Abstract
Breast cancer is a multifactorial disease classified by several sub-types which differ from each other by risk factors, specific molecular promoters and severity of outcomes. Tumour aggressiveness and metastatic disease are the key determinants of breast cancer outcomes. Tumour cell ability to degrade the extracellular matrix and to be motile is the hallmark of invasion and essential step in a development of breast cancer metastatic disease. Therefore, a coordinated action between cell motility and ability to degrade the extracellular matrix is currently under extensive investigation focused on molecular targets for both diagnostic and therapeutic purposes. Contextually, our current study was dedicated to patient stratification utilising MMP-9 serum activity levels and RhoA expression patterns measured in circulating leucocytes. Biomarker patterns were “masked” in non-stratified patient groups. In contrast, the multiparametric stratification approach led to highly improved clinical utility of biomarker patterns. Presented stratification system is recommended for population screening as a cost-effective non-invasive approach to facilitate predictive diagnostics of breast cancer predisposition, pre-lesions and early stages, when the pathology can be effectively prevented or cured. Proposed approach might be particularly useful for early and predictive breast cancer diagnostics applied to certain phenotypes such as premenopausal rather than postmenopausal women, women with dense breast tissue, where highly increased RhoA/MMPs activities are utilised for effective proteolysis of the matrix and cancer cell migration into dense matrices, as well as for breast cancer of unclear origin such as particularly aggressive triple-negative sub-type.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
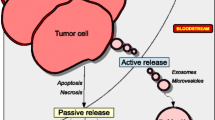
Breast cancer (BC) is the leading cancer type in female populations with permanently increasing prevalence and the leading cause of cancer-related mortality in females worldwide (WHO 2012). BC epidemic in the early 21st century is alarming for healthcare on a global scale (Golubnitschaja et al. 2016b). BC is a multifactorial disease classified by several sub-types which differ from each other by risk factors, specific molecular promoters and severity of outcomes. Tumour aggressiveness and metastatic disease are the key determinants of breast cancer outcomes. In case of particularly aggressive BC types, haematogenous dissemination of circulating tumour cells (CTC) can occur even before the primary tumour is or may be detected (Bhandary et al. 2015). Moreover, a surgical resection of tumour can increase the CTC invasion 1000-fold (Camara et al. 2006; Goldfarb and Ben-Eliyahu 2006). BC metastatic disease (BCMD) is a systemic disease with a local implication, when the advantageous microenvironment is created for a growth expansion of secondary tumours (metastases) originated from the CTC nested in distanced organs such as bones, lung, liver and brain. Although exact conditions which best meet the requirements of the advantageous microenvironment for distant metastases are yet not known, there is an accumulating evidence for hypoxic conditions (Cox et al. 2015), some classes of signalling molecules and other molecular pathways worsening the outcomes in BCMD.
Tumour cell ability, first, to degrade the extracellular matrix (ECM) and, second, to be motile is the hallmark of invasion and a consequent development of BCMD.
Regarding the 1st attribute, herewith we provide the rationale for measuring serum MMP-9 activities
An extensive degradation of ECM is essential for an effective tumour progression and aggressive metastatic disease. To the molecular pathways per evidence involved in the BCMD progression belong several proteolytic enzyme systems, one of which is the family of matrix metalloproteinases (MMPs). Excessive degradation of the extracellular matrix (ECM) and basement membrane facilitating the penetration of cancer cells through the tissue and into blood stream is believed to be the principal mechanism of the MMP-dependent tumour invasion and metastases spread (Egeblad and Werb 2002). In particular, the activity of gelatinase B (MMP-9) elevated in BC is associated with poor prognosis specifically in BC (Ranuncolo et al. 2003; Talvensaari-Mattila et al. 2003; Leppä et al. 2004), metastatic disease in the most aggressive BC phenotypes (such as triple-negative breast cancer) (Mehner et al. 2014) and formation of one of the most fatal type of distanced metastases, namely the liver metastases in BCMD (Tabariès et al. 2015).
There are several steps in the regulation cascade of MMP-9 patterns resulting in the “end-product”, namely the extracellular gelatinase activity which can be ex vivo measured in blood serum samples by Zymography and has been demonstrated as highly relevant for BC prognosis and development of metastatic disease (Provatopoulou et al. 2009; Sung et al. 2012). Consequently, our current paper hypothesises the clinical utility of the patient stratification by serum activities of MMP-9.
