Abstract
Asymmetric dimethylarginine (ADMA) is an endogenous inhibitor of nitric oxide (NO) synthesis, whereas l-arginine (Arg) and l-homoarginine (hArg) serve as substrates for NO synthesis. ADMA and other methylated arginines are generally believed to exclusively derive from guanidine (N G)-methylated arginine residues in proteins by protein arginine methyltransferases (PRMTs) that use S-adenosylmethionine (SAM) as the methyl donor. l-Lysine is known for decades as a precursor for hArg, but only recent studies indicate that arginine:glycine amidinotransferase (AGAT) is responsible for the synthesis of hArg. AGAT catalyzes the formation of guanidinoacetate (GAA) that is methylated to creatine by guanidinoacetate methyltransferase (GAMT) which also uses SAM. The aim of the present study was to learn more about the mechanisms of ADMA and hArg formation in humans. Especially, we hypothesized that ADMA is produced by N G-methylation of free Arg in addition to the known PRMTs-involving mechanism. In knockout mouse models of AGAT- and GAMT-deficiency, we investigated the contribution of these enzymes to hArg synthesis. Arg infusion (0.5 g/kg, 30 min) in children (n = 11) and ingestion of high-fat protein meals by overweight men (n = 10) were used to study acute effects on ADMA and hArg synthesis. Daily Arg ingestion (10 g) or placebo for 3 or 6 months by patients suffering from peripheral arterial occlusive disease (PAOD, n = 20) or coronary artery disease (CAD, n = 30) was used to study chronic effects of Arg on ADMA synthesis. Mass spectrometric methods were used to measure all biochemical parameters in plasma and urine samples. In mice, AGAT but not GAMT was found to contribute to plasma hArg, while ADMA synthesis was independent of AGAT and GAMT. Arg infusion acutely increased plasma Arg, hArg and ADMA concentrations, but decreased the plasma hArg/ADMA ratio. High-fat protein meals acutely increased plasma Arg, hArg, ADMA concentrations, as well as the plasma hArg/ADMA ratio. In the PAOD and CAD studies, plasma Arg concentration increased in the verum compared to the placebo groups. Plasma ADMA concentration increased only in the PAOD patients who received Arg. Our study suggests that in humans a minor fraction of free Arg is rapidly metabolized to ADMA and hArg. In mice, GAMT and N G-methyltransferases contribute to ADMA and hArg synthesis from Arg, whereas AGAT is involved in the synthesis of hArg but not of ADMA. The underlying biochemical mechanisms remain still elusive.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
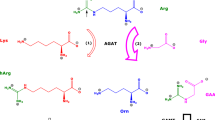
l-Arginine (Arg), a nutritionally semi-essential proteinogenic amino acid, is involved in many pathways and numerous physiological processes. As an example, Arg is the substrate of nitric oxide synthase (NOS; EC 1.14.13.39) isoforms which convert Arg to nitric oxide (NO) and l-citrulline (Moncada and Higgs 1993) (see reaction R1). Guanidine (N G)-methylation of Arg residues in proteins (R2) and their subsequent proteolysis (R3) are generally believed to be the sole mechanism by which l-N G-monomethylarginine (MMA), l-N G,N G-dimethylarginine (asymmetric dimethylarginine, ADMA) and l-N G,N´G-dimethylarginine (symmetric dimethylarginine, SDMA) are produced in mammals (Leiper and Vallance 1999). N G-Methylation of Arg residues in proteins is catalyzed by protein arginine methyltransferases (PRMTs) which use S-adenosylmethionine (SAM) as the methyl ([CH3]) donor. MMA, ADMA and SDMA are endogenous inhibitors of NOS activity (Tsikas et al. 2000). Homoarginine (hArg), an Arg homolog, has an additional methylene group (CH2) in its main chain and may also serve as NOS substrate (Hecker et al. 1991; Moali et al. 1998; Bretscher et al. 2003). Yet, its considerably lower physiological concentrations and affinity to NOS compared to Arg challenge the utility of hArg as an appreciable source of NO in humans. Arginine:glycine amidinotransferase (AGAT; EC 2.1.4.1; MIM 602360) is responsible for the synthesis of guanidinoacetate (GAA) from Arg and glycine (Ryan and Wells 1964; Ryan et al. 1968, 1969; Cathelineau et al. 1974; Levin et al. 1974; Kato et al. 1988; Wyss and Kaddurah-Daouk 2000; Cullen et al. 2006; Davids et al. 2012a) (R4). AGAT is also involved in the synthesis of hArg in humans (Davids et al. 2012a). This reaction (R5) utilizes lysine (Ryan and Wells 1964; Ryan et al. 1968, 1969) but the underlying mechanism is not yet explored. GAA is methylated to creatine (Cr) by guanidinoacetate:N-methyltransferase (GAMT; EC 2.1.1.2; MIM 601240) which uses SAM as the methyl donor (Ogawa et al. 1983; Roberts and Walker 1985; Takata et al. 1991) (R6).
It is well established that high circulating concentrations of ADMA are associated with cardiovascular diseases (Siroen et al. 2006; Böger et al. 2009; Teerlink et al. 2009). Recently, low circulating hArg concentrations have emerged as a risk factor for stroke (Pilz et al. 2011a), cardiovascular morbidity and mortality (Schmidt et al. 2004; März et al. 2010; Pilz et al. 2011b; Drechsler et al. 2011; Atzler et al. 2013; Choe et al. 2013a, b; Khalil et al. 2013; van der Zwan et al. 2013; Atzler et al. 2014; Kayacelebi et al. 2014a; Pilz et al. 2014, 2015a), and with liver dysfunction and mortality in chronic liver disease (Pilz et al. 2015b). Yet, the underlying mechanisms remain unclear. Elevated serum hArg concentrations during the third trimenon of pregnancy were related to increased flow-mediated vasodilatation, thus suggesting involvement of hArg in endothelial function (Valtonen et al. 2008).
Given the incompletely understood mechanisms of action, biosynthesis, metabolism and elimination of hArg and ADMA, we investigated the l-arginine/nitric oxide (Arg/NO) pathway in children, overweight men, and in elderly patients suffering from cardiovascular diseases which are closely associated with altered Arg/NO pathway. We have hypothesized that acute administration of Arg, either with high doses using the intravenous route or with lower doses as protein in a meal, may reveal additional information about potential mechanisms of hArg and ADMA biosynthesis and metabolism. These mechanisms may have remained undiscovered using chronic oral administration of Arg either as a drug or in form of proteins. The latter leads to several times lower circulating Arg concentrations compared to intravenous Arg use in humans and animals (Bode-Böger et al. 1998; Bode-Böger 2006; Wu et al. 2007; Yang et al. 2015).
Methods
Chemicals and reagents
The hydrochloride salts of Arg, hArg, MMA, ADMA and creatine were purchased from Sigma (Deisenhofen, Germany). Tetradeuterated methanol (CD3OD, 99 % at 2H) was supplied by Aldrich (Steinheim, Germany) and used in the de novo synthesis of deuterium-labelled methyl esters of amino acids for use as internal standards (Tsikas et al. 2003; Tsikas 2009). Pentafluoropropionic anhydride was obtained from Pierce (Rockford, IL, USA) and used for N-acylation of amino acids (Tsikas et al. 2003). All other chemicals were obtained from Merck (Darmstadt, Germany). Vivaspin 2 Hydrosart cartridges (cut-off, 10 kDa) were supplied by Sartorius (Göttingen, Germany) and used for generation of plasma ultrafiltrate in which the amino acids were finally analyzed (Tsikas et al. 2003). The Arg preparations used as drugs in the human studies are described below in the respective sections. The infusion solution of Arg, the effervescent tablets of Arg and the placebo tablets were analyzed by GC–MS (Tsikas et al. 2003; Kayacelebi et al. 2014b). They were found to contain the declared content of Arg and to be free of hArg, ADMA and MMA (data not shown).
