Abstract
A literature review was conducted to assess risk of cardiac valve regurgitation (CVR) associated with use of ergot-derived and non-ergot dopamine agonists (DAs) in patients with Parkinson’s disease (PD). Inclusion criteria: case-control/observational studies of >10 patients with PD treated with DAs, including a control group and assessment of incidence/risk of CVR. Of the 166 publications identified, 14 met all inclusion criteria and included 1,750 patients. In 11 of the studies, a significant increase in CVR frequency of any severity (at the aortic, mitral or tricuspid valve) in the ergot group vs. the non-ergot or control group was described. No study reported increased risk of CVR for non-ergot DAs, compared with controls. In the studies identified in the literature, the use of ergot-derived DAs (pergolide and cabergoline) in patients with PD was associated with increased risk of CVR. Increased risk of CVR was not associated with the use of non-ergot DAs.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Parkinson’s disease (PD) is a chronic progressive neurological disorder. For many years, levodopa (l-dopa) has been the first-line treatment for PD due to the fact that it is well tolerated and provides rapid onset of symptom relief (Cotzias et al. 1967). l-dopa treatment, however, may also be associated with motor fluctuations, dyskinesia and psychosis (Marsden and Parkes 1977; Nutt 1990; Obeso et al. 1989). Current therapeutic strategies rely on the use of l-dopa and/or dopamine agonists (DAs) to compensate for the dopaminergic deficit in patients with PD (Miyasaki et al. 2002; Pahwa et al. 2006). DAs provide symptomatic relief of PD symptoms, with a reduced incidence of motor complications, compared with l-dopa (Holloway et al. 2004; Rascol et al. 2000; Schwarz 2003), and may be given as monotherapy in early stage PD (Adler et al. 1997; Clarke and Guttman 2002; Rascol et al. 2000) or as adjunctive treatment to l-dopa in more advanced PD (Brunt et al. 2002; Lieberman et al. 1997, 1998; Mizuno et al. 2003).
Dopamine agonists may be ergot-derived, such as pergolide, cabergoline and bromocriptine. Pergolide and cabergoline have been reported to be potent 5-HT2B-receptor agonists, whereas bromocriptine potently blocks 5-HT2B receptors (Newman-Tancredi et al. 2002). The non-ergot-derived DAs ropinirole and pramipexole are non- or less-potent 5-HT2B-receptor agonists, and have demonstrated less affinity for 5-HT2B-receptors (Millan et al. 2002).
There have been several reports of cardiac valve regurgitation (CVR) in patients with migraine treated with ergot-derived methysergide and ergotamine (Bana et al. 1974; Hendrikx et al. 1996; Redfield et al. 1992; Wilke et al. 1997), and in patients treated with the appetite suppressants fenfluramine and dexfenfluramine (Connolly et al. 1997; Jollis et al. 2000). Initial reports of CVR in patients with PD were described as fibrotic complications in patients treated with bromocriptine (Serratrice et al. 2002). In addition, there have been numerous reports of CVR in patients treated with pergolide, which, although approved for the treatment of PD in Europe and the USA, has recently been voluntarily withdrawn from the market in the USA due to the risk of valvular heart disease (Baseman et al. 2004; Corvol et al. 2007; Dewey et al. 2007; Flowers et al. 2003; Horvath et al. 2004; Junghanns et al. 2007; Kenangil et al. 2007; Kim et al. 2006; Peralta et al. 2006; Pritchett et al. 2002; Schade et al. 2007; Van Camp et al. 2003, 2004; Waller et al. 2005; Yamamoto et al. 2006; Zanettini et al. 2007). More recently, there have been growing concerns over the use of cabergoline (approved for the treatment of PD in Europe and for the treatment of hyperprolactinaemia in the USA), due to cardiovascular adverse events similar to those reported for pergolide (Horvath et al. 2004; Junghanns et al. 2007; Kenangil et al. 2007; Peralta et al. 2006; Pinero et al. 2005; Schade et al. 2007; Yamamoto et al. 2006; Zanettini et al. 2007).