Regarding the 2nd attribute, herewith we provide the rationale for measuring RhoA expression patterns in circulating leucocytes
Although some pathology-specific molecular signatures and circulating biomarkers have been identified in breast cancer, there is a lack of validated molecular patterns to optimise predictive diagnostics and targeted prevention and/or treatment of metastatic disease (Marino et al. 2013). For these purposes, a coordinated action between cell motility and ability to degrade the ECM is currently under extensive investigation focused on molecular targets for both diagnostic and therapeutic purposes. Contextually, Rho family GTPases are the most potent molecular targets promoting cell migration, invasion of the extracellular matrix, and metastasis. Specifically, the RhoA/MMPs pathway is considered as concerted for the cancer cell-specific motility and ability to degrade the ECM and a potential therapeutic target even for the most problematic triple-negative, basal-like breast cancers (Cáceres et al. 2005; Fagan-Solis et al. 2013; Sun et al. 2016). Indeed, the activation of the small G protein RhoA is essential for cancer migration and invasion: during cell movement through ECM, RhoA controls the actomyosin contraction crucial for efficient ECM invasion and metastasing (Narumiya et al. 2009; Friedl and Wolf 2010; Sanz-Moreno and Marshall 2010; Carr et al. 2013).
Further, our previous study revealed shifted expression patterns of RhoA in circulating leucocytes of breast cancer patients compared to non-diseased controls (Golubnitschaja et al. 2013). Therefore, specific expression patterns of RhoA in circulating leucocytes are considered clinically useful for evaluating the pathology-specific molecular signature. Consequently, our current paper hypothesises the clinical utility of the expression patterns of RhoA in circulating leucocytes of breast cancer patients.
Taking into consideration the above summarised facts, our current study was dedicated to non-invasive multiparametric approach to stratify patients with breast benignancies and malignancies utilising MMP9 serum activity levels and RhoA expression patterns measured in circulating leucocytes. Potential impacts are considered as being remarkable for overall breast cancer risk assessment, early/predictive diagnostics and targeted treatments.
Materials and methods
Recruitment of patients
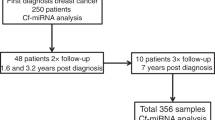
Altogether, 161 patients proportionally distributed between two pools with malignant (invasive lobular and ductal carcinomas, 82 patients) and group with benignant breast alterations (fibroadenomas, fibrocystic diseases, lipomas, adenosis and breast traumas, 79 patients) were recruited at the “Breast Cancer Research Center”, Rheinische Friedrich-Wilhelms-University of Bonn. According to the diagnosis, the recruited patients were grouped as follows: benign breast alterations in premenopausal women (group 1, n = 59); benign breast alterations in postmenopausal women (group 2, n = 20); invasive breast cancer in premenopausal women (group 3, n = 19); invasive breast cancer in postmenopausal women (group 4, n = 63). Blood samples of all patients with breast tumours were taken prior to core needle biopsy at the Department of Obstetrics and Gynaecology. All study participants were informed about the purposes of the study and signed their consent of the patient. All investigations conformed to the principles outlined in the Declaration of Helsinki and were performed with permission by the responsible Ethic’s Committee of the Medical Faculty, University of Bonn. Each blood sample underwent an immediate isolation of blood serum and circulating leucocytes.
Isolation of blood serum, circulating leucocytes, biobanking and biopreservation
Blood samples (20 ml) anti-coagulated with heparin were collected from patients. Blood serum was isolated from 0.5 ml individual blood samples by a direct centrifugation as decribed elsewhere, consequently frozen and stored till the zymography was performed (see below the “Zymography” description). Circulating leucocytes were separated from 19.5 ml individual blood samples using Fi-coll-Histopaque gradients (Histopaque 1077, Sigma, USA) as described previously (Golubnitschaja-Labudova et al. 2000). Briefly, blood samples were diluted with equal volumes of physiological buffer solution (PBS, Biochrom AG, Germany). Then, 2 ml of histopaque was placed into 10 ml sterile centrifuge tubes and 5 ml of diluted blood samples was carefully layered onto each histopaque gradient. Gradients were centrifuged at 475g and 20 °C for 15 min. The leucocyte bands were removed from the interface between plasma and histopaque layers of each tube and collected into one 50 ml tube. The total volume was brought to 50 ml with cold Dulbecco’s Modified Eagle Medium (DMEM, Gibco™, USA). The cell suspension was washed three times with PBS, aliquoted and the total number of cells was determined in each aliquot. Leucocytes were frozen as dry pellets. All the samples with frozen leucocytes were stored at −80 °C before being processed for the "Western-Blot" analysis (see below the corresponding description).
