Abstract
Dopamine is a key neurotransmitter that induces critical effects in the nervous system and in many peripheral organs, via 5 dopamine receptors (DRs): D1R–D5R. Dopamine also induces many direct and very potent effects on many DR-expressing immune cells, primarily T cells and dendritic cells. In this review, we focus only on dopamine receptors, effects and production in T cells. Dopamine by itself (at an optimal concentration of~0.1 nM) induces multiple function of resting normal human T cells, among them: T cell adhesion, chemotactic migration, homing, cytokine secretion and others. Interestingly, dopamine activates resting effector T cells (Teffs), but suppresses regulatory T cells (Tregs), and both effects lead eventually to Teff activation. Dopamine-induced effects on T cells are dynamic, context-sensitive and determined by the: T cell activation state, T cell type, DR type, and dopamine concentration. Dopamine itself, and also few dopaminergic molecules/ drugs that are in clinical use for cardiac, neurological and other non-immune indications, have direct effects on human T cells (summarized in this review). These dopaminergic drugs include: dopamine = intropin, L-DOPA, bromocriptine, pramipexole, pergolide, haloperidol, pimozide, and amantadine. Other dopaminergic drugs were not yet tested for their direct effects on T cells. Extensive evidence in multiple sclerosis (MS) and experimental autoimmune encephalomyelitis (EAE) show dopaminergic dysregulations in T cells in these diseases: D1-like DRs are decreased in Teffs of MS patients, and dopamine does not affect these cells. In contrast, D1-like DRs are increased in Tregs of MS patients, possibly causing functional Treg impairment in MS. Treatment of MS patients with interferon β (IFN-β) increases D1-like DRs and decreases D2-like DRs in Teffs, decreases D1-like DRs in Tregs, and most important: restores responsiveness of patient’s Teffs to dopamine. DR agonists and antagonists confer some benefits in EAE-afflicted animals. In a single clinical trial, MS patients did not benefit from bromocriptine, which is a D2-like DR agonist. Nevertheless, multiple evidence showing dopaminergic abnormalities in T cells in MS encourages testing other DR analogues/drugs in MS, possibly as “add-on” to IFN-β or other MS-immunomodulating therapies. Together, abnormalities in DRs in T cells can contribute to MS, and DRs in T cells can be therapeutic targets in MS. Finally and in a more general scope: the direct effects of all dopaminergic drugs on human T cells should be studied in further depth, and also taken into consideration whenever treating patients with any disease, to avoid detrimental side effects on the immune system of the patients.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Part 1: Introduction to dopamine: history, structure and function in the brain
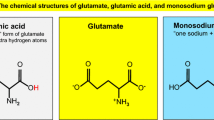
Dopamine’s chemical formula is C6H3(OH)2–CH2–CH2–NH2. Dopamine is a monoamine, and a member of a group of neurotransmitters called “Biogenic amines”, consisting of dopamine, norepinephrine, epinephrine and serotonin (Fig. 1). Dopamine’s precursor is 3,4-dihydroxyphenylalanine (L-DOPA). Dopamine itself is a precursor to norepinephrine (noradrenaline), which in turn is the precursor of epinephrine (adrenaline), and these three neurotransmitters are collectively called catecholamines (CAs).
The Nobel Prize in Physiology or Medicine in 2000 was awarded jointly to Arvid Carlsson, Paul Greengard and Eric R. Kandel “for their discoveries concerning signal transduction in the nervous system”. Arvid Carlsson received this Nobel Prize for his pioneering studies during the late 1950s, which showed that dopamine is an important transmitter in the brain. He further found that patients with Parkinson’s disease (PD) have abnormally low concentrations of dopamine in the basal ganglia, due to the degeneration of dopamine-producing nerve cells in this brain region, and that this causes tremor, rigidity and akinesia. In consequence of these findings, L-DOPA was developed as a drug for PD, and is still the most important treatment for PD. L-DOPA is converted to dopamine in the brain, and compensates for the lack of dopamine. Since the pioneering discoveries of Arvid Carlsson, an enormous amount of research has been performed worldwide on many aspects of dopamine physiology and pharmacology, contributing substantially to many fields and topics in biology and medicine. Among these fields are: neurology, cognition, attention, memory, psychiatry, psychopharmacology, drug addiction, reward, cardiology, emergency medicine, blood pressure and others (Iversen and Iversen 2007).
Dopamine is known now as one of the principal neurotransmitters in the CNS of both humans and animals, involved in behavior, cognition, control of movement, endocrine regulation and cardiovascular function. Dopamine has also many important exocrine and paracrine effects on few peripheral organs and systems among them: the blood, kidneys, pancreas, intestine, heart and the entire immune system. As to the potent and important effects of dopamine on the immune system: in recent years it has become clear that most if not all types of immune cells express functional on dopamine receptors (DRs) their cells surface, that dopamine by itself activates its DRs in immune cells, especially T cells, and induces powerful effects on these cells (see Fig. 3), and that some immune cells can in fact produce dopamine and even affect themselves (in an autocrine manner) and other cells (in a paracrine manner) via their immune-derived dopamine. All of this is reviewed and discussed in “Parts 3–6” this review, in an already published book chapter on dopamine in the immune system, and in a related review (Levite 2012, 2016). “Part 6” of this review specifically focuses on the abnormalities of the dopaminergic system in patients with multiple sclerosis (MS) in comparison to healthy individuals, and in animals afflicted by experimental allergic encephalomyelitis (EAE).
The dopamine receptors (DRs). The DRs are a class of G protein-coupled receptors that are prominent in the vertebrate CNS, in several peripheral organs, and in many types of immune cells. There are at least five DR types: D1R, D2R, D3R, D4R and D5R, grouped in two DR families: the D1-like receptor family, consisting of D1R and D5R, and the D2-like receptor family, consisting of D2R, D3R and D4R. Activation of the D1-like receptors, coupled to the G protein Gαs, leads to the activation of adenylyl cyclase, and subsequently to an increase in the intracellular concentration of the secondary messenger cyclic adenosine monophosphate (cAMP). The D2-like receptors are characterized by a large third cytoplasmic loop and a short carboxyl-terminal tail. Activation of the D2-like receptors is coupled to the G protein Gαi, and inhibits the formation of cAMP by inhibiting the enzyme adenylate cyclase. Dopamine is the primary endogenous ligand for all the DRs. Yet, there are many dopaminergic analogues and drugs that bind selectively or preferentially only specific DR types and affect their function, while inducing much less potent, if at all, effects on the other DRs. In general terms, the DR agonists activate DRs, while DR antagonists block them. Further information about the DRs can be read in Beaulieu et al. (2015), and in numerous original papers, reviews and book chapters published over the years about the DRs
Part 2: Introduction to dopamine receptors
The dopamine receptors (DRs) (Fig. 2; Beaulieu et al. 2015) are metabotropic G protein-coupled receptors expressed in various cell types in various organs and tissues, including several regions of the CNS, the heart, kidney, gastrointestinal tract, various vascular beds, and the immune system. In the latter, different types of immune cells, among them T cells, DCs and others, express functional DRs on their surface which mediate very important effects, as discussed in “Parts 4 and 5” below, in (Levite 2012), and of course in the original papers of various groups that discovered these effects, and that are cited below in the respective parts. Peripheral DRs influence cardiovascular and renal function by decreasing afterload and vascular resistance and promoting sodium excretion (Hussain and Lokhandwala 2003).
There are at least five subtypes of DRs: D1R, D2R, D3R, D4R, and D5R (Fig. 2). These are grouped in two DR families: the D1R-like family, consisting of D1R and D5R, and the D2R-like family, consisting of D3R, D4R and D5R. Figure 3 shows few characteristic features of the two DR families. The D1-like receptors are coupled to the G protein Gαs, which subsequently activates adenylyl cyclase, increasing the concentration of cyclic adenosine monophosphate (cAMP). In contrast, the D2-like receptors are coupled to the G protein Gαi, which inhibits cAMP formation by inhibiting adenylate cyclase. There is also some evidence suggesting the existence of possible D6R and D7R, but such receptors have not been conclusively identified. Dopamine is the primary endogenous ligand for all the DR types, and as such activates all of them. In contrast, there are many types of selective DR agonists and antagonists that bind selectively/preferentially to specific DR types. These selective DR agonists and antagonists are used for biological and medical research, and some of them are also drugs for PD and several neuropsychiatric disorders including schizophrenia, bipolar disorder and depression.
The direct and potent effects of dopamine on resting effector T cells, in a low physiological concentration range. Dopamine by itself induce many, direct, potent and important effects of T cells. Dopamine on its own, at an optimal physiological conc. of ~10 nM (10−8 M) activates and/or elevates several important functions and features of human resting Teffs, resulting in an elicitation or augmentation of key effective T cell responses. Some of the dopamine-induced T cell functions known so far are listed in the figure. Ongoing studies whose results are not published yet, and further studies that will hopefully be performed in the future, will undoubtedly reveal many more effects of dopamine on Teffs, and also on other types of T cells, and other types of immune cells. The figure is drawn based on the compilation of findings revealed by several research groups worldwide, cited and summarized in this review, and in Levite (2012, 2016)
The expression of DRs is abnormal in various types of diseases, and the abnormal DR function is suspected to contribute actively to the pathological scenario. Yet, in some other diseases, the abnormal DR expression serves only as a marker for the disease. For more information about the localization, expression, structure, signaling and function of the DRs in health and disease, the reader is referred to many book chapters and reviews on this topic, among them the review by Beaulieu et al. (2015). Interestingly, in this review, Beaulieu summarizes recent evidence showing that besides their canonical action on cAMP-mediated signaling, DRs can regulate numerous cellular responses to fine-tune dopamine-associated behaviors and functions (Beaulieu et al. 2015).