The aim of this paper is to summarize and compare available published literature on the frequency of CVR in patients with PD being treated with ergot-derived and non-ergot-derived DAs. As randomized controlled trials to test the risk of an adverse event such as CVR would not be ethical; all of these reports are case reports or case-control studies.
Materials and methods
Identification of all studies
A systematic search was performed on electronic publication databases including PubMed, Medline, BioMed Central, Web of Science and the Cochrane Library, (as well as the bibliographies of reviews identified during the search), and clinical trial registries using both the generic and brand names for pergolide (Permax®; Valeant Pharmaceuticals International, CA, USA), cabergoline (Dostinex®; Pfizer, NY, USA), ropinirole (REQUIP®; GlaxoSmithKline, Brentford, UK), pramipexole (Mirapex®; Boehringer Ingelheim GmbH, Ingelheim, Germany) bromocriptine (Parlodel®; Novartis Pharmaceuticals AG, Basel, Switzerland), piribedil (Trivastal®; Servier, Neuilly-sur-Seine, France), lisuride (Dopergin®; Schering AG, Berlin, Germany) and rotigotine (Neupro®; Schwarz Pharma AG, Monheim, Germany). The search term used was ‘dopamine agonists’ AND ‘fibrosis’ OR ‘valvular heart disease’ OR ‘valvulopathy’. Individual searches were also performed for each individual agonist to ensure that no citations were missed. The search included publications up to and including December 2007 and no lower date limit was applied. Papers in a foreign language were included, provided there was an English abstract and all other criteria were met.
Screening and evaluation of studies
Studies included in the literature review were case-control or observational in nature and included ten or more patients per group. A group was defined as patients receiving ergot DAs, those receiving non-ergot DAs or the control group. Each study must have had an active DA treatment group and a control group untreated with a DA or treated with a different agonist. Untreated patients may have been patients with PD or healthy, untreated controls. Studies for inclusion must have assessed the incidence, odds or risk of fibrosis, valvular heart disease or cardiac valvulopathy, as confirmed by echocardiography, and have included patients aged over 18 years, with PD of any duration.
Abstracts that did not meet inclusion criteria were eliminated and case reports of fibrosis, valvular heart disease or valvulopathy without a control group were excluded. The studies included were reviewed and agreed upon by the author group.
Data extraction
Once the studies were chosen, information regarding patient populations, treatments and outcomes were collated. For each study the number of patients per treatment group, gender and mean ages were extracted, along with the type of current treatment received by each patient and whether or not previous treatment with DAs was specified. Average daily dose, cumulative dose, duration of treatment and duration of disease were also noted. In addition, the number or proportion of patients who experienced an event of aortic, mitral or tricuspid regurgitation or any event of regurgitation, and any associated calculation of risk [e.g. odds ratio (OR)] and P-value, if calculated, were recorded. Mitral tenting area (defined as the area between the systolic coaptation point of the mitral leaflets and the mitral annulus by echocardiography) was also measured in some of the studies. The mitral tenting area in restrictive valvular heart disease is a measure of the intensity of the retraction of the mitral valve towards the apex due to the restrictive valvulopathy.