Zymography
For determination of the gelatinase activity B (MMP-9) in blood serum “Ready-gelatin-gels” (Bio-Rad, USA) were used according to the instructions of the manufacturer. Two microliters from individual serum samples were electrophoresed under non-reducing conditions using Criterion™ Precast Gel System (Bio-Rad, USA). After electrophoresis, each gel was incubated at room temperature in 2% Triton X-100 for 2 × 30 min to remove the traces of sodium dodecyl sulphate, and then incubated overnight at 37 °C in buffer (150 mM NaCl, 50 mM Tris–HCl, pH 7.6, containing 5 mM CaCl2 and 0.02% NaN3). Afterwards a staining with 0.5% Coomassie blue G-250 (Sigma, USA) was performed for each gel. The proteolytic activity of gelatinase B was identified as a clear band on a blue background according to the correspondent molecular weight of MMP-9. Gels were dried between cellophane sheets with a GelAir™ Drying System (Bio-Rad, USA) and then scanned with a yellow filter using Adobe Photoshop (Adobe System, USA) in grey-scale mode. Densitometric analysis of zymographic lysis zones at 86 kDa for gelatinases B was performed using “Quantity One” imaging system (Bio-Rad, USA). Evaluation of relative gelatinase activity was performed in arbitrary units followed by sub-grouping according to the “low”, “intermediate” and “high” level of activities measured in individual samples as described previously (Golubnitschaja et al. 2016c).
Western-blot analysis
All analyses were performed two times for each sample as described elsewhere. Primary anti-body incubation was performed at room temperature using a 1:200 dilution of the specific anti-bodies to human RhoA 24 kDa (mouse monoclonal IgG raised against an epitope corresponding to amino acids 120–150 of RhoA of human origin, RhoA (26C4): sc-418 Santa Cruz, USA), and to human actin 43 kDa (goat polyclonal IgG, epitope mapping at the C-terminus of actin of human origin, recommended for detection of a broad range of actin isoforms of human origin, sc-1616 Santa Cruz, USA) The protein-specific signals were measured densitometrically using the “Quantity One®” imaging system (Bio-Rad, USA).
Statistical analysis
For analytical and statistical evaluations, the data were transferred to Microsoft Excel. The Student t test, one-way ANOVA as well as Turkey’s test were applied. P values equal or below 0.05 were considered statistically significant.
Results
Proteolytic activity patterns of MMP-9
Comprehensive patterns of the proteolytic activities of MMP-9 (gelatinase B activity) were systematically analysed followed by sub-grouping according to the “low”, “intermediate” and “high” level of activities measured in individual samples (see Fig. 1). This systematic approach for sub-grouping of MMP-9 activities is described in detail in our currently published article (Golubnitschaja et al. 2016c); its high clinical utility is well justified by the authors.
Proteolytic activity of gelatinase B. Localisation (according to the electrophoretic protein markers—sample M) and evaluation of the gelatinase activity B (MMP-9, 86 kDa) followed by sub-grouping of samples (patients) with the “low”, “middle” and “high” level of activities, where “low” levels correspond to the sample 6, “intermediate”—samples 2 and 4, and “high”—samples 1, 3, 5
Expression patterns of RhoA
Amongst the analytical methods, evaluation of the Western-Blot imaging provides highly precise information about individual values of protein expression measured in corresponding protein bands. RhoA expression imaging revealed either one or two specific bands corresponding to 17 and 24 kDa as demonstrated in Fig. 2. Since both “single-band” and “double-band” images have been reported for RhoA Western-blot analysis (Fritz et al. 1999; Chang et al. 2006), both images have been taken into consideration and statistically analysed in the study.
Consequently, both “single-band” (24 kDa only) and “double-band” (both 17 and 24 kDa) expression patterns of RhoA have been evaluated individually. As demonstrated in Fig. 2, highly heterogeneous expression patterns have been recorded for both patient groups of “malignancies” and “benignancies”. Statistical analysis performed for RhoA patterns in non-stratified patient groups has, further, confirmed highly heterogeneous RhoA expression profiles and consequent necessity of appropriate patient stratification as summarised below.
Statistical analysis of RhoA expression patterns in non-stratified patient groups
In non-stratified patient groups, elevated RhoA expression rates have been recorded for breast cancer patients compared to the benignant group as demonstrated in Fig. 3. In particular, the highest median is demonstrated for the sub-group of premenopausal breast cancer patients. However, Student t test, one-way ANOVA as well as Turkey’s test demonstrate non-significant differences between individual groups. Standard deviations in all sub-groups indicate extremely high level of heterogeneity in both benignant and malignant groups of patients that significantly decreases the level of potential clinical utility for RhoA as a single biomarker and argues in favour of further patient stratification.
