maternal sensitivity to infant distress but not non-distress is positively associated with infant development (McElwain and Booth-Laforce 2006; Leerkes et al. 2009). As depression is experienced by 10–15 % of women during the perinatal period (Bennett et al. 2004), understanding how maternal depression disrupts maternal response to infant distress is an important focus for research.
In animals, it is well established that maternal responses develop during pregnancy and that disruption to this development leads to impaired maternal responses after birth (Numan 2007). Women studies have shown that mother’s mental representation of the infant as wells as mother–foetal attachment during pregnancy predicts postnatal maternal responses (Shin et al. 2006; Siddiqui and Hagglof 2000; Thun-Hohenstein et al. 2008). Therefore, in the current study, we investigated the impact of factors during pregnancy on responses to infant distress.
Symptoms of depression are even more common during pregnancy than following birth (Evans et al. 2001; Gavin et al. 2005). Antenatal depression has been associated with impairments in the infant’s emotional and cognitive development (Deave et al. 2008; Evans et al., submitted for publication) and antisocial/violent behaviour during adolescence (Hay et al. 2010; Field 2011) independent of the effects of postnatal depression (Evans et al., submitted for publication; Hay et al. 2010). One prominent theory to explain the negative effects of depression on infant development concerns foetal programming of the HPA axis. High maternal cortisol levels, associated with depression, are passed to the foetus via the placenta and may have a direct impact on the neuro-development of the foetus (Bergman et al. 2007; Talge et al. 2007). However, here we suggest another potential mechanism.
We propose that depression during pregnancy could lead to poorer infant outcomes by disrupting the initial development of women’s basic instinct to respond towards infant distress. Disrupting this initial development would impair long-term maternal responses irrespective of whether the depression continues after birth. Depression, specifically anhedonic symptoms, may disrupt responses towards infant distress through the dysfunctional reward system that is found in depression. This is because, a mother’s response towards infant distress involves activation of the amygdala and dopaminergic meso-limbic system also involved in reward processing and approach motivation (Swain et al. 2007). Such activation may drive a mother’s motivation to engage with her infant and respond to their signals even in the face of extreme fatigue. Without activation of the reward systems, a distressed infant may not be approached and engaged with by a mother.
A wealth of behavioural and neurological evidence suggests that the anhedonic symptoms of depression are associated with disrupted reward processing (Keedwell et al. 2005; Martin-Soelch 2009; Pizzagalli et al. 2009; Schaefer et al. 2006). This disrupted reward processing may, therefore, disrupt responses towards infant distress in depressed pregnant women. In line with this hypothesis, we have already reported that anhedonic symptoms of depression during pregnancy are associated with reduced attentional engagement with infant distress as compared to non-distressed infant pictures (Pearson et al. 2010).
Reduced engagement with infant distress may be explained by abnormal reward processing in depression (Naranjo et al. 2001). However, depression is not only associated with abnormal reward responses, but also increased negative affect responses, cognitive biases towards negative information and over activation in neural structures involved in negative affect (Drevets 2000; Knutson et al. 2008; Martin-Soelch 2009). This may suggest that women who are depressed not only fail to show reward/salience responses towards infant distress stimuli but may overrepresent the negative aspects of the stimulus. For example, a recent study suggests that depressed mothers rate negative infant faces as more negative than non-depressed mothers (Stein et al. 2010).
As such, there are two possible explanations for our findings of a reduced attentional engagement towards infant distress compared to non-distressed infant faces in the presence of anhedonic symptoms of depression. Firstly, that depressed pregnant women are insensitive to the emotional content of the distressed infant faces and so are equally able to disengage attention from the distressed as from the neutral faces. This may be due to lack of reward response to infant distress resulting in no preferential processing. Secondly, it may be because the early attentional systems of these women disengage from the distressed infant face to avoid the emotional content of the face. This may be explained not only by the lack of reward response but also by oversensitivity to the negative content of the face. The latter would be consistent with cognitive theories of depression as well as observational evidence that depressed mothers behaviourally avoid their infant’s distress signals (Field et al. 2006; Murray et al. 1996a, b).
In the current study, in order to further understand how anhedonic symptoms of depression influence women’s responses towards infant distress, we investigated the impact of anhedonic symptoms of depression on women’s autonomic response towards infant distress during early and late pregnancy. Autonomic responses to stimuli, particularly sympathetic responses, prepare us for behavioural action. A mother needs to rapidly prepare to act in order to wake, go to, soothe or feed her distressed infant because distress signals the infant is in need. As such, a mother’s sympathetic response to infant distress will be a fundamental early component of sensitive maternal response towards infant distress. Indeed, there is evidence that mothers show greater sympathetic responses towards their own compared to unfamiliar infant cries (Wiesenfeld et al. 1981). Parasympathetic responses, reflected by pulse rate decelerations, are also relevant to maternal responses because they reflect attentional vigilance towards stimuli (Bradley et al. 2001). This is important to engage a mother to her infant when they are in need. Indeed, suggesting that changes in autonomic responses are important preparations for motherhood, there is evidence that autonomic responsivity increases across pregnancy (Dipietro et al. 2005).
