Abstract
Objective
Orthostatic hypotension (OH) is common in Parkinson disease (PD) and multiple system atrophy of parkinsonian type (MSA-P), but the pathophysiology of OH is different in the two. We hypothesised that the baroreflex-independent sympathetic reactivity may also be different in them. To evaluate this we assessed the sympathetic vascular reactivity and the heart rate response to the standard cold pressor test (CPT) in these patients.
Methods
The study was conducted in ten patients with PD with OH, 5 PD without OH, 13 MSA-P with OH, and 7 MSA-P without OH. Lead II ECG and finger PPG (photoplethysmography) were simultaneously acquired during a baseline period of 1 min followed by a 10 °C cold exposure (1 min) of the contralateral hand (CPT). The vascular response was then evaluated by computing the pulse transit time (PTT).
Results
The percentage decrease in PTT during the CPT was significantly higher in patients with PD as compared to MSA-P, irrespective of the presence or absence of OH (−2.74 ± 0.96 vs −0.05 ± 0.75 %, p = 0.03; PD vs MSA-P with OH and −3.04 ± 0.85 vs 0.48 ± 1.13 %, p = 0.04; PD vs MSA-P without OH). The rise in heart rate during CPT was similar in patients with PD and MSA-P with or without OH (4.95 ± 1.6 vs 5.99 ± 1.04, p = 0.28; PD vs MSA-P with OH and 5.62 ± 1.31 vs 13.15 ± 2.89, p = 0.06; PD vs MSA-P without OH).
Interpretation
Vasoconstrictor response to CPT is compromised in MSA-P as compared to PD, but the baroreflex-independent heart rate response is similar in the two.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Autonomic dysfunction is common in patients with parkinsonian syndromes [1]. Orthostatic hypotension (OH) being a cardinal feature of autonomic failure fails to differentiate between them [2]. However, the pathophysiology of OH in Parkinson disease (PD) and multiple system atrophy of parkinsonian type (MSA-P) has been suggested to be of different origins. Central lesions in the upper brainstem in association with cardiac denervation in PD [3] and central lesions of the upper brainstem only in MSA-P have been suggested to be the cause of dysautonomia-related orthostatic hypotension. We hypothesised that the baroreflex-independent sympathetic reactivity could also be different in them. To evaluate this, we assessed the change in pulse transit time as a measure of the sympathetic vasoconstrictor response and the heart rate response to moderate cold exposure in patients with PD and MSA-P.
Method
Patients with PD diagnosed under the UKBB criteria [4] and multiple system atrophy of the MSA-P under the Second Consensus Criteria 2008 [5] were recruited from the Neurology Outpatient Department of All India Institute of Medical Sciences (AIIMS), New Delhi, India. Only male patients of the age group 50 ± 10 years were included in the study. Patients with PD with severity by Hoehn and Yahr scale of IV and V and MSA-C diagnosed under the Second Consensus Criteria 2008 [5] were excluded from the study. Special care was taken to select patients without other co-morbidities such as hypertension, diabetic neuropathy, and any vascular disorders (Table 1).
The study was conducted on 35 patients with Parkinson disease (10 patients with PD with OH, 5 PD without OH, 13 MSA-P with OH, and 7 MSA-P without OH) from April 2012 to August 2013. The diagnosis of OH was done by a 5 min head-up tilt test. The American Autonomic Society (AAS) and the American Academy of Neurology (AAN) define OH as a systolic blood pressure decrease of at least 20 mmHg or a diastolic blood pressure decrease of at least 10 mmHg within 3 min of standing up [6]. Subjects were included in the study only after written consent. All subjects were asked to refrain from exercise, alcohol, caffeine, and nicotine for at least 4 h prior to the tests.
