Abstract
On June 2008, the European Medicines Agency (EMA) introduced changes to the Summary of Product Characteristics (SPC) for cabergoline and pergolide, to reduce the risk of cardiac valvulopathy in users of these drugs. To assess the effectiveness of EMA recommendations in Italian clinical practice, we retrospectively reviewed medical charts of patients with degenerative Parkinsonism treated with cabergoline in three large Italian clinics between January 2006 and June 2012. The prevalence and the severity of cardiac valve regurgitation were assessed in patients who stopped cabergoline therapy prior to June 2008 or continued therapy after that date. In addition, the proportion of patients undergoing echocardiographic examination in each cohort was evaluated. A total of 61 patients were available for evaluation. The proportion of patients who underwent a baseline echocardiographic examination increased from 64 % in the period before the 2008 SPC changes to 71 % among those who continued treatment after that date. However, only 18 and 29 % of patients underwent at least two echocardiographic examinations during the pre-SPC and cross-SPC change period, respectively. No severe cardiac valve regurgitation was documented in any of the study patients using cabergoline either prior or after 26th June 2008. Our findings show that the 2008 changes to the SPC resulted in an increase in physicians’ awareness of cabergoline-induced valvulopathy risk in Italy. However, only a small percentage of patients underwent serial echocardiography. Further efforts are needed to achieve better compliance with the prescribing guidelines for cabergoline treated patients in clinical practice.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
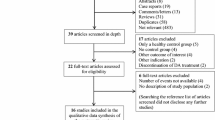
Treatment of Parkinson’s disease (PD) with the ergot-derived dopamine agonists (DAs) pergolide and cabergoline is known to be associated with a substantial risk of cardiac valve regurgitation (Rasmussen et al. 2008; Oeda et al. 2009; Steiger et al. 2009; Zanettini et al. 2007; Trifiro et al. 2012; Simonis et al. 2007; Van Camp et al. 2003; Antonini and Poewe 2007). Pergolide and cabergoline have high affinity to the 5-HT2B serotonin receptors, which are expressed in heart valves. Through the activation of these receptors, ergot-derived DAs might induce mitogenesis and, in turn, proliferation of fibroblasts, leading to valve fibrosis (Antonini and Poewe 2007). The fibrotic changes cause thickening, retraction, and stiffening of valves, which result in incomplete leaflet coaptation and clinically significant regurgitation. The association between cabergoline and valvular insufficiency was documented in a large body of scientific evidence, including case reports and series as well as prospective and retrospective observational studies (Schade et al. 2007; Zanettini et al. 2007; Rasmussen et al. 2008; Oeda et al. 2009; Steiger et al. 2009; Fietzek et al. 2012). Overall, the risk of cardiac valve fibrosis following therapy with ergot-derived DAs appears to be associated with the cumulative exposure to the drug (dose- and treatment duration-dependent), generally occurring after at least 6 months of treatment and usually with high daily dose in PD patients (Trifiro et al. 2012). Conversely, ergot-derived DAs usage in patients with hyperprolactinemia, who require about 10–20 times lower dosage of cabergoline, has not been associated with an increase in risk so far (Auriemma et al. 2013; Trifiro et al. 2012). In Italy, a first warning by the National Drug Agency (AIFA) concerning the risk of cabergoline-induced cardiac valvulopathy was issued in April 2007. Following this measure, the Summary of Product Characteristics (SPC) of cabergoline was modified to restrict cabergoline use in line with measures adopted for pergolide. Use of cabergoline and pergolide was restricted only as second-line therapy in PD patients intolerant or unresponsive to non-ergot derived DAs. Moreover, echocardiography examination was recommended before starting treatment with cabergoline/pergolide and regularly (every 6 months) during treatment to monitor the occurrence