Statistical evaluation of the RhoA expression rates in “malignancies” versus “benignancies”: the median values with standard deviation (SD) are presented for corresponding patient groups divided into sub-groups. Corresponding values of the expression rates are provided in arbitrary units. a Single-band expression patterns for RhoA protein corresponding to 24 kDa. b “Double-band” expression patterns for RhoA protein corresponding to 24 and 17 kDa
Multiparametric stratification of the patterns
The results for the multiparametric stratification of the patterns are summarised in Fig. 4. Following stratification parameters have been used:
Stratification results for premenopausal versus postmenopausal women. Median values in corresponding sub-groups are shown for the RhoA expression patterns. “Benign” is used for “benignancies” and “malign” for “malignancies”. For better transparency, corresponding results are presented by both bar plot and 3-D plot. a Premenopausal women, “single-band” RhoA expression patterns. b Postmenopausal women, “single-band” RhoA expression patterns. c Premenopausal women, “double-band” RhoA expression patterns. d Postmenopausal women, “double-band” RhoA expression patterns
-
Hormonal status: premenopausal versus postmenopausal patients;
-
MMP-9 blood serum activity discriminating between sub-groups with “low”, “intermediate” and “high” levels.
This multiparametric stratification approach has allowed for detecting the RhoA patterns which are highly specific for individual sub-group as demonstrated in Fig. 4. These sub-group-specific patterns obviously have been “masked” in non-stratified patient groups as demonstrated in Fig. 3. In contrast, the multiparametric patient stratification led to a highly improved prognostic value of RhoA patterns and, consequently, their potential clinical utility.
When stratified by the MMP-9 activity levels, a statistically significant difference for both “single-band” and “double-band” images is demonstrated between benign and malignant premenopausal women: high MMP-9 activity and significantly increased RhoA expression levels is characteristic for breast malignancy in early age that fully confirms the main hypothesis of this paper regarding the concerted RhoA/MMP-9 pathway activation as the multiparametric risk factor justified in the “Introduction” (Cáceres et al. 2005; Fagan-Solis et al. 2013; Sun et al. 2016). Indeed, this result corresponds well with the clinical observations and further data obtained in this study, which demonstrate the highest rates of RhoA in the “premenopausal” malignancies stratified by high MMP-9 activities: breast cancer manifested in young (premenopausal) women frequently corresponds with the most aggressive tumour sub-types with worse outcomes compared to other sub-groups.
Obvious limitation of the stratification system presented in the current study
Current multiparametric stratification approach does not consider the patient category of the premenopausal malignancies with low level of both MMP-9 activities and RhoA expressions. Obviously this type of breast cancer malignancies is conditioned by molecular mechanisms which differ from these of the concerted RhoA/MMP-9 pathway activation.
Discussion
Frequent metastatic dissemination is the main cause of breast cancer-related morbidity. Keeping in mind extremely high level of the disease heterogeneity, potential predictors of particularly aggressive sub-types of BC and metastatic disease are of great clinical utility to discriminate between high and low-risk individuals, therefore, avoiding overtreatments in low-risk sub-groups but selecting the high-risk individuals for early and preventive treatment modalities. Therefore, potent targets are of great importance to accurately stratify the patients and to tailor the treatments individually at molecular level. Accumulating research data demonstrates RhoA to be one of the biomarkers for identifying and treating actively metastasing tumours (Gou et al. 2011; Sayagués et al. 2016). Hence, there is a positive correlation between the level of RhoA expression and corresponding morphological stage of metastatic proliferation in the liver (Gou et al. 2011), which is one of the most frequent metastatic sites of the aggressive BC (Abraham and Golubnitschaja 2016; Golubnitschaja and Sridhar 2016). Further, a suppression of RhoA inhibits cancer cell growth and their migration capacity (Gou et al. 2011). On the other hand, an ideal biomarker does not exist: an optimal biomarker panel allows for much more precise patient stratification in breast cancer as it is well justified in the literature now (Girotra et al. 2016). Contextually, our project was focused on improved patient stratification and increased predictive power by a multiparametric diagnostics. A significant innovation and advantage of the proposed approach is its non-invasive and predictive character, since the biomarker panel utilises molecular profiling of peripheral leucocytes which is disease-specific but might be measurable in blood before clinical onset of the pathology (visible breast tissue alterations) as published by us earlier (Debald et al. 2013).