AGAT- and GAMT-knockout mice
AGAT-knockout mice (AGAT−/−) and GAMT-knockout mice (GAMT−/−) were generated as described previously (Schmidt et al. 2004; Choe et al. 2013a, b). Some animals were fed a special diet containing 0.5 or 1 % creatine ad libitum after weaning (Ssniff, Germany). All experiments were approved by the local Ethics Committee for animals (TV-Nr. 08/08 and 110/10).
Infusion of Arg in children with suspected growth hormone deficiency
Children with short stature but not with other endocrinologic, organic, chromosomal, metabolic or psycho-social reasons for microsomia were routinely examined for growth hormone deficiency (GHD) by the so-called arginine test as described below. Children consumed fish for the last 24 h were excluded from analysis in our study. All children were overnight fasting for at least 9 h prior to the test. Sixty-six children (38 boys, 28 girls; aged 9.5 ± 3.2 years, range 3.5–17.3 years) with short stature were infused with an Arg hydrochloride solution in 0.9 % NaCl (Braun, Melsungen, Germany) at an infusion rate of 0.5 g Arg/kg bodyweight for 30 min. In 47 (30 boys, 17 girls) GHD was confirmed. In nine patients with confirmed and in two patients with non-confirmed GHD (Table 1), venous blood samples (2.7 mL) were collected in EDTA monovettes (Sarstedt, Germany) before starting the infusion, and 30, 45, 60, 90, and 120 min thereafter. In addition to blood, urine samples from spontaneous micturition were collected just before and 120 min after starting the infusion in 6 children. Urine (5 mL) and EDTA plasma (1 mL) samples were stored aliquoted at −20 and −80 °C, respectively, until analysis. The study was approved by the Ethics Committee of the Ruhr University Bochum.
Postprandial changes after the ingestion of high-fat protein meals in overweight men
Ten overweight (BMI > 25 kg/m2) men with enlarged waist circumference (>94 cm) (aged 21–50 years), without any serious illness, were recruited. The study was approved by the Institutional Review Board for Saint-Germain-en-Laye Hospital and the French Ministry for Health. All participants gave their written informed consent prior to enrolment. Three high-fat meals of the same nutritional composition but differing in the protein source were tested in a randomized crossover design. Each period consisted of a postprandial study, separated by at least 2 weeks. The composition of the meals was as follows: energy, 1200 kcal; fat, 93.3 g (70 % energy); carbohydrates, 45 g (15 % energy); crude protein, 45 g (15 % energy). The test meals consisted of a mixture of 233 g 40 %-fat cream, 45 g sucrose, 45 g protein as protein isolates, and 160 mL water. After the overnight fasting, the subjects ingested the meal and blood was sampled before the meal and 0.5, 1, 1.5, 2, 3, 4 and 6 h after the meal. Blood was centrifuged (2000×g, 5 min) immediately and plasma EDTA samples were kept frozen at −80 °C until analysis.
Oral administration of Arg to elderly subjects suffering from cardiovascular diseases
We performed two placebo-controlled studies on patients suffering from peripheral arterial occlusive disease (PAOD) (Table 2) or coronary artery disease (CAD) (Table 3). Patients received effervescent tablets (C. Hedenkamp GmbH, Hövelhof, Germany) that contained 2 g Arg hydrochloride (1.66 g Arg) or 2 g mannitol (placebo group), thrice a day, for 3 months in the PAOD study or 6 months in the CAD study resulting in a total amount of 9.96 g Arg per day in each study. Blood (9 mL) and spot urine samples (40 mL) were collected at the start of the studies, after 3 months (PAOD and CAD studies) and after 6 months (CAD study). Blood was centrifuged (2000×g, 5 min) immediately. EDTA plasma and urine samples were stored at −80 and −20 °C, respectively, until analysis. In the CAD study, plasma parameters were analyzed at the start and the end of study, yet not 3 months after the start. Both studies were approved by the Ethics Committee of the Hannover Medical School.
Biochemical analyses
Arg in plasma (Tsikas et al. 2003), hArg in plasma and urine (Kayacelebi et al. 2014b, 2015a) were measured by GC–MS. Plasma ADMA and MMA and urine ADMA concentrations were determined by GC–MS/MS (Tsikas et al. 2003). Creatinine in urine was determined by GC–MS (Tsikas et al. 2010). Urinary biomarkers were corrected for creatinine excretion and are expressed as µmol analyte per mmol creatinine.
Calculations and statistical analyses
Statistical analyses were performed and graphs were constructed by Origin 7.5G, GraphPad Prism 5.04 (GraphPad Prism Software Inc. San Diego, California, USA), or SigmaPlot. Distribution of variables was tested by Kolmogorov–Smirnov or D’Agostino and Pearson omnibus K2 test. Normally distributed parameters were compared by parametric tests (Student’s t test) and are presented as mean ± standard deviation (SD) or standard error of the mean (SEM). Non-normally distributed parameters were analyzed by non-parametric tests (Mann–Whitney test) and are presented as median and interquartile range (25th–75th percentile) or 95 % confidence interval. Correlations between variables were assessed by Pearson (parametric) or Spearman (non-parametric) correlation. P values <0.05 were considered as statistically significant. Where needed additional information is provided in the respective sections.
Results
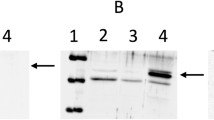
hArg and ADMA concentrations in plasma and urine of AGAT- and GAMT-knockout mice
Plasma hArg concentrations in AGAT−/− mice were significantly lower compared to AGAT-wild type (AGAT+/+) mice (Fig. 1a), suggesting that AGAT is a major contributor to plasma hArg in mice. The plasma hArg concentration did not differ in the GAMT−/− and GAMT-wild-type (GAMT+/+) mice (Fig. 1c), suggesting that GAMT is not a major contributor to plasma hArg in mice. The plasma ADMA concentration was similar in AGAT−/− and GAMT−/− mice compared to the wild-type mice (Fig. 1b, d), suggesting that neither AGAT nor GAMT are considerable contributors to plasma ADMA in mice. The plasma hArg/ADMA molar ratio tended (P = 0.12) to be lower in the AGAT−/− mice compared to the AGAT+/+ mice (Fig. 1g). The plasma hArg/ADMA molar ratio did not differ in the AGAT+/+ and GAMT+/+ mice, while it differed significantly (P = 0.02) in the AGAT−/− and GAMT−/− mice (Fig. 1g). Creatine supplementation tended (P = 0.08) to lower the plasma hArg concentration in AGAT+/+ mice (Fig. 1e), while it did not change plasma ADMA concentration in these mice (Fig. 1f). Plasma hArg (Fig. 1e) and plasma ADMA concentration (Fig. 1f) did not change in AGAT−/− mice supplemented with creatine.
