Abstract
Autonomic dysfunction in multiple system atrophy (MSA) comprises cardinal symptoms of orthostatic hypotension (OH) and urinary incontinence. Additionally, cardiovagal and sudomotor abnormalities can be present. Previous studies compared hand skin temperature and its response to cooling in subjects with probable MSA and Parkinson’s disease (PD). Significant differences were found indicating that disturbed thermoregulation belongs to MSA autonomic features and could be helpful in differentiation of MSA from PD. The objective of this study was to improve our knowledge about impaired thermoregulation of distal extremities in MSA with parkinsonian features (MSA-P) and PD and to assess the possible interrelations for the different subtypes of autonomic dysfunction in a large cohort of MSA-P, PD and control patients. The patients underwent a standard cooling—rewarming procedure, termed ice test (IT). Electroneurography, heart rate variability, sympathetic skin response and orthostatic tests were performed for the subdivision of the patients. The prevalence of pathological IT was slightly increased in MSA compared with PD and control groups. The presence of pathological IT was related with older patient’s age in PD and control groups significantly (p < 0.05). This relation was absent for the MSA patients, who themselves were significantly younger (p = 0.001). Significant association between the presence of pathological IT and OH was determined (p < 0.001). Defective thermoregulation of distal extremities seems to be more severe in the MSA patients. The dysfunction of preganglionic sympathetic neurons might be involved in impaired response to cooling for MSA. The results suggest pathophysiological affinity of impaired sympathetic neurovascular regulation between pathological IT and OH.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Multiple system atrophy (MSA) is a sporadic, adult-onset and relatively rapidly progressive neurodegenerative disorder. Disease onset occurs most often in the sixth decade of life. Both genders are generally equally affected. Clinically MSA is characterized by prominent autonomic dysfunction with combinations of parkinsonian features (MSA-P), cerebellar ataxia (MSA-C) and possible corticospinal symptoms (Fanciulli and Wenning 2015).
Autonomic dysfunction in MSA comprises mainly orthostatic hypotension (OH) and urinary incontinence or incomplete bladder emptying. Additionally, sudomotor and cardiovagal abnormalities are frequently present among the MSA patients (Fanciulli and Wenning 2015; Iodice et al. 2012). As reported in previous publications, disturbed neurovascular thermoregulation of distal extremities potentially belongs to MSA autonomic features as well (Klein et al. 1997; Pietzarka et al. 2010). It could be helpful in clinical differentiation of MSA from Parkinson’s disease (PD), while the presence of OH alone or combined with urinary incontinence does not distinguish MSA from PD with certainty (Jost and Augustis 2015; Jost 2013).
Previous studies compared hand skin temperature and its response to cooling in subjects with PD and probable MSA-P. Significant differences regarding hand temperature before and after cooling, as well as kinetics of natural rewarming were found (Klein et al. 1997; Pietzarka et al. 2010). To date only a minor study sample has been reported. The prevalence of disturbed neurovascular thermoregulation in sizeable patient cohorts and thereby its value for differential diagnosis of MSA-P and PD remains obscure.
The methodology for testing hand skin temperature and its response to cooling has been established in some specialized medical centers and routinely used examining patients with parkinsonian syndromes. Here we report the results of a retrospective study on PD and MSA-P patients from a specialized neurological department. The objective of this study was to improve our knowledge about impaired thermoregulation of distal extremities in patients suffering from MSA-P and PD. Moreover, we sought to assess the possible interrelations for the different subtypes of autonomic dysfunction in a large cohort of MSA-P, PD and control patients.
Patients
A retrospective study was conducted on the patients from a specialized neurological department, recruited from August, 1997 until July, 2015. Study cohort comprises 577 patients diagnosed with PD according to the UK PD Society Brain Bank diagnostic criteria (PD group) (Hughes et al. 1992) and 130 probable MSA-P patients (MSA group) (Gilman et al. 2008). Further, 150 patients having insufficient clinical evidence of a possible α-synucleinopathy were recruited to form a control group. The complaints of the controls after a thorough clinical assessment were addressed to a cerebrovascular disease, neurological complications of diabetes or functional disorders. In the follow-up the controls developed no signs of a neurodegenerative disease. Demographical and anamnestic data of the patients are presented in Table 1. Over the course of the follow-up in the study groups the overlapping of parkinsonian syndromes could be largely excluded. This study was carried out in accordance with the approved guidelines of the university research ethics committee.