Part 3: Dopamine production by immune cells
Dopamine is produced mainly by neuronal cells, but low levels of dopamine have been found in several non-neuronal cells, such as cells in the gastrointestinal system, the renal system, and also the immune system (Bergquist and Silberring 1998). As to the later, indeed, a large body of evidence shows that dopamine is undoubtedly produced in many, if not all, types of immune cells, including peripheral blood mononuclear cells (PBMCs), peripheral blood lymphocyets (PBLs), T cells (regulatory T cells (Tregs) ≫> effector T cells (Teffs)), B cells, macrophages, and spleen cells (Levite 2012; Bergquist and Silberring 1998; Josefsson et al. 1996; Bergquist et al. 1994, 1997; Cosentino et al. 2007; Ferrari et al. 2004; Musso et al. 1997; Nakano et al. 2009a, b; Flierl et al. 2007, 2009; Santambrogio et al. 1993; Mckenna et al. 2002; Levite et al. 2001; Besser et al. 2005). Under certain conditions, mainly upon activation of immune cells, the internally produced dopamine (and the other CAs) can be released by the immune cells to the extracellular milieu, resulting in autocrine and paracrine effects (Levite 2012; Bergquist and Silberring 1998; Josefsson et al. 1996; Bergquist et al. 1994, 1997; Cosentino et al. 2007; Ferrari et al. 2004; Musso et al. 1997; Nakano et al. 2009a, b; Flierl et al. 2007, 2009; Santambrogio et al. 1993; Mckenna et al. 2002; Levite et al. 2001; Besser et al. 2005).
Dopamine content in various immune cells was found to be in the range of ~10−19 to 10−17 mol per cell (Bergquist and Silberring 1998; Josefsson et al. 1996; Bergquist et al. 1997), or ~10−12 to 10−11 mol dopamine/per 106 human T cells (Cosentino et al. 2007).
Among all the studies performed on the production and/or presence of CAs in immune cells, the study of Bergquist and Silberring (1998) seems to be the most comprehensive one. In addition, Table 1.1 in the paper of Levite (2012) summarizes the evidence accumulated until 2012 for the production of dopamine in various types of immune cells.
Several interesting features regarding to the production, release and uptake of dopamine by immune cells are summarized briefly here. Intracellular dopamine levels increase following an increase in extracellular dopamine, suggesting a cellular uptake mechanism in lymphocytes (Bergquist et al. 1994). Interestingly, activation of human T cells and B cells (called also T and B lymphocytes), for example with a PKC activator, induce tyrosine hydroxylase (TH) mRNA expression, as well as increase the amount of intracellular CAs (Ferrari et al. 2004) in these cells. This indicates that dopamine production by lymphocytes is dynamic, activation-induced and context-sensitive. Furthermore, based on various types of findings revealed by various groups including ours, we hypothesize that the extent and timing of dopamine production by T cells and B cells is dependent on, and dictated by, the lymphocyte’s internal needs and usage of dopamine for their own: adhesion, migration, homing, survival, proliferation, communication with other cells that express functional DRs (immune, neural and other cells) and more. We further hypothesize that lymphocytes need dopamine to combat infectious organisms and cancer, and help the nervous system overcome neuropathologies. Yet, at this time point, these are indeed suggestions, and further studies, epseically in vivo, are required to validate or rule them out. help the nervous system overcome neuropathologies.
Of further interest are the relevant findings that neurotransmitters other than CAs can influence CA synthesis in lymphocytes. This was shown for example for acetylcholine, that can regulate CA synthesis in lymphocytes through activation of the rate-limiting enzyme TH (Musso et al. 1997).
Human CD4+ CD25+ Tregs constitutively express TH, and contain substantial amounts of dopamine, as well as norepinephrine and epinephrine. These CAs are released upon treatment with reserpine (Cosentino et al. 2007). Moreover, dopamine released by Tregs can act in an autocrine/paracrine inhibitory loop, resulting in down-regulation of Treg function (Cosentino et al. 2007). Thus, dopamine suppresses CD4+ CD25+ regulatory T cells in an autocrine manner (Cosentino et al. 2007), and as a result of that effector T cells (Teffs) can start proliferating and functioning.
Dopamine production and release by the immune system is not restricted to T cells and also takes place in other immune cells. Furthermore, the synthesis and release of dopamine by immune cells is inducible by various stimuli, and in turn induces by itself potent effects on other immune cells and processes, like the T cell-derived dopamine does. One example is dopamine in dendritic cells (DC): human monocyte-derived DCs store and release dopamine, which polarizes Th2 differentiation (Nakano et al. 2009a). This interesting study (Flierl et al. 2007) identified DCs as a new source of dopamine, which functions as a Th2-polarizing factor in DC-naive T cell interface. Another example is dopamine in phagocytes: phagocytes generate, store and release CA, and exposure of phagocytes to LPS leads to a release of CAs, and to an induction of CA-generating and degrading enzymes. These findings indicate that phagocytes contain the complete intracellular machinery for the generation, release and inactivation of CAs (Flierl et al. 2007), and that CAs release by phagocytes is induced by specific molecules. Furthermore, up regulation of phagocyte-derived CAs augments the acute inflammatory response (Flierl et al. 2009). The abnormalities in the production of dopamine and of the other CAs by PBLs or T cells of MS patients is discussed below in “part 6”.
Part 4: Various types of immune cells, especially normal human T cells, express various types of functional dopamine receptors on their cell surface
Most, if not all types of immune cells express DRs, but at different levels and compositions. The immune cells shown so far to express DRs include: PBLs, effector T cells (Teffs), regulatory T cells (Tregs), B cells, natural killer (NK) cells, DCs, monocytes, macrophages, microglia and neutrophils (Cosentino et al. 2007; Santambrogio et al. 1993; Mckenna et al. 2002; Levite et al. 2001; Besser et al. 2005; Nakano et al. 2009b; Gaskill et al. 2009; Sarkar et al. 2010; Pacheco et al. 2009; Zhao et al. 2013; Ricci et al. 1997a, b, 1999). For a summary of the DR types expressed by each type of immune cell, see part G1 and Table 1.2 in the book chapter of Levite (2012), and the numerous original papers cited therein. DR expression in immune cells is highly dynamic, context-sensitive and variable. It changes from one immune cell type to another, and in any given immune cell according to its resting or rather activated state. Exposure of resting immune cells to different stimuli/molecules/drugs can also change their DR expression [reviewed in (Levite 2012, 2016)]. Moreover, age-dependent changes in the expression of DRs subtypes in human PBLs has been reported (Barili et al. 1996).
The most studied immune cells with regard to their DR expression and function are T cells. The main findings thus far with regards to the expression of DRs in human T cells, which are the focus of this review, are summarized and discussed briefly in the following paragraphs, and discussed in further depth in Levite (2012, 2016), and in the original papers cited in them.
-
1.
In general, human T cells express on their cell surface functional DRs of all D1R–D5R types, but the expression level of each of the DR1–D5R types differs between different T cell types and subtypes, and between resting and activated T cells. In general, activated T cells express higher levels of DRs than resting T cells. DR expression in T cells is also very sensitive and dynamic, and sometimes different in patients with various diseases compared to healthy subjects [reviewed in Levite (2012, 2016)] and mentioned again in point 3 below).
Collectively, the T cells types and subtypes found so far to express DRs include the following: heterogeneous population of peripheral normal human T cells, CD8+ cytotoxic T cells (CD8+ Teffs), CD4+ helper T cells (CD4+ Teffs), naïve CD45RA+ T cells, naive CD3+ CD4+ CD45RA+ CCR7+ T cells, memory CD45RO+ T cells, central memory CD3+ CD4+ CD45RA− CCR7+ T cells, effector memory CD3+ CD4+ CD45RA− CCR7− T cells, and CD4+ CD25+ Tregs (Levite et al. 2001; Besser et al. 2005; Cosentino et al. 2007; Watanabe et al. 2006; Kustrimovic et al. 2014). These T cell types and subtypes differ in the protein levels of the functional DRs expressed on their cell surface, and in their DR mRNA levels. For example, a different level and composition of DRs is expressed in helper CD4+ T cells vis-à-vis cytotoxic CD8+ T cells, in Th1 cells vis-à-vis Th2 cells, in CD4+ CD25− Teffs vis-à-vis CD4+ CD25+ Tregs, and in naïve CD45RA+ T cells vis-à-vis memory CD45RO+ T cells.
-
2.
The protein levels of the DRs expressed on the cell surface of T cells are often without any correlation to their DR mRNA levels [see for example Cosentino et al. 2007; Kustrimovic et al. 2014)]. Due to that, and since in terms of DR activity only the membrane-anchored functional DRs are important (because they are the receptors that bind and respond to dopamine and DR analogues), further studies should focus primarily on the functional membranal DRs, and avoid reaching conclusions on DR function only based on DR mRNA levels.
-
3.