Plasma hArg (a, c) and plasma ADMA (b, d) concentrations measured in AGAT−/−, GAMT−/−, AGAT+/+ and GAMT+/+ mice. Plasma hArg (e) and plasma ADMA (f) concentrations measured in AGAT−/−and AGAT+/+ mice supplemented with 0.5 or 1 % creatine. Data are shown as median ± interquartile range. g Plasma hArg/ADMA molar ratio in AGAT+/+, AGAT−/−, GAMT+/+ and GAMT−/− mice; data are shown as mean ± SEM. Cr creatine, WT wild type, KO knockout
Metabolism of infused Arg in children with growth hormone deficiency
Arg infusion (0.5 g/kg) for 30 min in children resulted in several-fold (about 18-fold) increase in mean Arg plasma concentration (from 79 to 1435 µM), which began to fall immediately after stopping the infusion (Fig. 2a). At the end of the arginine test (120 min), the mean Arg plasma concentration (468 µM) was still far above baseline. hArg (Fig. 2b) and ADMA (Fig. 2c) plasma concentrations increased during the infusion period as well, albeit to a far lower extent compared to Arg. At the infusion end, mean hArg and ADMA plasma concentrations were increased each about twofold over their baseline levels. In contrast to Arg, hArg and ADMA plasma concentrations seem to have reached a 15-min lasting plateau. At the end of the arginine test, the hArg and ADMA plasma concentrations did not reach baseline values. Interestingly, the baseline plasma hArg/ADMA ratio did not change at the end of the infusion (2.76:1 vs 2.80:1), but it fell subsequently by about 20 % after 90 min (2.18:1) and 120 min (2.19:1) (Fig. 2d). With regard to the urinary excretion, ADMA but not hArg excretion increased statistically significantly after Arg infusion (Fig. 3). ADMA excretion after the arginine test correlated well with the baseline ADMA excretion, while hArg excretion varied remarkably.
Plasma concentration (mean ± SEM) of Arg (a), hArg (b) and ADMA (c), and plasma hArg/ADMA molar ratio (d) at the start (0 min) and the end (30 min) of Arg the infusion (0.5 g/kg body weight) into 11 children, as well as at the indicated time points after stopping the infusion. Two of the children investigated underwent two times the arginine test. Horizontal dotted lines indicate the levels of the respective baseline values
Creatinine-corrected urinary excretion of ADMA (a) and hArg (c) in six children who received Arg infusion (0.5 g/kg body weight) for 30 min (data are presented as mean ± SEM). One of the children underwent two times the arginine test as indicated by arrows in b and d. Urine from spontaneous micturition was collected before (BEFORE) and 120 min after infusion start (AFTER). Linear regression analysis between the excretion value (µmol/mmol creatinine) of ADMA (b) or hArg (d) AFTER (y axis) and that BEFORE (x axis). For simplicity the units are not indicated on the x and y axes in b and d
Postprandial changes after ingestion of high-fat protein meals in overweight men
For the purpose of the present study, results were averaged and analyzed for the postprandial changes only, i.e., collapsing the protein factor, using a mixed model for analysis of repeated data (Proc Mixed, SAS). Post hoc difference from baseline value was analyzed using Bonferroni corrections. Plasma concentrations of Arg, ADMA and hArg changed after meal ingestion (all P < 0.001) (Fig. 4a). Mean plasma Arg concentrations were significantly higher than the mean fasting value for the first 2 h after meals. Yet, the highest plasma Arg concentration was only by 10 % higher than its baseline concentration. Plasma hArg concentrations for the first 4 h and plasma ADMA concentrations for the first hour were significantly higher than the baseline values (Fig. 4a). The plasma hArg/ADMA ratio increased from 5.6:1 (RSD, 7.2 %) at baseline to maximally 6.7:1 (RSD, 6.6 %) at 4 h and fell slightly to 6.3:1 (RSD, 6.5 %) 6 h after meal (Fig. 4b). In the whole group, plasma hArg (Spearman’s r = 0.425, P < 0.0001) and plasma ADMA concentrations (Spearman’s r = 0.539, P < 0.0001) were positively correlated with plasma Arg concentration (Fig. 5a, b). There was also a positive even though weaker correlation between plasma concentrations of ADMA and hArg (Spearman’s r = 0.327, P < 0.0001) (Fig. 5c). The changes in circulating hArg concentrations seen upon ingestion of the high-fat protein meals may be due to their Lys content as Lys is a precursor of hArg (Ryan and Wells 1964).
a Plasma concentrations of Arg, ADMA and hArg, and b plasma hArg/ADMA molar ratio at baseline and at the indicated time points after high-fat meals ingestion by ten overweight men. Data are shown as mean ± SEM. Asterisks indicate statistical significance with respect to the respective baseline values. Horizontal dotted lines indicate the levels of the respective baseline values
Correlation analysis (Spearman’s correlation coefficient) between hArg and Arg (a), ADMA and Arg (b), and ADMA and hArg (c). All individual plasma concentrations of hArg, ADMA and ADMA in the postprandial measurement were considered. See also Fig. 4
Metabolism of orally administered Arg in elderly PAOD and CAD patients
In the PAOD and CAD studies we measured in plasma and urine samples of the verum and placebo groups Arg and its N G-methylated metabolites yet not hArg.
In the PAOD patients, Arg intake for 3 months significantly (P = 0.002) increased the mean plasma Arg concentration (1.4-fold from 56.5 to 80 µM); in the placebo group, the mean plasma Arg concentration (56.4 vs 50.9 µM) did not change significantly after 3 months (Fig. 6a). In the Arg group, the mean plasma ADMA concentration increased significantly (P = 0.05) from 0.51 to 0.55 µM after 3 months of Arg supplementation (Fig. 6b). In the placebo group, no significant change in mean plasma ADMA concentration (0.59 vs 0.54 µM) was observed (Fig. 6b). Excretion of Arg (Fig. 6c) and ADMA (Fig. 6d) in the urine increased only in the Arg group.
Plasma concentrations of Arg (a) and ADMA (b), and creatinine-corrected excretion rates of Arg (c) and ADMA (d) at baseline and after 3-months of oral ingestion of 9.96 g/day Arg (ARGININE, n = 20) or placebo (PLACEBO, n = 20) by PAOD patients. Data are presented as mean ± SD. An asterisk indicates P < 0.05. The symbol open triangle indicates the statistically significant difference for Arg and ADMA between baseline and 3-months in the ARGININE group
In the CAD patients, Arg ingestion for 6 months significantly (P < 0.001) increased (1.4-fold) the median plasma Arg concentration from 67.7 to 94.7 µM; in the placebo group, the median plasma Arg concentration did not change (58.9 to 60.6 µM) significantly after 6 months (Table 4). The median plasma ADMA concentration did not change significantly in the Arg group (from 0.50 to 0.50 µM) or in the placebo group (from 0.46 to 0.47 µM) after 6 months (Table 4). The median plasma MMA concentration increased significantly (P = 0.002) in the Arg group (1.6-fold from 0.15 to 0.24 µM) but not in the placebo group (from 0.15 to 0.15 µM) after 6 months. Excretion of Arg (after 3 and 6 months) and ADMA (after 3 months) in the urine increased only in the Arg group (Table 4). Interestingly, median Arg excretion increased by a factor of 1.8 after 3 months but only by a factor of 1.3 after 6 months, while median ADMA excretion increased only marginally (by a factor 1.046 and 1.034, respectively). The considerable decrease in Arg excretion after 6 months toward the baseline level suggests improved reabsorption of Arg in the kidney.
