Abstract
It is well known that the endothelium maintains the vascular homeostasis. Importantly, endothelial dysfunction is regarded as a key early step in the development of atherosclerosis. Back in the early 1990s, it was found that asymmetric dimethylarginine (ADMA), an arginine metabolite derived from l-arginine (Arg) residues in proteins by asymmetric dimethylation on its guanidine group, is an endogenous inhibitor of nitric oxide (NO) synthase (NOS) isoforms. Inhibition of NO synthesis from Arg by the endothelial NOS isoform (eNOS) leads to endothelial dysfunction. Due to this action, ADMA participates in the pathophysiology of atherosclerosis and potentially contributes to cardiovascular events. Nowadays, homoarginine (hArg) is considered as a new key player in atherogenesis. hArg is a non-essential, non-proteinogenic amino acid which is synthesized from Arg by arginine:glycine amidinotransferase (AGAT). hArg is structurally related to Arg; formally, hArg is by one methylene (CH2) group longer than Arg, and may serve as a substrate for NOS, thus contributing to NO synthesis. For several decades, the pathophysiological role of hArg has been entirely unknown. hArg has been in the shadow of ADMA. Clinical studies have sought to investigate the relationship between circulating hArg levels and human disease states as well as cardiovascular prognosis. Recent studies indicate that hArg is actively involved in the vascular homeostasis, yet the underlying mechanisms are incompletely understood. In this article, we review the available literature regarding the role of ADMA and hArg in endothelial dysfunction and in cardiovascular disease as well as the possible associations between these endogenous Arg derivatives.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Worldwide, the number of deaths from cardiovascular disease (CVD) has been increasing alarmingly, mainly due to atherosclerosis, which is a chronic disease affecting the entire arterial tree, representing an inflammatory response in the vessels (Ross et al. 1999; Tousoulis et al. 2011b).
Endothelium is of major importance in the vasculature, as it is involved in promoting and maintaining a protective environment via endothelial cell-derived vasoactive factors. Nitric oxide (NO) and reactive oxygen species (ROS) such as superoxide represent key factors of vascular homeostasis (Guzik et al. 2004). Endothelial dysfunction, widely accepted as the imbalance between NO and ROS production, is currently regarded as an important early event in the development of atherosclerosis (Tousoulis et al. 2010).
In 1992, it was reported that asymmetric dimethylarginine (ADMA) is a naturally occurring endogenous inhibitor of NO synthase (NOS) (Vallance et al. 1992). ADMA inhibits vascular NO production at concentrations found in pathophysiological conditions, and also causes local vasoconstriction when infused intra-arterially (Böger et al. 2003, 2005; Lenzen et al. 2006). Consequently, ADMA reduces NO production and consequently can thus lead to endothelial dysfunction and participate in the pathophysiology of atherosclerosis and cardiovascular events. Therefore, circulating ADMA has emerged as a possible cardiovascular risk marker (Miyazaki et al. 1999; Lu et al. 2003a).
Homoarginine (hArg), on the other hand, is endogenously produced from l-arginine (Arg) and is structurally closely related to its precursor Arg. Formally, hArg has an additional methylene group (CH2) in its molecule. Because of the involvement of other arginine metabolites in vascular homeostasis, the structural similarity has recently stimulated experimental and clinical studies aimed to explore the relationship between plasma hArg levels and human disease states as well as cardiovascular prognosis (Huynh and Chin-Dusting 2006; Atzler et al. 2013). In the present article we review the existing literature on the role of ADMA and hArg and their possible interrelationship in endothelial dysfunction and cardiovascular disease.
Homoarginine–biosynthesis and metabolism
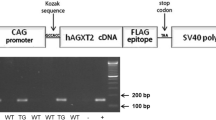
hArg (l-homoarginine) is a non-proteinogenic amino acid. It is formed from lysine during reactions similar to those of the urea cycle. Similar to urea cycle, ornithine is replaced by lysine and ornithine-transcarbamoylase, which is regarded as the main enzyme responsible for hArg synthesis. Even though ornithine-transcarbamoylase has a higher affinity to ornithine, it also catalyzes the transaminidation reaction of lysine, a key step to hArg’s production (Davids et al. 2012). Another pathway for its production includes arginine:glycine amidinotransferase (AGAT), an enzyme which catalyzes the transfer of an amidino group from Arg to glycine, resulting in formation of guanidinoacetate, which is methylated by guanidinoacetate methyltransferase (GAMT) to form creatine (Davids et al. 2012). AGAT may use lysine instead of glycine, thus resulting in the production of hArg. Evidence for in vivo synthesis of hArg from lysine had been previously first reported in experimental models. In humans, an increase in urinary hArg after oral lysine administration had been demonstrated in adults (Davids et al. 2012). The metabolic routes responsible for hArg synthesis from lysine in vivo have not yet been unraveled completely.