of cardiac valve fibrosis. In addition, the use of cabergoline was contraindicated in patients with evidence of heart valve problems or history of fibrosis. On June 26, 2008, the European Medicines Agency (EMA) required the manufacturers of cabergoline and pergolide to further restrict the use of these medications as a risk minimization measure (RMM) by making additional changes to the SPC (EMEA 2008). Along with the above-mentioned changes implemented in 2007, the 2008 SPC changes for cabergoline restricted the daily dose for the treatment of PD to a maximum of 3 mg per day and cardiac valve fibrosis was included in the SPC as a ‘a very common’ side effect. To date, few studies have investigated the effectiveness of the EMA recommendations to minimize the ergot-derived DA-related risks in clinical practice (Lledo et al. 2007; Nakaoka et al. 2011). In the study from Lledo et al. (2007) the authors performed a telephone survey of 244 neurologists in 12 European countries to explore physicians’ awareness of the pergolide SPC revisions and their resulting changes in clinical practice. Another study was performed in Japan to evaluate the impact of cabergoline SPC changes in clinical practice. As a follow-up to the 2008 SPC changes, the EMA requested that market authorization holders measure the compliance with and the effectiveness of RMMs for cabergoline in clinical practice. The “Study on Utilization of cabergoline for compliance with risk minimization activities” (SUCRE) was a post-approval safety study (PASS) carried out to comply with this regulatory request. The overall objectives of SUCRE were: first, to assess the compliance with the 2008 SPC changes for cabergoline, including second line usage for PD, maximum daily dose of 3 mg, and adherence to echocardiographic monitoring prior to and during treatment; and second, to assess the effectiveness of the 2008 SPC changes on the incidence and prevalence of cardiac valvulopathy. The compliance portion of SUCRE was carried out by conducting a retrospective cohort study using automated healthcare data from five databases in four European countries. This manuscript describes the results from the effectiveness portion of SUCRE, which was undertaken by abstracting data from medical charts of cabergoline users treated for PD in three large Italian clinical centres.
Methods
Setting
Three specialized neurological centres for the treatment of PD in Italy participated in this sub-study of SUCRE: (a) IRCCS Centro Neurolesi “Bonino Pulejo”, Messina; (b) IRCCS S. Raffaele Pisana, Rome; (c) Parkinson Institute, Istituti Clinici di Perfezionamento, Milan. These specialized neurological centres were selected because they provided the unique setting necessary to conduct the effectiveness portion of the SUCRE study, which required the collection of data from echocardiographic examinations in patients treated with cabergoline for PD and whose treatment was closely managed at these centres. Overall, more than 3,000 patients with PD and other neurodegenerative disorders are followed annually in these centres.
The SUCRE study protocol was submitted to the Ethical Committees of the respective centres and approved according to local laws and requirements.
Study population
All patients who were treated with cabergoline during the study period (1st January 2006–30th June 2012) and who could be retrospectively identified through medical chart review at these centres were included in the study. In detail, January 1, 2006 was chosen as the index date of the study to identify a pre-SPC period of approximately 2 years in length and during which prevalent users of cabergoline could be identified. Prevalent users were further divided into those whose treatment ended prior to the SPC changes in 2008 and those whose treatment continued after these changes. The end of the study period was June 30, 2012, to allow for at least 4 years of follow-up from the date of the SPC changes. No specific exclusion criteria were applied. For each patient, demographic and clinical information was collected using an electronic case report form (CRF), as described in the following section.