Recording
Subjects were made to rest for 15 min. Lead II ECG and finger PPG (photoplethysmogram) were simultaneously acquired until a stable baseline was obtained. Stability was assessed by the visual inspection of the records. The stable baseline was recorded for 1 min followed by the immersion of the contralateral hand in cold water of 10 °C for 1 min. Lead II ECG and PPG were continuously recorded during the complete procedure. The vascular response was evaluated by computing the pulse transit time (PTT) from the acquired ECG and PPG pulse waveforms.
Pulse transit time
Pulse transit time is the time interval between each R wave peak and the foot (defined as the point at which signal voltage is 10 % above the preceding baseline value) of the corresponding PPG pulse waveform.
Procedure of signal analysis and extraction of parameters
Identification of the R wave peak was done using the peak detection module of Labchart pro 7® software and selecting the peak detection algorithm for analyzing a human ECG. Appropriate threshold was set for peak detection, so that all the R wave peaks were properly detected on manual verification. Identification of the peaks and valleys of the PPG pulse waveform signal was done using the peak detection module of Labchart pro 7® software and selecting the peak detection algorithm for analyzing the cardiovascular finger pulse. Appropriate thresholds were set for peak detection of pulse waveforms so that all the systolic peaks were properly detected, which was subsequently verified by manual screening of the data. Fig. 1a shows a segment of recorded data comprising ECG and PPG signals with their peaks detected from beat to beat.
Baseline drifts were observed during all recordings of PPG. No attempt was made to correct the baseline drift using filters, etc., to avoid the influence of filtering per se on the amplitude component of the waveform. The foot point (start of the wave) was identified following the criteria that were built-in features of Labchart pro 7® software (AD instruments): T start is 5 % of the height away from the baseline sampling rate of 1 kHz.
After completing the identification of the signal waveform features, all the required parameters were extracted beat to beat in Microsoft excel format for further plotting and analysis. Pulse transit time was calculated using the extracted time parameters by applying the following formula as a math function in Excel: Pulse transit time = time point of the foot of pulse wave − (time point of the base of the corresponding R wave peak + time to the peak of R wave from R wave base).
Pulse transit time was calculated from the pulse waveform recorded prior to (PTTo) and during immersion of the hand in cold water (PTTf) for 1 min. The delta change in PTT (∆PTTCPT) is calculated from the difference between PTTo and PTTf:
The delta change is PTT is expressed as a percentage decrease from the baseline values:
Delta change in the heart rate (∆HCPT) was calculated from the ECG recordings before and during CPT. Analysis was done by Labchart pro 7® software. Average heart rate during 1 min of rest (H o) and maximum heart rate during CPT (H max) were calculated from the recorded ECG. Delta change in the heart rate was calculated from the difference:
Precautions
Continuous monitoring of the subjects prevented development of pain and/or hyperventilation. The procedure was stopped on any complaint of pain or discomfort and data were not recorded. This was done to avoid patient discomfort as well as to prevent pain or hyperventilation from becoming a confounder in the data being recorded. Continuous monitoring of the pulse waveform for assessing the change in respiratory rate was done to prevent the effect of hyperventilation on the vascular and respiratory responses. Hyperventilation usually occurs after 1 h of cold exposure [7].
Statistical analysis
Each parameter was tested for distribution of the data based on standard normality tests (D’ Agostino–Pearson omnibus normality test and Shapiro–Wilk test). Where the data distribution was “Gaussian”, parametric tests were applied and, for non-Gaussian distribution, appropriate nonparametric tests were applied. The following tests were used: independent t test and Mann–Whitney test as appropriate for the analysis of the data. The level of statistical significance was set at p < 0.05. All statistical analyses were performed using GraphPad Prism version 5.00 for Windows (GraphPad Software, Inc., USA).