Production of NO by the vascular endothelium is of crucial importance in the maintenance of vascular tone, an important determinant of blood pressure. Unlike the methylated arginine metabolites including ADMA, which are inhibitors of NOS (Tsikas et al. 2000a; Tsikas and Kayacelebi 2014; Kielstein et al. 2007), hArg can serve as an NOS substrate. hArg can also serve as substrate for arginase. hArg could thus lead to an increased availability of Arg for NOS to produce NO (Michel 2013). The ability of hArg to modulate NO bioavailability in the presence of about 20- to 40-fold higher Arg concentrations appears to be intriguing.
Homoarginine, nitric oxide and endothelial dysfunction
As endothelium-derived NO is generally considered as a biologically beneficial molecule, it seems a plausible hypothesis that hArg may affect the cardiovascular system by either enhancing or limiting NO production. Moreover, vascular endothelium is a major regulator of vascular tone via manufacturing and balancing vasodilators and vasoconstrictors, including NO and prostacyclin, which have contributed to the understanding of the pathogenesis of atherosclerosis (Bonetti et al. 2003). Under basal conditions, and in response to mechanical and humoral stimuli, the endothelium manufactures a large variety of vasoactive molecules in order to maintain normal vascular tone and blood fluidity. Endothelial dysfunction emerges as a result of an imbalance among those factors (Tousoulis et al. 2015).
Assuming an effect of hArg on NO bioavailability and, consequently, early atherogenesis, an association of hArg with endothelial function and vascular disease may be hypothesized. Specifically, transient elevations of hArg were correlated with brachial artery diameter and flow-mediated dilatation (FMD) during the second and third trimesters of pregnancy (Valtonen et al. 2008; Saarelainen et al. 2008). Moreover, according to a recent population-based cohort study of 746 elderly participants, plasma levels of hArg and Arg are independently associated with clinically relevant differences in blood pressure in an antagonistic fashion (van der Zwan et al. 2013). Accordingly, in a large study of patients with preserved left ventricular ejection fraction, higher levels of ADMA, symmetric dimethylarginine (SDMA) and lower levels of hArg were associated with diastolic dysfunction and negatively associated with N-terminal pro-B-type natriuretic peptide and mid-regional pro-adrenomedullin (Pilz et al. 2014). Of note, evidence suggests that long-term Arg supplementation may have harmful effects, raising concerns about long-term consequences of hArg supplementation, even though beneficial effects of short-term hArg supplementation in mouse stroke models have been reported recently (Choe et al. 2013). Significant decreases in hArg were recognized in plasma from AGATnull mice, associated with significant increases in the size of stroke (Choe et al. 2013).
It is also worth mentioning that in 3041 patients of the Ludwigshafen Risk and Cardiovascular Health (LURIC) Study referred for coronary angiography and 2102 participants of the Young Finns Study (YFS), a genome-wide association study was performed to identify genomic loci associated with hArg serum levels and tested for associations of identified single nucleotide polymorphisms with mortality in LURIC. Notably, 3 chromosomal regions were identified which were significantly associated with serum hArg, providing novel insights into the biological background of hArg (Kleber et al. 2013).
Homoarginine and cardiovascular disease
Further to this evidence, significant studies have recently investigated a possible role of hArg as a risk factor for vascular disease. A recent prospective study of male patients with intermittent claudication and age- and diabetes-matched controls showed an association of hArg and Arg with peripheral arterial disease (Vogl et al. 2015). In 3514 participants of the Dallas Heart Study, hArg was also inversely and independently associated with aortic wall thickness but not with aortic plaque burden and coronary artery calcium (Atzler et al. 2014). Furthermore, serum hArg was measured in 3305 participants of the LURIC Study, who were referred to coronary angiography at baseline and were followed-up for 9.9 years (Pilz et al. 2011b). It was shown in this study that hArg levels are a novel risk factor for fatal strokes. Interestingly, however, in healthy children and adolescents aged 3–18 years without coexistent diseases, hArg appears to be unrelated with intima-media thickness (IMT) and extra-medial thickness (EMT) of common carotid arteries estimated by B-mode ultrasound (Jazwinska-Kozuba et al. 2013). Regarding vascular disease, underlying mechanisms remain still not fully elucidated but there is accumulating evidence that hArg, apart from its role in NO metabolism, may affect other risk factors such as diabetes mellitus, arterial hypertension, or prothrombotic states (Radomski et al. 1990; Chen and Sanders 1993; März et al. 2010).