Methods
All patients underwent a standard cooling—rewarming procedure, termed ice test (IT). Hand skin temperature was initially measured at rest with a digital thermometer (Quigg TS 402) adhered to the palmar surface of the third finger in patient’s left hand. Then the hand was cooled between two standardly prepared ice packs for 5 min. Directly after removal from the ice packs, hand temperature was measured again and the hand was left over to rewarm naturally. The measurements were repeated consequently on the 7th, 9th, 11th, 13th and 15th min of the IT. All the measurements were performed in a specialized room with controlled temperature (20 °C) and neutral humidity. Patients were tested in the morning while they were fasting and had not taken their morning medications.
Some percentage of the patients did not tolerate IT because of painful, unpleasant sensations related to cooling. In such a case the IT was discontinued and the subject was excluded from the successive analysis (Table 2).
Once the hand temperature at the end of 15-min IT was lower than the initial temperature at rest, IT was stated to be pathological in terms of defective neurovascular regulation. As a result temperature decrement (initial minus endpoint temperature) was noted. Time to complete rewarming was noted for the patients who after the cooling recovered back to the initial hand temperature earlier than the end of the IT. Considering kinetics of natural rewarming temperature increment rate (endpoint temperature minus temperature directly after the cooling per time to complete rewarming) was calculated (Table 2).
Furthermore, the subdivision of the patients received peripheral and autonomic nervous systems clinically evaluated (Table 3). The evaluation included autonomic function tests of heart rate variability and sympathetic skin response (SSR). SSR was elicited by electrical stimulation of the median nerve and simultaneously recorded on the palm, corresponding to the previously described methodology (De Marinis et al. 2000). To evaluate orthostasis, lying-to-standing orthostatic test was performed according to the international consensus on the definition and diagnosis of OH (Freeman et al. 2011). Electroneurography was deployed in detection of axonal peripheral neuropathy (Cossu and Melis 2016).
Statistical analysis
Statistical analyses were performed using the statistical software IBM SPPS Statistics 23 (IBM Corp. Software, Armonk, NY). Data are presented as Mean (M) ± Standard Deviation (SD).
After testing for normality continuous variables were compared with the Student’s t test and ANOVA for independent or related groups. For the skewed data nonparametric criteria including Mann–Whitney U test, Kruskal–Wallis 1-way ANOVA or Friedman’s test were used when appropriate to compare quantitative samples.
The correlations or associations among the investigated parameters were evaluated by using Pearson’s correlation coefficient (r) or Contingency coefficient. To test hypotheses about independence the Chi-square testing was applied. For pairwise comparison of proportions z test was used. The level of statistical significance was set to 0.05.
Results
The mean age of the MSA patients was 67.07 ± 7.78 years (Mean ± standard deviation). The patients in the MSA study group were significantly younger (p = 0.001) than the PD and the control group patients (70.37 ± 8.97 and 74.84 ± 6.92 years, respectively). The MSA patients had higher Unified Parkinson’s Disease Rating Scale (UPDRS) motor and total scores than the PD patients (p < 0.001). The medical history of arterial hypertension, diabetes and hypothyrosis were similarly common in the MSA and the PD study groups (Table 1).
In the PD group the history of L-dopa medication was available for 275 patients. 28 out of 275 patients did not receive L-dopa, for the rest the mean L-dopa daily dosage was 463.25 ± 184.20 mg. Similarly, the history of L-dopa medication was available for 88 MSA patients. 9 patients received no L-dopa, for the rest 79 patients the mean L-dopa daily dosage was 651.66 ± 293.61 mg (p < 0.001). Principally used dopamine agonists in the MSA and the PD study groups are presented in Table 1.
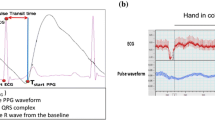
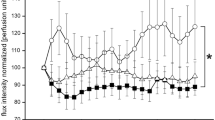
In MSA, PD and control study groups the hand skin temperatures measured at rest (30.75 ± 3.35; 30.11 ± 3.09 and 30.59 ± 3.13 °C, respectively, p = 0.072), immediately after the cooling (13.87 ± 7.64; 13.86 ± 6.66 and 13.96 ± 7.18 °C, respectively, p = 0.99) and subsequently at each measurement during natural rewarming did not differ significantly (Table 4; Fig. 1a).