There is also some evidence that abnormal physiological responses to distress are associated with impaired maternal behaviour (Frodi and Lamb 1980). Abnormally low sympathetic responses could lead to no action and insensitive behaviour towards infant distress, whilst abnormally high responses could lead to panic and behavioural avoidance. We thus reasoned that abnormally low autonomic responses would be consistent with insensitive responses towards infant distress whilst abnormally high responses would be more consistent with oversensitivity. In the current study, we therefore tested the hypothesis that anhedonic symptoms of depression during pregnancy would be associated with abnormal autonomic responses towards infant distress. We investigated women at both early and late pregnancy to account for the changes in autonomic systems (Dipietro et al. 2005), neural systems involved in maternal behaviour (Keyser-Marcus et al. 2001) and responses to emotional pictures (Pearson et al. 2009) that occur across pregnancy.
Method
Design
In a longitudinal study, we measured women’s autonomic responses towards infant distress during early and again during late pregnancy. This allowed us to investigate women’s responses across the pregnancy period. Women who agreed to participate in the study were visited at home during daytime or early evening, and all procedures described below were conducted whilst the participant was seated at a laptop computer. Participants were paid £7.50 for each test session. As well as the autonomic task described below, women completed a questionnaire regarding demographic and pregnancy information as well as the clinical interview schedule (CIS-R) which assessed symptoms of depression and anxiety disorders according to ICD-10 criteria (Lewis et al. 1992). Further emotion processing tasks were completed and are reported elsewhere (Pearson et al. 2009, 2010). The study was approved by The South East Research NHS Research Ethics Committee and North Bristol NHS Trust. All participants gave informed signed consent.
Sample
Healthy women were recruited through community midwives during routine booking appointments during early pregnancy. Women with a history of severe mental illness (taken as ever having seen a psychiatrist which in the UK provides an indication of a significant impairment to functioning), substance abuse or epilepsy were excluded from the study. Midwives invited as many eligible women as possible until the target was reached. One hundred one women were recruited and tested during early pregnancy between June 2007 and February 2008. Out of the 101 women who took part in the early pregnancy session, 76 of the same women also took part in the late pregnancy session. Of the 25 women who were not assessed at follow-up, 17 women were no longer eligible due to miscarriage or premature birth and a further eight were lost to attrition. Late pregnancy test sessions were completed by August 2008.
Only a subsample of the women who were originally recruited completed the autonomic response task. This task took 15 min, and due to the sensitivity of the recordings to outside distractions, the task was only attempted if there were no likely distractions in the home setting for the full duration (such as children or pets). In addition, the Portapres could not read pulse rates in 13 women during early and eight women during late pregnancy. Therefore, 72 women in early and 51 of these women also took part in the autonomic response task again during late pregnancy. Demographics for these women are given in Table 1.
Measures
Autonomic response task
This task was created using E-prime software. Four examples of each of the visual and audio stimuli parings described below were presented for 6 s with an interstimulus interval of 12–25 s. These presentation and interstimulus interval times were in line with previous task procedures using similar stimuli (Sarlo et al. 2005; Turpin et al. 1999). Types of stimuli were presented in blocks. However, stimuli presentation within blocks, interstimulus interval times and block order were randomised. An 8-min baseline was recorded at the beginning of the task to ensure the participant was relaxed and became used to the setup.
Primary stimulus: infant distress
This stimulus consisted of a crying infant audio clip played alongside presentation of pictures of infant distress faces.
Control stimulus type: non-salient
As an infant crying is a noise, and noises irrespective of meaning can evoke some changes in sympathetic arousal (Bradley et al. 2001; Turpin et al. 1999), it was important to also investigate whether changes in autonomic responses across pregnancy were seen in the response to a non-salient noise and visual stimulus. A second stimulus comprising infant irrelevant auditory and visual stimuli was also included. The control stimuli consisted of a flashing computer screen alongside a white noise. This stimulus was considered non-salient because although it alerts attention and is unpleasant it has no relevance towards motherhood.
Comparison of stimuli
During the task, all of the women rated the intensity of their reaction to each of these two types of stimulus on a scale from 1 to 9 after viewing them. Mean ratings for infant distress stimuli were 6.1 (SD 2.0) and for control stimuli 6.1 (SD 2.1). This confirms that the stimuli were experienced at an equivalent intensity and differed only as a function of infant salience.
Materials
Infant distress stimuli consisted of four photographs containing distressed baby faces. Full details can be found in Pearson et al. (2010). Briefly, the photographs were black and white and displayed an infant actively crying. Infant distress auditory stimuli consisted of two infant cries (from infants under 5 months) which were taken from sound effect internet sites and used in the current presentations. Control visual stimuli consisted of flashing computer screens which were created by rapidly presenting different colour slides using E-prime software. Control auditory stimuli consisted of two white noises which were also taken from sound effect internet sites and used in the current presentations.
Properties of noise stimuli
Loud, unexpected noises can evoke rapid and short-lived increases in sympathetic arousal, known as startle response (Bradley et al. 2001). These responses are non-specific and indiscriminate to the emotional nature of the stimulus. In the current study, we were interested in the response to the salience of the noise, and therefore, we took care to minimise startle responses. We did this by (1) adding a short buzz noise at the beginning of the task to remove startle to the novelty of the first stimuli; (2) warning participants that a stimulus will appear using a cue (a presentation of a fixation cross in the middle of the screen for 500 ms before each stimulus onset); and (3) modifying audio clips using Sony Sound Forge software to have a 500-ms rise time. This was because startle responses are found to be reduced if noises have a gradual presentation to full amplitude (rise time) of 200 ms or over (Turpin et al. 1999). The crying and white noises were matched on amplitude using Sony Sound Forge software. The sounds were measured, as played by the laptop through headphones, with a precision sound metre and an artificial ear. A range of ±3 dB is inaudible to the human ear. Results for peak amplitude of the noise ranged from 87.6 to 92.4 dB across repeated measurements and across both ear pieces of the headphones.