Low serum hArg has recently emerged as a potential new risk marker for cardiovascular mortality in several populations (Table 1). More specifically, in a large cohort, hemodialysed patients had lower mean hArg levels and experienced a fivefold increased mortality rate compared with LURIC patients (608 deaths during a median follow-up of 4 years) (Pilz et al. 2011b). It consistently affected mortality, in a second high-risk cohort of 1244 patients with type 2 diabetes mellitus receiving maintenance hemodialysis (4D study). Patients in the lowest quartile (<0.87 µM) had a twofold higher than in patients in the highest quartile (März et al. 2010). Furthermore, in the CAVASIC Study (Vogl et al. 2015) hArg was related to all-cause mortality implying a broader role in metabolic processes besides endothelial function. Accordingly, in 3514 participants of the Dallas Heart Study followed-up for 9.4 years, higher hArg was associated with lower rate of major adverse cardiovascular events (hazard ratio, 0.86; 95 % confidence interval, 0.75–0.98) and lower all-cause mortality (hazard ratio, 0.82; 0.73–0.92; per 1 log SD increase in hArg) (Atzler et al. 2014). In addition, in a prospective study of 3305 Caucasian patients who were referred for coronary angiography, multivariable adjusted hazard ratios (with 95 % CI) for the first versus the fourth hArg quartile were 2.44 (1.60–3.73) for sudden cardiac deaths, 3.44 (1.89–6.24) for heart failure deaths, and 3.78 (1.77–8.06) for fatal myocardial infarctions (Pilz et al. 2011a). Interestingly, increasing hArg levels were independently associated with a reduction in all-cause mortality in patients with ischemic stroke followed-up for 7.4 years; hazard ratio for 1-SD hArg, 0.79 P = 0.019). hArg was also independently associated with the National Institutes of Health Stroke Scale score and 30-day mortality after ischemic stroke (P < 0.05) (Choe et al. 2013). Also, according to the Mild to Moderate Kidney Disease (MMKD) Study, a prospective cohort study of 227 patients with chronic kidney disease in Europe. It was found that hArg concentrations were directly correlated with kidney function and were significantly associated with the progression of chronic kidney disease. This study provided evidence that low hArg concentrations might be an early indicator of kidney failure and a potential target for the prevention of disease progression (Drechsler et al. 2013). Furthermore, recent data have also indicate that plasma hArg concentrations are reduced in Takotsubo cardiomyopathy patients compared to healthy subjects, while 3-nitrotyrosine plasma concentrations, a biomarker of NO-related oxidative stress, were similar in Takotsubo cardiomyopathy patients and in healthy controls (Kayacelebi et al. 2014a).
Asymmetric dimethylarginine: biosynthesis and metabolism
ADMA biosynthesis has its basis on a post-translational modification of arginine remnants. A group of enzymes called protein arginine N-methyl transferases (PRMTs) are responsible for the catalysis of arginine remnants methylation (Tran et al. 2003). Both subtypes of PRMT, PRMT1 and PRMT2, are capable of promoting monomethylation of the guanidine group of arginine to form monomethyl arginine (MMA). More specifically, PRMT1 is involved in the generation of ADMA, while PRMT2 contributes to the formation of SDMA (Tran et al. 2003). In contrast to ADMA and MMA, SDMA is generally assumed not to inhibit NOS. However, at least for recombinant neuronal NOS (nNOS), SDMA was demonstrated to inhibit nNOS-catalyzed formation of NO from Arg (Tsikas et al. 2000b). Enhanced levels of ADMA result from increased arginine remnants methylation.
The major part of ADMA (up to 90 %) is mainly degraded via its hydrolysis to l-citrulline and dimethylamine by the enzyme dimethylarginine dimethylaminohydrolase (DDAH); the remaining fraction (up to 20 %) is excreted by urine (Achan et al. 2003; Kaito et al. 2005). There are two isoforms of DDAH: DDAH 1 which expresses neuronal (nNOS), and DDAH 2 expresses eNOS (Leiper et al. 1999). It has been proposed that the elevation in plasma ADMA that occurs with vascular disease and risk factors is largely due to impaired activity of DDAH (Ito et al. 1999). Of note, it has been suggested that the release of ADMA from endothelial cells is increased in the presence of native or oxidized low-density lipoprotein (LDL), possibly mediated by up-regulation of S-adenosylmethionine dependent methyl transferases. These findings suggest a novel mechanism by which ADMA concentration is elevated in hypercholesterolemia, leading to endothelial dysfunction and atherosclerosis (Böger et al. 2000). Moreover, significant evidence has indicated that the lung appears to be responsible for large amounts of protein bound ADMA, due to the high expression levels of various PRMTs in lung tissue (Bulau et al. 2007).