In several human autoimmune diseases, like MS, systemic lupus erythematosus (SLE) rheumatoid arthritis (RA), and/or in their animal models, the T cells have various dopamine-related abnormalities, including abnormal DR expression, and/or abnormal response to dopamine, and/or abnormal production of dopamine, or other [summarized in Levite (2012)]. Abnormalities in SLE have been reported by Jafari et al. (2013), and in RA by Nakano et al. (2011). Evidences for such abnormalities in MS and EAE are summarized and discussed in “part 6” based on original studies, among them (Basu et al. 2010; Fiszer et al. 1994, 2001; Rocc et al. 2002; Nagai et al. 1996; Hisanaga et al. 2001; Bas et al. 2001; Blandini et al. 2009; Alberio et al. 2012).
-
4.
Cancerous T cells: T leukemia cells and T lymphoma cells express functional DRs on their cell surface (Basu et al. 2010).
-
5.
In some neurological and psychiatric disorders, including PD, schizophrenia, Alzheimer disease, Tourette, depression and migraine, the patient’s T cells have abnormalities in: DRs expression, and/or responses to dopamine, and/or production of CAs [summarized in Levite (2012, 2016)]. Evidences for such abnormalities in PD are shown in various studies, among them: (Fiszer et al. 1994, 2001; Rocc et al. 2002; Nagai et al. 1996; Hisanaga et al. 2001; Bas et al. 2001; Blandini et al. 2009; Alberio et al. 2012; Kurkowska-Jastrzebska et al. 1999; Benner et al. 2008; Reynolds et al. 2009; Wandinger et al. 1999). Other studies reported DR abnormalities in T cells in schizophrenia (Kwak et al. 2001; Ilani et al. 2001; Brito-Melo et al. 2012; Boneberg et al. 2006), or Alzheimer disease (Barbanti et al. 2000; Cosentino et al. 2009) and migraine (Levite 2008; Barili et al. 1996; Strell et al. 2009).
Part 5: Dopamine by itself, at low physiological concentration (~10−8 M = 10 nM) induce many direct, potent and important effects on immune cells, by directly activating resting effector T cells and inducing many key effector T cell functions, and also by suppressing activated regulatory T cells in an autocrine/paracrine manner
Dopamine on its own, at low physiological concentration of ~10−8 M, induce many direct, potent and important functions on immune cells. The evidences for that were reported in various original papers (cited below).
T cells are the immune cell type most studied for their expression of functional DRs, and for their response to dopamine, DR agonists and DR antagonists. Collectively, the various studies show that dopamine by itself (without any additional molecules) triggers or increases substantially specific functions of resting effector T cells (Fig. 3). In addition, and in contrast, dopamine suppresses or decreases potently various functions of activated T cells and of Tregs. Thus, dopamine by itself, in a low physiological range ~10−8 M, can activate effector human Teffs in two independent ways: (1) direct activation of resting Teffs (Fig. 3), and (2) suppression of Tregs, which leads to activation of Teffs.
The main findings made thus far regarding dopamine effects on normal resting Teffs are summarized very briefly below, listed in Fig. 3, reviewed by Levite (2012, 2016), and of course described in the many original papers written by the research groups worldwide that revealed the pioneering findings.
-
1.
Dopamine-induced effects on T cells are very different for different dopamine concentrations, different T cell types and subtypes, different resting or activation states, and different healthy or diseases states [reviewed in Levite (2012, 2016)]. Thus, when talking about dopamine-induced effects on T cells, and also about the effects of other neurotransmitters on T cells, one needs to keep in mind that: “It is a matter of context” (Levite 2008).
With regard to the activation of resting Teffs: dopamine at an optimal physiological concentration of ~10−8 M, and on its own (i.e., in the complete absence of any other stimulating molecules such as antigens, mitogens, anti-CD3/CD28 antibodies, cytokines or others) activate resting/naive Teffs, (CD8+ Teffs seem to be more responsive than CD4+ Teffs) and induce many key T cell functions, including: T cell adhesion to fibronectin and laminin (the main proteins of the extracellular matrix), T cell chemotactic migration, T cell migration towards autologous cancer (of cancer patients), T cell homing into specific organs, T cell secretion of key cytokines primarily TNF-α and IL-10, and other T cell functions (Levite et al. 2001; Besser et al. 2005; Watanabe et al. 2006; Strell et al. 2009; Saussez et al. 2014; Levite 2012, 2016).
-
2.
Dopamine affects Th1, Th2 and Th17 differentiation (Nakano et al. 2008, 2009a, b, 2011; Nakagome et al. 2011; Prado et al. 2012; Nakano and Matsushita 2007).
-
3.
Dopamine inhibits already activated Teffs, (i.e., mitogen/antigen/anti-CD3 ± CD28 antibodies/cytokine-activated Teffs) (Bergquist et al. 1994, 1997, 2000; Josefsson et al. 1996; Strell et al. 2009; Cook-Mills et al. 1995; Saha et al. a, b; Ghosh et al. 2003; Carr et al. 2003; Ilani et al. 2004; Giorelli et al. 2005; Sarkar et al. 2006; Huang et al. 2010; Ferreira et al. 2011).
-
4.
Dopamine inhibits activated Tregs in an autocrine/paracrine manner. In other words, dopamine “suppresses the suppressors”. The dopamine-induced autocrine suppressive effect on Tregs can take place since Tregs produce and release dopamine, which subsequently binds to its D1-like receptors in Tregs, leading to the autocrine suppression of these T cells (Cosentino et al. 2014; Kipnis et al. 2004).
-
5.
Dopamine affects intracellular signaling molecules/cascades in T cells, e.g., ERK, Lck, Fyn, NFκB and KLF2, mainly after the T cells have been activated by either antigen, mitogen, anti-CD3 ± CD28 antibodies or PKC activators (Strell et al. 2009; Ghosh et al. 2003; Sarkar et al. 2006).
-
6.
Dopamine is important for antigen-specific interactions between T cells and DCs (Nakano et al. 2009a, b). This conclusion is based, for example, on the observations of Nakano et al. that monocyte-derived DC (Mo-DCs) store dopamine in secretary vesicles, and that antigen-specific interaction of these cells with naive CD4+ T cells induces the release of dopamine-containing vesicles from Mo-DCs. Subsequently, the secreted immune-derived dopamine affect various immune target cells (Nakano et al. 2009a, b).
-
7.
Dopamine itself, and also various approved drugs that affect the dopaminergic system, either still in use or that were used in the past, have various types of potent effects on human T cells (Table 1). These dopaminergic molecules include: dopamine = intropin, L-DOPA, bromocriptine, haloperidol, quinpirol, reserpine, pergolide, ecopipam, pimozide, amantadine, tetrabenzine, nomifensine, and butaclamol.
The effects of these dopaminergic molecules on T cells are described in the respective original studies (Josefsson et al. 1996; Bergquist et al. 1994, 1997; Cosentino et al. 2007; Nakano et al. 2009a; Wandinger et al. 1999; Carr et al. 2003; Ilani et al. 2004; Huang et al. 2010; Tsao et al. 1998; Mori et al. 2013; Musso et al. 1996; McMurray 2001; Bissay et al. 1994), as well as in (Levite 2012, 2016). Because these and other approved drugs that affect DRs or dopamine levels are different in their nature, mechanism of action and effects on different cell types, including T cells, it would be too long, complicated and potentially confusing to discuss the effects of each of them on T cells here, but the reader is referred to Table 1 herein. This table lists the approved drugs that act as dopamine agonists or antagonists, or that change the level of dopamine, and cites very few examples of their reported effects on T cells revealed so far. Table 1 also shows few dopaminergic drugs that their effects on T cells were not tested yet.
Table 1 The effects of dopaminergic molecules on T cells. Several dopaminergic drugs have already been shown to have direct effects on T cells. Other dopaminergic drugs were not tested yet for such effects, and should be investigated for their immune effects, especially on T cells of patients who receive these drugs -
8.
Dopamine, DR agonists and DR antagonists have potent effects on human autoimmune diseases and/or on their animal models [summarized in part by Pacheco et al. (2014a, b)], including the supressive effect of DR antagonists on EAE (Nakano et al. 2008) (discussed below in “part 6”), and on collagen-induced arthritis (Nakashioya et al. 2011).
-
9.
Dopamine, DR agonists and DR antagonists affect T cell cancers: T-lymphoma and T-leukemia (Meredith et al. 2006).
Based on all the above, we suggest that it may be therapeutically advantageous to use either dopamine itself or selective DR agonists to activate DRs in resting Teffs of patients with either solid cancers or severe chronic infectious diseases. Such activation of DRs in ‘good’ Teffs may augment the T cell’s ability to reach and eradicate the cancer and the disease-causing microorganisms. In addition and independently, we hypothesize that it could be therapeutically advantageous to block DRs in autoimmune T cells that cause T cell-mediated autoimmune diseases. Likewise, it may be therapeutically beneficial to block/target DRs in cancerous T cells: in T-leukemia and T-lymphoma (and maybe other types of cancers). Blocking in vivo DRs expressed in such detrimental T cells is expected to block or even kill the disease-causing T cells.
Part 6: Dopamine and its receptors in multiple sclerosis and experimental autoimmune encephalomyelitis
Abnormalities in dopamine levels, receptors, transporters or function in multiple sclerosis patients
With the exception of a study published in the late 1970s, suggesting that some patients with MS may have lower homovanillic acid, one of the main metabolites of dopamine, in the cerebrospinal fluid (CSF) (Tabaddor et al. 1978), there is no direct evidence concerning dopaminergic pathways and activity in the CNS of MS patients. Such findings in the CSF were recently partially confirmed by another study which showed that homovanillic acid levels are lower only in progressive MS, with a negative correlation to duration of illness, and a strong negative correlation to EDSS score (Markianos et al. 2009).