Autonomic response recordings
During the presentation of stimuli, pulse rate and blood pressure were measured using Portapres. This is a non-invasive instrument where a cuff is placed around a subject’s finger. The Portapres measured pulse rate and blood pressure for every heartbeat in real time. The measurements were recorded offline and then downloaded onto a PC using beatscope software. Using this software, the measurements were exported into a beat to beat format in an Excel spreadsheet. Each row in Excel indicated a heartbeat. For each heart beat, the precise time relative to the start of the recording was given as well as the pulse rate, systolic blood pressure, diastolic blood pressure and mean arterial pressure.
The E-prime software that was used to present stimuli recorded the time to 0.001 ms that each stimulus presentation occurred relative to a programmed starting point. The Portapres marked recordings with an event when a button on the main portable unit was pressed. E-prime was programmed so that pressing a keyboard response initiated the start of stimuli presentations. An event key on the Portapres was pressed at the same time as this keyboard response creating a manually synchronised starting point in both recordings. E-prime then recorded exactly when stimuli were presented relative to this synchronised starting point. The time given for each heart beat in the Portapres recording was then recalculated to be relative to this synchronised starting point. The E-prime recorded stimuli presentation times were then applied to the Portapres recording. Analysis of pulse rate and blood pressure changes within specific time ranges was therefore possible to derive. This enabled us to measure the autonomic response to each of the stimuli presented for 6 s. As in previous studies, baseline was taken from the three heart beats before presentation (Jonsson and Sonnby-Borgstrom 2003; Sarlo et al. 2005). Response was indexed as the mean change from baseline across the 6-s presentation of each stimulus. Mean systolic blood pressure and pulse rate responses (as described below) for each stimulus type were derived as outcome variables.
It was not possible to further synchronise the presentations of stimuli with Portapres recordings. This was because the Portapres cannot output communication to software to indicate to present stimuli directly following a heartbeat. Further equipment that has this function was not possible to use outside of the laboratory. It was important to see women in home settings for representative recruitment of pregnant women and the advantages of seeing women in their relaxed home setting.
Outcome measures
Diastolic, systolic and mean arterial blood pressures were recorded by the Portapres. However, due to the time-consuming nature of the manual analysis of each cardiac response, it was not practical to investigate each of these indices of cardiac changes in this study. We selected systolic blood pressure as the most widely used measure of sympathetic nervous system activity. Furthermore, studies that have looked at both systolic and diastolic blood pressure responses towards emotional stimuli have found similar effects in both indices of blood pressure (Sarlo et al. 2005).
Our primary prediction was that there would be an increase in sympathetic arousal. As such, our primary outcome variable was change in systolic BP (millimetre of mercury). This response was derived as the mean systolic blood pressure during the 6-s stimuli presentation minus the mean systolic blood pressure during the three heart beats before presentation. Our secondary outcome variable was change in pulse rate. Pulse rate responses, particularly heart rate decelerations, also give an indication of parasympathetic responses. This response was derived as the mean pulse rate during the 6-s stimuli presentation minus the mean pulse rate during the three heart beats before presentation.
Clinical interview schedule
The CIS-R is a self-administered, computerised interview that establishes the severity of 14 symptoms which constitute anxiety and depression disorders using algorithms based on ICD-10 criteria (Lewis et al. 1992). Each symptom is scored on a scale from 0 to 4, according to the severity (frequency, duration and unpleasantness) of the symptom experienced. The CIS-R is widely used to detect common mental health disorders in the UK including use in the National Surveys of Psychiatric Morbidity (Bebbington et al. 2003) .The interview has been fully standardised and the interview is equally reliable whether conducted by a lay or clinically trained interviewer (Lewis et al. 1992). The computerised version shows very close agreement with the interviewer-administered version (Patton et al. 1999; Bell et al. 2005).
Initial reliability studies for the CIS-R were conducted in primary health care clinics, a correlation between CIS-R scores on initial and repeated interviews was 0.9 and a reliability estimate of 0.79 was found using a confirmatory factor analysis model (Lewis et al. 1992). The CIS-R was also validated against clinical judgements of trained psychiatrists, and the correlation between CIS-R score and clinical judgement was 0.77 (Lewis et al. 1992). The CIS-R is designed for and has been widely used within community samples (Brugha et al. 2003; Brugha et al. 2005a, b; Lewis et al. 2003; Targosz et al. 2003) including repeated use at baseline and follow-up (Brugha et al. 2005a, b; Weich et al. 1997). The reliability and validity of the CIS-R are comparable to another commonly used clinical interview, the Composite International Diagnostic Interview (Brugha et al. 2005a, b; Lewis et al. 1992).