DDAH overexpression reduces ADMA levels and increases NO synthesis. Furthermore, it has been shown more ADMA is cleared by the liver due to the higher blood flow through the liver compared to the kidneys. Therefore, decline of organ function, by diminished clearance, may result in raised ADMA levels. In addition, increased ADMA levels may promote organ dysfunction.
Asymmetric dimethylarginine, nitric oxide and endothelial dysfunction
It is well established that NO is the main key player facilitating vascular homeostasis with established anti-atherogenic effects. It has been also shown that ADMA can reduce NO production/bioavailability by inhibiting eNOS activity. In end-stage renal failure patients, ADMA accumulates in the blood, however dialysis improves endothelial function by diminishing ADMA levels (Vallance et al. 1992). In addition, other studies have shown strong associations between risk factors for atherosclerosis and ADMA (Fig. 1). Thus, in patients with diabetes mellitus it has been found that ADMA can increase rapidly after acute administration of high-fat meal resulting to significantly impaired flow-mediated dilatation (FMD) (Fard et al. 2000). In hypertensives, plasma ADMA levels were increased after salt loading and decreased after salt restriction, while the change in plasma NO level was correlated inversely with those in blood pressure and plasma ADMA level after salt loading and restriction. Therefore, it can be speculated that salt intake may play a role in modulation of NO synthesis. This may suggest a mechanism for salt sensitivity in human hypertension, presumably via the change in ADMA (Fujiwara et al. 2000). Also in hypertensives, circulating ADMA concentration is elevated, but remains unchanged after methionine loading, suggesting that ADMA plays an important role in endothelial dysfunction in hypertensives, but it is not responsible for homocysteine-induced endothelial dysfunction in these patients (Tousoulis et al. 2011a). According to a case–control study of essential hypertensive patients, only ADMA and l-arginine were independent correlates, accounting for 33.9 % and 8.9 % of the variability in the peak forearm blood flow response to acetylcholine. Therefore, l-arginine and endogenous inhibitor of nitric oxide synthase, ADMA, was suggested to be inversely related to endothelial function in this population (Perticone et al. 2005). Furthermore, ADMA synthesis is activated in acute hyper-homocysteinemia by mechanisms independent of inflammation and oxidative stress (Antoniades et al. 2006).
In larger cohorts it was found an inverse association between ADMA and FMD, which remained even after adjustment for risk factors of atherosclerosis (Juonala et al. 2007). Further studies have demonstrated that ADMA can promote spasm of the coronary arteries (Hori et al. 2003), while it is raised in subjects with slow coronary flow (Selcuk et al. 2007). However, in a study of coronary artery disease (CAD) patients, there was no association between ADMA and endothelial function which is in disagreement to the previous findings (Maas et al. 2007). Notably, a recent cross-sectional study of 231 healthy male volunteers evaluated the effects of cigarette smoking on hArg and other biomarkers. In smokers, it was found that plasma hArg levels were 17 % lower compared with non-smokers after adjusting for age, body mass index, plasma creatinine, and metal blood levels while plasma ADMA levels were only 6 % higher in smokers when compared with the levels found in non-smokers. Therefore, in contrast to ADMA, there is a strong association between exposure to tobacco smoke and plasma hArg levels (Sobczak et al. 2014).
Asymmetric dimethylarginine and cardiovascular disease
Several studies have investigated the prognostic role of ADMA for cardiovascular disease (Table 2).
More specifically, in a large number of subjects without overt cerebro-cardiovascular diseases plasma level of ADMA was shown to be a strong and independent determinant of intima-media thickness (IMT) of the carotid artery (Furuki et al. 2007). ADMA is not only associated strongly with endothelial dysfunction, but also with the risk for CVD. Thus, circulating ADMA levels predicted cardiovascular events in patients undergoing haemodialysis (Zoccali et al. 2001). In a larger cohort including patients with and without CAD, subjects in the higher quartiles of ADMA had increased risk of death and all-cause mortality due to cardiovascular disorders. However, the predictive value of ADMA was not significant in the non-CAD subgroup (Valkonen et al. 2001). In a prospective cohort, baseline serum concentration of ADMA was assessed in 1874 consecutive patients with CAD. ADMA levels in patients who subsequently experienced the primary endpoint (death/fatal MI) were significantly higher than in patients who did not reach the primary end-point during a mean follow-up of 2.6 ± 1.2 years (Schnabel et al. 2005). In addition, it has been shown (Leong et al. 2008) that increased ADMA levels in healthy women is associated with 30 % increase risk for CVD. In this study, ADMA levels increased the risk for CVD beyond the known Framingham risk score. Moreover, in patients with acute coronary syndrome, increased levels of ADMA represent a strong and independent predictor of myocardial infarction and all-cause mortality (Cavusoglu et al. 2009). Further to that patients with unstable angina and decreased ADMA levels 6 weeks post percutaneous coronary intervention (PCI) had less recurrent cardiovascular events compared to subjects with raised ADMA levels (Krempl et al. 2005). In the context of PCI, in another study it was found that although ADMA levels did not correlate with negative coronary remodeling, treatment with sirolimus was associated with lower ADMA levels and less intima hyperplasia compared to mycophenolate mofetil (Potena et al. 2008). Furthermore, in patients with peripheral arterial disease (PAD), ADMA predicted major adverse cardiovascular events (MACE) occurrence (Mittermayer et al. 2006). More specifically patients in the highest quartile exhibited 39 % MACE occurrence. Finally, in a prospective study of type 2 diabetes mellitus patients, the highest quartiles of ADMA were associated with increased hazard ratios for cardiovascular events incidence (Krzyzanowska et al. 2007).