Results
Literature review
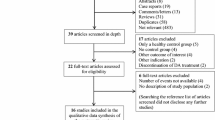
Using the term ‘dopamine agonists’ and ‘fibrosis’ or ‘valvular heart disease’ or ‘valvulopathy’, 166 publications were identified. Of these, 43 publications were written in a language other than English (with no English abstract), 36 were not relevant to the analysis, 16 had no abstract available, 13 were comments or letters, 19 were reviews, 25 were case studies of fewer than ten patients and none was a randomized controlled trial. No further publications were identified when the terms ‘pergolide’, ‘cabergoline’, ‘bromocriptine’, ‘ropinirole’ or ‘pramipexole’ were used in place of ‘dopamine agonists’, and no publications were identified with the DAs lisuride, piribedil and rotigotine. In all, 14 citations were relevant according to the inclusion criteria and were included in the descriptive review. All were case-control or observational studies (Baseman et al. 2004; Corvol et al. 2007; Dewey et al. 2007; Dhawan et al. 2005; Junghanns et al. 2007; Kenangil et al. 2007; Kim et al. 2006; Peralta et al. 2006; Ruzicka et al. 2007; Schade et al. 2007; Van Camp et al. 2004; Waller et al. 2005; Yamamoto et al. 2006; Zanettini et al. 2007). The individual studies are described below. For each study the demographic and treatment details are shown in Table 1, and the proportions of patients with CVR in individual valves and/or any valve are presented in Table 2.
Corvol et al. (2007) reported an observational study of 146 patients with PD. Of these, 86 patients treated with pergolide for at least 3 months and 47 patients in the non-pergolide group underwent two-dimensional echocardiography. The severity of CVR was assessed in the aortic, mitral and tricuspid valves.
Moderate-to-severe CVR in at least one heart valve was seen in 15 (17.4%) patients in the pergolide-treated group compared with two patients (4.3%) in the control group [OR 4.75; 95% confidence intervals (CI) 1.02, 22.1; P = 0.03). In addition, analysis of individual valves demonstrated significantly higher moderate-to-severe CVR in the tricuspid valve in the pergolide group, compared with the non-pergolide group. Moderate-to-severe CVR was found in multiple valves in four pergolide-treated patients and no patients in the non-pergolide group. Higher cumulative doses were observed in patients with multiple valve regurgitation (P < 0.05). Furthermore, the presence of a thickened or restrictive valve was associated with the cumulative dose of pergolide (P = 0.02).
Dewey et al. (2007) conducted a case-control study in 72 patients receiving DAs for PD (n = 70) or Restless Legs Syndrome (RLS; n = 2). Patients treated with pergolide (n = 36) were compared with controls who had been treated with a non-ergot DA (ropinirole or pramipexole) and who were matched by age, sex, diagnosis and lifetime dose of agonist (n = 36). All patients underwent transthoracic echocardiographic evaluation and the degree of CVR was assessed. A significant difference in mean valve scores was reported for aortic (P = 0.01), mitral (P < 0.01) and tricuspid (P < 0.001) valves, demonstrating a significantly increase in CVR in the pergolide group, compared with the non-ergot DA groups.
Kenangil et al. (2007) evaluated the effect of ergot-derived DAs on CVR in patients with PD. Frequency of CVR was assessed by transthoracic echocardiography in 46 patients who had been taking pergolide, cabergoline or a combination of the two for a minimum of 1 year (n = 46) vs. age-matched healthy controls (n = 46). A significant association was found between moderate CVR and the use of pergolide and/or cabergoline (aortic CVR, P = 0.021; mitral CVR P = 0.005; tricuspid CVR, P = 0.021). Mild CVR was also significantly more common in this group vs. the healthy controls (P = 0.013). In addition, significantly more degeneration and calcification of the mitral and aortic valves were observed in the ergot DA group, compared with the healthy controls (P < 0.05). The frequency of CVR did not differ between the group of patients taking either pergolide or cabergoline and those patients taking both agonists.
Zanettini et al. (2007) performed a transthoracic echocardiographic prevalence study in 245 patients taking DAs for PD. The relative risk of CVR of any valve, as well as in the individual aortic, mitral and tricuspid valves, was estimated in patients treated with the ergot DAs, pergolide (n = 64) and cabergoline (n = 49), and the non-ergot DAs ropinirole (n = 6) and pramipexole (n = 36), as well as in healthy controls (n = 90).