Where the CIS-R indicated the presence of an anxiety or depressive disorder, women were informed and advised to inform their GP if they felt they needed help. Women were asked to provide information at both test sessions regarding current medication or medical treatment for mental health problems. No participants reported use of medication or treatment for mental health problems.
Symptoms of depression
As described in the “Introduction”, we hypothesised that anhedonic symptoms of depression specifically may be associated with disrupted response towards infant distress. Furthermore, these anhedonic symptoms (a low mood and/ or loss of pleasure for a significant duration, frequency and impact to functioning as specified in ICD-10 criteria) provide the ‘entry criteria’ for a depressive episode in ICD-10 as well as DSM-IV. These symptoms are currently used in the UK to screen for antenatal depression because they have been shown to have a high sensitivity for detecting perinatal depression in primary care equivalent with other case finding instruments such as the Quick Diagnostic Interview Schedule (Whooley et al. 1997).
At least two of seven possible associated symptoms are also required for a diagnosis (disturbed appetite, sleep, motor responses and concentration, fatigue, poor self-esteem and suicidality). However, some of these associated symptoms may be confounded by physiological changes during pregnancy. In particular, appetite problems are suggested to be invalid to discriminate depression during pregnancy (Kammerer et al. 2009) and symptoms of fatigue were found in 85 % of the current sample. CIS-R total scores and diagnoses were therefore potentially problematic indicators of depression during pregnancy. Furthermore, there are no diagnostic interviews validated for depression during pregnancy specifically. Therefore, we categorised women into those with and without anhedonic depressive symptoms This method was also adopted in our previous study looking at the influence of depression on attentional response to infant distress (Pearson et al. 2010).
Analyses
All analyses were performed using stata version 9. In order to investigate the influence of depressive symptoms on autonomic responses, we used random effect linear regression analyses. We adopted linear regression models because autonomic measures were continuous and normally distributed. Random effect linear regression models were used because these analyses model repeated observations from the same individual. This is because such analyses take a multi-level modelling approach and model both at the individual and observation levels. For example, these analyses take into account all of the early and late pregnancy observations because they use each observation from an individual as a single data point (i.e. if the same woman took part in both sessions she would have two data points, if she only took part in one session she had one data point) whilst taking into account the paired nature of the data.
Although these analyses included individuals with data at one time point only, there is no reason to believe that this should bias findings. For example, there was no evidence for differences in any of the potentially confounding variables between the women who were tested during early pregnancy and the women who remained during late pregnancy (see table preliminary analyses below). Furthermore, adjustments were made for demographic variables in all analysis (see below). Random effect analyses were preferred as they take into account all available data and maximise power.
For the linear random effects regression model, the outcome variables were autonomic responses towards infant distress. The exposure variable was the presence of depressive symptoms (1 = present or 0 = not present). The random effects model approach allowed us to compare the effect of each observation of depression on the co-occurring physiological response. The effect of stage of pregnancy was automatically adjusted for in these analyses to take account of the fact that some observations of depression were during early and some during late pregnancy. All analyses were performed with and without adjustments for the potential confounding variables described below.
Results
Sample demographics
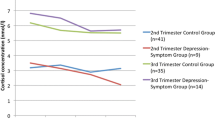
The 72 women who took part in the physiological task during early pregnancy were on average 29.5 years old, at 11 weeks gestation (range 7–14 weeks S.D. 13 days), and 45 % were multiparous and 22 (30 %) were experiencing one or more symptoms of depression. The 51 women who took part in the physiological task during late pregnancy were on average 29.1 years old, at 36 weeks (range 33–39 SD 10 days) gestation, and 42 % were multiparous and 16 (31 %) were experiencing symptoms of depression (see Table 1). Eleven women (50 % of the depressive symptom group) during early pregnancy and eight women (50 % of the depressive symptom group) during late pregnancy met ICD-10 criteria for a depressive episode. The mean combined symptom severity score (sum of the two individual depressive symptom severity scores each with a range of 0–4) in the depressive symptom groups were 3.0 (SD = 2.0) during early and 2.0 (SD = 1.1) during late pregnancy. Out of the total 38 observations (across early and late pregnancy) where women were experiencing symptoms of depression, in 24 (63 %) observations, women were also experiencing one or more symptoms of anxiety. There was a high level of comorbidity between symptoms of anxiety and depression, as would be expected. However, it was not possible to compare comorbid and non-comorbid groups due to low sample sizes.
Preliminary analyses
Association between depression and confounding variables
Using linear regression and chi-squared analyses of the early and late pregnancy data, depressive symptoms were associated with a younger age (during early pregnancy, β = −2.5, 95 % CI −5.4 to 0.1, p = 0.09 and late pregnancy, β = −5.1, 95 % CI −8.1 to −2.2, p = 0.001), single marital status (during early pregnancy, chi-squared (2) = 10.3, p = 0.006 and late pregnancy, chi-squared (2) = 4.6, p = 0.09) and an unplanned pregnancy (during early pregnancy, chi-squared (1) = 8.2, p = 0.004 and during late pregnancy, chi-squared (1) = 3.0, p = 0.09). We therefore controlled for these variables in our analyses to investigate the association between depression and responses to infant distress. There were no significant associations between depressive symptoms at either stage of pregnancy and social class, education level or gestation. However, as these variables are theoretically and previously related to depression and maternal responses, they were also controlled for.