Conclusions
It has become evident that ADMA and hArg play a significant role in endothelial dysfunction, which is likely mediated by their effects on NO synthesis/bioavailability. ADMA is an endogenous inhibitor of eNOS activity. By this action, ADMA inhibits vascular NO production, thus leading to endothelial dysfunction and contributing to atherogenesis. hArg has been in the shadow of ADMA until recently, but it is now emerging as a new key player in the cardiovascular field. Yet, the underlying mechanisms remain still unrevealed. NO-related actions of hArg are possible as hArg may serve as substrate both for eNOS and arginase that may control the concentration of Arg, the substrate of eNOS. Both ADMA and hArg participate in and contribute actively not only to atherogenesis, but also to cardiovascular disease with a possible predictive role. More specifically, circulating hArg and ADMA levels seem to be independently associated with cardiovascular risk, death and major adverse cardiovascular events. Although they are promising molecules, there are not enough data to support their predictive role and use in clinical practice. Therefore, more studies are needed to elucidate the underlying pathophysiological mechanisms and pathways involved in synthesis and metabolism of these molecules. In addition, large-scale studies are required to evaluate the predictive role of ADMA and hArg in cardiovascular disease.
Abbreviations
- ADMA:
-
Asymmetric dimethylarginine
- AGAT:
-
Arginineglycine amidinotransferase
- CAD:
-
Coronary artery disease
- CVD:
-
Cardiovascular disease
- DDAH:
-
Dimethylarginine dimethylaminohydrolase
- FMD:
-
Flow-mediated dilatation
- GAMT:
-
Guanidinoacetate methyltransferase
- hArg:
-
Homoarginine
- IMT:
-
Intima-media thickness
- MMA:
-
Monomethylarginine
- NO:
-
Nitric oxide
- NOS:
-
NO synthase
- eNOS:
-
Endothelial nitric oxide synthase
- nNOS:
-
Neuronal nitric oxide synthase
- PCI:
-
Percutaneous coronary intervention
- PRMTs:
-
Protein arginine N-methyltransferases
- ROS:
-
Reactive oxygen species
- SDMA:
-
Symmetric dimethylarginine
References
Achan V, Broadhead M, Malaki M et al (2003) Asymmetric dimethylarginine causes hypertension and cardiac dysfunction in humans and is actively metabolized by dimethylarginine dimethylaminohydrolase. Arterioscler Thromb Vasc Biol 23:1455–1459
Antoniades C, Tousoulis D, Marinou K et al (2006) Asymmetrical dimethylarginine regulates endothelial function in methionine-induced but not in chronic homocystinemia in humans: effect of oxidative stress and proinflammatory cytokines. Am J Clin Nutr 84:781–788
Atzler D, Rosenberg M, Anderssohn M et al (2013) Homoarginine–an independent marker of mortality in heart failure. Int J Cardiol 168:4907–4909
Atzler D, Gore MO, Ayers CR et al (2014) Homoarginine and cardiovascular outcome in the population-based Dallas Heart Study. Arterioscler Thromb Vasc Biol 34:2501–2507
Böger RH (2003) The emerging role of asymmetric dimethylarginine as a novel cardiovascular risk factor. Cardiovasc Res 59:824–833
Böger RH (2005) Asymmetric dimethylarginine (ADMA) and cardiovascular disease: insights from prospective clinical trials. Vasc Med 10(Suppl 1):S19–S25
Böger RH, Sydow K, Borlak J et al (2000) LDL cholesterol upregulates synthesis of asymmetrical dimethylarginine in human endothelial cells: involvement of S-adenosylmethionine-dependent methyltransferases. Circ Res 87:99–105
Bonetti PO, Lerman LO, Lerman A (2003) Endothelial dysfunction: a marker of atherosclerotic risk. Arterioscler Thromb Vasc Biol 23:168–175
Bulau P, Zakrzewicz D, Kitowska K et al (2007) Analysis of methylarginine metabolism in the cardiovascular system identifies the lung as a major source of ADMA. Am J Physiol Lung Cell Mol Physiol 2007(292):L18–L24
Cavusoglu E, Ruwende C, Chopra V et al (2009) Relationship of baseline plasma ADMA levels to cardiovascular outcomes at 2 years in men with acute coronary syndrome referred for coronary angiography. Coron Artery Dis 20:112–117