Data collection
A CRF was newly developed with the aim of facilitating and harmonizing the clinical data collection from different clinical centres through manual chart review. Anonymised data were collected locally by each centre using the electronic CRF and were automatically stored in a safe, remote research environment (RRE) at the Erasmus University Medical Center in Rotterdam. All the researchers in charge of data collection at each centre received remote training on how to utilize the CRF and store it in the RRE. Each recruiting centre received a token with personal credentials to access the CRF. This system allowed for safe data collection and storage from each centre while offering the opportunity to the principal investigator (PI) to monitor the quality of data collection. Each identified error or incomplete field was sent back to the specific recruiting centre for further checks. Once data collection from the three centres was completed, data were extracted and analysed. For all patients who were treated with cabergoline, investigators from the clinical centres retrospectively collected demographic and clinical data from the medical charts, as well as routine transthoracic echocardiographic examinations, which were available in the clinical centres. For each study patient, the following information was collected: unique patient identifier (ID), date of registration, age (at the date of registration), sex, current and prior PD medication history (type of drug, treatment start and stop date, daily and cumulative dose and duration), specific indication for use (e.g. diagnosis of PD or any other degenerative Parkinsonism) (Litvan et al. 2003), disease duration and severity (evaluated using Hoehn and Yahr stage and UPRDS scale), co-morbidities (e.g. hypertension, diabetes mellitus, hyperlipidemia, heart failure, history of myocardial infarction and cerebrovascular disease, peripheral arterial disease, chronic obstructive pulmonary disease and chronic kidney disease) and any potential alternative causes of cardiac valve regurgitation, including specific diseases (e.g. history of valvulopathy, rheumatic valve disease, history of pleural, pericardial, retroperitoneal fibrosis, bacterial endocarditis, carcinoid syndrome, congenital and autoimmune diseases such as SLE, and Marfan syndrome), and prior use of drugs known to induce fibrosis (i.e. pergolide, fenfluramine, amiodarone, ergotamine, phentermine, and methysergide). Occurrence of cardiac valve disorders was assessed through the evaluation of the echocardiographic examinations. Anonymised electronic copies (as pdf files) of echocardiographic examinations of the enrolled patients were uploaded to the RRE and carefully scrutinized. Collection of the exposure and outcome information is described in more detail in the following paragraph.
Exposure assessment
Among patients with diagnosis of PD (or Parkinsonism) who were registered in the three clinical centres, we identified a cohort of patients treated with cabergoline at any time during the study period. This cohort was divided into new users and prevalent users of cabergoline based on the date on which this drug was started. New users (post-SPC change users) were all subjects who received the first prescription of cabergoline after the June 26th, 2008 SPC changes were implemented. Prevalent users were all cohort members who started cabergoline treatment prior to these SPC changes. The latter group of cabergoline users was further divided into those who stopped therapy prior to June 26th, 2008 (pre-SPC change users) and those who continued therapy with cabergoline after that date (cross-SPC change users).
Outcome ascertainment
For each cabergoline user, all echocardiographic examinations that were performed during the study period were retrieved and analysed. Each patient’s echocardiographic examinations were assigned the same patient ID as was given to the patient for identification purposes and were uploaded to the RRE. For each echocardiography the following information was collected: (a) date of examination; (b) type of valve disorder (if any); (c) valve affected by the lesion; (d) clinical manifestation (i.e. regurgitation, stenosis, prolapse) and type of lesion (i.e. fibrosis, sclerosis, and calcification); (e) degree of certainty of the valvulopathy (possible, definite); and (f) severity of the lesion with grading from 1 to 3, based on parameters of regurgitation volume, fraction and effective regurgitation orifice using valve-specific limits following practice recommendations of the American Society of Echocardiography (Zoghbi et al. 2003). Severity of valve regurgitation has been routinely classified as normal (grade 0), mild (grade 1), moderate (grade 2), and severe (grade 3) by each operator. As digital versions were not available for most of the echocardiographic examinations, the findings that were assigned by the operator who had conducted the echocardiographic examination were used.
Data analysis
Demographic and clinical characteristics of cabergoline users prior to and after June 26th, 2008 were evaluated at the first visit during the study period and reported as proportions (categorical variables) and means with standard deviation (continuous variables).
To measure the effectiveness of the new prescribing guidelines, the prevalence of cardiac valve regurgitation was assessed in the three cohorts. In addition, cumulative incidence was calculated for descriptive purposes only since there is no comparative incidence of cardiac valvulopathy prior to the 2008 SPC changes (as pre-treatment echocardiographic examinations were not yet a requirement). Therefore, changes in prevalence of cardiac valve regurgitation across the three cohorts were utilized as the main parameter to assess effectiveness of risk minimization measures in clinical practice. Additional data captured from each centre included the proportion of patients with at least one and two echocardiographic examinations, the total number and the mean number of echocardiographic examinations per patient and changes in prescribed dosages of cabergoline over time.