Association between autonomic responses and confounding variables
To investigate the influence of socio-demographic variables on autonomic responses across early and late pregnancy, random effect logistic regression analyses were performed to take account of the repeated observations for individuals across pregnancy stage. There were no main effects of age, planned pregnancy, parity or marital status on autonomic responses towards infant distress. However, there was a trend for multiparous women to show greater systolic blood pressure responses towards infant distress than primiparous women (β = 1.0, 95 % CI −0.1 to 2.1, p = 0.08). This is consistent with previous research (Stallings et al. 2001) and it was therefore particularly important to control for parity in our main analyses. Correlations between variables are given in Table 2.
Main analyses
Association between symptoms of depression and autonomic responses towards infant distress
We predicted that symptoms of depression during pregnancy would disrupt autonomic responses towards infant distress. To investigate this prediction, we looked at all observations from the pregnant sample from both early and late stages. We compared observations where women were experiencing symptoms of depression with observations where they were not (total of 123 observations, 72 in early pregnancy and 51 in late pregnancy). As can be seen in Table 3, women’s systolic blood pressure responses to infant distress were greater in the presence of depressive symptoms during pregnancy. However, there were no differences in response to irrelevant stimuli. There were also no differences in pulse rate responses according to depression for either condition.
A random effects linear regression model, incorporating all observations from early and late pregnancy (n = 123), was performed to investigate the relationship between depressive symptoms during pregnancy and autonomic responses to infant distress statistically.
Systolic BP responses
Systolic blood pressure response to infant distress was the dependent variable and the presence of depressive symptoms (0 = none, 1 = present) was the independent variable. Adjustments were made for the covariates of stage, parity, age, social class, marital status, gestation (weeks) and planned pregnancy. As can be seen in Table 4, these analyses revealed that, after these adjustments, the systolic blood pressure response to infant distress in pregnant women with depressive symptoms was 1.6 mmHg (95 % CI 0.5 to 2.6, p = 0.004) higher than women without such symptoms. This is equivalent to an increase in systolic blood pressure change of 0.6 standard deviations. However, when repeating this analysis for systolic blood pressure responses towards irrelevant stimuli, we found no differences between those with and without symptoms of depression (see Table 4).
Pulse rate responses
The main analyses were repeated with change in pulse rate in response to infant distress as the outcome variable. This analysis found no evidence for any differences between pulse rate responses to infant distress between observations in the presence or absence of symptoms of depression (crude β = −0.2, 95 % CI −1.1 to 0.7, p = 0.6; adjusted β = 0.3, 95 % CI −0.7 to 1.3, p = 0.6). There was also no evidence for any differences between pulse rate responses to irrelevant stimuli between observations in the presence or absence of symptoms of depression (before adjustments β = 0.1, 95 % CI −0.9 to 1.1, p = 0.8; adjusted β = 0.1, 95 % CI −1.0 to 1.2, p = 0.8).
Discussion
We found that anhedonic symptoms of depression during pregnancy were associated with heightened systolic blood pressure towards infant distress stimuli. This was not explained by greater systolic blood pressure response to arousing stimuli in general because there was no evidence that such symptoms influenced women’s autonomic responses towards irrelevant stimuli. These results may provide insight into the two competing explanations for our previous findings that depression during pregnancy disrupts attentional engagement with distressed infant faces (Pearson et al. 2010). For example, these findings suggest that anhedonic pregnant women were not, in their systolic blood pressure responses at least, insensitive to infant distress signals. Rather they were showing a greater response to these signals. In fact, these results suggest that anhedonic pregnant women were more sensitive to infant distress signals compared to non-depressed women. This may discount the insensitivity explanation for our previous findings and would be consistent with an avoidance of infant distress signals.
However, sympathetic responses, such as increases in systolic blood pressure, do not give an indication of the valence of the sympathetic arousal. For example, increased arousal is found for relevant signals that are both unpleasant, for example threat, and pleasant, for example erotic pictures (Sander et al. 2003; Sarlo et al. 2005). This is because the purpose of sympathetic responses is to prepare the organism to act upon important stimuli. As such, it is not possible to conclude that a more sensitive sympathetic response is due to a negative/avoidance response towards infant distress. Indeed, the increased sympathetic response would also be consistent with an increased appetitive motivation to approach the distress signal. However, taken together with our previous finding that depressed women showed reduced attentional engagement with infant distress, this increased response is most consistent with an aversive reaction and avoidance of these stimuli. Further indication that the physiological oversensitivity we report here may be more consistent with cognitive avoidance of the stimuli comes from previous research that depression is associated with impairments in women’s conscious ability to distinguish infant cries (Donovan et al. 1998). For example, the heightened blood pressure response we report here may lead to impairments rather than greater sensitivity in later processing of distress.
Neuro-imaging of depressed pregnant women’s response to infant distress would be necessary to establish whether disrupted responses to infant distress result from abnormal reward activation. Such research may also disentangle whether disrupted responses are due to insensitivity, which would be represented by the lack of reward activation, or an avoidance, which would be represented by activation of areas associated with negative affect. Previous research in mothers who show insecure attachment styles has suggested that, in response to infant distress, these mothers show a reduced reward response and increased activation in regions associated with negative affect (Strathearn et al. 2009). This may suggest that disrupted maternal responses are associated with both a lack of reward and an avoidance of infant distress. Similar neuro-imaging work could explore reward and affective responses towards infant distress in depressed and non-depressed pregnant women.