Discussion
Arg and hArg
Arg belongs to the best investigated, nutritionally semi-essential, proteinogenic, multi-functional amino acids (Wu et al. 2009). Less than 0.1 % of Arg is utilized in healthy untreated humans for the NOS-catalyzed formation of NO virtually in all types of cell. Nevertheless, the Arg/NO pathway plays a pivotal role in health and disease. The endogenous N G-methylated Arg derivatives, MMA, ADMA and SDMA, and synthetic N G-substituted Arg analogs such as N G-nitroarginine (free acid, NNA; methyl ester, l-NAME) are inhibitors of NOS activity (Tsikas et al. 2000; Kielstein et al. 2007). Unlike Arg, our present knowledge of the biochemistry and pathophysiology of hArg, the methylene homolog of Arg, is fragmentary, although hArg is known for at least five decades (Ryan and Wells 1964). hArg only very recently received particular scientific attention in the area of human physiology and pathology. Low circulating hArg concentrations were found to be associated with cardiovascular morbidity and mortality (Pilz et al. 2011a, b; März et al. 2010; Drechsler et al. 2011; Atzler et al. 2013, 2014; Choe et al. 2013a; Kayacelebi et al. 2014a; Pilz et al. 2015a), as well as with liver dysfunction and mortality in chronic liver disease (Pilz et al. 2015b). Although the underlying mechanisms of action of ADMA and much less of hArg are not yet fully understood, hArg seems to behave antagonistically to ADMA in the cardiovascular system (Siroen et al. 2006; Böger et al. 2009; Teerlink et al. 2009). We therefore introduced the hArg/ADMA molar ratio in order to take into account the supposed opposite actions of hArg and ADMA (Khalil et al. 2013; Tsikas and Kayacelebi 2014). hArg can be utilized by NOS isoforms to produce NO, but the concentration of hArg in human circulation (0.5–3 µM) and the affinity of hArg to NOS isoforms are several times lower than those of Arg (Hecker et al. 1991; Moali et al. 1998; Bretscher et al. 2003). Therefore, circulating concentrations of hArg are unlikely to play a direct role in NO-related dysfunctions. Furthermore, as ADMA is a very weak inhibitor (IC50 ≈ 12 µM) of endothelial NOS (eNOS) activity (Kielstein et al. 2007), one may reasonably assume that ADMA may exert additional activities in the circulation beyond eNOS inhibition.
N G-Methylation of Arg
MMA, ADMA and SDMA formation is assumed to exclusively occur via N G-methylation of Arg residues in proteins by the action of PRMTs and subsequent regular proteolysis (Leiper and Vallance 1999). We hypothesized that other, not yet explored biochemical pathways and physiological functions of ADMA and hArg are likely to exist and to be even more potent in the cardiovascular system than their involvement as inhibitors/substrates in the Arg/NO pathway. Specifically, we assumed that MMA, ADMA and SDMA are also formed from N G-methylation of free Arg. hArg’s biochemistry includes Arg and the enzymes AGAT and GAMT (Ryan and Wells 1964; Ryan et al. 1968, 1969; Cathelineau et al. 1974; Levin et al. 1974; Ogawa et al. 1983; Roberts and Walker 1985; Kato et al. 1988; Takata et al. 1991; Wyss and Kaddurah-Daouk 2000; Cullen et al. 2006; Davids et al. 2012a). We therefore performed an animal study in knockout mouse models of AGAT- and GAMT-deficiency. As the mechanisms leading to hArg formation in humans are not entirely delineated, we performed post hoc analyses of three human studies in order to better understand the pathways responsible for the hypothetical biosynthesis of hArg and ADMA from soluble Arg. For not yet fully elucidated analytical reasons (Tsikas et al. 2011) the quantitative determination of SDMA in plasma by our GC–MS and GC–MS/MS methods (Kayacelebi et al. 2015a) is not accurate and precise enough, so that we cannot provide dependable data for circulating SDMA which is also an inhibitor of NOS activity (Tsikas et al. 2000) and a risk factor for morbidity and mortality in various diseases including chronic liver disease (Pilz et al. 2015b).
Role of AGAT and GAMT in the synthesis of hArg and ADMA
The results obtained from mice experiments (previous study Choe et al. 2013a, b; and present study) suggest that AGAT is involved in the synthesis of hArg from Arg. In the AGAT+/+ mice, creatine supplementation resulted in borderline inhibition of hArg formation, suggesting that creatine, presumably at high concentrations, may inhibit AGAT-mediated formation of hArg. These findings are supported by published work indicating that AGAT activity is inhibited in chick and rat tissues by creatine and its N-alkylated analogs rather than by GAA (Walker and Hannan 1976; Roberts and Walker 1985). It is also worth mentioning that creatine supplementation (0.4 %) led to a decrease in AGAT activity in rat pancreas (da Silva et al. 2014). A recent study provided evidence for the involvement of AGAT in hArg synthesis in humans (Davids et al. 2012a). These observations suggest that AGAT plays a major role in hArg synthesis in mice and humans. The inherent reaction that is catalyzed by AGAT has been suggested to be the reaction of Arg with Gly to produce GAA and Orn (R4) but not hArg (Humm et al. 1997). AGAT-catalyzed formation of hArg from Arg would therefore require either reaction of Arg with Lys to form Orn and hArg (R5) or reaction of GAA with Lys to form Gly and hArg (R7). The net reaction of (R4) and (R7) would be reaction (R5). The AGAT-catalyzed formation of hArg from Arg could be regarded as a consecutive reaction consisting of the preceding reaction (R4) and the subsequent reaction (R7). This would mean, that reaction (R4) delivers GAA which is subsequently consumed in (R7) to produce hArg. In this concept, GAA would play a decisive role, reaction (R4) would be the rate-limiting step of the whole reaction (R5), and AGAT would have an additional catalytic activity that finally yields hArg after reaction (R7).
As GAA is a substrate for GAMT in reaction (R6), the activity of AGAT regarding reaction (R4) may also influence the activity of GAMT with respect to reaction (R6), and perhaps reversely. Thus, a mutual interaction between AGAT and GAMT appears reasonable, whereby AGAT activity could have a higher effect on GAMT activity than reversely, at least in mice. Supplementation of rats with creatine decreased SAM synthesis (da Silva et al. 2014). In our mice experiments, creatine supplementation borderline decreased plasma hArg concentrations. These findings are supportive of an overlap and interdependency of AGAT- and GAMT-catalyzed reactions.
Our results from the mice experiments suggest that neither AGAT nor GAMT are involved in ADMA synthesis in mice. Whether the observations of these experiments can be translated to humans, remains to be demonstrated. Reported data on hArg and ADMA in AGAT- and GAMT-deficient humans are not available thus far. It is worth mentioning that mice had comparable plasma ADMA concentrations with those of children and men, but mice had 5–10 times lower plasma hArg concentrations than humans. Thus, from the quantitative point of view considerable differences between mice and humans regarding AGAT and GAMT activity may occur.
Effect of Arg infusion on hArg and ADMA
The children study was carried out in the setting of a routinely performed Arg infusion, the so-called arginine test, in the clinic. The arginine test includes a 30-min lasting infusion of a concentrated Arg solution in physiological saline (i.e., 0.5 g Arg per kg bodyweight). This procedure results in high circulating free Arg concentrations and allows study acute effects of Arg and the derivatives that may be rapidly formed from Arg including NO (Bode-Böger et al. 1999; Mariotti et al. 2013).
Arg infusion in the children resulted in average in 18-fold increase of the plasma Arg concentration. At the end of the Arg infusion (time 30 min), the concentration of both, hArg and ADMA, in the plasma was two times higher than immediately before the infusion (time 0 min). At the end of the arginine test (120 min), a small portion of circulating hArg and ADMA was found to be excreted in the urine. Impaired excretion of circulating hArg and ADMA is unlikely to explain the sudden increase in the plasma hArg and ADMA concentrations measured at the infusion end. A doubling of the plasma concentration of hArg and ADMA after 30 min would require an acute and almost complete displacement of intracellular hArg and ADMA, including erythrocytic hArg and ADMA. Because of the high molar excess of exogenous Arg over endogenous Arg, hArg and ADMA, and because of the existence of cellular cationic amino acid transporters, such a displacement cannot be fully excluded. Arg-induced proteolysis of intracellular ADMA-rich proteins could explain an increase in ADMA but not in hArg plasma concentration. Thus, Arg-induced proteolysis upon Arg infusion seems to be of purely theoretical value. Rather, the changes in circulating hArg concentrations seen upon infusion of Arg may be due to Arg-induced increases in growth hormone (McGuire et al. 1980). In theory, guanidination of Lys residues in proteins and their subsequent proteolysis could also yield hArg. However, guanidination of Lys moieties in proteins requires high concentrations of activated urea derivatives such as O-methylisourea and drastic reactions conditions (Yin et al. 2015). Perhaps more likely is the formation of hArg from homocitrulline previously formed from free Lys by the catalytic action of ornithine transcarbamylase (OTC), although Lys is a much poorer substrate than Orn (Burnett and Cohen 1957).