The attributes of the tumour invasion are cancer cell adhesion to the ECM, proteolytic degradation of the surrounding tissue and migration of the tumour cells. The potential and extent of the tumour invasion condition the aggressiveness of the cancer disease. During tumour invasion, the activated MMPs perform the ECM degradation (Ranuncolo et al. 2003; Talvensaari-Mattila et al. 2003; Leppä et al. 2004), while the tumour cell migration is operated by the protein-complex of the small GTPase RhoA (Narumiya et al. 2009; Friedl and Wolf 2010; Sanz-Moreno and Marshall 2010; Carr et al. 2013). Consequently, RhoA/MMPs pathway activation is considered as the key mechanism in development of both BC and BCMD (Cáceres et al. 2005; Fagan-Solis et al. 2013; Sun et al. 2016) being associated with poor prognosis in the breast cancer patients effected by the concerted RhoA/MMPs activation.
Considering the core of MMPs, our particular attention was attracted by MMP-9 (gelatinase B), the increased activities of which, on the one side, are associated with particularly poor prognosis in BC and BCMD (Ranuncolo et al. 2003). On the other side, MMP-9 regulation is dependent on the level of NO· (nitric oxide) which plays an important (both pro-metastatic and anti-metastatic) role in nearly all steps of cancer development and metastastatic disease progression, depending on specific factors and tumour progression (Cheng et al. 2014). Further, anti-metastatic NO· regulation and potential nitric oxide therapy is possible at very early stages of the tumour progression and potentially in BC-predisposed individuals before the clinical manifestation of the disease, such as improvement of microcirculation and minimisation of harmful effects of a hypoxic condition. In this context, our above described stratification system might be particularly useful for early and predictive BC diagnostics applied to certain phenotypes in the population such as
-
premenopausal rather than postmenopausal women for predicting and preventing BC and its particularly aggressive sub-types,
-
(rather young) women with dense breast tissue, where—depending on the tissue density—highly increased RhoA/MMPs activities are utilised for effective proteolysis of the matrix and cancer cell migration into dense matrices (Raviraj et al. 2012).
-
BC of unclear origin such as hormone-receptor independent particularly aggressive triple-negative sub-type (Covington et al. 2013; Cox et al. 2015).
-
BRCA1/2 carriers predisposed to breast cancer malignancies, who might, particularly, benefit from the proposed stratification system as an independent biomarker panel.
-
hypoxia-stimulated BC and metastatic diseases (Muñoz-Nájar et al. 2006; Cox et al. 2015).
-
potential formation of pre-metastatic niches (Golubnitschaja et al. 2016a).
-
disturbed but restorable microcirculation, e.g., in individuals with “Flammer syndrome” (Konieczka et al. 2014).
The estimated level of the potential clinical utility of here presented results is very high. The proposed stratification system is conform with the field requirements as considered in our previous publications (Braun et al. 2009; Debald et al. 2013; Golubnitschaja et al. 2013). Further, the proposed stratification system might be cost-effective, if used additionally to UPA/PAI-1 biomarker-combination. Urokinase plasminogen activator (UPA) is an extracellular matrix-degrading protease involved in cancer invasion and metastasis, interacting with plasminogen activator inhibitor-1 (PAI-1)—together are well established biomarker-set stratifying lymph node-negative breast cancer patients for adjuvant chemotherapy (Jacobs et al. 2013; Duffy et al. 2014). However, neither individually nor in the combination UPA/PAI-1 cannot be considered as a reliable predictor avoiding sentinel lymph node biopsy, e.g., in case of a negative result by testing UPA and PAI-1 (Harms et al. 2014).
Conclusions and expert recommendations
-
Our results demonstrate the relevance of the two biomarkers measured in blood serum and peripheral leucocytes that is conform to the previously published considerations of BC as a systemic disease. This conclusion empowers much broader application of non-invasive approaches utilising blood biomarkers for risk assessment, prediction and prognosis in overall breast cancer management avoiding technical, analytical, ethical and economical problems linked to the breast tissue analysis.
-
RhoA used as alone biomarker might act as an indicator, however, does not provide information strong enough to ascertain BC risk and follow-up prognosis. Hence, we have demonstrated that relatively high expression rates of RhoA measured in postmenopausal women with breast benignancies which, however, are not accompanied by increased MMP-9 activities in blood serum cannot be considered as a risk factor for BC development.