Results
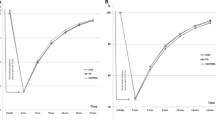
Decrease in PTT (vasoconstriction) during CPT was obtained in PD, but not in MSA-P
In patients with PD, the decrease in the pulse transit time during cold immersion was significantly greater than that of patients with MSA-P, irrespective of the presence or absence of OH (−2.85 ± 0.66 vs 0.13 ± 0.61 %, p = 0.002) as shown in Fig. 2a. The percentage fall in PTT during CPT in patients with PD with OH was significantly higher than in MSA-P with OH (−2.74 ± 0.96 vs −0.05 ± 0.75 %, p = 0.03) as shown in Fig. 2b, and in PD without OH was significantly higher than in MSA-P without OH (−3.04 ± 0.85 vs 0.48 ± 1.13 %, p = 0.04) as shown in Fig. 2c.
a The percentage fall in PTT during CPT in patients with PD was significantly higher than in MSA-P (−2.85 ± 0.66 vs 0.13 ± 0.61 %, p = 0.002). b The percentage fall in PTT during CPT in patients with PD with OH was significantly higher than in MSA-P with OH (−2.74 ± 0.96 vs −0.05 ± 0.75 %, p = 0.03). c The percentage fall in CPT in patients with PD without OH was significantly higher than in MSA-P without OH (−3.04 ± 0.85 vs 0.48 ± 1.13 %, p = 0.04)
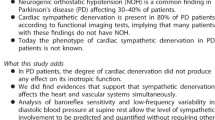
Heart rate rise during CPT was similar in PD and MSA-P
The rise in heart rate during moderate cold exposure was similar in Parkinson disease and MSA-P (4.65 ± 1.68 vs 5.99 ± 1.046 bpm, p = 0.28) as shown in Fig. 3a. In patients with OH, the result was similar (4.95 ± 1.6 vs 5.99 ± 1.04 bpm, p = 0.28) as shown in Fig. 3b, but in those without OH the rise in heart rate showed an increasing trend in MSA-P when compared to patients with Parkinson disease (5.62 ± 1.31 vs 13.15 ± 2.89 bpm, p = 0.06) as shown in Fig. 3c. The rise in heart rate in patients with MSA-P without OH was significantly higher than patients with MSA-P with OH (13.15 ± 2.89 vs 5.99 ± 1.04 bpm, p = 0.01) as shown in Fig. 3d.
a The rise in heart rate during CPT was similar in patients with PD and MSA-P (4.65 ± 1.68 vs 5.99 ± 1.046 bpm, p = 0.28). b The rise in heart rate during CPT was similar in patients with PD with OH and MSA-P with OH (4.95 ± 1.6 vs 5.99 ± 1.04 bpm, p = 0.28); c in PD and MSA-P without OH (5.62 ± 1.31 vs 13.15 ± 2.89 bpm, p = 0.06). d Rise in heart rate in patients with MSA-P without OH was significantly higher than in patients with MSA-P with OH (13.15 ± 2.89 vs 5.99 ± 1.04 bpm, p = 0.01)
Discussion
Exposure to a temperature of 10 °C for a short duration elicits cardiovascular responses independent of the baroreflex pathway. It has been postulated that acute cold exposure evokes marked vasoconstriction [8, 9] and increase in heart rate [10]. A temperature below 10° renders the cold receptors inactive [11]. Cardiovascular responses at still lower temperatures are elicited due to pain rather than cold.
In this study, the baroreflex independently sympathetically mediated vasoconstrictor response in patients with PD, and multiple system atrophy of MSA-P was assessed by comparing the pulse transit time before and during a cold pressor test (CPT). Pulse transit time (PTT) is the time interval between the R-peak of the ECG and the arrival of the pulse wave at the finger. Thus, all the components of the arterial tree contribute to this transit time. The arterial stiffness is not uniform throughout the path of the pulse wave; thus, no global measurement will be able to differentiate between regional arterial stiffness and the pulse wave velocities. These issues assume more importance when single time measurements are made and form the basis of comparison between individuals on the absolute values obtained. In the present study, the change in the pulse transit time during the hand immersion in cold water was done in the same person.