Chen PY, Sanders PW (1993) Role of nitric oxide synthesis in salt-sensitive hypertension in Dahl/Rapp rats. Hypertension 22:812–818
Choe CU, Atzler D, Wild PS et al (2013) Homoarginine levels are regulated by l-arginine:glycine amidinotransferase and affect stroke outcome: results from human and murine studies. Circulation 128:1451–1461
Davids M, Ndika JD, Salomons GS, Blom HJ, Teerlink T (2012) Promiscuous activity of arginine:glycine amidinotransferase is responsible for the synthesis of the novel cardiovascular risk factor homoarginine. FEBS Lett 586:3653–3657
Drechsler C, Kollerits B, Meinitzer A et al (2013) Homoarginine and progression of chronic kidney disease: results from the Mild to Moderate Kidney Disease Study. PLoS One 8:e63560
Fard A, Tuck CH, Donis JA et al (2000) Acute elevations of plasma asymmetric dimethylarginine and impaired endothelial function in response to a high-fat meal in patients with type 2 diabetes. Arterioscler Thromb Vasc Biol 20:2039–2044
Fujiwara N, Osanai T, Kamada T et al (2000) Study on the relationship between plasma nitrite and nitrate level and salt sensitivity in human hypertension:modulation of nitric oxide synthesis by salt intake. Circulation 101:856–861
Furuki K, Adachi H, Matsuoka H et al (2007) Plasma levels of asymmetric dimethylarginine (ADMA) are related to intima-media thickness of the carotid artery: an epidemiological study. Atherosclerosis 191:206–210
Guzik TJ, Sadowski J, Kapelak B et al (2004) Systemic regulation of vascular NAD(P)H oxidase activity and nox isoform expression in human arteries and veins. Arterioscler Thromb Vasc Biol 24:1614–1620
Hori T, Matsubara T, Ishibashi T et al (2003) Significance of asymmetric dimethylarginine (ADMA) concentrations during coronary circulation in patients with vasospastic angina. Circ J 67:305–311
Huynh NN, Chin-Dusting J (2006) Amino acids, arginase and nitric oxide in vascular health. Clin Exp Pharmacol Physiol 33:1–8
Ito A, Tsao PS, Adimoolam S et al (1999) Novel mechanism for endothelial dysfunction: dysregulation of dimethylarginine dimethylaminohydrolase. Circulation 99:3092–3095
Jaźwińska-Kozuba A, Martens-Lobenhoffer J, Kruszelnicka O et al (2013) Opposite associations of plasma homoarginine and ornithine with arginine in healthy children and adolescents. Int J Mol Sci 14:21819–21832
Juonala M, Viikari JS, Alfthan G et al (2007) Brachial artery flowmediated dilation and asymmetrical dimethylarginine in the cardiovascular risk in young Finns study. Circulation 116:1367–1373
Kaito K, Otsubo H, Usui N et al (2005) Platelet size deviation width, platelet large cell ratio, and mean platelet volume have sufficient sensitivity and specificity in the diagnosis of immune thrombocytopenia. Br J Haematol 128:698–702
Kayacelebi AA, Pham VV, Willers J et al (2014a) Plasma homoarginine (hArg) and asymmetric dimethylarginine (ADMA) in patients with rheumatoid arthritis: is homoarginine a cardiovascular corrective in rheumatoid arthritis, an anti-ADMA? Int J Cardiol 176:1129–1131
Kayacelebi AA, Nguyen TH, Neil C, Horowitz JD, Jordan J, Tsikas D (2014b) Homoarginine and 3-nitrotyrosine in patients with Takotsubo cardiomyopathy. Int J Cardiol 173:546–547
Kielstein A, Tsikas D, Galloway GP, Mendelson JE (2007) Asymmetric dimethylarginine (ADMA)–a modulator of nociception in opiate tolerance and addiction? Nitric Oxide 17:55–59
Kleber ME, Seppälä I, Pilz S et al (2013) Genome-wide association study identifies 3 genomic loci significantly associated with serum levels of homoarginine: the Athero Remo Consortium. Circ Cardiovasc Genet 6:505–513
Krempl TK, Maas R, Sydow K, Meinertz T, Böger RH, Kahler J (2005) Elevation of asymmetric dimethylarginine in patients with unstable angina and recurrent cardiovascular events. Eur Heart J 26:1846–1851