-
MMP-9 is a multifunctional player with both physiologic and pathologic roles in local and systemic events. Therefore, similar to the RhoA, when used alone, this biomarker may provide solely indirect indications towards BC-related processes, however, cannot be considered as an independent predictive or prognostic biomarker.
-
In contrast, when RhoA expression rates in circulating leucocytes become stratified by corresponding MMP-9 activities in blood serum, the comprehensive mechanisms towards BC are evaluated more completely, consequently providing more precise pathology-related indication increasing, therefore the predictive power of biomarker specifically for BC. To this end, for premenopausal women with benignancies demonstrating both biomarkers increased a regular check-up is recommended, due to an evident risk of BC development.
-
Extremely high rates monitored for both MMP-9 blood serum activity and RhoA expression rates in circulating leucocytes in premenopausal women correlate well with highly aggressive BC malignancies reported specifically for this cohort of BC-patients and provide more precise insights into molecular mechanisms underlying the aggressive malignancies.
-
The above justified biomarker-combination is, further, recommended for an advanced population screening as an effective and cheap non-invasive approach to facilitate BC risk assessment, targeted prediction and corresponding preventive measures at the level of BC predisposition, pre-lesions and early stages, when the pathology can be effectively prevented or cured.
-
Obvious limitation of the stratification system presented in the current study: the multiparametric stratification approach does not consider the patient category of the premenopausal malignancies with low level of both MMP-9 activities and RhoA expressions. Obviously this type of breast cancer malignancies is conditioned by molecular mechanisms which differ from these of the concerted RhoA/MMP-9 pathway activation.
-
Because of the multifactorial origin and heterogeneity of invasive breast cancer, a more detailed examination of the type/origin/grade of cancer may, further, lead to better patient stratification and improved pathology-specific biomarker patterns. Proposed stratification system requires a systematic validation based on a statistically significant number of cases per patient sub-groups nominated above.
References
Abraham J-A, Golubnitschaja O (2016) Time for paradigm change in management of hepatocellular carcinoma: is an personalized approach on the horizon? Pers Med 13:455–467. doi:10.2217/pme-2016-0013
Bhandary L, Whipple RA, Vitolo MI et al (2015) ROCK inhibition promotes microtentacles that enhance reattachment of breast cancer cells. Oncotarget 6:6251–6266. doi:10.18632/oncotarget.3360
Braun M, Fountoulakis M, Papadopoulou A et al (2009) Down-regulation of microfilamental network-associated proteins in leukocytes of breast cancer patients: potential application to predictive diagnosis. Cancer Genom Proteom 6:31–40
Cáceres M, Guerrero J, Martínez J (2005) Overexpression of RhoA-GTP induces activation of the epidermal growth factor receptor, dephosphorylation of focal adhesion kinase and increased motility in breast cancer cells. Exp Cell Res 309:229–238. doi:10.1016/j.yexcr.2005.05.020
Camara O, Kavallaris A, Nöschel H et al (2006) Seeding of epithelial cells into circulation during surgery for breast cancer: the fate of malignant and benign mobilized cells. World J Surg Oncol 4:67. doi:10.1186/1477-7819-4-67
Carr HS, Zuo Y, Oh W, Frost JA (2013) Regulation of focal adhesion kinase activation, breast cancer cell motility, and amoeboid invasion by the RhoA guanine nucleotide exchange factor Net1. Mol Cell Biol 33:2773–2786. doi:10.1128/MCB.00175-13
Chang Y-WE, Marlin JW, Chance TW, Jakobi R (2006) RhoA mediates cyclooxygenase-2 signaling to disrupt the formation of adherens junctions and increase cell motility. Cancer Res 66:11700–11708. doi:10.1158/0008-5472.CAN-06-1818
Cheng H, Wang L, Mollica M et al (2014) Nitric oxide in cancer metastasis. Cancer Lett 353:1–7. doi:10.1016/j.canlet.2014.07.014