An increased frequency of moderate-to-severe CVR (grade 3 or 4 where CVR was measured on a scale of 0–4) was reported with both pergolide, (15/64 patients; 23%) and cabergoline (14/49; 29%), compared with non-ergot DAs (0/42) or controls (5/90; 6%). The proportion of patients with CVR in the pergolide group was significantly increased, vs. the control group, for mitral CVR, relative risk 6.3 (P = 0.008) and aortic CVR, relative risk 4.2 (P = 0.01), but not for tricuspid CVR, relative risk 5.6 (P = 0.16). The proportion of patients with CVR in the cabergoline group was significantly increased, vs. controls for aortic CVR, relative risk 7.3 (P < 0.001), but not for mitral CVR, relative risk 4.6 (P = 0.09) or tricuspid CVR, relative risk 5.5 (P = 0.12). The risk of CVR with non-ergot DAs was similar to that for healthy controls. In addition, a positive association was found between the increased risk of CVR and patients who had received higher cumulative doses of pergolide or cabergoline.
Leaflet thickening of any valve was found in 17/64 (27%) of patients in the pergolide group and 8/49 (16%) of patients in the cabergoline group. No cases of leaflet thickening were reported in the non-ergot or control groups. Furthermore, the mitral tenting areas in the pergolide, cabergoline and non-ergot groups (pramipexole and ropinirole) were significantly higher than in the control group. In the ergot group, the mitral tenting area changed significantly with increasing grade of mitral regurgitation (P = 0.003).
Schade et al. (2007) conducted a nested case-control study on a cohort of 31 patients diagnosed with CVR from a population of over 11,000 patients from the UK General Practice Research Database who had been prescribed anti-PD drugs between 1988 and 2005 (Schade et al. 2007). For each patient with a recorded diagnosis of CVR, records of patient examination, echocardiogram and heart catheterization were assessed. Of the 31 patients, six had received treatment with pergolide, six with cabergoline and 19 with no DA.
Compared with patients who had not received a DA, an increased risk of CVR of any severity was reported for both pergolide (incidence rate ratio 7.1) and cabergoline (incidence rate ratio 4.9). The risk of CVR in the non-DA control group was similar to that for healthy controls (incidence rate ratio 1.0).
The risk of CVR with both pergolide and cabergoline increased with cumulative doses of more than 3 mg (adjusted incidence rate ratio 37.1 and 50.3, respectively), and with a treatment duration of over 6 months (adjusted incidence rate ratio 9.8 and 7.8, respectively).
Junghanns et al. conducted a retrospective, two-dimensional, transthoracic echocardiographic study in patients with PD taking DAs (Junghanns et al. 2007). The frequency of valvular heart disease was then determined. The study assessed 123 patients who were treated with pergolide (n = 25), cabergoline (n = 24), ropinirole (n = 13), or pramipexole (n = 23) or were healthy controls (n = 38).
A significantly increased frequency of moderate valvular heart disease (grade 2, where CVR was measured on scale of 0–3) was reported with ergot DAs (11/49 patients; 22%) vs. non-ergot DAs (1/36; 3%) vs. controls (0 patients) (P = 0.001). In contrast, the risk of CVR with non-ergot DAs was reported as being similar to that for healthy controls.
No correlation was found between echocardiogram findings and cumulative dose or treatment duration. Similarly, no correlation was found between the mitral and aortic valve tenting distances, and areas and grade of CVR or vascular heart disease score. Moreover, no relevant association of tenting parameters with treatment status was observed.
Peralta et al. (2006) compared the frequency of CVR in 75 patients with PD treated with pergolide (n = 29), cabergoline (n = 13), ropinirole (n = 8) or pramipexole (n = 25) with 49 control patients without PD by transthoracic echocardiography.
A greater proportion of patients had CVR of grade 2–3 (where CVR was scored on a scale of 1–3) in the pergolide group (9/29 patients; 31%) and the cabergoline group (6/13; reported as 47%), than the non-ergot group (3/33; reported as 10%) or the age-matched controls (6/49; reported as 13%). A significantly increased risk of moderate-to-severe CVR was reported with pergolide vs. controls (P = 0.04) and cabergoline vs. controls (P = 0.013). The frequency of moderate-to-severe CVR in the non-ergot DA group vs. controls was not statistically significant (P = 0.47). The study reported that the risk of CVR was not associated with cumulative dose or treatment duration.