Prevalence of cardiac valve regurgitation
For each re-assessable echocardiographic examination, the grade and presence of mild, moderate, and severe valvulopathy in the mitral, aortic, tricuspidal, and pulmonary valves were assessed. The prevalence of any degree of valve regurgitation for each of the patient groups (pre-SPC change users, post-SPC change users and cross-SPC change users) was calculated as the number of patients with valve regurgitation divided by the number of patients with at least one echocardiographic examination conducted during cabergoline therapy. If a patient had more than one echocardiographic examination, the results of the most recent examination were used. The prevalence of mild/moderate/severe regurgitation was calculated in both incident and prevalent users. Effectiveness of the SPC changes was assessed by comparing the prevalence of regurgitation after the SPC changes in new users of cabergoline (post-SPC change users) with the prevalence of regurgitation in prevalent users (pre-SPC change users and cross-SPC change users), as defined above.
Incidence of valve regurgitation
In each of the three user groups, cumulative incidence of valve regurgitation was assessed among persons who underwent echocardiographic examinations prior to and during treatment with cabergoline with no evidence of valve damage at baseline (prior to the start of the cabergoline treatment).
Results
Overall, 61 patients (42 from Milan, 9 from Messina, and 10 from Rome) who were treated with cabergoline during the period January 1st, 2006–June 30th, 2012 were available for the study. The distribution of the number of enrolled patients across the three clinical centres reflects the size of the PD patients who are followed by these recruitment centres. The number of recruited cabergoline users is lower than the expected number (N = 80) due to the difficulty, especially in Messina and Rome, to retrieve retrospectively all the requested key clinical information about the cabergoline users through the medical chart review. Nevertheless, this is an exploratory study and in no way the final number of recruited patients affects the validity of the results. Demographic and clinical characteristics of cabergoline users who started treatment prior to (N = 59; 96.7 %) and after (N = 2; 3.3 %) the date of the SPC change (June 26th, 2008) are reported in Table 1. Patients who started cabergoline treatment prior to June 26th, 2008 were further categorized into those who discontinued therapy before the SPC changes (pre-SPC change users—N = 11; 18.6 % of total cabergoline users) and those who continued therapy after that date (cross-SPC change users—N = 48; 78.7 %). The total cohort was on average 63.3 years old and was mostly composed by males (75 %); no major differences in age and sex were observed among the three centres (data not shown). Most of the cabergoline users were affected by PD (97 %), with an average of more than 8 years of disease history at the initiation of cabergoline therapy. Pre-SPC change users had a higher degree of PD severity as compared to cross-SPC change users and the two post-SPC change users (as demonstrated by lower mean values of UPDS scale) when cabergoline was initiated. Overall, post-SPC change users (two patients who initiated cabergoline after June 26th, 2008) were younger than those who began treatment before that date and were healthier (no reported comorbidities). Hypertension, which is a risk factor for valve disorders, was the most frequently reported comorbidity among pre-SPC change cabergoline users. Overall, only two cabergoline users (3.4 %) were previously exposed to other potentially inducing fibrosis drugs prior to the start of cabergoline therapy. Dosage of cabergoline ranged from 1 to 6 mg/day at baseline (Table 2). The mean dosage was reduced in those who continued cabergoline treatment after SPC changes as compared to those who stopped therapy before them. Among the two post-SPC change users, one patient received dosages of cabergoline higher than 3 mg/day (i.e. 4 mg/day) as a starting dose. The maximum allowed daily dose for PD is 3 mg. Overall, 72.7 % of the pre-SPC change users discontinued treatment versus 54.2 % of the cross-SPC change users, while a similar proportion of patients in each group added another anti-Parkinson drug during the treatment with cabergoline. The dose of cabergoline was increased during the treatment in 27.3 % of the pre-SPC change users vs. 14.6 % of the cross-SPC change users.