Hyperprolactinemia is a common finding in MS patients, and it is usually considered as an indicator of hypothalamic lesions. It is, however, uncertain whether this implies specific dysfunction of the dopaminergic tuberoinfundibular pathways which are involved in the tonic inhibition of prolactin secretion (Kira et al. 1991).
Of potential interest, two haplotypes of the DR D2 gene have been reported to be possibly associated with the age at onset and/or diagnosis of MS. However, such results have not yet been published. Their relevance is, therefore, hard to be established (J.P. MacMurray et al. unpublished observation, cited by Gade-Andavolu et al. (1998).
In contrast with the lack of data regarding CNS, extensive evidence indicates that in MS, dopaminergic pathways are dysregulated in the peripheral immune system (Cosentino et al. 2002). It has been reported that dopamine production is reduced in stimulated lymphocytes of patients with chronic progressive MS or relapsing-remitting MS in relapse. We suggest that under health conditions endogenous CAs in human lymphocytes may contribute to the regulation of activation-induced apoptosis (Cosentino et al. 2002). If so, reduced dopamine production in cells of MS patients may be associated with the impaired apoptotic mechanisms occurring in activated immune cells during MS.
Protein and mRNA levels of D5R (D1-like DR), but not of D3R (D2-like DR), are reduced in PBMCs of untreated relapsing-remitting MS patients (Giorelli et al. 2005). In the same study, in vitro experiments showed that dopamine reduces the proliferation, IFN-γ secretion, and matrix metalloproteinase-9 production in activated (by anti-CD3 antibodies + IL-2) PBMCs of healthy subjects, but not in the activated PBMCs of MS patients. Upon treatment of patients with IFN-β, however, lymphocytes showed reduced D3R and restored ability of dopamine to regulate cell functions (Giorelli et al. 2005).
In a longitudinal study of relapsing-remitting MS patients undergoing treatment with IFN-β (Zaffaroni et al. 2008), it was found that during the 12 months of treatment, the mRNA levels of D5R (D1-like DR) increased in circulating PBMCs, while the D2R (D2-like DR) mRNA levels progressively decreased, suggesting that IFN-β treatment affects dopaminergic pathways in circulating lymphocytes, shifting the balance from D2-like DR prevalence in untreated patients, towards D1-like DR prevalence after IFN-β treatment. Interestingly, the D1-like D5R is possibly inhibitory on both human CD4+ and CD8+ T cells (Saha et al. 2001a, b), while activation of D2-like DRs in resting T cells leads to activation of these cells and to the induction of several T cell functions among them: adhesion, migration, cytokines secretion and others (Levite et al. 2001; Levite 2012, 2016; Besser et al. 2005) (Fig. 3).
Zaffaroni et al. (2008) also measured TH mRNA levels and the production of endogenous dopaminergic, noradrenaline and adrenaline in circulating PBMCs of MS patients treated with IFN-β. They showed that IFN-β therapy increases TH mRNA as well as CAs production. Such an effect resembles the previously reported in vitro ability of IFN-β to increase TH as well as endogenous CAs production and release in human lymphocytes (Cosentino et al. 2005).
Recently, Cosentino et al. showed that higher mRNA levels for the D1-like D5R in circulating lymphocytes may predict subsequent response to IFN-β therapy in relapsing-remitting MS patients (Cosentino et al. 2014).
The effect of IFN-β therapy on MS was also studied in circulating CD4+CD25highFoxP3+ Tregs. These suppressor Tcells may be directly involved in EAE and MS [reviewed by Venken et al. (2010) and Zozulya et al. (2008)]. Tregs contain dopamine, noradrenaline and adrenaline. Interestingly, the endogenous dopamine in Tregs inhibits their own suppressive function in a D1-like D5R-mediated autocrine/paracrine mechanism (Cosentino et al. 2007). In relapsing-remitting MS patients undergoing IFN-β treatment, before treatment (i.e., in drug-naive subjects) Tregs have increased mRNA of D1-like D5R and of TH. During IFN-β, both D5R and TH mRNA decrease to values lower than those of cells of Tregs of healthy subjects (Cosentino et al. 2012). In functional in vitro experiments, dopamine reduces the suppressive activity of Tregs of healthy subjects, and completely abolishes the suppressive activity of Tregs of untreated MS patients. In contrast, dopamine has no inhibitory effects on Tregs of patients treated with IFN-β (Cosentino et al. 2012). The increased TH mRNA in Tregs of untreated patients suggests increased dopamine production, which in turn may suppress the regulatory function of Tregs through increased D1-like D5R (whose mRNA is actually increased). This is indirectly confirmed by the reported ability of dopamine to completely abolish ex vivo the regulatory function of Tregs. Increased endogenous dopamine-dependent inhibition of Tregs likely contributes to the functional impairment of these cells in MS, resulting in enhanced disease activity (Venken et al. 2010; Zozulya et al. 2008). In agreement with this hypothesis, TH mRNA after 12 months of IFN-β was higher (on average 55%) in Tregs of patients experiencing clinical relapses, in comparison to those without relapses during the study (Cosentino et al. 2012).
In summary, endogenous CAs in lymphocytes are extensively involved in MS. Dysregulation seems to affect mainly (even if not only) dopamine. This is, however, different in the various cell subsets. In PBMCs as a whole, the production of CAs may be impaired. Cell sensitivity to D1-like -mediated anti-inflammatory effects is reduced. In Tregs, CA production may be increased, and D5R pathways (which in these cells “suppress the suppressors”, enhancing the effective immune responses) show increased activity. A recent study shows that in T cells of MS patients not taking any immunomodulatory drug for at least 3 months, dopamine has pro-inflammatory effects, amplifying glucocorticoid-resistant Th17 cells, possibly through IL-6 production by monocytes and CD4+ T cells (Ferreira et al. 2014). IFN-β therapy in MS patients possibly restores a “physiological” situation in all the lymphocyte subsets, exerting opposite effects in PBMCs and in Tregs (Table 2).
Part 7: Abnormalities in dopamine levels, receptors, transporters or function in experimental autoimmune encephalomyelitis-afflicted animals
White et al. (1983) showed that in rats with EAE most spinal cord regions are depleted of noradrenaline, while dopamine depletion is specific to the cervical dorsal horn. In rats with EAE, splenic dopamine concentrations decreased on day 14 post-inoculation (at the peak of the clinical symptoms of EAE), but they were not different from controls on day 7 and 52 post-inoculation.
As to mice with EAE induced by myelin oligodendrocyte glycoprotein (MOG) 35–55 in complete Freund’s adjuvant (CFA) - in the acute phase dopamine levels in the striatum were higher, while the ratio of homovanillic acid/dopamine (HVA/dopamine) and 3,4-dihydroxyphenylacetic acid/dopamine was lower, suggesting decreased dopamine turnover (Bałkowiec-Iskra et al. 2007a, b). Significantly, immunization with MOG 35-55 peptide in CFA of C57BL mice previously intoxicated with 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP, a neurotoxin whichupon conversion to MPP+selectively kills dopaminergic neurons in the substantia nigra), resulted in a reduction of dopamine in striatum as compared to non-immunized animals. This suggested that a suppressive influence of autoimmune reaction was induced after injury on regeneration of MPTP-intoxicated dopaminergic neurons (Balkowiec-Iskra et al. 2003). Reduced dopamine release and unbalanced D1-like/D2-like dopamine receptor signaling in mice with EAE have been recently reported and linked to increased expression in striatum of interleukin-1β and associated with depressive-like behavior of the animals (Gentile et al. 2015).
Part 8: The effect of dopamine and/or its agonists and antagonists on multiple sclerosis patients
Berne-Fromell et al. (1987) report on a clinical study in which 300 MS patients were treated with the dopamine precursor L-DOPA and with tri- and tetracyclic antidepressants. There were substantial sensory, motor and autonomic symptom improvements in 75% of the subjects after 1–2 months (Berne-Fromell et al. 1987). The effects were interpreted in terms of increased noradrenaline, but a contribution of dopamine cannot be ruled out in view of the pharmacology of the drugs employed.
The D2-like agonist bromocriptine (an ergoline derivative selective for the D2-like D2/D3 receptors) was tested on 18 patients with MS (10 relapsing-remitting and 8 chronic progressive), in an open pilot study with 2.5 mg two times a day. After one year, 14 of the 15 patients who completed the study showed disease progression, suggesting that bromocriptine does not suppress ongoing disease activity in MS patients (Bissay et al. 1994).
Amantadine, an antiviral and anti-Parkinson drug with several pharmacological activities, (including dopaminergic, noradrenergic and serotoninergic, MAO-A blockade and NMDA receptor antagonism (Huber et al. 1999)), is presently recommended for the treatment of MS-related fatigue. Improvements in fatigue may be, however, small. A recent review concludes that good quality randomized clinical trials are still needed (Qiu et al. 2004). Amantadine has been shown in a double-blind, placebo-controlled cross-over trial in MS patients to be beneficial on early cognitive processes, but only in subjects with longer disease duration (Sailer et al. 2000). The relevant mechanism(s) involved in this effect has not been established.
Finally, it should be mentioned that treatment of MS patients with dopamine antagonists (antipsychotics) is frequent, due to the relatively common occurrence of psychiatric symptoms in these subjects (Davids et al. 2004). There is, however, a paucity of systematic studies about the clinical effects of these drugs in MS. In particular, their effects on MS itself have been never considered.