The findings of increased systolic blood pressure responses in women experiencing anhedonic symptoms are consistent with increases in sympathetic responses. However, there was no evidence for an increase in parasympathetic orientation responses, which would be reflected by pulse rate decelerations. However, it is possible that changes in parasympathetic arousal were undetected because they were counterbalanced by sympathetic changes. For example, overall pulse rate responses across 6 s were the combined effect of sympathetic (acceleratory) and parasympathetic (deceleratory) pulse rate responses. As such, parasympathetic responsivity towards stimuli may have also increased during late pregnancy but this may have balanced the effect of increased sympathetic responsivity on overall pulse rate responses. This would have resulted in no overall changes in response. Precisely mapping pulse rate to smaller and unknown portions of time within the 6-s period, in order to investigate accelerative and decelerative components, was unfortunately not possible in the current study.
Limitations
Some limitations should be noted. Firstly, further work is needed to investigate how sympathetic responses towards infant distress are related to a mother’s behavioural response towards her own infant’s distress in real life. As such, the relevance of the current findings for mother–infant interactions is still unclear. However, if shown to be relevant to behaviour, understanding of the impact of depression on autonomic responses towards infant distress may guide interventions to improve maternal responses in depressed women.
Another potential limitation was that a number of women did not complete the late pregnancy phase of the study. This may have led to a biased late pregnancy sample. However, dropout was mainly due to miscarriages and premature births and these rates were similar to national rates. There is no reason to believe that these women would have been different in regard to their responses to infant distress if they had reached late pregnancy. Furthermore, sample demographics were very similar in the early and in the late pregnancy sample. Therefore, there was no evidence that the complete case sample was biased relative to the early pregnancy sample.
Due to constraints of the home setting and physiological recordings, it was only possible to obtain physiological responses from a subsample (70 %) of the women that were originally recruited. The main reason for not completing the autonomic tasks was the presence of a significant distracter in the home (most often a barking dog or another child). In addition, time constraints of the test session meant that where it was not possible to reasonably quickly obtain an autonomic recording, women had to move on to other tasks. However, there was no evidence that the sample of women who completed the autonomic task were different from the full sample. As such, there is no reason to believe that women for whom we did not obtain physiological responses were different with regards to their response towards infant distress.
This study looked at the relationship between autonomic responses to infant distress and depressive symptoms within a non-clinical sample. Half of the women classed as showing anhedonic depressive symptoms did meet criteria for depression. However, the current study did not have sufficient power to look conclusively at women who had a diagnosis of depression separately. Therefore, the implications for pregnant women with a diagnosis of depression by a psychiatrist according to DSM-IV criteria are unclear. Furthermore, the women in this study were in general in good social circumstances. Therefore, the effect of depressive symptoms on autonomic responses to infant distress in women living in social adversity is unclear.
Finally, it is important to note that the autonomic recording equipment was only manually synchronised to the stimuli presentations. This resulted in crude measurements of autonomic responses which may have been less sensitive to changes within smaller portions of time across the overall response. For example, the first few milliseconds of responses to stimuli may have been slightly misaligned. As explained above, this may explain why no differences in pulse rate responses were detected between those with and without depression. However, despite the crude measure, differences were detected in systolic blood pressure response towards infant distress between women with and without anhedonic symptoms. In addition, due to the time-consuming nature of the manual analysis of each cardiac response, it was not practical to investigate further indices of cardiac changes such as diastolic blood pressure or mean arterial blood pressure in this study. It was also considered unnecessary to investigate these indices because they all reflect sympathetic arousal. Indeed, similar changes in systolic, diastolic and mean arterial blood pressure were seen in all these indices of blood pressure in response to emotional stimuli in previous research (Sarlo et al. 2005). Nonetheless, future studies are needed to replicate these findings using more sophisticated and sensitive laboratory based autonomic recordings and using more ecologically valid stimuli such as video clips.
Conclusion
In conclusion, the results provide further evidence that anhedonic symptoms during pregnancy are associated with abnormal responses towards infant distress. Further work is needed to clarify whether these responses are relevant to maternal behaviour and mother–infant interactions. However, the findings could provide insight as to why depression during pregnancy leads to poor infant development and suggest that we should consider the impact of depression during pregnancy on maternal responses as well as depression that occurs after birth.