Both patients (100 %) who began cabergoline treatment after June 26th, 2008 received baseline echocardiographic examination, while only 63.6 % of prevalent users did, with a slightly higher proportion among those who continued therapy after June 26th, 2008 (70.8 %) (Table 3). Only two patients among the pre-SPC change users underwent echocardiographic examinations both prior to the start and during the cabergoline treatment; among these, there was one documented case of valvulopathy occurring after the start of the cabergoline treatment. On the other hand, four cross-SPC users (57.1 %) reported mild valvulopathy after the start of cabergoline among a total of seven persons without evidence of valve damage at baseline (start of cabergoline treatment). Prevalence of valvulopathy was slightly reduced among those who continued treatment after June 26th, 2008 as compared to those who discontinued cabergoline treatments before this date (55.9 vs. 57.2 %). Among documented cases of valvulopathy, the majority affected the mitral valve (83.3 %) and in 37.5 % of cases fibrosis was reported. In pre-SPC users, 50 % of valve regurgitation was of mild degree and 50 % of moderate degree, while in the cross-SPC users the majority of valve regurgitation was of mild degree (84.2 %). No severe valve regurgitation was documented in any of the study patients using cabergoline either prior or after June 26th, 2008.
Discussion
To our knowledge, this is the first European observational study that explored the actual compliance and effectiveness of risk minimization measures for cardiac valvulopathy in association with cabergoline use in PD/Parkinsonism.
Our findings demonstrate that there was a moderate increase in the proportion of cabergoline users receiving baseline echocardiographic examination after the 2008 SPC changes as compared to before. However, less than one-third of cabergoline users who were treated both prior and after the 2008 SPC changes received both baseline and follow-up echocardiographic examinations. This suggests that the recommendations for baseline and follow-up (i.e., every 6 months) echocardiographic monitoring have been only partly implemented in the three Italian neurological centres. Regarding the RMMs in the SPC concerning the maximum allowable daily dose of 3 mg for PD, we noted that before the 2008 SPC changes, there was a tendency to progressively increase cabergoline dosages, probably in an effort to control extrapyramidal symptoms. After the 2008 SPC changes, we observed an opposite trend concerning dose reduction, probably, as a result of prescriber awareness of the SPC changes as a result of the dose dependency in the cabergoline-related risk of fibrosis.
In our study only two patients initiated treatment with cabergoline after the 2008 SPC changes during a 4-year time period. Interestingly, these patients were younger and healthier (no comorbidities were reported) as compared to those starting before the 2008 SPC changes. These results indicate that cabergoline is now rarely prescribed to PD patients, and if so only to healthier patients, as a number of safer alternative pharmacological options are available. A previous Italian drug utilization study carried out even before 2008 demonstrated a much larger use of the non-ergot derived DAs, such as ropinirole and pramipexole (Trifiro et al. 2008). On the contrary, cabergoline remains the mainstay of the pharmacological therapy in hyperprolactinemia patients, who require a 10-fold lower dosage of cabergoline than PD patients and have very limited alternative treatment options.
We documented a very slight reduction in the prevalence of cardiac valve regurgitation among cabergoline users who continued treatment after the 2008 SPC changes as compared to those who stopped cabergoline treatment before the SPC changes. This may indicate risk reduction, in line with the intended purpose of the SPC changes, despite our findings on the effectiveness of RMMs on the risk of valvulopathy in cabergoline users should be considered exploratory.
The only other study which evaluated the impact of the cabergoline SPC changes in clinical practice was performed in Japan by Nakaoka et al. (2011) on 57 patients. In this study, the authors analysed medical claim databases to assess whether changes in guidelines for dopamine agonists resulted in a higher number of requests for echocardiographic examinations. They found that the percentage of patients treated with cabergoline who underwent echocardiographic assessment was lower than that in our study, both before and after changes to SPC recommended by the national regulatory agency. An increase from 6.4 to 20.6 % in the number of patients receiving echocardiography examination was reported after labelling changes; however, the proportion of patients who underwent echocardiography after the labelling revisions was not significantly higher than that in controls. Overall, after product label revisions only 20 % of PD patients who were prescribed cabergoline had an echocardiography. Similar to our findings, the proportion of patients with evidence of at least two follow-up examinations was low (2/57). Interestingly, the frequency of patients prescribed dosage >2.5 mg/day was significantly higher among patients receiving an echocardiography than those without any examination.