Despite the absence of consistent group difference, to evaluate the kinetics of cooling and rewarming accurately, hand temperature at each measurement of the IT was expressed as the percentage of initial resting hand temperature. The percentage values at each point after the cooling were consistently, but not significantly lower in the MSA group (Table 4; Fig. 1b).
The prevalence of pathological IT was higher in the MSA than in the PD and the control groups (58.93; 52.0 and 56.59%, respectively), the difference, however, was not statistically significant. There was no statistically significant relation between the study group (MSA, PD and controls) and IT result (normal or pathological) determined (p = 0.33).
Patients in the MSA study group were significantly younger than the PD patients and the controls. To alleviate the possible influence of age, we have arranged all the study patients into three preset age-layers of younger than 65; 65–75; and older than 75 years of age. Further, we have compared the prevalence of pathological IT between the three study groups in the each age-layer separately and found no significant relation for the study group and IT result (p = 0.21; 0.14 and 0.32, respectively).
In the study cohort the patients having a pathological IT had a significantly lower hand temperature already before the cooling compared to the patients with a non-pathological IT (29.92 ± 3.26 and 30.73 ± 2.90 °C, respectively, p < 0.001).
Hypothesizing that potentially the pathological IT gains more specificity in the differentiation of MSA versus PD along with the increasing temperature decrement, the frequencies of temperature decrement ≥1, 2, …, 11 °C in the three study groups were estimated. The frequencies of gradually increasing temperature decrement were consistently higher in the MSA group, the differences remained not sufficient for a statistical significance (Table 2). The greatest temperature decrement observed in the study cohort was 17.4 °C (the PD group).
Defective thermal regulation of distal extremities could possibly occur due to conditions such as hypothyrosis, known peripheral neuropathy, diabetes and microangiopathy, which are merely associated with autonomic dysfunction (Klein et al. 1997; Pietzarka et al. 2010). To avoid this potential confusion we have re-evaluated the prevalence of pathological IT excluding the patients with hypothyrosis and diabetes in their medical history or with detected peripheral neuropathy. Still, the results remained similar, there was no statistically significant difference for the prevalence of pathological IT in the three study groups observed (p = 0.52).
Neither the presence of pathological IT, nor the temperature decrement in case of pathological IT were associated with the L-dopa daily dosage or the principally used dopamine agonist in the MSA and the PD study groups.
In the PD group the presence of pathological IT was related with older patient’s age (p < 0.001), older age at onset of disease (p < 0.001), higher UPDRS motor (p = 0.007) and total scores (p = 0.002). Interestingly, there was no such a relation in the MSA group observed. In the control group the presence of pathological IT was related to patient’s age in a statistically significant manner (p = 0.034).
A significant association for the presence of pathologic IT and suppressed SSR in the study cohort was determined (p = 0.003). The rate of suppressed SSR itself was significantly higher in the MSA group compared to the PD and the control groups (80.00; 65.75 and 62.96%, respectively, p = 0.04) (Table 3).
There was no statistically significant relation between the pathological IT and the history of arterial hypertension, diabetes, hypothyrosis or detected peripheral neuropathy neither in the three study groups separately, nor in the study cohort observed. An association for the pathological IT and patient’s gender could not be determined.
In the study cohort we observed a significant association between the presences of pathological IT and the symptom of orthostatic hypotension (p < 0.001). The association remained statistically significant in the PD study group (p < 0.01). To evaluate the influence of possible confounders (patient’s age, age at onset of disease, disease duration, UPDRS motor and total scores, history of arterial hypertension, hypothyrosis, diabetes and detected peripheral neuropathy) we performed multivariate logistic regression analysis. These confounders were determined having no significant influence (p > 0.05).
In case of pathologic IT and a drop of systolic blood pressure after active standing in orthostatic test there was no statistically significant correlation for the temperature decrement and the maximal drop of systolic blood pressure determined (p = 0.27).
The symptom of OH was significantly more prevalent in the MSA than in the PD and the control groups (66.67, 32.76 and 26.68%, respectively, p = 0.015). Male patients suffered from OH more often than female patients (p = 0.001). The symptom of OH was not related with the history of arterial hypertension, diabetes, hypothyrosis as well as with the detected peripheral neuropathy, reduced heart rate variability and suppressed SSR in a statistically significant manner. Neither the OH itself, nor the maximal drop of systolic blood pressure after active standing were associated with the L-dopa daily dosage nor with the principally used dopamine agonist in the MSA and the PD study groups.