Krzyzanowska K, Mittermayer F, Wolzt M, Schernthaner G (2007) Asymmetric dimethylarginine predicts cardiovascular events in patients with type 2 diabetes. Diabetes Care 30:1834–1839
Leiper JM, Santa Maria J, Chubb A et al (1999) Identification of two human dimethylarginine dimethylaminohydrolases with distinct tissue distributions and homology with microbial arginine deiminases. Biochem J 343:209–214
Lenzen H, Tsikas D, Böger RH (2006) Asymmetric dimethylarginine (ADMA) and the risk for coronary heart disease: the multicenter CARDIAC Study. Eur J Clin Pharmacol 62(Suppl 1):45–49
Leong T, Zylberstein D, Graham I et al (2008) Asymmetric dimethylarginine independently predicts fatal and nonfatal myocardial infarction and stroke in women: 24-year follow-up of the population study of women in Gothenburg. Arterioscler Thromb Vasc Biol 28:961–967
Lu TM, Ding YA, Lin SJ, Lee WS, Tai HC (2003a) Plasma levels of asymmetrical dimethylarginine and adverse cardiovascular events after percutaneous coronary intervention. Eur Heart J 24:1912–1919
Lu TM, Ding YA, Charng MJ, Lin SJ (2003b) Asymmetrical dimethylarginine: a novel risk factor for coronary artery disease. Clin Cardiol 26:458–464
Maas R, Quitzau K, Schwedhelm E et al (2007) Asymmetrical dimethylarginine (ADMA) and coronary endothelial function in patients with coronary artery disease and mild hypercholesterolemia. Atherosclerosis 191:211–219
März W, Meinitzer A, Drechsler C et al (2010) Homoarginine, cardiovascular risk, and mortality. Circulation 122:967–975
Meinitzer A, Seelhorst U, Wellnitz B et al (2007) Asymmetrical dimethylarginine independently predicts total and cardiovascular mortality in individuals with angiographic coronary artery disease (the Ludwigshafen Risk and Cardiovascular Health Study). Clin Chem 53:273–283
Michel T (2013) R is for arginine: metabolism of arginine takes off again, in new directions. Circulation 128:1400–1404
Mittermayer F, Krzyzanowska K, Exner M et al (2006) Asymmetric dimethylarginine predicts major adverse cardiovascular events in patients with advanced peripheral artery disease. Arterioscler Thromb Vasc Biol 26:2536–2540
Miyazaki H, Matsuoka H, Cooke JP et al (1999) Endogenous nitric oxide synthase inhibitor: a novel marker of atherosclerosis. Circulation 99:1141–1146
Nicholls SJ, Wang Z, Koeth R et al (2007) Metabolic profiling of arginine and nitric oxide pathways predicts hemodynamic abnormalities and mortality in patients with cardiogenic shock after acute myocardial infarction. Circulation 116:2315–2324
Perticone F, Sciacqua A, Maio R et al (2005) Asymmetric dimethylarginine, l-arginine, and endothelial dysfunction in essential hypertension. J Am Coll Cardiol 46:518–523
Pilz S, Meinitzer A, Tomaschitz A et al (2011a) Low homoarginine concentration is a novel risk factor for heart disease. Heart 97:1222–1227
Pilz S, Tomaschitz A, Meinitzer A et al (2011b) Low serum homoarginine is a novel risk factor for fatal strokes in patients undergoing coronary angiography. Stroke 42:1132–1134
Pilz S, Edelmann F, Meinitzer A et al (2014) Associations of methylarginines and homoarginine with diastolic dysfunction and cardiovascular risk factors in patients with preserved left ventricular ejection fraction. J Card Fail 20:923–930
Potena L, Fearon WF, Sydow K et al (2008) Asymmetric dimethylarginine and cardiac allograft vasculopathy progression: modulation by sirolimus. Transplantation 85:827–833
Radomski MW, Palmer RM, Moncada S (1990) An l-arginine/nitric oxide pathway present in human platelets regulates aggregation. Proc Natl Acad Sci 87:5193–5197
Ross R (1999) Atherosclerosis - an inflammatory disease. N Engl J Med 340:115–126
Saarelainen H, Valtonen P, Punnonen K et al (2008) Subtle changes in ADMA and l-arginine concentrations in normal pregnancies are unlikely to account for pregnancy-related increased flow-mediated dilatation. Clin Physiol Funct Imaging 28:120–124