A telephone survey of 244 neurologists from 12 European countries was performed to explore physicians’ awareness of the pergolide SPC revisions and following changes in clinical practice (Lledo et al. 2007). In that study, the overall awareness of the SPC revisions was 94.2 %. More than an half (58.3 %) of the neurologists reported that they prescribed pergolide only as second-line treatment, although 21.9 % still prescribed pergolide as first-line treatment. Most of the neurologists performed echocardiography examinations prior to treatment (67.5 %) and during treatment (76.7 %), and over half (55 %) avoided prescribing doses exceeding the recommended maximum dosage.
Since similar safety warnings about both ergot-derived dopamine agonists, cabergoline and pergolide, have been issued by regulatory agencies, we can hypothesize that the perception of risk about cabergoline treatment among European neurologists is comparable to pergolide.
Limitations
A number of limitations were present in this study. First, to assess the effectiveness of the cabergoline SPC changes in reducing cardiac valve regurgitation, it was necessary to calculate the incidence of valve regurgitation before and after the SPC changes. Since the true incidence of cardiac valve regurgitation prior to SPC changes was not available as baseline echocardiographic examinations were not yet required during that period, the prevalence of regurgitation in the pre- and post-SPC change periods was used as an alternative measure. For this reason, and given the limited numbers of patients in the study, the assessment of the effectiveness of risk minimization measures on the risk of cardiac valve regurgitation in users of cabergoline should be considered as exploratory. Only two patients started cabergoline treatment after June 26th, 2008, which suggests that cabergoline nowadays is rarely used for the treatment of PD and Parkinsonism. Because of this very low number of new users, our assessment was primarily based on the comparison between cabergoline users who started and stopped cabergoline treatment prior to June 26th, 2008 and those who started cabergoline treatment before June 26th 2008 and continued treatment after that date. The results of echocardiographic examinations were available for almost all cabergoline users. For those lacking a documented echocardiographic examination, we cannot rule out the possibility that the patient received no echocardiographic examination at all, either before or during treatment. Initially, we planned to request digital echocardiographic examinations for standardized re-reading and assessment of valvulopathy. However, digital versions were available only for very few patients; for this reason, the analysis of echocardiographic examinations was based on the results of the examinations as described by the operator. Misclassification of echocardiographic findings due to heterogeneity of the operator may have affected our results, but its effects would be expected to be randomly distributed, thus not substantially influencing the main findings. Finally, on April 13th, 2007 the Italian Drug Agency (AIFA) issued a warning for health professionals about cardiac valve regurgitation associated with cabergoline when used in PD at high dosage and for long duration of use which may have already influenced prescriber behaviour prior to the SPC changes on June 26th, 2008.
Conclusion
The present study demonstrated that the 2008 SPC changes for cabergoline use increased physicians’ awareness about the risks of cabergoline-induced cardiac valvulopathy, as demonstrated by adherence to the maximum allowable daily dose and an increase in the number of echocardiographic examinations performed after the SPC changes as compared to before. However, the RMMs included in the SPC were not consistently carried out, thus highlighting the need for additional efforts to achieve a higher level of compliance with the SPC guidelines by physicians who prescribe cabergoline for PD. Furthermore, it is noteworthy that no severe cases of cardiac valve regurgitation were documented after the June 26th, 2008 SPC changes. On the other hand, this study suggests that cabergoline is nowadays rarely prescribed to PD patients.