Leaflet thickening of the mitral and tricuspid valves was observed in one patient in the pergolide group, one patient in the cabergoline group and no patients in the non-ergot DA or control groups. Mitral tenting distances and areas were not reported.
Yamamoto et al. (2006) conducted a case-control study using transthoracic echocardiography to determine the frequency of CVR in 210 patients with PD treated with and without DAs. Patients treated with pergolide (n = 66), cabergoline (n = 16) or pramipexole (n = 16) were assessed, along with a group of patients who had previously been treated with an ergot-derived DA (treatment discontinued at least 6 months prior to the study; n = 27) and control patients with PD who had never been treated with a DA (n = 85).
A statistically significant increase in the frequency of moderate-to-severe CVR (grade 2 or 3 on a scale of 0–3) was reported in patients treated with cabergoline (11/16 patients; 69%) vs. controls (15/85; 18%; P < 0.001). The proportion of patients with moderate-to-severe CVR was 19/66 (29%) for the pergolide group, and 4/16 (25%) for the pramipexole group, although these proportions were not significant vs. the control group. The odds of experiencing dopamine-agonist-related valvular abnormalities was significantly higher in the cabergoline group (adjusted OR: 12.96; 95% CI: 3.59–46.85) than in the pergolide group (adjusted OR: 2.18; 95% CI: 0.90–5.30), the pramipexole group (adjusted OR 1.62; 95% CI 0.45–5.87) or the group previously treated with ergot DAs (adjusted OR 1.26; 95% CI 0.40–4.02). Interestingly, the proportion of patients with CVR who had previously received treatment with an ergot DA (6/27; 22%) was not statistically significantly different from the proportion of patients with CVR in the control group (15/85; 18%).
The risk of CVR was associated with cumulative dose and duration of treatment with cabergoline (P < 0.05), although no further information was available on the past-treated group. No significant difference was reported, however, among the pergolide, cabergoline or pramipexole groups, or the group previously treated with ergot DAs in terms of valvular calcification and thickness.
Waller et al. (2005) performed a retrospective study of patient records between 1998 and 2003 by electronically searching for the presence of the word ‘pergolide’ and the presence of a two-dimensional echocardiogram. The majority of the patients in this study (64%) were receiving treatment for RLS and 29% were receiving treatment for PD.
In total, 118 patients were included in the study; 55 in the pergolide group and 63 who had not taken pergolide prior to undergoing an echocardiogram (the control group).
A significantly increased frequency of CVR of the aortic valve of any degree of severity or frequency was reported with pergolide (25/55 patients; 45%) vs. control (13/63; 21%) P = 0.006; however, no significant difference in the frequency of moderate-to-severe CVR at the mitral (7/55; 13% vs. 3/63; 5%), aortic (7/55; 13% vs. 5/63; 8%) or tricuspid (6/55; 11% vs. 5/63; 8%) valves was reported with pergolide vs. control (P = 0.19, P = 0.55 and P = 0.75, respectively).
The study reported evidence of an association between higher daily doses of pergolide and moderate-to-severe CVR (P = 0.05). Moreover, it was noted that patients in this study were taking relatively low doses of pergolide; the median daily dose was 0.71 mg/day, although one patient who was receiving 16 mg/day pergolide did have severe CVR. No apparent association between the duration of treatment and the presence of moderate-to-severe CVR was reported.
Van Camp et al. (2004) evaluated 96 patients with PD using transthoracic echocardiography to determine the frequency, severity, dose-dependency and reversibility of pergolide-induced CVR. The pergolide group contained 78 patients; 26 of these were receiving at least 5 mg/day pergolide and 52 patients were receiving less than 5 mg/day pergolide. The control group comprised 18 patients who were being treated with non-ergot DAs.