Methionine is the precursor of SAM. A recent study demonstrated formation of methyl-trideuterated MMA, ADMA and SDMA just 60 min after starting infusion of [methyl-2H3]-1-[13C]methionine into humans (Davids et al. 2012b). Thus, another likely mechanism for the rapid increase seen in the plasma ADMA concentration in our infusion study could involve direct N G-methylation of the infused Arg prior to its incorporation in proteins. That free ADMA measured in the plasma samples of our children from blood taken just 30 min after starting the infusion is derived exclusively by the action of PRMTs on Arg residues in proteins cannot be excluded but is unlikely. A time period of only 30 min would most likely not suffice to synthesize specific proteins that are subsequently N G-methylated on Arg and proteolyzed to finally release free ADMA in the plasma in an amount that would double its baseline plasma concentration (Miller et al. 1949; Yuile et al. 1951). The kinetics of ADMA and hArg observed in the children study argues against a considerable contribution of PRMTs to ADMA from infused Arg during the study. It is more likely that N-methyltransferases in organs such as liver and kidney and in cells such as erythrocytes have contributed to ADMA to a much higher extent than PRMTs during the short infusion period of 30 min. A driving force for the rapid ADMA formation from infused Arg by N-methyltransferases could be the supraphysiological concentration of Arg in the children’s bodies.
Effect of short-term and long-term oral Arg administration on hArg and ADMA
The second and the third human study aimed at investigating short-term and long-term effects of Arg at circulating concentrations of the same order of physiological blood concentrations of Arg. Short-term effects of Arg were managed by using protein-rich meals as a source of Arg. Long-term effects of Arg were studied by oral intake of Arg at amounts that are comparable to those regularly ingested by adults daily (Brosnan and Brosnan 2004).
Interestingly, ingestion of high-fat protein meals by overweight men also resulted in acute increases of ADMA and hArg plasma concentrations, although the increase in plasma Arg concentration was very low (1.1-fold). Even just 30 min after the meals, the plasma concentrations of ADMA, hArg and Arg were all significantly increased. Although the kinetics observed for these amino acids was different from that seen in children upon Arg infusion, the rapid appearance of ADMA in blood strongly argues for ADMA synthesis by a rapid mechanism that does not involve N G-methylation of Arg residues in proteins. It is worth mentioning that children and men had comparable fasting plasma concentrations of Arg and ADMA, but different fasting plasma hArg concentrations. This resulted in quite different fasting plasma hArg/ADMA molar ratios, i.e., 2.8:1 in children and 5.6:1 in adults. Yet, the most striking difference between children and adults concerns the course of the plasma hArg/ADMA molar ratios. During Arg infusion the plasma hArg/ADMA molar ratio remained unchanged and decreased slowly after stopping the infusion. By contrast, the plasma hArg/ADMA molar ratio increased slowly over 4 h after the meals. Considering that hArg and ADMA are likely to antagonize each other in the cardiovascular system (Tsikas and Kayacelebi 2014), Arg infusion would shift the balance between hArg and ADMA in favor of ADMA. Because Arg is well tolerated by children and adults (Bode-Böger 2006), the acute and slight decrease of the hArg/ADMA caused by infused Arg seems to be of minor importance.
That the plasma hArg/ADMA molar ratio decreased after the end of Arg infusion and remained below the baseline value for at least 90 min, suggests that Arg-derived amino acids, most likely ornithine (Orn), and other substances derived from Arg metabolism in the urea cycle, may have inhibited hArg formation from Arg. Such an effect was not observed in men who have received high-fat protein meals, presumably because the concentration of Arg metabolites was not high enough to inhibit hArg formation to a measurable extent.
Is free Arg N G-methylated to MMA, ADMA and SDMA?
SAM is the common donor of methyl groups in transmethylation reactions which are catalyzed by numerous different N-, O- and S-methyltransferases (Katz et al. 2003). In such a reaction, the first reaction product of free Arg would be free MMA which could be further N G-methylated to form free ADMA and SDMA. Such a reaction is supported by the observation that infusion of the SAM precursor [methyl-2H3]-1-[13C]methionine to humans did not result in formation of hexadeutero-ADMA (2H6-ADMA) and hexadeutero-SDMA (2H6-SDMA) (Davids et al. 2012b). A possible explanation for this finding may be that already available endogenous unlabeled MMA was simply N G-methylated by [2H3,13C]SAM to produce trideutero-ADMA (2H3-ADMA) and trideutero-SDMA (2H3-SDMA). We are not aware from the literature that the N G-methyltransferases GAMT and PRMTs are also able to N G-methylate free (soluble) Arg. In the PAOD and CAD studies, orally administered Arg may also have contributed to the formation of ADMA via MMA from soluble Arg by the catalytic action of N G-methyltransferases. That in the CAD study plasma MMA concentration after 6 months of Arg ingestion had been doubled compared to the beginning, is supportive of N G-methylation of free MMA to yield ADMA and SDMA. The concentration of MMA in plasma of healthy adults is several times lower than that of SDMA and ADMA (e.g., Table 4) (Martens-Lobenhoffer and Bode-Böger 2012). This may be an indication that MMA (i.e., simply N G-methylated Arg) is an intermediate product in the synthesis of ADMA and SDMA (i.e., doubly N G-methylated Arg) from soluble (free) Arg.
An alternative mechanism for PRMTs-independent formation of MMA, ADMA and SDMA could be a combination of GAMT- and AGAT-like activities. Thus, guanidinoacetate (GAA) could be N-methylated to intermediates (R8; Me is CH3), which subsequently react with Orn to generate Arg, MMA, ADMA, SDMA and N-methylglycine (i.e., sarcosine) (R9a–R9e). Such a mechanism is supported by findings indicating that the methyl group of N-methylglycine is derived from methionine in humans (Walker and Hannan 1976) and in rats (Horner and Mackenzie 1950). The broad class of SAM-dependent methyltransferases is also supportive of such a mechanism (Yuile et al. 1951). Yet, to the best of our knowledge there are no reports on the physiological appearance of [N G,N G-Me2]GAA and [N G,N´ G-Me2]GAA.
In the studies reported here, we did not measure SDMA, Cit, Orn and other members of the urea cycle. We can, therefore, not exclude that certain substances of this pathway may have contributed to the enhancement of ADMA concentration seen upon Arg infusion. For instance, Cit at mM-concentrations has been reported to inhibit the activity of dimethylarginine dimethylaminohydrolase (DDAH) (MacAllister et al. 1996), i.e., the enzyme that hydrolyses ADMA to Cit and dimethylamine (DMA) (R10). However, in consideration of the weak inhibitory potency of Cit on DDAH activity, the increase in ADMA excretion and the parallel kinetics of hArg and ADMA upon Arg infusion argue against a considerable contribution of Arg-derived Cit to plasma ADMA concentration via DDAH activity inhibition. In contrast, in citrullinemic children, with plasma citrulline concentrations ranging between 0.3 and 2.1 mM, we have observed even an elevated whole body ADMA synthesis (Lücke et al. 2006). This observation also argues against a contribution of Cit to the increased plasma ADMA concentrations seen upon Arg infusion.