References
American Society of E, Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA, Nihoyannopoulos P, Otto CM, Quinones MA, Rakowski H, Stewart WJ, Waggoner A, Weissman NJ (2003) Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 16:777–802
Antonini A, Poewe W (2007) Fibrotic heart-valve reactions to dopamine-agonist treatment in Parkinson’s disease. Lancet Neurol 6:826–829
Auriemma RS, Pivonello R, Perone Y, Grasso LF, Ferreri L, Simeoli C, Iacuaniello D, Gasperi M, Colao A (2013) Safety of long-term treatment with cabergoline on cardiac valve disease in patients with prolactinomas. Eur J Endocrinol 169:359–366
EMEA (2008) Questions and answers on the review of ergot-derived dopamine agonists. London Doc.ref. EMEA/CHMP/319054/2008. June 26 Accessed 15th September 2008
Fietzek UM, Riedl L, Ceballos-Baumann AO (2012) Risk assessment and follow-up of valvular regurgitation in Parkinson patients treated with cabergoline. Parkinsonism Relat Disord 18:654–656
Lledo A, Dellva MA, Strombom IM, Wilkie JL, Jungemann ME, Royer MG, Simmons VE, Cavazzoni PA (2007) Awareness of potential valvulopathy risk with pergolide and changes in clinical practice after label change: a survey among European neurologists. Eur J Neurol 14:644–649
Movement Disorders Society Scientific Issues Committee, Litvan I, Bhatia KP, Burn DJ, Goetz CG, Lang AE, McKeith I, Quinn N, Sethi KD, Shults C, Wenning GK (2003) Movement Disorders Society Scientific Issues Committee report: SIC task force appraisal of clinical diagnostic criteria for Parkinsonian disorders. Mov Disord 18:467–486
Nakaoka S, Ishizaki T, Urushihara H, Satoh T, Ikeda S, Morikawa K, Nakayama T (2011) Echocardiography for the detection of valvulopathy associated with the use of ergot-derived dopamine agonists in patients with Parkinson’s disease. Intern Med 50:687–694
Oeda T, Masaki M, Yamamoto K, Mizuta E, Kitagawa N, Isono T, Taniguchi SK, Yaku H, Yutani C, Kawamura T, Kuno S, Sawada H (2009) High risk factors for valvular heart disease from dopamine agonists in patients with Parkinson’s disease. J Neural Transm 116:171–178
Rasmussen VG, Poulsen SH, Dupont E, Ostergaard K, Safikhany G, Egeblad H (2008) Heart valve disease associated with treatment with ergot-derived dopamine agonists: a clinical and echocardiographic study of patients with Parkinson’s disease. J Intern Med 263:90–98
Schade R, Andersohn F, Suissa S, Haverkamp W, Garbe E (2007) Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med 356:29–38
Simonis G, Fuhrmann JT, Strasser RH (2007) Meta-analysis of heart valve abnormalities in Parkinson’s disease patients treated with dopamine agonists. Mov Disord 22:1936–1942
Steiger M, Jost W, Grandas F, Van Camp G (2009) Risk of valvular heart disease associated with the use of dopamine agonists in Parkinson’s disease: a systematic review. J Neural Transm 116:179–191
Trifiro G, Savica R, Morgante L, Vanacore N, Tari M, Moretti S, Galdo M, Spina E, Caputi AP, Arcoraci V (2008) Prescribing pattern of anti-Parkinson drugs in Southern Italy: cross-sectional analysis in the years 2003–2005. Parkinsonism Relat Disord 14:420–425
Trifiro G, Mokhles MM, Dieleman JP, van Soest EM, Verhamme K, Mazzaglia G, Herings R, de Luise C, Ross D, Brusselle G, Colao A, Haverkamp W, Schade R, van Camp G, Zanettini R, Sturkenboom MC (2012) Risk of cardiac valve regurgitation with dopamine agonist use in Parkinson’s disease and hyperprolactinaemia: a multi-country, nested case-control study. Drug Saf Int J Med Toxicol Drug Exp 35:159–171
Van Camp G, Flamez A, Cosyns B, Goldstein J, Perdaens C, Schoors D (2003) Heart valvular disease in patients with Parkinson’s disease treated with high-dose pergolide. Neurology 61:859–861
Zanettini R, Antonini A, Gatto G, Gentile R, Tesei S, Pezzoli G (2007) Valvular heart disease and the use of dopamine agonists for Parkinson’s disease. N Engl J Med 356:39–46
Acknowledgments
This study was funded by Pfizer. Pfizer is the manufacturer of CABASER and DOSTINEX (cabergoline).
Conflict of interest
Cynthia de Luise and Douglas Ross are employees of Pfizer.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Italiano, D., Bianchini, E., Ilardi, M. et al. Effectiveness of risk minimization measures for cabergoline-induced cardiac valve fibrosis in clinical practice in Italy. J Neural Transm 122, 799–808 (2015). https://doi.org/10.1007/s00702-014-1314-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-014-1314-z