In the MSA group the higher drop of systolic blood pressure after active standing tended to correlate with older patient’s age (p = 0.051, r = 0.48) and correlated with older age at onset of disease significantly (p = 0.029, r = 0.53). For the PD patients suffering from OH this correlation however could not be determined.
In the MSA and the PD groups the presence of suppressed SSR was associated with the detected peripheral axonal neuropathy significantly (p = 0.044 and 0.018, respectively). Such a correlation however was absent in the control study group.
The prevalence of reduced heart rate variability was higher in the MSA than in the PD and the control groups, but did not differ significantly (90.54; 85.48 and 76.67%, respectively, p > 0.05) (Table 3).
Discussion
MSA together with PD, Lewy body dementia and pure autonomic failure forms a group of neurodegenerative disorders—the α-synucleinopathies, characterized by the abnormal accumulation of misfolded α-synuclein. A definitive diagnosis of MSA requires the neuropathological findings of widespread α-synuclein positive glial cytoplasmic inclusions associated with neurodegenerative changes in striatonigral or olivopontocerebellar structures (Trojanowski and Revesz 2007). Furthermore, neurodegenerative changes affect the central autonomic nervous system, including the hypothalamus, brainstem nuclei, dorsal nucleus of the vagus nerve, nucleus ambiguus, Onuf nucleus and sympathetic preganglionic neurons in the intermediolateral column of thoracolumbar spinal cord (Fanciulli and Wenning 2015; Jellinger and Wenning 2016; Wenning et al. 2012; Lipp et al. 2009a). Whereas in PD autonomic dysfunction seems to be caused by the postganglionic lesion (Lipp et al. 2009a, b).
MSA has been determined by degeneration in central nervous system, recent research however found phospho-α-synuclein deposition in cutaneous small fiber nerves in patients with MSA indicating a peripheral component of this disorder (Doppler et al. 2015).
Due to overlapping motor presentations it can be very challenging to distinguish MSA from PD. The cardinal MSA autonomic symptoms—OH and urinary incontinence—are of limited assistance while these symptoms are common among the PD patients as well (Koga et al. 2015). Neuroimaging modalities, like myocardial 123I-metaiodobenzylguanidin scintigraphy, do not always provide a certain differentiation between these two diseases (Chung et al. 2009; Jost et al. 2010; Kimpinski et al. 2012).
Nevertheless, previous studies have showed, that particularly for the MSA patients impaired autonomic regulation extends over many different autonomic domains. The severity of autonomic dysfunction is substantially more devastating in patients with MSA (Iodice et al. 2012; Lipp et al. 2009a). Probably there is no single autonomic test having sufficient reliability to differentiate MSA and PD (Kimpinski et al. 2012), still the search of new methodology in autonomic testing remains of great importance, while widespread and well documented dysautonomia should increase specificity in this distinction. In the sudomotor autonomic domain thermoregulatory sweat test has been already reported providing some significant differentiation between MSA and PD (Kimpinski et al. 2012).
Our results reveal the disturbed neurovascular thermoregulation of distal extremities as shown by the pathological IT to be highly prevalent for the MSA and the PD patients. The prevalence of pathological IT was slightly increased in the MSA group compared with the PD and the control groups. The frequencies of gradually increasing temperature decrement were consistently higher in the MSA group. The mean temperature decrement in pathological IT was also higher for the MSA patients, although there were no statistically significant differences observed. This study shows that despite the substantial overlap the autonomic feature of defective thermoregulation is more severe in the MSA patients. The underlying pathophysiology remains rather incompletely understood.
Our results however disagree with the previously published study (Klein et al. 1997), which observed significantly lower initial hand skin temperature, greater reduction of hand temperature after cooling and significantly prolonged rewarming for the MSA patients compared with the PD patients and the controls. The previous study reported only a minor study sample though.
Having in mind the observed pattern of natural rewarming (Fig. 1a, b), which was quite similar in the three study groups during 10 min after the cooling, extending temperature observation should be considered to increase the specificity of pathological IT. To unify the conditions in the three study groups, the IT was performed on the left hand for all the patients. In patients with motor asymmetry the association between the presence of pathological IT and more affected side seems to be probable and should be further investigated to get more insight into the pathology causing impaired thermoregulation. Furthermore, a considerable percentage of the patients did not tolerate IT because of painful, unpleasant sensations related to cooling. It could be beneficial to quantify the patients’ painful sensations experienced in the course of the IT using, for example, the Numeric Pain Rating Scale (Taylor et al. 2005).