Part 9: The effect of dopamine and/or its agonists and antagonists on experimental autoimmune encephalomyelitis-afflicted animals
Neurotoxins
Administration in the CNS of 6-hydroxydopamine (6-OHDA), which selectively kills dopaminergic and noradrenergic neurons, increases CD8+ T cells in the perivascular lesions, and reduces the clinical manifestations of EAE in rats (Karpus et al. 1988). These results were confirmed by the same group. It was suggested that the effect of 6-OHDA is due to reduced noradrenergic activity (Konkol et al. 1990). However, in view of the mechanism of action of the neurotoxin, a contribution of dopaminergic mechanisms cannot be ruled out.
CNS depletion of dopamine by use of MPTP results in EAE exacerbation (Balkowiec-Iskra et al. 2007b).
Dopamine agonists
In female Lewis rats with EAE, administration of the dopaminergic agonist bromocriptine reduces both the severity and the clinical signs of EAE, an effect which can be explained in terms of bromocriptine-induced reduction of pituitary secretion of prolactin, which has a stimulatory role on immune function (Riskind et al. 1991). In a subsequent study, bromocriptine treatment started after the onset of clinical signs, reduced both severity and duration in acute EAE. In chronic relapsing EAE, it did not affect the severity and duration of the first attack, but reduced the duration of the subsequent second attack (Dijkstra et al. 1994).
Dopamine antagonists
SCH23390, a D1-like D1R/D5R selective antagonist, has the ability to prevent EAE in mice, possibly by inhibiting DC-mediated Th17 lymphocyte differentiation (Nakano et al. 2008). The role of D5R on DCs in mice has been extensively characterized by Prado et al. (2012), who show that such receptors induce IL-23 and IL-12 production, and consequently promote the activation and proliferation of antigen-specific CD4+ T cells. In the same study, D5R-deficient DC prophylactically transferred into wild-type mice reduce the severity of EAE, as well as the percentage of Th17 cells infiltrating the CNS.
The atypical antipsychotic risperidone, which is a D2-like DR antagonist, also endowed with anti-serotonergic, anti-adrenergic and anti-histaminergic properties, reduces the severity of EAE, and decreases both the size and number of spinal cord lesions, possibly through the reduction of antigen-specific production of IL-17a, IL-2, and IL-4 by splenocytes (O’Sullivan et al. 2014). In the same study, clozapine, another atypical antipsychotic agent, reduced EAE. However, such an effect cannot be attributed to D1-like or D2-like DR antagonism alone (O’Sullivan et al. 2014; Fig. 4).
Dysfunctional DR pathways and endogenous CA in MS. Panel A. In healthy subjects, lymphocytes express DRs, and produce and store CAs. Cell stimulation results in increased intracellular CAs, which can act as autocrine/paracrine transmitters. D1-like DR (mainly inhibitory) and D2-like DR (mainly stimulatory) modulate cell activation processes. Intracellular CAs contribute to the regulation of activation-induced apoptosis. CD4+ CD25high T cells produce endogenous dopamine, which subserves an inhibitory loop, resulting in suppression of their regulatory functions. Panel B. In MS patients, dysregulation of DRs and of endogenous CAs occur at several levels: 1 D1-like DRs are reduced and D2-like DRs are increased; 2. D2-like DR stimulation of cell function prevails; 3. TH is downregulated, and the production of dopamine, noradrenaline and adrenaline is impaired, possibly resulting in reduced activation-induced apoptosis (3a) and reduced release, consequently with reduced effects on neighboring cells (3b); 4 CD4+CD25high T cells overexpress D1-like DRs as well as TH, possibly resulting in increased dopamine production, and enhanced activity of the auto-inhibitory loop (for further details, see “Part 6” and Table 2)
MAO inhibitors
The non-selective and irreversible MAO inhibitor phenelzine reduces the clinical severity of EAE, and improves the exploratory behavior in mice without affecting the infiltration of CD4+ T cells into the spinal cord. Treatment with phenelzine is associated with higher levels of dopamine, as well as GABA and noradrenaline in the brain and spinal cord (Benson et al. 2013).
Part 10: Concluding remarks
Dopamine has direct and potent effects in many types of immune cells, particularly T cells of several types and subtypes. These dopamine-induced effects are mediated by functional DRs expressed on the cell surface of T cells and of other immune cells. Dopamine on its own, at low physiological concentration usually activate s resting human Teffs, and triggers various very important T cell functions. Yet, dopamine suppresses activated Teffs. On top of that, dopamine suppresses the suppressors, i.e., suppresses Tregs, and by doing so activates Teffs. Immune cells also produce dopamine. The effects of dopamine on T cells, the expression of DRs in T cells, and the production of dopamine in T cells are highly dynamic and context-sensitive, and vary between T cells types, and between different conditions. Moreover, dopamine-induced effects, and/or DR expression, and/or dopamine production in T cells are abnormal in certain human diseases and their animal models, and sometimes restored to normal values upon successful treatment of the disease. This seems to be the case in MS and EAE. Thus, an impressive amount of experimental preclinical and clinical data supports the immune modulating effects of dopamine and its receptors and their role in EAE and MS. Dopaminergic agents have been shown to be effective therapeutics for EAE in several animal models. It is, therefore, quite disappointing that the few trials of dopaminergic agents in MS patients provide no evidence of clinical benefit.
In this regard, however, a key finding in recent studies, at least in relapsing-remitting MS, is that dopaminergic pathways are extensively dysregulated, with a prevalence of D2-like DR-dependent pro-inflammatory effects on Teffs, and D1-like DR-induced inhibition of Tregs, which as a consequence possibly fail in their role of anti-inflammatory cells (Table 2). Interestingly, therapy of MS patients with IFN-β has been shown to “reset” dopaminergic pathways in lymphocytes, apparently reestablishing the optimal conditions for the exploitation of the therapeutic potential of dopaminergic agonists.
There is a wide array of directly and indirectly acting dopaminergic agents currently used for various non-immune indications, with a usually favorable therapeutic index (Cosentino and Marino 2013). Dopamine agonists selective for D1-like receptors (e.g., fenoldopam), or D2-like receptors (e.g., pramipexole), or active on both D1- and D2-like receptors (e.g., rotigotine) are currently used in therapeutics for various indications, and some of them have been already shown to exert immune effects on T cells (see Table 1). Some of these dopaminergic drugs could be potentially relevant for MS treatments. Whether D1- or D2-like receptor agonists might be preferred is still a matter of debate. However, available evidence seems to suggest that beneficial effects in MS might come preferentially from D1-like rather than D2-like receptor activation (Marino and Cosentino 2016). Anyway, the time is coming for clinical trials aimed at testing dopaminergic agonists in association with conventional first-line immunomodulating agents like IFN-β, with the aim to improve their efficacy without serious adverse reactions.