The pulse waveform was recorded by means of a finger photoplethysmograph (PPG). Recording beat-to-beat blood pressure along with the photoplethysmogram would have been a better option for interpreting the results, but since one hand of the subject was immersed in cold water, the option was to use the other hand for PPG along with beat-to-beat blood pressure monitoring on different fingers of the same hand. The choice was made for PPG for the convenience of the patient and issues with beat-to-beat measurement during peripheral vasoconstriction [12].
The vasoconstrictor response as assessed by the PTT was less pronounced in patients with MSA-P when compared to patients with PD. The vascular response was compromised in patients with MSA-P, irrespective of the presence or absence of orthostatic hypotension.
The baroreflex-independent rise in heart rate as a response to CPT in patients with PD and MSA-P was assessed by comparing the maximum heart rate during CPT with the baseline. Maximum heart rate instead of average heart rate during CPT was compared to the baseline to negate the role of baroreceptors in modulating the heart rate. During CPT there is activation of the sympathetic system via a baroreceptor-independent pathway leading to an increase in blood pressure and heart rate. This increase in blood pressure would result in firing of the baroreceptors which would result in a decrease of the heart rate. Hence, an average of the heart rate during cold exposure would not produce a sympathetic system-mediated increase in heart rate.
The rise in heart rate as a response to CPT in patients with Parkinson disease, irrespective of the presence or absence of OH, was less than that of normal healthy individuals. Normal percentage increase in heart rate as a response to cpt is 11–13 % [13, 14]. This could be attributed to the fact that patients with PD have been found to have cardiac denervation proven by various MIBG studies [15, 16]. Patients with MSA-P with OH also had a similarly low rise in heart rate in response to moderate cold exposure. This could be due to the fact that 25–30 % of patients with MSA-P have also been found to have cardiac denervation on MIBG studies [16]. Patients with MSA-P without OH had a rise in heart rate comparable to healthy individuals [13, 14]. This could be either because patients with MSA-P without OH do not have a compromised cardiac response, or the rise in heart rate could be a compensatory response to the compromised vascular response, or it could be possible that patients had a different diagnosis altogether.
The compromised vascular response in patients with MSA-P could be due to a lesion in any of the following sites: (1) the sensory pathway carrying the cold responses; (2) the center; (3) sympathetic innervations to the vessels; (4) effector organ (vessels) in isolation. In patients with MSA-P without OH, the increase in heart rate in response to cold appears to be better when compared to patients with PD and MSA-P with OH, but the vascular response remains compromised. From this result, a lesion in the sensory pathway and/or the center can be ruled out in MSA-P without OH.
The poor vascular and heart rate response to cold exposure seen in patients with MSA-P with OH can be explained by the fact that in MSA-P there is a lesion at the level of the rostroventrolateral medulla (RVLM) [17], but this is not the case in PD [18]. The compromised heart rate response in PD could be due to cardiac denervation. Several studies show involvement of the IML, sympathetic ganglia, and adrenal medulla by alpha-synuclein (alpha-SYN)-associated pathology in PD. In MSA, involvement of the RVLM has been reported.