Covington KR, Brusco L, Barone I et al (2013) Metastasis tumor-associated protein 2 enhances metastatic behavior and is associated with poor outcomes in estrogen receptor-negative breast cancer. Breast Cancer Res Treat 141:375–384. doi:10.1007/s10549-013-2709-5
Cox TR, Rumney RMH, Schoof EM et al (2015) The hypoxic cancer secretome induces pre-metastatic bone lesions through lysyl oxidase. Nature 522:106–110. doi:10.1038/nature14492
Debald M, Yeghiazaryan K, Cebioglu M et al (2013) “Suspect molecular signature” in blood as the indicator of undiagnosed breast cancer, cancer risk and targeted prevention. EPMA J 4:22. doi:10.1186/1878-5085-4-22
Duffy MJ, McGowan PM, Harbeck N et al (2014) uPA and PAI-1 as biomarkers in breast cancer: validated for clinical use in level-of-evidence-1 studies. Breast Cancer Res 16:428. doi:10.1186/s13058-014-0428-4
Egeblad M, Werb Z (2002) New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer 2:161–174. doi:10.1038/nrc745
Fagan-Solis KD, Schneider SS, Pentecost BT et al (2013) The RhoA pathway mediates MMP-2 and MMP-9-independent invasive behavior in a triple-negative breast cancer cell line. J Cell Biochem 114:1385–1394. doi:10.1002/jcb.24480
Friedl P, Wolf K (2010) Plasticity of cell migration: a multiscale tuning model. J Cell Biol 188:11–19. doi:10.1083/jcb.200909003
Fritz G, Just I, Kaina B (1999) Rho GTPases are over-expressed in human tumors. Int J Cancer 81:682–687
Girotra S, Yeghiazaryan K, Golubnitschaja O (2016) Potential biomarker panels in overall breast cancer management: advancements by multilevel diagnostics. Pers Med 13:469–484. doi:10.2217/pme-2016-0020
Goldfarb Y, Ben-Eliyahu S (2006) Surgery as a risk factor for breast cancer recurrence and metastasis: mediating mechanisms and clinical prophylactic approaches. Breast Dis 26:99–114
Golubnitschaja O, Sridhar KC (2016) Liver metastatic disease: new concepts and biomarker panels to improve individual outcomes. Clin Exp Metastasis. doi:10.1007/s10585-016-9816-8
Golubnitschaja O, Yeghiazaryan K, Costigliola V et al (2013) Risk assessment, disease prevention and personalised treatments in breast cancer: is clinically qualified integrative approach in the horizon? EPMA J 4:6. doi:10.1186/1878-5085-4-6
Golubnitschaja O, Debald M, Kuhn W et al (2016a) Flammer syndrome and potential formation of pre-metastatic niches: a multi-centred study on phenotyping, patient stratification, prediction and potential prevention of aggressive breast cancer and metastatic disease. EPMA J 7(Suppl 1):A25. doi:10.1186/s13167-016-0054-6
Golubnitschaja O, Debald M, Yeghiazaryan K et al (2016b) Breast cancer epidemic in the early twenty-first century: evaluation of risk factors, cumulative questionnaires and recommendations for preventive measures. Tumour Biol. doi:10.1007/s13277-016-5168-x
Golubnitschaja O, Yeghiazaryan K, Stricker H et al (2016c) Patients with hepatic breast cancer metastases demonstrate highly specific profiles of matrix metalloproteinases MMP-2 and MMP-9 after SIRT treatment as compared to other primary and secondary liver tumours. BMC Cancer 16:357. doi:10.1186/s12885-016-2382-2
Golubnitschaja-Labudova O, Liu R, Decker C et al (2000) Altered gene expression in lymphocytes of patients with normal-tension glaucoma. Curr Eye Res 21:867–876
Gou L, Wang W, Tong A et al (2011) Proteomic identification of RhoA as a potential biomarker for proliferation and metastasis in hepatocellular carcinoma. J Mol Med 89:817–827. doi:10.1007/s00109-011-0753-3
Harms W, Malter W, Krämer S et al (2014) Clinical significance of urokinase-type plasminogen activator (uPA) and its type-1 inhibitor (PAI-1) for metastatic sentinel lymph node involvement in breast cancer. Anticancer Res 34:4457–4462
Jacobs VR, Kates RE, Kantelhardt E et al (2013) Health economic impact of risk group selection according to ASCO-recommended biomarkers uPA/PAI-1 in node-negative primary breast cancer. Breast Cancer Res Treat 138:839–850. doi:10.1007/s10549-013-2496-z
Konieczka K, Ritch R, Traverso CE et al (2014) Flammer syndrome. EPMA J 5:11. doi:10.1186/1878-5085-5-11
Leppä S, Saarto T, Vehmanen L et al (2004) A high serum matrix metalloproteinase-2 level is associated with an adverse prognosis in node-positive breast carcinoma. Clin Cancer Res 10:1057–1063