In the present study, we observed remarkable correlations (P < 0.0001 for all cases) between the plasma concentrations of hArg and Arg, ADMA and Arg (r = 0.539), and even between ADMA and hArg (r = 0.327) before and after the meals (Fig. 5). In previous studies from our and other groups, considerable correlations were found between ADMA, hArg and Arg in plasma and urine of healthy and sick subjects at the basal state (e.g., Khalil et al. 2013; van der Zwan et al. 2013; Jaźwińska-Kozuba et al. 2013; Kayacelebi et al. 2014b; Tomaschitz et al. 2014). Yet, in other studies no correlations were found between hArg and ADMA, for instance in a large cohort of subjects referred to coronary angiography (März et al. 2010) or in rheumatic disease (Kayacelebi et al. 2015b). In general, reported associations between ADMA and Arg or between hArg and Arg are stronger than between ADMA and hArg. A possible explanation for correlations found in the studies mentioned above may be that not only hArg, but also ADMA are derived directly from free Arg (Fig. 7).
Schematic illustration of proposed reactions, enzymes and reaction products involved in the synthesis of hArg and ADMA from free Arg catalyzed by AGAT and free Arg N G-methyltransferases (free Arg N G-MT), respectively. Guanidinoacetate is produced from Arg and Gly by AGAT. GAMT methylates guanidinoacetate to produce creatine. Free Arg N G-MT and GAMT require SAM as the methyl donor. The N G-methylated hArg, homoMMA, homoSDMA and homoADMA are purely hypothetical; they have not been detected in human body fluids and tissues so far. SAH S-adenosyl homocysteine
Limitations of the studies
With exception of the knock out mice studies, the studies described in the present work were not primarily designed to address the questions of the present paper, but are rather post hoc analyses. In general, the hArg, ADMA and MMA content of the meals and chow in the studies is unknown and we cannot therefore entirely exclude that diet may have contributed to the changes we observed for some amino acids, notably in the short-term ingestion of high-fat protein meals study. Another limitation of our studies is the relatively small sample size and the possible problems of multiple testing. The availability of SDMA data would have certainly enhanced the informative value of our studies regarding the N G-methylation of free Arg to form MMA and ADMA.
Conclusions and perspectives
The results of the knockout mice experiments reported in the present work provide evidence that AGAT is involved in the synthesis of hArg from free Arg, but they do not reveal the underlying mechanism (Fig. 7). As AGAT-catalyzed hArg synthesis seems to be inhibited by creatine, i.e., the reaction product of GAMT, AGAT and GAMT pathways may overlap in the mouse, with GAA being probably the point of intersection (Fig. 7). In humans, hArg synthesis has been reported to be regulated by AGAT. Although the present study does not provide direct evidence of the involvement of AGAT in the conversion of Arg to hArg in children and adults, our observations strongly suggest that hArg is biosynthesized from free Arg in humans. We also acknowledge that our human studies do not provide direct evidence of the N G-methylation of free Arg to ADMA. Yet, the almost parallel and sudden increases in hArg and ADMA plasma concentration upon acute Arg administration as an infusion or protein meal is a strong indication for the direct conversion of free Arg to ADMA. Our study also does not answer the question which enzymes catalyze N G-methylation of free Arg to ADMA in humans. Yet, the mice experiments do not support the idea that GAMT belongs to these SAM-dependent N G-methyltransferases. This issue remains to be evaluated in forthcoming, highly challenging and therefore well-conducted studies.
Further investigations are warranted, which should involve measurement of a variety of analytes potentially being involved in Arg-related pathways, including Orn, Lys, Gly, GAA and creatine. Determination and use of the plasma hArg/ADMA molar ratio may help not only delineate related biochemical pathways, but also monitor, control and optimize nutritional and pharmacological treatments of cardiovascular diseases. The biosynthesis and metabolism of hArg has been only little investigated thus far. Forthcoming studies need to address whether the known Arg pathways also apply to hArg. For instance, decarboxylation of hArg would yield the biogenic amine homoagmatine. N G-Methylation of free hArg would yield homo-MMA (hMMA), homo-SDMA (hSDMA) and homo-ADMA (hADMA) (Fig. 7). Do these substances occur in human fluids and tissues? If existent, they would be expectable at much lower concentrations than their congeners MMA, SDMA and ADMA, and would represent a big analytical challenge.
The kidney and the liver play major roles in the biosynthesis and metabolism of Arg, hArg and relatives. These both organs seem to be of decisive importance not only for their own wellness, but also for a healthy and well-functioning cardiovascular system. l-Arginine is well tolerated by humans. Acute administration of Arg (i.e., the l-arginine test) in combination with the use of stable-isotope labeled Arg, notably [guanidine-15N2]-l-arginine, in vitro and in vivo studies in animals and humans should help delineate the biochemistry of hArg which lived in the shadow of Arg until very recently, and would also help evaluate the pharmacological potential of this “exotic” amino acid.
Abbreviations
- ADMA:
-
Asymmetric dimethylarginine (l-N G,N G-dimethylarginine)
- AGAT:
-
Arginine:glycine amidinotransferase
- CAD:
-
Coronary artery disease
- Cr:
-
Creatine
- DDAH:
-
Dimethylarginine dimethylaminohydrolase
- DMA:
-
Dimethylamine
- GAA:
-
Guanidinoacetate
- GAMT:
-
Guanidinoacetate methyltransferase
- GC–MS:
-
Gas chromatography–mass spectrometry
- GC–MS/MS:
-
Gas chromatography–tandem mass spectrometry
- GHD:
-
Growth hormone deficiency
- hArg:
-
Homoarginine
- KO:
-
Knockout
- Me:
-
Methyl
- MMA:
-
l-N G-Monomethylarginine
- NO:
-
Nitric oxide
- NOS:
-
Nitric oxide synthase
- PAOD:
-
Peripheral arterial occlusive disease
- PRMT:
-
Protein arginine methyltransferase
- SAM:
-
S-Adenosylmethionine
- SDMA:
-
Symmetric dimethylarginine (l-N G,N´ G-dimethylarginine)
- WT:
-
Wild type
References
Atzler D, Rosenberg M, Andersso M, Choe CU, Lutz M, Zugck C et al (2013) Homoarginine—an independent marker of mortality in heart failure. Int J Cardiol 168:4907–4909
Atzler D, Gore MO, Ayers CR, Choe CU, Böger RH, de Lemos JA, McGuire DK, Schwedhelm E (2014) Homoarginine and cardiovascular outcome in the population-based Dallas Heart Study. Arterioscler Thromb Vasc Biol 34:2501–2507
Bode-Böger SM (2006) Effect of arginine supplementation on NO production in man. Eur J Clin Pharmacol 62:91–99
Bode-Böger SM, Böger RH, Galland A, Tsikas D, Frölich JC (1998) Arginine-induced vasodilation in healthy humans: pharmacokinetic-pharmacodynamic relationship. Br J Clin Pharmacol 46:489–497