References
Bebbington P, Dunn G, Jenkins R, Lewis G, Brugha T, Farrell M et al (2003) The influence of age and sex on the prevalence of depressive conditions: report from the National Survey of Psychiatric Morbidity. Int Rev Psychiatry 15:74–83
Bell T, Watson M, Sharp D, Lyons I, Lewis G (2005) Factors associated with being a false positive on the General Health Questionnaire. Soc Psychiatry Psychiatr Epidemiol 40:402–407
Bennett HA, Einarson A, Taddio A, Koren G, Einarson TR (2004) Prevalence of depression during pregnancy: systematic review. Obstet Gynecol 103:698–709
Bergman K, Sarkar P, O’Connor TG, Modi N, Glover V (2007) Maternal stress during pregnancy predicts cognitive ability and fearfulness in infancy. J Am Acad Child Adolesc Psychiatry 46:1454–1463
Bradley MM, Codispoti M, Cuthbert BN, Lang PJ (2001) Emotion and motivation I: defensive and appetitive reactions in picture processing. Emotion 1:276–298
Brugha TS, Meltzer H, Jenkins R, Bebbington PE, Taub NA (2005a) Comparison of the CIS-R and CIDI lay diagnostic interviews for anxiety and depressive disorders. Psychol Med 35:1089–1091
Brugha TS, Morgan Z, Bebbington P, Jenkins R, Lewis G, Farrell M et al (2003) Social support networks and type of neurotic symptom among adults in British households. Psychol Med 33:307–318
Brugha TS, Weich S, Singleton N, Lewis G, Bebbington PE, Jenkins R et al (2005b) Primary group size, social support, gender and future mental health status in a prospective study of people living in private households throughout Great Britain. Psychol Med 35:705–714
Deave T, Heron J, Evans J, Emond A (2008) The impact of maternal depression in pregnancy on early child development. BJOG 115:1043–1051
Dipietro JA, Costigan KA, Gurewitsch ED (2005) Maternal psychophysiological change during the second half of gestation. Biol Psychol 69:23–38
Donovan WL, Leavitt LA, Walsh RO (1998) Conflict and depression predict maternal sensitivity to infant cries. Infant Behav Dev 21:505–517
Drevets WC (2000) Neuroimaging studies of mood disorders. Biol Psychiatry 48:813–829
Evans J, Heron J, Francomb H, Oke S, Golding J (2001) Cohort study of depressed mood during pregnancy and after childbirth. BMJ 323:257–260
Field T, Hernandez-Reif M, Diego M (2006) Intrusive and withdrawn depressed mothers and their infants. Dev Rev 26:15–30
Field T (2010) Postpartum depression effects on early interactions, parenting, and safety practices: a review. Infant Behav Dev 33:1–6
Field T (2011) Prenatal depression effects on early development: a review. Infant Behav Dev 34(1):1–14
Frodi AM, Lamb ME (1980) Child abusers’ responses to infant smiles and cries. Child Dev 51:238–241
Gavin NI, Gaynes BN, Lohr KN, Meltzer-Brody S, Gartlehner G, Swinson T (2005) Perinatal depression: a systematic review of prevalence and incidence. Obstet Gynecol 106:1071–1083
Hay DF, Pawlby S, Waters CS, Perra O, Sharp D (2010) Mothers’ antenatal depression and their children’s antisocial outcomes. Child Dev 81:149–165
Jonsson P, Sonnby-Borgstrom M (2003) The effects of pictures of emotional faces on tonic and phasic autonomic cardiac control in women and men. Biol Psychol 62:157–173
Kammerer M, Marks MN, Pinard C, Taylor A, von Castelberg B, Kunzli H et al (2009) Symptoms associated with the DSM IV diagnosis of depression in pregnancy and post partum. Arch Womens Ment Health 12:135–141
Keedwell PA, Andrew C, Williams SC, Brammer MJ, Phillips ML (2005) The neural correlates of anhedonia in major depressive disorder. Biol Psychiatry 58:843–853
Keyser-Marcus L, Stafisso-Sandoz G, Gerecke K, Jasnow A, Nightingale L, Lambert KG et al (2001) Alterations of medial preoptic area neurons following pregnancy and pregnancy-like steroidal treatment in the rat. Brain Res Bull 55:737–745
Kim-Cohen J, Moffitt TE, Taylor A, Pawlby SJ, Caspi A (2005) Maternal depression and children’s antisocial behavior: nature and nurture effects. Arch Gen Psychiatry 62:173–181
Knutson B, Bhanji JP, Cooney RE, Atlas LY, Gotlib IH (2008) Neural responses to monetary incentives in major depression. Biol Psychiatry 63:686–692
Leerkes EM, Nayena BA, O’Brien M (2009) Differential effects of maternal sensitivity to infant distress and nondistress on social–emotional functioning. Child Dev 80:762–775
Lewis G, Bebbington P, Brugha T, Farrell M, Gill B, Jenkins R et al (2003) Socio-economic status, standard of living, and neurotic disorder. Int Rev Psychiatry 15:91–96
Lewis G, Pelosi AJ, Araya R, Dunn G (1992) Measuring psychiatric disorder in the community: a standardized assessment for use by lay interviewers. Psychol Med 22:465–486
Mantymaa M, Puura K, Luoma I, Salmelin R, Davis H, Tsiantis J et al (2003) Infant–mother interaction as a predictor of child’s chronic health problems. Child Care Health Dev 29:181–191
Martin-Soelch C (2009) Is depression associated with dysfunction of the central reward system? Biochem Soc Trans 37:313–317
McElwain NL, Booth-Laforce C (2006) Maternal sensitivity to infant distress and nondistress as predictors of infant–mother attachment security. J Fam Psychol 20:247–255
Murray L, Fiori-Cowley A, Hooper R, Cooper P (1996a) The impact of postnatal depression and associated adversity on early mother-infant interactions and later infant outcome. Child Dev 67:2512–2526