The presence of pathological IT was significantly associated with older patient’s age in the PD and the control study groups. This was not the case for the MSA patients, who themselves were significantly younger than the patients of the PD and the control groups. Defective thermoregulation appears to be an intrinsic factor to MSA. Furthermore it should be considered in aging patients with PD and in aging population comprehensively.
In the study cohort pathologic IT was significantly associated with the suppressed SSR. It is reported that SSR to electric stimulation are mediated through the efferent pathway consisting of preganglionic and postganglionic sympathetic neurons. The amplitudes of responses are suppressed or responses could be even absent when disturbance in efferent pathway occurs (Haapaniemi et al. 2000; Shahani et al. 1990). Having regard to the results of our study, preganglionic sympathetic neurons might be involved in the pathological mechanisms responsible for impaired response to cooling in MSA.
This is the first study to determine a significant association between the presence of pathological IT and the symptom of OH. The results suggest a pathophysiological affinity between these two types of autonomic dysfunction, which again could be a defective sympathetic neurovascular regulation. We did not find any other numeric values of temperature decrement in pathological IT and maximal drop of systolic blood pressure after active standing from supine position, therewith these two pathophysiologically related symptoms could correlate each other stronger than with the contemporary consensus values of temperature decrement ≥0 °C and drop of systolic blood pressure ≥20 mmHg.
The severity of OH expressed in maximal drop of systolic blood pressure tended to correlate with older patient’s age and correlated with older age at onset of disease significantly in the MSA group. In compliance with the recent publications for the PD patients suffering from OH this correlation could not be determined (Jost and Augustis 2015; Sun et al. 2016).
OH and suppressed SSR were significantly more prevalent in the MSA group. Abnormalities in different domains of autonomic regulation, like pathologic IT and reduced heart rate variability, were more common among the MSA patients than in the PD and the control study groups, thus adding more evidence on the multisystemic nature of underlying neuropathology.
This retrospective study however suffers from some limitations, which should be addressed. First of all, the definite diagnosis of MSA requires characteristic autopsy findings (Fanciulli and Wenning 2015). The postmortem analysis was not possible in the settings of our study, therefore we used published diagnostic criteria of probable MSA (Gilman et al. 2008). In the present retrospective study we have often had to rely on patients records, which unfortunately had no data on the rates of smokers in the study groups. Though we have analyzed the role of some co-morbidities influencing autonomic regulation, like arterial hypertension and medication with beta-adrenoceptor blockers or hypothyrosis, the data regarding psychiatric medication with tricyclic antidepressants and noradrenaline reuptake inhibitors was unavailable for analysis. Patients in the MSA study group were significantly younger than the PD patients and the controls. We have tried to alleviate the possible influence of age to the comparison of the study groups by analyzing the prevalence of pathological IT in the preset age-layers. However, younger age and more rapid deterioration constitute some particular features for the MSA.
To sum up, the abnormal IT provides supplementary information on the extent of autonomic failure. Widespread and well documented dysautonomia should increase specificity in the distinction of MSA-P and PD. Accurate antemortem diagnosis of MSA is of great importance in defining patient’s prognosis or enrolling in particular clinical trials.