Marino N, Woditschka S, Reed LT et al (2013) Breast cancer metastasis: issues for the personalization of its prevention and treatment. Am J Pathol 183:1084–1095. doi:10.1016/j.ajpath.2013.06.012
Mehner C, Hockla A, Miller E et al (2014) Tumor cell-produced matrix metalloproteinase 9 (MMP-9) drives malignant progression and metastasis of basal-like triple negative breast cancer. Oncotarget 5:2736–2749. doi:10.18632/oncotarget.1932
Muñoz-Nájar UM, Neurath KM, Vumbaca F, Claffey KP (2006) Hypoxia stimulates breast carcinoma cell invasion through MT1-MMP and MMP-2 activation. Oncogene 25:2379–2392. doi:10.1038/sj.onc.1209273
Narumiya S, Tanji M, Ishizaki T (2009) Rho signaling, ROCK and mDia1, in transformation, metastasis and invasion. Cancer Metastasis Rev 28:65–76. doi:10.1007/s10555-008-9170-7
Provatopoulou X, Gounaris A, Kalogera E et al (2009) Circulating levels of matrix metalloproteinase-9 (MMP-9), neutrophil gelatinase-associated lipocalin (NGAL) and their complex MMP-9/NGAL in breast cancer disease. BMC Cancer 9:390. doi:10.1186/1471-2407-9-390
Ranuncolo SM, Armanasco E, Cresta C et al (2003) Plasma MMP-9 (92 kDa-MMP) activity is useful in the follow-up and in the assessment of prognosis in breast cancer patients. Int J Cancer 106:745–751. doi:10.1002/ijc.11288
Raviraj V, Fok S, Zhao J et al (2012) Regulation of ROCK1 via Notch1 during breast cancer cell migration into dense matrices. BMC Cell Biol 13:12. doi:10.1186/1471-2121-13-12
Sanz-Moreno V, Marshall CJ (2010) The plasticity of cytoskeletal dynamics underlying neoplastic cell migration. Curr Opin Cell Biol 22:690–696. doi:10.1016/j.ceb.2010.08.020
Sayagués JM, Corchete LA, Gutiérrez ML et al (2016) Genomic characterization of liver metastases from colorectal cancer patients. Oncotarget. doi:10.18632/oncotarget.12140
Sun K, Duan X, Cai H et al (2016) Curcumin inhibits LPA-induced invasion by attenuating RhoA/ROCK/MMPs pathway in MCF7 breast cancer cells. Clin Exp Med 16:37–47. doi:10.1007/s10238-015-0336-7
Sung H, Choi J-Y, Lee S-A et al (2012) The association between the preoperative serum levels of lipocalin-2 and matrix metalloproteinase-9 (MMP-9) and prognosis of breast cancer. BMC Cancer 12:193. doi:10.1186/1471-2407-12-193
Tabariès S, Ouellet V, Hsu BE et al (2015) Granulocytic immune infiltrates are essential for the efficient formation of breast cancer liver metastases. Breast Cancer Res 17:45. doi:10.1186/s13058-015-0558-3
Talvensaari-Mattila A, Pääkkö P, Turpeenniemi-Hujanen T (2003) Matrix metalloproteinase-2 (MMP-2) is associated with survival in breast carcinoma. Br J Cancer 89:1270–1275. doi:10.1038/sj.bjc.6601238
WHO (2012) WHO|cancer. In: WHO. http://www.who.int/mediacentre/factsheets/fs297/en/. Accessed 15 Jun 2016
Acknowledgements
The authors thank the European Association for Predictive, Preventive and Personalised Medicine (EPMA, Belgium) for professional and financial support of the project. Further, our cordial thanks belong to Prof. Dr. J. Flammer, University of Basel, Switzerland for professional considerations of potential implementing areas for the stratification system published here and critical reading of the manuscript. For the performance of “Western-blot” analysis, the authors thank Mrs. G. Windisch-Schuster, Department of Radiology, University of Bonn.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
This article does not contain any studies with animals performed by any of the authors.
Funding
The study funding has been performed by the Breast Cancer Research Centre, University of Bonn, Bonn, Germany. KY has been awarded with corresponding fellowship by the European Association for Predictive, Preventive and Personalised Medicine (EPMA, Belgium).
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Handling Editor: G. J. Peters.
Rights and permissions
About this article
Cite this article
Golubnitschaja, O., Yeghiazaryan, K., Abraham, JA. et al. Breast cancer risk assessment: a non-invasive multiparametric approach to stratify patients by MMP-9 serum activity and RhoA expression patterns in circulating leucocytes. Amino Acids 49, 273–281 (2017). https://doi.org/10.1007/s00726-016-2357-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-016-2357-2