Murray L, Hipwell A, Hooper R, Stein A, Cooper P (1996b) The cognitive development of 5-year-old children of postnatally depressed mothers. J Child Psychol Psychiatry 37:927–935
Naranjo CA, Tremblay LK, Busto UE (2001) The role of the brain reward system in depression. Prog Neuropsychopharmacol Biol Psychiatry 25:781–823
Numan M (2007) Motivational systems and the neural circuitry of maternal behavior in the rat. Dev Psychobiol 49:12–21
O’Brien LM, Heycock EG, Hanna M, Jones PW, Cox JL (2004) Postnatal depression and faltering growth: a community study. Pediatrics 113:1242–1247
Patton GC, Coffey C, Posterino M, Carlin JB, Wolfe R, Bowes G (1999) A computerised screening instrument for adolescent depression: population-based validation and application to a two-phase case-control study. Soc Psychiatry Psychiatr Epidemiol 34:166–172
Pearson RM, Cooper RM, Penton-Voak IS, Lightman SL, Evans J (2010) Depressive symptoms in early pregnancy disrupt attentional processing of infant emotion. Psychol Med 40:621–631
Pearson RM, Lightman SL, Evans J (2009) Emotional sensitivity for motherhood: late pregnancy is associated with enhanced accuracy to encode emotional faces. Horm Behav 56:557–563
Pizzagalli DA, Holmes AJ, Dillon DG, Goetz EL, Birk JL, Bogdan R et al (2009) Reduced caudate and nucleus accumbens response to rewards in unmedicated individuals with major depressive disorder. Am J Psychiatry 166:702–710
Sander D, Grafman J, Zalla T (2003) The human amygdala: an evolved system for relevance detection. Rev Neurosci 14:303–316
Sarlo M, Palomba D, Buodo G, Minghetti R, Stegagno L (2005) Blood pressure changes highlight gender differences in emotional reactivity to arousing pictures. Biol Psychol 70:188–196
Schaefer HS, Putnam KM, Benca RM, Davidson RJ (2006) Event-related functional magnetic resonance imaging measures of neural activity to positive social stimuli in pre- and post-treatment depression. Biol Psychiatry 60:974–986
Shaw DS, Schonberg M, Sherrill J, Huffman D, Lukon J, Obrosky D et al (2006) Responsivity to offspring’s expression of emotion among childhood-onset depressed mothers. J Clin Child Adolesc Psychol 35:490–503
Shin H, Park YJ, Kim MJ (2006) Predictors of maternal sensitivity during the early postpartum period. J Adv Nurs 55:425–434
Siddiqui A, Hagglof B (2000) Does maternal prenatal attachment predict postnatal mother–infant interaction? Early Hum Dev 59:13–25
Stallings J, Fleming A, Corter C, Worthman C, Steiner M (2001) The effects of infant cries and odors on sympathy, cortisol, and autonomic responses in new mothers and non-postpartum women. Parenting Sci Pract 1:71–100
Stein A, Arteche A, Lehtonen A, Craske M, Harvey A, Counsell N et al (2010) Interpretation of infant facial expression in the context of maternal postnatal depression. Infant Behav Dev 33:273–278
Strathearn L, Fonagy P, Amico J, Montague PR (2009) Adult attachment predicts maternal brain and oxytocin response to infant cues. Neuropsychopharmacology 34(13):2655–2666
Swain JE, Lorberbaum JP, Kose S, Strathearn L (2007) Brain basis of early parent–infant interactions: psychology, physiology, and in vivo functional neuroimaging studies. J Child Psychol Psychiatry 48:262–287
Talge NM, Neal C, Glover V (2007) Antenatal maternal stress and long-term effects on child neurodevelopment: how and why? J Child Psychol Psychiatry 48:245–261
Targosz S, Bebbington P, Lewis G, Brugha T, Jenkins R, Farrell M et al (2003) Lone mothers, social exclusion and depression. Psychol Med 33:715–722
Thun-Hohenstein L, Wienerroither C, Schreuer M, Seim G, Wienerroither H (2008) Antenatal mental representations about the child and mother–infant interaction at three months post partum. Eur Child Adolesc Psychiatry 17:9–19
Turpin G, Schaefer F, Boucsein W (1999) Effects of stimulus intensity, risetime, and duration on autonomic and behavioral responding: implications for the differentiation of orienting, startle, and defense responses. Psychophysiology 36:453–463
Weich S, Churchill R, Lewis G, Mann A (1997) Do socio-economic risk factors predict the incidence and maintenance of psychiatric disorder in primary care? Psychol Med 27:73–80
Wiesenfeld AR, Malatesta CZ, Deloach LL (1981) Differential parental response to familiar and unfamiliar infant distress signals. Infant Behav Dev 4:281–295
Whooley MA, Avins AL, Miranda J, Browner WS (1997) Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med 12(7):439–45
Acknowledgments
This study was supported by an MRC studentship held at the University of Bristol by R. Pearson. Participant’s payment of £7.50 was given for the additional tasks they completed at the test session, which was supported by a British Academy small grant held by I. Penton-Voak. We thank the Community Midwifery team based at Southmead Hospital who greatly assisted with recruitment and the women and their partners who took part in the study.
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Pearson, R.M., Lightman, S.L. & Evans, J. Symptoms of depression during pregnancy are associated with increased systolic blood pressure responses towards infant distress. Arch Womens Ment Health 15, 95–105 (2012). https://doi.org/10.1007/s00737-012-0269-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00737-012-0269-z