References
Chung EJ, Lee WY, Yoon WT, Kim BJ, Lee GH (2009) MIBG scintigraphy for differentiating Parkinson’s disease with autonomic dysfunction from Parkinsonism-predominant multiple system atrophy. Mov Disord 24(11):1650–1655
Cossu G, Melis M (2016) The peripheral nerve involvement in Parkinson Disease: a multifaceted phenomenon. Parkinsonism Relat Disord 25:17–20
De Marinis M, Stocchi F, Gregori B, Accornero N (2000) Sympathetic skin response and cardiovascular autonomic function tests in Parkinson’s disease and multiple system atrophy with autonomic failure. Mov Disord 15(6):1215–1220
Doppler K, Weis J, Karl K, Ebert S, Ebentheuer J, Trenkwalder C, Klebe S, Volkmann J, Sommer C (2015) Distinctive distribution of misfolded alpha-synuclein in dermal nerves in multiple system atrophy. Mov Disord 30(12):1688–1692
Fanciulli A, Wenning GK (2015) Multiple-system atrophy. N Engl J Med 372(14):1375–1376
Freeman R, Wieling W, Axelrod FB et al (2011) Consensus statement on the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci 161(1–2):46–48
Gilman S, Wenning GK, Low PA et al (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology 71(9):670–676
Haapaniemi TH, Korpelainen JT, Tolonen U, Suominen K, Sotaniemi KA, Myllylä VV (2000) Suppressed sympathetic skin response in Parkinson disease. Clin Auton Res 10(6):337–342
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of the clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Iodice V, Lipp A, Ahlskog JE et al (2012) Autopsy confirmed multiple system atrophy cases: Mayo experience and role of autonomic function tests. J Neurol Neurosurg Psychiatry 83(4):453–459
Jellinger KA, Wenning GK (2016) Multiple system atrophy: pathogenic mechanisms and biomarkers. J Neural Transm (Vienna) 123(6):555–572
Jost WH (2013) Urological problems in Parkinson’s disease: clinical aspects. J Neural Transm (Vienna) 120(4):587–591
Jost WH, Augustis S (2015) Severity of orthostatic hypotension in the course of Parkinson’s disease: no correlation with the duration of the disease. Parkinsonism Relat Disord 21(3):314–316
Jost WH, Del Tredici K, Landvogt C, Braune S (2010) Importance of 123I-metaiodobenzylguanidin (MIBG) scintigraphy/SPECT for diagnosis and deferential diagnostics of Parkinson syndromes. Neurodegener Dis 7:341–347
Kimpinski K, Iodice V, Burton DD, Camilleri M, Mullan BP, Lipp A, Sandroni P, Gehrking TL, Sletten DM, Ahlskog JE, Fealey RD, Singer W, Low PA (2012) The role of autonomic testing in the differentiation of Parkinson’s disease from multiple system atrophy. J Neurol Sci 317(1–2):92–96
Klein C, Brown R, Wenning G, Quinn N (1997) The “cold hands sign” in multiple system atrophy. Mov Disord 12(4):514–518
Koga S, Aoki N, Uitti RJ et al (2015) When DLB, PD, and PSP masquerade as MSA: an autopsy study of 134 patients. Neurology 85(5):404–412
Lipp A, Sandroni P, Ahlskog JE, Fealey RD, Kimpinski K, Iodice V, Gehrking TL, Weigand SD, Sletten DM, Gehrking JA, Nickander KK, Singer W, Maraganore DM, Gilman S, Wenning GK, Shults CW, Low PA (2009a) Prospective differentiation of multiple system atrophy from Parkinson disease, with and without autonomic failure. Arch Neurol 66(6):742–750. doi:10.1001/archneurol.2009.71
Lipp A, Sandroni P, Low PA (2009b) Systemic postganglionic adrenergic studies do not distinguish Parkinson’s disease from multiple system atrophy. J Neurol Sci 281(1–2):15–19. doi:10.1016/j.jns.2009.03.006
Pietzarka K, Reimann M, Schmidt C et al (2010) The cold hand sign in multiple system atrophy: skin perfusion revisited. J Neural Transm (Vienna) 117(4):475–479
Shahani BT, Day TJ, Cros D, Khalil N, Kneebone CS (1990) RR interval variation and the sympathetic skin response in the assessment of autonomic function in peripheral neuropathy. Arch Neurol 47(6):659–664
Sun Z, Jia D, Shi Y et al (2016) Prediction of orthostatic hypotension in multiple system atrophy and Parkinson disease. Sci Rep 6:2164–2169
Taylor LJ, Harris J, Epps CD, Herr K (2005) Psychometric evaluation of selected pain intensity scales for use with cognitively impaired and cognitively intact older adults. Rehabil Nurs 30(2):55–61
Trojanowski JQ, Revesz T (2007) Proposed neuropathological criteria for the post mortem diagnosis of multiple system atrophy. Neuropathol Appl Neurobiol 33:615–620
Wenning GK, Granata R, Krismer F et al (2012) Orthostatic hypotension is differentially associated with the cerebellar versus the parkinsonian variant of multiple system atrophy: a comparative study. Cerebellum 11(1):223–226
Acknowledgements
We thank Ms. Tanja Fiesel for a kind assistance in the collection of data.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
This is a retrospective study; for this type of study, formal consent is not required.
Rights and permissions
About this article
Cite this article
Augustis, S., Saferis, V. & Jost, W.H. Autonomic disturbances including impaired hand thermoregulation in multiple system atrophy and Parkinson’s disease. J Neural Transm 124, 965–972 (2017). https://doi.org/10.1007/s00702-016-1665-8
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-016-1665-8