Bode-Böger SM, Böger RH, Löffler M, Tsikas D, Brabant G, Frölich JC (1999) l-Arginine stimulates NO-dependent vasodilation in healthy humans—effect of somatostatin pretreatment. J Investig Med 47:43–50
Böger RH, Maas R, Schulze F, Schwedhelm E (2009) Asymmetric dimethylarginine (ADMA) as a prospective marker of cardiovascular disease and mortality-an update on patient populations with a wide range of cardiovascular risk. Pharmacol Res 60:481–487
Bretscher LE, Li H, Poulos TL, Griffith OW (2003) Structural characterization and kinetics of nitric-oxide synthase inhibition by novel N5-(iminoalkyl)- and N5-(iminoalkenyl)-ornithines. J Biol Chem 278:46789–46797
Brosnan ME, Brosnan JT (2004) Renal arginine metabolism. J Nutr 134:2791S–2895S
Burnett GH, Cohen PP (1957) Study of carbamyl phosphate-ornithine transcarbamylase. J Biol Chem 229:337–344
Cathelineau L, Saudubray JM, Charpentier C, Polonovski C (1974) Letter: the presence of the homoanalogues of substrates of the urea cycle in the presence of argininosuccinate synthetase deficiency. Pediatr Res 8:857
Choe CU, Atzler D, Wild PS, Carter AM, Boger RH, Ojeda F et al (2013a) Homoarginine levels are regulated by arginine:glycine amidinotransferase and affect stroke outcome: results from human and murine studies. Circulation 128:1451–1461
Choe CU, Nabuurs C, Stockebrand MC, Neu A, Nunes P, Morellini F et al (2013b) Arginine:glycine amidinotransferase deficiency protects from metabolic syndrome. Hum Mol Genet 22:110–123
Cullen ME, Yuen AH, Felkin LE, Smolenski RT, Hall JL, Grindle S et al (2006) Myocardial expression of the arginine:glycine amidinotransferase gene is elevated in heart failure and normalized after recovery: potential implications for local creatine synthesis. Circulation 114:I16–I20
da Silva RP, Clow K, Brosnan JT, Brosnan ME (2014) Synthesis of guanidinoacetate and creatine from amino acids by rat pancreas. Br J Nutr 111:571–577
Davids M, Ndika JD, Salomons GS, Blom HJ, Teerlink T (2012a) Promiscuous activity of arginine:glycine amidinotransferase is responsible for the synthesis of the novel cardiovascular risk factor homoarginine. FEBS Lett 586:3653–3657
Davids M, Swieringa E, Palm F, Smith DE, Smulders YM, Scheffer PG et al (2012b) Simultaneous determination of asymmetric and symmetric dimethylarginine, l-monomethylarginine, arginine, and l-homoarginine in biological samples using stable isotope dilution liquid chromatography tandem mass spectrometry. J Chromatogr B 900:38–47
Drechsler C, Meinitzer A, Pilz S, Krane V, Tomaschitz A, Ritz E et al (2011) Homoarginine, heart failure, and sudden cardiac death in haemodialysis patients. Eur J Heart Fail 13:852–859
Hecker M, Walsh DT, Vane JR (1991) On the substrate specificity of nitric oxide synthase. FEBS Lett 294:221–224
Horner WH, Mackenzie CG (1950) The biological formation of sarcosine. J Biol Chem 187:15–22
Humm A, Fritsche E, Steinbacher S, Huber R (1997) Crystal structure and mechanism of human l-arginine:glycine amidinotransferase: a mitochondrial enzyme involved in creatine biosynthesis. EMBO J 16:3373–3385
Jaźwińska-Kozuba A, Martens-Lobenhoffer J, Kruszelnicka O, Rycaj J, Chyrchel B, Surdacki A, Bode-Böger SM (2013) Opposite associations of plasma homoarginine and ornithine with arginine in healthy children and adolescents. Int J Mol Sci 14:21819–21832
Kato T, Sano M, Mizutani N, Hayakawa C (1988) Homocitrullinuria and homoargininuria in hyperargininaemia. J Inherit Metab Dis 11:261–265
Katz JE, Dlakić M, Clarke S (2003) Automated identification of putative methyltransferases from genomic open reading frames. Mol Cell Proteomics 2:525–540
Kayacelebi AA, Nguyen TH, Neil C, Horowitz JD, Jordan J, Tsikas D (2014a) Homoarginine and 3-nitrotyrosine in patients with takotsubo cardiomyopathy. Int J Cardiol 173:546–547
Kayacelebi AA, Beckmann B, Gutzki FM, Jordan J, Tsikas D (2014b) GC–MS and GC–MS/MS measurement of the cardiovascular risk factor homoarginine in biological samples. Amino Acids 46:2205–2217
Kayacelebi AA, Knöfel AK, Beckmann B, Hanff E, Warnecke G, Tsikas D (2015a) Measurement of unlabeled and stable isotope-labeled homoarginine, arginine and their metabolites in biological samples by GC–MS and GC–MS/MS. Amino Acids. doi:10.1007/s00726-015-1984-3
Kayacelebi AA, Willers J, Pham VV, Hahn A, Schneider JY, Rothmann S, Frölich JC, Tsikas D (2015b) Plasma homoarginine, arginine, asymmetric dimethylarginine and total homocysteine interrelationships in rheumatoid arthritis, coronary artery disease and peripheral artery occlusion disease. Amino Acids. doi:10.1007/s00726-015-1915-3
Khalil AA, Tsikas D, Akolekar R, Jordan J, Nicolaides KH (2013) Asymmetric dimethylarginine, arginine and homoarginine at 11–13 weeks’ gestation and preeclampsia: a case-control study. J Hum Hypertens 27:38–43
Kielstein A, Tsikas D, Galloway GP, Mendelson JE (2007) Asymmetric dimethylarginine (ADMA)—a modulator of nociception in opiate tolerance and addiction? Nitric Oxide 17:55–59
Leiper J, Vallance P (1999) Biological significance of endogenous methylarginines that inhibit nitric oxide synthases. Cardiovasc Res 43:542–548
Levin B, Oberholzer VG, Palmer T (1974) Letter: the high levels of lysine, homocitrulline, and homoarginine found in argininosuccinate synthetase deficiency. Pediatr Res 8:857–858
Lücke T, Tsikas D, Kanzelmeyer N, Vaske B, Das AM (2006) Elevated plasma concentrations of the endogenous nitric oxide synthase inhibitor asymmetric dimethylarginine in citrullinemia. Metabolism 55:1599–1603
MacAllister RJ, Parry H, Kimoto M, Ogawa T, Russell RJ, Hodson H et al (1996) Regulation of nitric oxide synthesis by dimethylarginine dimethylaminohydrolase. Br J Pharmacol 119:1533–1540
Mariotti F, Petzke KJ, Bonnet D, Szezepanski I, Bos C, Huneau JF et al (2013) Kinetics of the utilization of dietary arginine for nitric oxide and urea synthesis: insight into the arginine-nitric oxide metabolic system in humans. Am J Clin Nutr 97:972–979
Martens-Lobenhoffer J, Bode-Böger SM (2012) Quantification of l-arginine, asymmetric dimethylarginine and symmetric dimethylarginine in human plasma: a step improvement in precision by stable isotope dilution mass spectrometry. J Chromatogr B 904:140–143
März W, Meinitzer A, Drechsler C, Pilz S, Krane V, Kleber ME et al (2010) Homoarginine, cardiovascular risk, and mortality. Circulation 122:967–975
McGuire DM, Tormanen CD, Segal IS, Van Pilsum JF (1980) The effect of growth hormone and thyroxine on the amount of l-arginine:glycine amidinotransferase in kidneys of hypophysectomized rats. Purification and some properties of rat kidney transamidinase. J Biol Chem 255:1152–1159
Miller LL, Bale WF, Yuile CL, Masters RE, Tishkoff GH, Whipple GH (1949) The use of radioactive lysine in studies on protein metabolism. Synthesis and utilization of plasma proteins. J Exp Med 90:297–313
Moali C, Boucher JL, Sari MA, Stuehr DJ, Mansuy D (1998) Substrate specificity of NO synthases: detailed comparison of arginine, homo-arginine, their N omega-hydroxy derivatives, and N omega-hydroxynor-arginine. Biochemistry 37:10453–10460