References
Iodice V, Low DA, Vichayanrat E, Mathias CJ (2011) Cardiovascular autonomic dysfunction in MSA and Parkinson’s disease: similarities and differences. J Neurol Sci 310:133–138
Riley DE, Chelimsky TC (2003) Autonomic nervous system testing may not distinguish multiple system atrophy from Parkinson’s disease. J Neurol Neurosurg Psychiatry 74:56–60
Goldstein DS (2003) Dysautonomia in Parkinson’s disease: neurocardiological abnormalities. Lancet Neurol 2:669–676
Hughes AJ, Daniel SE, Kilford L, Lees AJ (1992) Accuracy of clinical diagnosis of idiopathic Parkinson’s disease: a clinico-pathological study of 100 cases. J Neurol Neurosurg Psychiatry 55:181–184
Gilman S, Wenning GK, Low PA, Brooks DJ, Mathias CJ, Trojanowski JQ, Wood NW, Colosimo C, Dürr A, Fowler CJ, Kaufmann H, Klockgether T, Lees A, Poewe W, Quinn N, Revesz T, Robertson D, Sandroni P, Seppi K, Vidailhet M (2008) Second consensus statement on the diagnosis of multiple system atrophy. Neurology. 71:670–676
Freeman R, Wieling W, Axelrod FB, Benditt DG, Benarroch E, Biaggioni I, Cheshire WP, Chelimsky T, Cortelli P, Gibbons CH, Goldstein DS, Hainsworth R, Hilz MJ, Jacob G, Kaufmann H, Jordan J, Lipsitz LA, Levine BD, Low PA, Mathias C, Raj SR, Robertson D, Sandroni P, Schatz IJ, Schondorf R, Stewart JM, van Dijk JG (2011) Consensus statement in the definition of orthostatic hypotension, neurally mediated syncope and the postural tachycardia syndrome. Auton Neurosci 161:46–48
Hanna JN, McN Hill P, Sinclair JD (1975) Human cardiorespiratory responses to acute cold exposure. Clin Exp Pharmacol Physiol 2:229–238
Abboud FM, Eckstein JW (1966) Active reflex vasodilatation in man. Fed Proc 25:1611–1617
Lovallo W (1975) The cold pressor test and autonomic function: a review and integration. Psychophysiology 12:268–282
Saab P, Llabre M, Hurwitz B, Wohlgemuth W, Durel L, Massie C, Nagel J (1993) The cold pressor test: vascular and myocardial response patterns and their stability. Psychophysiology 30:366–373
Barrett K, Barman S, Boitano S, Brooks H (2010) Ganong’s review of medical physiology. McGraw-Hill, USA
Raamat R, Jagomagi K, Talts J (2000) Different responses of Finapress and the oscillometric finger blood pressure monitor during intensive vasomotion. J Med Eng Technol 24:95–101
Singh PI, Khurana I (1991) Cardiovascular responses to cold pressor test: a test for autonomic functions. J Indian Med Assoc 89:229–231
Mourot L, Bouhaddi M, Regnard J (2009) Effects of the cold pressor test on cardiac autonomic control in, normal subjects. Physiol Res 58:83–91
Chung EJ, Lee WY, Yoon WT, Kim BJ, Lee GH (2009) MIBG scintigraphy for differentiating Parkinson’s disease with autonomic dysfunction from parkinsonism-predominant multiple system atrophy. Mov Disord 24(11):1650–1655
Köllensperger M, Seppi K, Liener C, Boesch S, Heute D, Mair KJ, Mueller J, Sawires M, Scherfler C, Schocke MF, Donnemilier E, Virgolini I, Wenning GK, Poewe W (2007) Diffusion weighted imaging best discriminates PD from MSA-P: a comparison with tilt table testing and heart MIBG scintigraphy. Mov Disord 22(12):1771–1776
Cersosimo M, Benarroch EE (2013) Central control of autonomic function and involvement in neurodegenerative disorders. Handb Clin Neurol 117:45–57
Benarroch EE, Schmeichel AM, Parisi JE (2000) Involvement of the ventrolateral medulla in parkinsonism with autonomic failure. Neurology 54:963–968
Conflict of interest
On behalf of all authors, the corresponding author states that there is no conflict of interest.
Ethical approval
The study was approved by the ethics committee for research on human subjects, All India Institute of Medical Sciences, New Delhi (Ref.No. IESC/T-84/dated 02.03.2012), and was carried out after a written consent from the participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Roy, S., Srivastava, A.K., Jaryal, A.K. et al. Cardiovascular responses during cold pressor test are different in Parkinson disease and multiple system atrophy with parkinsonism. Clin Auton Res 25, 219–224 (2015). https://doi.org/10.1007/s10286-015-0294-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s10286-015-0294-x