Abbreviations
- L-DOPA:
-
3,4-Dihydroxyphenylalanine
- CAs:
-
Catecholamines
- DCs:
-
Dendritic cells
- DR:
-
Dopamine receptor
- EAE:
-
Experimental autoimmune encephalomyelitis
- MS:
-
Multiple sclerosis
- PBMCs:
-
Peripheral blood mononuclear cells
- PBLs:
-
Peripheral blood lymphocytes
- TH:
-
Tyrosine hydroxylase
- NK cells:
-
Natural killer cells
- PD:
-
Parkinson’s disease
- SLE:
-
Systemic lupus erythematosus
- Teff:
-
Effector T cell
- Treg:
-
Regulatory T cell
- CSF:
-
Cerebrospinal fluid
- RA:
-
Rheumatoid arthritis
References
Alberio T, Pippione AC, Comi C, Olgiati S, Cecconi D, Zibetti M, Lopiano L, Fasano M (2012) Dopaminergic therapies modulate the T-CELL proteome of patients with Parkinson’s disease. IUBMB Life 64(10):846–852
Balkowiec-Iskra E, Kurkowska-Jastrzebska I, Joniec I, Czlonkowska A, Czlonkowski A (2003) Post intoxicative therapeutic immunization with myelin oligodendrocyte glycoproteine (MOG 35–55) suppresses spontaneous regeneration of dopaminergic neurons injured with 1-methyl-4 phenyl-1,2,3,6-tetrahydropiridine (MPTP). Acta Neurobiol Exp (Wars) 63(2):109–115
Bałkowiec-Iskra E, Kurkowska-Jastrzebska I, Joniec I, Ciesielska A, Członkowska A, Członkowski A (2007a) Dopamine, serotonin and noradrenaline changes in the striatum of C57BL mice following myelin oligodendrocyte glycoprotein (MOG) 35-55 and complete Freund adjuvant (CFA) administration. Acta Neurobiol Exp (Wars) 67(4):379–388
Bałkowiec-Iskra E, Kurkowska-Jastrzebska I, Joniec I, Ciesielska A, Muszynska A, Przybyłkowski A, Członkowska A, Członkowski A (2007b) MPTP-induced central dopamine depletion exacerbates experimental autoimmune encephalomyelitis (EAE) in C57BL mice. Inflamm Res 56(8):311–317
Barbanti P, Fabbrini G, Ricci A, Bruno G, Cerbo R, Bronzetti E, Amenta F, Luigi Lenzi G (2000) Reduced density of dopamine D2-like receptors on peripheral blood lymphocytes in Alzheimer’s disease. Mech Ageing Dev 120(1–3):65–75
Barili P, Bronzetti E, Felici L, Ferrante F, Ricci A, Zaccheo D, Amenta F (1996) Age-dependent changes in the expression of dopamine receptor subtypes in human peripheral blood lymphocytes. J Neuroimmunol 71(1–2):45–50
Bas J, Calopa M, Mestre M, Molleví DG, Cutillas B, Ambrosio S, Buendia E (2001) Lymphocyte populations in Parkinson’s disease and in rat models of parkinsonism. J Neuroimmunol 113(1):146–152
Basu B, Sarkar C, Chakroborty D, Ganguly S, Shome S, Dasgupta PS, Basu S (2010) D1 and D2 dopamine receptor-mediated inhibition of activated normal T cell proliferation is lost in jurkat T leukemic cells. J Biol Chem 285(35):27026–27032
Beaulieu JM, Espinoza S, Gainetdinov RR (2015) Dopamine receptors—IUPHAR Review 13. Br J Pharmacol 172(1):1–23
Benner EJ, Banerjee R, Reynolds AD, Sherman S, Pisarev VM, Tsiperson V, Nemachek C, Ciborowski P, Przedborski S, Mosley RL, Gendelman HE (2008) Nitrated alpha-synuclein immunity accelerates degeneration of nigral dopaminergic neurons. PLoS One 3(1):e1376
Benson CA, Wong G, Tenorio G, Baker GB, Kerr BJ (2013) The MAO inhibitor phenelzine can improve functional outcomes in mice with established clinical signs in experimental autoimmune encephalomyelitis (EAE). Behav Brain Res 252:302–311
Bergquist J, Silberring J (1998) Identification of catecholamines in the immune system by electrospray ionization mass spectrometry. Rapid Commun Mass Spectrom 12(11):683–688
Bergquist J, Tarkowski A, Ekman R, Ewing A (1994) Discovery of endogenous catecholamines in lymphocytes and evidence for catecholamine regulation of lymphocyte function via an autocrine loop. Proc Natl Acad Sci USA 91(26):12912–12916
Bergquist J, Josefsson E, Tarkowski A, Ekman R, Ewing A (1997) Measurements of catecholamine-mediated apoptosis of immunocompetent cells by capillary electrophoresis. Electrophoresis 18(10):1760–1766
Bergquist J, Ohlsson B, Tarkowski A (2000) Nuclear factor-kappa B is involved in the catecholaminergic suppression of immunocompetent cells. Ann N Y Acad Sci 917:281–289
Berne-Fromell K, Fromell H, Lundkvist S, Lundkvist P (1987) Is multiple sclerosis the equivalent of Parkinson’s disease for noradrenaline? Med Hypotheses 23(4):409–415
Besser MJ, Ganor Y, Levite M (2005) Dopamine by itself activates either D2, D3 or D1/D5 dopaminergic receptors in normal human T-cells and triggers the selective secretion of either IL-10. TNFalpha or both. J Neuroimmunol 169(1–2):161–171
Bissay V, De Klippel N, Herroelen L, Schmedding E, Buisseret T, Ebinger G, De Keyser J (1994) Bromocriptine therapy in multiple sclerosis: an open label pilot study. Clin Neuropharmacol 17(5):473–476
Blandini F, Bazzini E, Marino F, Saporiti F, Armentero MT, Pacchetti C, Zangaglia R, Martignoni E, Lecchini S, Nappi G, Cosentino M (2009) Calcium homeostasis is dysregulated in parkinsonian patients with L-DOPA-induced dyskinesias. Clin Neuropharmacol 32(3):133–139
Boneberg EM, von Seydlitz E, Pröpster K, Watzl H, Rockstroh B, Illges H (2006) D3 dopamine receptor mRNA is elevated in T cells of schizophrenic patients whereas D4 dopamine receptor mRNA is reduced in CD4+-T cells. J Neuroimmunol 173(1–2):180–187
Brito-Melo GE, Nicolato R, de Oliveira AC, Menezes GB, Lélis FJ, Avelar RS, Sá J, Bauer ME, Souza BR, Teixeira AL, Reis HJ (2012) Increase in dopaminergic, but not serotoninergic, receptors in T-cells as a marker for schizophrenia severity. J Psychiatr Res 46(6):738–742
Carr L, Tucker A, Fernandez-Botran R (2003) In vivo administration of L-dopa or dopamine decreases the number of splenic IFN gamma-producing cells. J Neuroimmunol 137(1–2):87–93
Clark C, Woodson MM, Winge VB, Nagasawa HT (1989) The antiviral drug amantadine has a direct inhibitory effect on T-lymphocytes. Immunopharmacology 18:195–204
Clark C, Woodson MM, Nagasawa HT (1991) Inhibition of lymphocyte proliferation by amantadine and its isomer, 2-aminoadamantane; impact on Lyt-2 + T cells while sparing L3T4+ T cells. Immunopharmacology 21:41–50
Cook-Mills JM, Cohen RL, Perlman RL, Chambers DA (1995) Inhibition of lymphocyte activation by catecholamines: evidence for a non-classical mechanism of catecholamine action. Immunology 85(4):544–549
Cosentino M, Marino F (2013) Adrenergic and dopaminergic modulation of immunity in multiple sclerosis: teaching old drugs new tricks? J Neuroimmune Pharmacol 8(1):163–179
Cosentino M, Zaffaroni M, Marino F, Bombelli R, Ferrari M, Rasini E, Lecchini S, Ghezzi A, Frigo G (2002) Catecholamine production and tyrosine hydroxylase expression in peripheral blood mononuclear cells from multiple sclerosis patients: effect of cell stimulation and possible relevance for activation-induced apoptosis. J Neuroimmunol 133(1–2):233–240
Cosentino M, Zaffaroni M, Ferrari M, Marino F, Bombelli R, Rasini E, Frigo G, Ghezzi A, Comi G, Lecchini S (2005) Interferon-gamma and interferon-beta affect endogenous catecholamines in human peripheral blood mononuclear cells: implications for multiple sclerosis. J Neuroimmunol 162(1–2):112–121
Cosentino M, Fietta AM, Ferrari M, Rasini E, Bombelli R, Carcano E, Saporiti F, Meloni F, Marino F, Lecchini S (2007) Human CD4+ CD25+ regulatory T cells selectively express tyrosine hydroxylase and contain endogenous catecholamines subserving an autocrine/paracrine inhibitory functional loop. Blood 109(2):632–642
Cosentino M, Colombo C, Mauri M, Ferrari M, Corbetta S, Marino F, Bono G, Lecchini S (2009) Expression of apoptosis-related proteins and of mRNA for dopaminergic receptors in peripheral blood mononuclear cells from patients with Alzheimer disease. Alzheimer Dis Assoc Disord 23(1):88–90
Cosentino M, Zaffaroni M, Trojano M, Giorelli M, Pica C, Rasini E, Bombelli R, Ferrari M, Ghezzi A, Comi G, Livrea P, Lecchini S, Marino F (2012) Dopaminergic modulation of CD4 + CD25(high) regulatory T lymphocytes in multiple sclerosis patients during interferon-beta therapy. NeuroImmunoModulation 19(5):283–292
Cosentino M, Zaffaroni M, Marino F (2014) Levels of mRNA for dopaminergic receptor D5 in circulating lymphocytes may be associated with subsequent response to interferon-β in patients with multiple sclerosis. J Neuroimmunol 277(1–2):193–196
Davids E, Hartwig U, Gastpar M (2004) Antipsychotic treatment of psychosis associated with multiple sclerosis. Prog Neuropsychopharmacol Biol Psychiatry 28(4):743–744
Dijkstra CD, van der Voort ER, De Groot CJ, Huitinga I, Uitdehaag BM, Polman CH, Berkenbosch F (1994) Therapeutic effect of the D2-dopamine agonist bromocriptine on acute and relapsing experimental allergic encephalomyelitis. Psychoneuroendocrinology 19(2):135–142