Moncada S, Higgs A (1993) The arginine-nitric oxide pathway. New Engl J Med 329:2002–2012
Ogawa H, Ishiguro Y, Fujioka M (1983) Guanidoacetate methyltransferase from rat liver: purification, properties, and evidence for the involvement of sulfhydryl groups for activity. Arch Biochem Biophys 226:265–275
Pilz S, Tomaschitz A, Meinitzer A, Drechsler C, Ritz E, Krane V, Wanner C, Böhm BO, März W (2011a) Low serum homoarginine is a novel risk factor for fatal strokes in patients undergoing coronary angiography. Stroke 42:1132–1134
Pilz S, Meinitzer A, Tomaschitz A, Drechsler C, Ritz E, Krane V et al (2011b) Low homoarginine concentration is a novel risk factor for heart disease. Heart 97:1127–1222
Pilz S, Teerlink T, Scheffer PG, Meinitzer A, Rutters F, Tomaschitz A, Drechsler C, Kienreich K, Nijpels G, Stehouwer CD, März W, Dekker JM (2014) Homoarginine and mortality in an older population: the Hoorn study. Eur J Clin Invest 44:200–208
Pilz S, Meinitzer A, Gaksch M, Grübler M, Verheyen N, Drechsler C, Hartaigh BÓ, Lang F, Alesutan I, Voelkl J, März W, Tomaschitz A (2015a) Homoarginine in the renal and cardiovascular systems. Amino Acids. doi:10.1007/s00726-015-1993-2
Pilz S, Putz-Bankuti C, Meinitzer A, März W, Kienreich K, Stojakovic T, Pieber TR, Stauber RE (2015b) Association of homoarginine and methylarginines with liver dysfunction and mortality in chronic liver disease. Amino Acids. doi:10.1007/s00726-015-2000-7
Roberts JJ, Walker JB (1985) Higher homolo and N-ethyl analog of creatine as synthetic phosphagen precursors in brain, heart, and muscle, repressors of liver amidinotransferase, and substrates for creatine catabolic enzymes. J Biol Chem 260:13502–13508
Ryan WL, Wells IC (1964) Homocitrulline and homoarginine synthesis from lysine. Science 144:1122–1127
Ryan WL, Barak AJ, Johnson RJ (1968) Lysine, homocitrulline, and homoarginine metabolism by the isolated perfused rat liver. Arch Biochem Biophys 123:294–297
Ryan WL, Johnson RJ, Dimari S (1969) Homoarginine synthesis by rat kidney. Arch Biochem Biophys 131:521–526
Schmidt A, Marescau B, Boehm EA, Renema WK, Peco R, Das A et al (2004) Severely altered guanidino compound levels, disturbed body weight homeostasis and impaired fertility in a mouse model of guanidinoacetate N-methyltransferase (GAMT) deficiency. Hum Mol Genet 13:905–921
Siroen MP, Teerlink T, Nijveldt RJ, Prins HA, Richir MC, van Leeuwen PA (2006) The clinical significance of asymmetric dimethylarginine. Annu Rev Nutr 26:203–228
Takata Y, Date T, Fujioka M (1991) Rat liver guanidinoacetate methyltransferase. Proximity of cysteine residues at positions 15, 90 and 219 as revealed by site-directed mutagenesis and chemical modification. Biochem J 277(Pt 2):399–406
Teerlink T, Luo Z, Palm F, Wilcox CS (2009) Cellular ADMA: regulation and action. Pharmacol Res 60:448–460
Tomaschitz A, Meinitzer A, Pilz S, Rus-Machan J, Genser B, Drechsler C et al (2014) Homoarginine, kidney function and cardiovascular mortality risk. Nephrol Dial Transplant 29:663–671
Tsikas D (2009) De novo synthesis of trideuteromethyl esters of amino acids for use in GC- MS and GC-tandem MS exemplified for ADMA in human plasma and urine: standardization, validation, comparison and proof of evidence for their aptitude as internal standards. J Chromatogr B 877:2308–2320
Tsikas D, Kayacelebi AA (2014) Do homoarginine and asymmetric dimethylarginine act antagonistically in the cardiovascular system? Circ J 78:2092–2093
Tsikas D, Böger RH, Sandmann J, Bode-Böger SM, Frölich JC (2000) Endogenous nitric oxide synthase inhibitors are responsible for the Arginine paradox. FEBS Lett 478:1–3
Tsikas D, Schubert B, Gutzki FM, Sandmann J, Frölich JC (2003) Quantitative determination of circulating and urinary asymmetric dimethylarginine (ADMA) in humans by gas chromatography-tandem mass spectrometry as methyl ester tri(N-pentafluoropropionyl) derivative. J Chromatogr B 798:87–99
Tsikas D, Wolf A, Mitschke A, Gutzki FM, Will W, Bader M (2010) GC–MS determination of creatinine in human biological fluids as pentafluorobenzyl derivative in clinical studies and biomonitoring: inter-laboratory comparison in urine with Jaffé, HPLC and enzymatic assays. J Chromatogr B 878:2582–2592
Tsikas D, Beckmann B, Gutzki FM, Jordan J (2011) Simultaneous gas chromatography-tandem mass spectrometry quantification of symmetric and asymmetric dimethylarginine in human urine. Anal Biochem 413:60–62
Valtonen P, Laitinen T, Lyyra-Laitinen T, Raitakari OT, Juonala M, Viikari JS et al (2008) Serum l-homoarginine concentration is elevated during normal pregnancy and is related to flow-mediated vasodilatation. Circ J 72:1879–1884
van der Zwan LP, Davids M, Scheffer PG, Dekker JM, Stehouver CDA, Teerlink T (2013) l-Homoarginine and arginine are antagonistically related to blood pressure in an elderly population: the Hoorn study. J Hypertens 31:1114–1123
Walker JB, Hannan JK (1976) Creatine biosynthesis during embryonic development. False feedback suppression of liver amidinotransferase by N-acetimidoylsarcosine and 1-carboxymethyl-2-iminoimidazolidine (cyclocreatine). Biochemistry 15:2519–2522
Wu G, Bazer FW, Cudd TA, Jobgen WS, Kim SW, Lassala A, Li P, Matis JH, Meininger CJ, Spencer TE (2007) Pharmacokinetics and safety of arginine supplementation in animals. J Nutr 137(6 Suppl 2):1673S–1680S
Wu G, Bazer FW, Davis TA, Kim SW, Li P, Marc Rhoads J et al (2009) Arginine metabolism and nutrition in growth, health and disease. Amino Acids 37:153–168
Wyss M, Kaddurah-Daouk R (2000) Creatine and creatinine metabolism. Physiol Rev 80:1107–1213
Yang Y, Wu Z, Jia S, Dahanayaka S, Feng S, Meininger CJ, McNeal CJ, Wu G (2015) Safety of long-term dietary supplementation with l-arginine in rats. Amino Acids. doi:10.1007/s00726-015-1992-3
Yin J, Ren W, Hou Y, Wu M, Xiao H, Duan J, Zhao Y, Li T, Yin Y, Wu G, Nyachoti CM (2015) Use of homoarginine for measuring true ileal digestibility of amino acids in food protein. Amino Acids. doi:10.1007/s00726-015-1958-5
Yuile CL, Lampson BG, Miller LL, Whipple GH (1951) Conversion of plasma protein to tissue protein without evidence of protein breakdown; results of giving plasma protein labeled with carbon 14 parenterally to dogs. J Exp Med 93:539–557
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical statement
All studies reported here were approved by the local Ethics Committees for animals and humans. All adult participants and the parents of the children gave their written informed consent prior to enrolment.
Author information
Authors and Affiliations
Corresponding author
Additional information
A. A. Kayacelebi and J. Langen contributed equally to this work.
T. Lücke and D. Tsikas are joint senior authors.
Rights and permissions
About this article
Cite this article
Kayacelebi, A.A., Langen, J., Weigt-Usinger, K. et al. Biosynthesis of homoarginine (hArg) and asymmetric dimethylarginine (ADMA) from acutely and chronically administered free l-arginine in humans. Amino Acids 47, 1893–1908 (2015). https://doi.org/10.1007/s00726-015-2012-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00726-015-2012-3