Schnabel R, Blankenberg S, Lubos E et al (2005) Asymmetric dimethylarginine and the risk of cardiovascular events and death in patients with coronary artery disease: results from the AtheroGene Study. Circ Res 97:e53–e59
Schulze F, Lenzen H, Hanefeld C et al (2006) Asymmetric dimethylarginine is an independent risk factor for coronary heart disease: results from the multicenter Coronary Artery Risk Determination investigating the Influence of ADMA Concentration (CARDIAC) study. Am Heart J 152:493.e1–493.e8
Schwedhelm E, Wallaschofski H, Atzler D, et al. (2014) Incidence of all-cause and cardiovascular mortality predicted by symmetric dimethylarginine in the population-based study of health in Pomerania. PLoS One 9(5):e96875
Selcuk MT, Selcuk H, Temizhan A et al (2007) Asymmetric dimethylarginine plasma concentrations and l-arginine/asymmetric dimethylarginine ratio in patients with slow coronary flow. Coron Artery Dis 18:545–551
Sobczak A, Prokopowicz A, Radek M et al (2014) Tobacco smoking decreases plasma concentration of the emerging cardiovascular risk marker, l-homoarginine. Circ J 78:1254–1258
Tousoulis D, Koutsogiannis M, Papageorgiou N et al (2010) Endothelial dysfunction: potential clinical implications. Minerva Med 101:271–284
Tousoulis D, Bouras G, Antoniades C et al (2011a) Methionine-induced homocysteinemia impairs endothelial function in hypertensives: the role of asymmetrical dimethylarginine and antioxidant vitamins. Am J Hypertens 24:936–942
Tousoulis D, Kampoli AM, Papageorgiou N et al (2011b) Pathophysiology of atherosclerosis: the role of inflammation. Curr Pharm Des 17:4089–4110
Tousoulis D, Psaltopoulou T, Androulakis E et al (2015) Oxidative stress and early atherosclerosis: novel antioxidant treatment. Cardiovasc Drugs Ther 29:75–88
Tran CT, Leiper JM, Vallance P (2003) The DDAH/ADMA/NOS pathway. Atheroscler Suppl 4:33–40
Tsikas D, Kayacelebi AA (2014) Do homoarginine and asymmetric dimethylarginine act antagonistically in the cardiovascular system? Circ J 78:2094–2095
Tsikas D, Böger RH, Sandmann J, Bode-Böger SM, Frölich JC (2000a) Endogenous nitric oxide synthase inhibitors are responsible for the l-arginine paradox. FEBS Lett 478:1–3
Tsikas D, Sandmann J, Savva A et al (2000b) Assessment of nitric oxide synthase activity in vitro and in vivo by gas chromatography-mass spectrometry. J Chromatogr 742:143–153
Valkonen VP, Paiva H, Salonen JT et al (2001) Risk of acute coronary events and serum concentration of asymmetrical dimethylarginine. Lancet 358:2127–2128
Vallance P, Leone A, Calver A, Collier J, Moncada S (1992) Accumulation of an endogenous inhibitor of nitric oxide synthesis in chronic renal failure. Lancet 339:572–575
Valtonen P, Laitinen T, Lyyra-Laitinen T et al (2008) Serum l-homoarginine concentration is elevated during normal pregnancy and is related to flow-mediated vasodilatation. Circ J 72:1879–1884
van der Zwan LP, Davids M, Scheffer PG, Dekker JM, Stehouwer CD, Teerlink T (2013) l-Homoarginine and l-arginine are antagonistically related to blood pressure in an elderly population: the Hoorn Study. J Hypertens 31:1114–1123
Vogl L, Pohlhammer J, Meinitzer A et al (2015) Serum concentrations of l-arginine and l-homoarginine in male patients with intermittent claudication: a cross-sectional and prospective investigation in the CAVASIC Study. Atherosclerosis 239:607–614
Zoccali C, Bode-Böger S, Mallamaci F et al (2001) Plasma concentration of asymmetrical dimethylarginine and mortality in patients with end-stage renal disease: a prospective study. Lancet 358:2113–2117
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
This article does not contain any studies with human subjects or animals.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Papageorgiou, N., Androulakis, E., Papaioannou, S. et al. Homoarginine in the shadow of asymmetric dimethylarginine: from nitric oxide to cardiovascular disease. Amino Acids 47, 1741–1750 (2015). https://doi.org/10.1007/s00726-015-2017-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-015-2017-y