Fanciulli A, Misasi R, Campanelli D, Buttarelli FR, Pontieri FR (2011) Dopaminergic drug-induced modulation of the expression of the dopamine transporter in peripheral blood lymphocytes in Parkinson’s disease. Pharmacol Rep 63:1056–1060
Ferrari M, Cosentino M, Marino F, Bombelli R, Rasini E, Lecchini S, Frigo G (2004) Dopaminergic D1-like receptor-dependent inhibition of tyrosine hydroxylase mRNA expression and catecholamine production in human lymphocytes. Biochem Pharmacol 67(5):865–873
Ferreira TB, Kasahara TM, Barros PO, Vieira MM, Bittencourt VC, Hygino J, Andrade RM, Linhares UC, Andrade AF, Bento CA (2011) Dopamine up-regulates Th17 phenotype from individuals with generalized anxiety disorder. J Neuroimmunol 238(1–2):58–66
Fiszer U (2001) Does Parkinson’s disease have an immunological basis? The evidence and its therapeutic implications. BioDrugs 15(6):351–355
Fiszer U, Mix E, Fredrikson S, Kostulas V, Link H (1994) Parkinson’s disease and immunological abnormalities: increase of HLA-DR expression on monocytes in cerebrospinal fluid and of CD45RO+ T cells in peripheral blood. Acta Neurol Scand 90(3):160–166
Flierl MA, Rittirsch D, Nadeau BA, Chen AJ, Sarma JV, Zetoune FS, McGuire SR, List RP, Day DE, Hoesel LM, Gao H, Van Rooijen N, Huber-Lang MS, Neubig RR, Ward PA (2007) Phagocyte-derived catecholamines enhance acute inflammatory injury. Nature 449(7163):721–725
Flierl MA, Rittirsch D, Nadeau BA, Sarma JV, Day DE, Lentsch AB, Huber-Lang MS, Ward PA (2009) Upregulation of phagocyte-derived catecholamines augments the acute inflammatory response. PLoS One 4(2):e4414
Gade-Andavolu R, MacMurray JP, Blake H, Muhleman D, Tourtellotte W, Comings DE (1998) Association between the gamma-aminobutyric acid A3 receptor gene and multiple sclerosis. Arch Neurol 55(4):513–516
Gaskill PJ, Calderon TM, Luers AJ, Eugenin EA, Javitch JA, Berman JW (2009) Human immunodeficiency virus (HIV) infection of human macrophages is increased by dopamine: a bridge between HIV-associated neurologic disorders and drug abuse. Am J Pathol 175(3):1148–1159
Gentile A, Fresegna D, Federici M, Musella A, Rizzo FR, Sepman H, Bullitta S, De Vito F, Haji N, Rossi S, Mercuri NB, Usiello A, Mandolesi G, Centonze D (2015) Dopaminergic dysfunction is associated with IL-1beta-dependent mood alterations in experimental autoimmune encephalomyelitis. Neurobiol Dis 74:347–358
Ghosh MC, Mondal AC, Basu S, Banerjee S, Majumder J, Bhattacharya D, Dasgupta PS (2003) Dopamine inhibits cytokine release and expression of tyrosine kinases, Lck and Fyn in activated T cells. Int Immunopharmacol 3(7):1019–1026
Giorelli M, Livrea P, Trojano M (2005) Dopamine fails to regulate activation of peripheral blood lymphocytes from multiple sclerosis patients: effects of IFN-beta. J Interferon Cytokine Res 25(7):395–406
Hisanaga K, Asagi M, Itoyama Y, Iwasaki Y (2001) Increase in peripheral CD4 bright+ CD8 dull+ T cells in Parkinson disease. Arch Neurol 58(10):1580–1583
Huang Y, Qiu AW, Peng YP, Liu Y, Huang HW, Qiu YH (2010) Roles of dopamine receptor subtypes in mediating modulation of T lymphocyte function. Neuro Endocrinol Lett 31(6):782–791
Huber TJ, Dietrich DE, Emrich HM (1999) Possible use of amantadine in depression. Pharmacopsychiatry 32(2):47–55
Hussain T, Lokhandwala MF (2003) Renal dopamine receptors and hypertension. Exp Biol Med (Maywood) 228(2):134–142
Ilani T, Ben-Shachar D, Strous RD, Mazor M, Sheinkman A, Kotler M, Fuchs S (2001) A peripheral marker for schizophrenia: increased levels of D3 dopamine receptor mRNA in blood lymphocytes. Proc Natl Acad Sci USA 98(2):625–628
Ilani T, Strous RD, Fuchs S (2004) Dopaminergic regulation of immune cells via D3 dopamine receptor: a pathway mediated by activated T cells. Faseb J 18(13):1600–1602
Iversen SD, Iversen LL (2007) Dopamine: 50 years in perspective. Trends Neurosci 30(5):188–193
Jafari M, Ahangari G, Saberi M, Samangoui S, Torabi R, Zouali M (2013) Distorted expression of dopamine receptor genes in systemic lupus erythematosus. Immunobiology 218(7):979–983
Josefsson E, Bergquist J, Ekman R, Tarkowski A (1996) Catecholamines are synthesized by mouse lymphocytes and regulate function of these cells by induction of apoptosis. Immunology 88(1):140–146
Karpus WJ, Konkol RJ, Killen JA (1988) Central catecholamine neurotoxin administration. 1. Immunological changes associated with the suppression of experimental autoimmune encephalomyelitis. J Neuroimmunol 18(1):61–73
Kipnis J, Cardon M, Avidan H, Lewitus GM, Mordechay S, Rolls A, Shani Y, Schwartz M (2004) Dopamine, through the extracellular signal-regulated kinase pathway, downregulates CD4+ CD25+ regulatory T-cell activity: implications for neurodegeneration. J Neurosci 24(27):6133–6143
Kira J, Harada M, Yamaguchi Y, Shida N, Goto I (1991) Hyperprolactinemia in multiple sclerosis. J Neurol Sci 102(1):61–66
Konkol RJ, Wesselmann U, Karpus WJ, Leo GL, Killen JA, Roerig DL (1990) Suppression of clinical weakness in experimental autoimmune encephalomyelitis associated with weight changes, and post-decapitation convulsions after intracisternal-ventricular administration of 6-hydroxydopamine. J Neuroimmunol 26(1):25–34
Kuric E, Ruscher K (2014) Reduction of rat brain CD8(+) T-cells by levodopa/benserazide treatment after experimental stroke. Eur J Neurosci 40:2463–2470
Kurkowska-Jastrzebska I, Wronska A, Kohutnicka M, Czlonkowski A, Czlonkowska A (1999) The inflammatory reaction following 1-methyl-4-phenyl-1,2,3, 6-tetrahydropyridine intoxication in mouse. Exp Neurol 156(1):50–61
Kustrimovic N, Rasini E, Legnaro M, Marino F, Cosentino M (2014) Expression of dopaminergic receptors on human CD4 + T lymphocytes: flow cytometric analysis of naive and memory subsets and relevance for the neuroimmunology of neurodegenerative disease. J Neuroimmune Pharmacol 9(3):302–312
Kwak YT, Koo MS, Choi CH, Sunwoo I (2001) Change of dopamine receptor mRNA expression in lymphocyte of schizophrenic patients. BMC Med Genet 2:3
Levite M (2008) Neurotransmitters activate T-cells and elicit crucial functions via neurotransmitter receptors. Curr Opin Pharmacol 8(4):460–471
Levite M (2012) Dopamine in the Immune System: Dopamine Receptors in Immune Cells, Potent Effects, Endogenous Production and Involvement in Immune and Neuropsychiatric Diseases. Nerve Driven Immunity: Neurotransmitters and Neuropeptides in the Immune System. Springer, Vienna, pp 1–45
Levite M (2016) Dopamine and T cells: dopamine receptors and potent effects on T cells, dopamine production in T cells, and abnormalities in the dopaminergic system in T cells in autoimmune, neurological and psychiatric diseases. Acta Physiol (Oxf) 216(1):42–89
Levite M, Chowers Y, Ganor Y, Besser M, Hershkovits R, Cahalon L (2001) Dopamine interacts directly with its D3 and D2 receptors on normal human T cells, and activates beta1 integrin function. Eur J Immunol 31(12):3504–3512
Marino F, Cosentino M (2016) Multiple sclerosis: repurposing dopaminergic drugs for MS - The evidence mounts. Nat Rev Neurol 12(4):191–192
Markianos M, Koutsis G, Evangelopoulos ME, Mandellos D, Karahalios G, Sfagos C (2009) Relationship of CSF neurotransmitter metabolite levels to disease severity and disability in multiple sclerosis. J Neurochem 108(1):158–164
McKenna F, McLaughlin PJ, Lewis BJ, Sibbring GC, Cummerson JA, Bowen-Jones D, Moots RJ (2002) Dopamine receptor expression on human T- and B-lymphocytes, monocytes, neutrophils, eosinophils and NK cells: a flow cytometric study. J Neuroimmunol 132(1–2):34–40
McMurray RW (2001) Bromocriptine in rheumatic and autoimmune diseases. Semin Arthritis Rheum 31(1):21–32
Meredith EJ, Holder MJ, Rosén A, Lee AD, Dyer MJ, Barnes NM, Gordon J (2006) Dopamine targets cycling B cells independent of receptors/transporter for oxidative attack: implications for non-Hodgkin’s lymphoma. Proc Natl Acad Sci USA 103(36):13485–13490
Miyara M, Gorochov G, Ehrenstein M, Musset L, Sakaguchi S, Amoura Z (2011) Human FoxP3+ regulatory T cells in systemic autoimmune diseases Autoimmun Rev 10(12):744–755
Mori T, Kabashima K, Fukamachi S, Kuroda E, Sakabe J, Kobayashi M, Nakajima S, Nakano K, Tanaka Y, Matsushita S, Nakamura M, Tokura Y (2013) D1-like dopamine receptors antagonist inhibits cutaneous immune reactions mediated by Th2 and mast cells. J Dermatol Sci 71(1):37–44
Morikawa K, Oseko F, Morikawa S (1994) Immunosuppressive activity of bromocriptine on human T lymphocyte function in vitro. Clin Exp Immunol 95:514–518
Musso NR, Brenci S, Setti M, Indiveri F, Lotti G (1996) Catecholamine content and in vitro catecholamine synthesis in peripheral human lymphocytes. J Clin Endocrinol Metab 81(10):3553–3557
Musso NR, Brenci S, Indiveri F, Lotti G (1997) L-tyrosine and nicotine induce synthesis of L-Dopa and norepinephrine in human lymphocytes. J Neuroimmunol 74(1–2):117–120
Nagai Y, Ueno S, Saeki Y, Soga F, Hirano M, Yanagihara T (1996) Decrease of the D3 dopamine receptor mRNA expression in lymphocytes from patients with Parkinson’s disease. Neurology 46(3):791–795
Nakagome K, Imamura M, Okada H, Kawahata K, Inoue T, Hashimoto K, Harada H, Higashi T, Takagi R (2011) Dopamine D1-like receptor antagonist attenuates Th17-mediated immune response and ovalbumin antigen-induced neutrophilic airway inflammation. J Immunol 186(10):5975–5982
Nakano K, Matsushita S (2007) The immunomodulatory effect of dopamine. Arerugi 56(7):679–684
Nakano K, Higashi T, Hashimoto K, Takagi R, Tanaka Y, Matsushita S (2008) Antagonizing dopamine D1-like receptor inhibits Th17 cell differentiation: preventive and therapeutic effects on experimental autoimmune encephalomyelitis. Biochem Biophys Res Commun 373(2):286–291
Nakano K, Higashi T, Takagi R, Hashimoto K, Tanaka Y, Matsushita S (2009a) Dopamine released by dendritic cells polarizes Th2 differentiation. Int Immunol 21(6):645–654
Nakano K, Matsushita S, Saito K, Yamaoka K, Tanaka Y (2009b) Dopamine as an immune-modulator between dendritic cells and T cells and the role of dopamine in the pathogenesis of rheumatoid arthritis. Nihon Rinsho Meneki Gakkai Kaishi 32(1):1–6
Nakano K, Yamaoka K, Hanami K, Saito K, Sasaguri Y, Yanagihara N, Tanaka S, Katsuki I, Matsushita S, Tanaka Y (2011) Dopamine induces IL-6-dependent IL-17 production via D1-like receptor on CD4 naive T cells and D1-like receptor antagonist SCH-23390 inhibits cartilage destruction in a human rheumatoid arthritis/SCID mouse chimera model. J Immunol 186(6):3745–3752
Nakashioya H, Nakano K, Watanabe N, Miyasaka N, Matsushita S, Kohsaka H (2011) Therapeutic effect of D1-like dopamine receptor antagonist on collagen-induced arthritis of mice. Mod Rheumatol 21(3):260–266
O’Sullivan D, Green L, Stone S, Zareie P, Kharkrang M, Fong D, Connor B, La Flamme AC (2014) Treatment with the antipsychotic agent, risperidone, reduces disease severity in experimental autoimmune encephalomyelitis. PLoS One 9(8):e104430
Pacheco R, Prado CE, Barrientos MJ, Bernales S (2009) Role of dopamine in the physiology of T-cells and dendritic cells. J Neuroimmunol 216(1–2):8–19
Pacheco R et al. (2014a) Dopaminergic regulation of T-cell mediated response involved in Multiple Sclerosis and Parkinson’s disease. Abstract of talk in 2nd International Nerve-Driven Immunity meeting, Stockhom. http://ndimeetings.org/previous-meetings/. Accessed 20 August 2014
Pacheco R, Contreras F, Zouali M (2014) The dopaminergic system in autoimmune diseases. Front Immunol 5:117
Prado C, Contreras F, González H, Díaz P, Elgueta D, Barrientos M, Herrada AA, Lladser Á, Bernales S, Pacheco R (2012) Stimulation of dopamine receptor D5 expressed on dendritic cells potentiates Th17-mediated immunity. J Immunol 188(7):3062–3070
Qiu YH, Peng YP, Jiang JM, Wang JJ (2004) Expression of tyrosine hydroxylase in lymphocytes and effect of endogenous catecholamines on lymphocyte function. NeuroImmunoModulation 11(2):75–83
Reynolds AD, Stone DK, Mosley RL, Gendelman HE (2009) Nitrated (Alberio et al.)-synuclein-induced alterations in microglial immunity are regulated by CD4+ T cell subsets. J Immunol 182(7):4137–4149
Ricci A, Bronzetti E, Felici L, Tayebati SK, Amenta F (1997a) Dopamine D4 receptor in human peripheral blood lymphocytes: a radioligand binding assay study. Neurosci Lett 229(2):130–134
Ricci A, Mariotta S, Greco S, Bisetti A (1997b) Expression of dopamine receptors in immune organs and circulating immune cells. Clin Exp Hypertens 19(1–2):59–71
Ricci A, Bronzetti E, Mignini F, Tayebati SK, Zaccheo D, Amenta F (1999) Dopamine D1-like receptor subtypes in human peripheral blood lymphocytes. J Neuroimmunol 96(2):234–240
Riskind PN, Massacesi L, Doolittle TH, Hauser SL (1991) The role of prolactin in autoimmune demyelination: suppression of experimental allergic encephalomyelitis by bromocriptine. Ann Neurol 29(5):542–547
Rocc P, De Leo C, Eva C, Marchiaro L, Milani AM, Musso R, Ravizza L, Zanalda E, Bogetto F (2002) Decrease of the D4 dopamine receptor messenger RNA expression in lymphocytes from patients with major depression. Prog Neuropsychopharmacol Biol Psychiatry 26(6):1155–1160
Saha B, Mondal AC, Majumder J, Basu S, Dasgupta PS (2001a) Physiological concentrations of dopamine inhibit the proliferation and cytotoxicity of human CD4+ and CD8+ T cells in vitro: a receptor-mediated mechanism. NeuroImmunoModulation 9(1):23–33
Saha B, Mondal AC, Basu S, Dasgupta PS (2001b) Circulating dopamine level, in lung carcinoma patients, inhibits proliferation and cytotoxicity of CD4+ and CD8+ T cells by D1 dopamine receptors: an in vitro analysis. Int Immunopharmacol 1(7):1363–1374
Sailer M, Heinze HJ, Schoenfeld MA, Hauser U, Smid HG (2000) Amantadine influences cognitive processing in patients with multiple sclerosis. Pharmacopsychiatry 33(1):28–37
Sakaguchi S (2011) Regulatory T cells: history and perspective. Methods Mol Biol 707:3–17
Santambrogio L, Lipartiti M, Bruni A, Dal Toso R (1993) Dopamine receptors on human T- and B-lymphocytes. J Neuroimmunol 45(1–2):113–119
Sarkar C, Das S, Chakroborty D, Chowdhury UR, Basu B, Dasgupta PS, Basu S (2006) Cutting Edge: stimulation of dopamine D4 receptors induce T cell quiescence by up-regulating Kruppel-like factor-2 expression through inhibition of ERK1/ERK2 phosphorylation. J Immunol 177(11):7525–7529
Sarkar C, Basu B, Chakroborty D, Dasgupta PS, Basu S (2010) The immunoregulatory role of dopamine: an update. Brain Behav Immun 24(4):525–528
Saussez S, Laumbacher B, Chantrain G, Rodriguez A, Gu S, Wank R, Levite M (2014) Towards neuroimmunotherapy for cancer: the neurotransmitters glutamate, dopamine and GnRH-II augment substantially the ability of T cells of few head and neck cancer patients to perform spontaneous migration, chemotactic migration and migration towards the autologous tumor, and also elevate markedly the expression of CD3zeta and CD3epsilon TCR-associated chains. J Neural Transm 121(8):1007–1027
Strell C, Sievers A, Bastian P, Lang K, Niggemann B, Zänker KS, Entschladen F (2009) Divergent effects of norepinephrine, dopamine and substance P on the activation, differentiation and effector functions of human cytotoxic T lymphocytes. BMC Immunol. 8(10):62
Tabaddor K, Wolfson LI, Sharpless NS (1978) Ventricular fluid homovanillic acid and 5-hydroxyindoleacetic acid concentrations in patients with movement disorders. Neurology 28(12):1249–1253
Tsao CW, Lin YS, Cheng JT (1998) Inhibition of immune cell proliferation with haloperidol and relationship of tyrosine hydroxylase expression to immune cell growth. Life Sci 62(21):PL335–PL344
Venken K, Hellings N, Liblau R, Stinissen P (2010) Disturbed regulatory T cell homeostasis in multiple sclerosis. Trends Mol Med 16(2):58–68
Wandinger KP, Hagenah JM, Klüter H, Rothermundt M, Peters M, Vieregge P (1999) Effects of amantadine treatment on in vitro production of interleukin-2 in de-novo patients with idiopathic Parkinson’s disease. J Neuroimmunol 98(2):214–220
Watanabe Y, Nakayama T, Nagakubo D, Hieshima K, Jin Z, Katou F, Hashimoto K, Yoshie O (2006) Dopamine selectively induces migration and homing of naive CD8+ T cells via dopamine receptor D3. J Immunol 176(2):848–856
White SR, Bhatnagar RK, Bardo MT (1983) Norepinephrine depletion in the spinal cord gray matter of rats with experimental allergic encephalomyelitis. J Neurochem 40(6):1771–1773
Zaffaroni M, Marino F, Bombelli R, Rasini E, Monti M, Ferrari M, Ghezzi A, Comi G, Lecchini S, Cosentino M (2008) Therapy with interferon-beta modulates endogenous catecholamines in lymphocytes of patients with multiple sclerosis. Exp Neurol 214(2):315–321
Zhao W, Huang Y, Liu Z, Cao BB, Peng YP, Qiu YH (2013) Dopamine receptors modulate cytotoxicity of natural killer cells via cAMP-PKA-CREB signaling pathway. PLoS One 8(6):e65860
Zozulya AL, Wiendl H (2008) The role of regulatory T cells in multiple sclerosis. Nat Clin Pract Neurol 4(7):384–398
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Levite, M., Marino, F. & Cosentino, M. Dopamine, T cells and multiple sclerosis (MS). J Neural Transm 124, 525–542 (2017). https://doi.org/10.1007/s00702-016-1640-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-016-1640-4