A significantly increased risk of CVR was reported with pergolide vs. controls, for any severity of CVR [pergolide, 26/78 patients (33%) vs. controls, 0 patients; P = 0.0025]. The risk of moderate-to-severe CVR (of any valve), however, was not found to be significantly different [15/78 patients (19%) vs. 0 patients; P = 0.066].
A higher frequency of moderate-to-severe CVR was reported in patients who were receiving high doses of pergolide [≥5 mg/day, 11/26 (42%)] than in those receiving low doses of pergolide [<5 mg/day, 15/52 (29%)] and the effects of pergolide treatment were shown to be reversible in two patients in whom the drug was stopped.
Tenting distances and areas were measured, and a significant correlation was recorded between cumulative doses of pergolide and the tenting areas of the mitral valves (r = 0.412; P = 0.017).
Baseman et al. (2004) reviewed the clinical database of the Clinical Center for Movement Disorders at the University of Texas Southwestern Medical School to identify patients believed to be taking pergolide (Baseman et al. 2004). All patients were being treated for PD, with the exception of three who had RLS. In total, 46 patients being treated with pergolide who agreed to undergo echocardiography were included in the study. Descriptive terms for the degree of regurgitation observed were converted to numerical values. These scores for CVR for this group of patients were then compared with those from an age-matched control group derived from the Framingham study (n = 46) (Singh et al. 1999).
The Baseman study reported that 41/46 (89%) patients treated with pergolide had some degree of valvular insufficiency. The risk of abnormal CVR (aortic CVR ≥ trace severity, mitral CVR ≥ mild severity and tricuspid CVR ≥ mild severity) with pergolide vs. controls at individual valves increased two- to threefold, which was statistically significant (P ≤ 0.03). In addition, the significant risk of concerning CVR (aortic CVR ≥ mild severity, mitral CVR ≥ moderate severity and tricuspid CVR ≥ moderate severity) increased fourfold in the aortic valve (P = 0.04) and 14-fold in the tricuspid valve (P = 0.02). There was a threefold higher risk of concerning CVR in the mitral valve (P = 0.12), but this was not significant. Valve thickening was noted in 15 patients; however, the presence of one or more thickened valves was not associated with lifetime pergolide ingestion.
Kim et al. (2006) performed a two-dimensional echocardiographic study on selected patients from an outpatient clinic (n = 58) with probable PD who were taking ergot-derived DAs. Patients taking pergolide (n = 36) or bromocriptine (n = 22) were compared with age-matched healthy controls (n = 20).
The study reported a non-significant increased frequency of CVR of any severity in the pergolide and bromocriptine groups, compared with healthy controls. The mean dose of pergolide in this study was 1.1 mg, and it was noted that patients in this study were on much lower doses of pergolide than in some other studies. One patient with mild CVR, however, who was on a higher dose of pergolide (4.4 mg/day) and one patient on a low dose (2.5 mg/day) had severe multiple CVR. The daily dose of pergolide was found to correlate with the tenting area of the mitral valve (r = 0.385; P = 0.020).
Dhawan et al. (2005) retrospectively reviewed data from three UK centers for 234 patients with PD treated with cabergoline to identify symptoms suggestive of pleuro-pulmonary, cardiac or retroperitoneal fibrosis. Of the 243 patients, 15 (6%) were identified with symptoms suggestive of respiratory or cardiac fibrosis, although only three cases were found to be possibly associated with fibrotic side-effects.
Ruzicka et al. (2007) reported mild mitral regurgitation in 40 out of 90 (45%) patients with PD and in 13 out of 36 controls. In one patient only, moderate mitral regurgitation was seen. There was no correlation between the current or cumulative dose of pergolide and tenting area and tenting distance on echocardiography. The mean pergolide dose was however relatively low at 2.9 ± 0.75 mg/day.
Summary of the literature review
Eleven of the 13 studies found a significant increase in the frequency of CVR of any severity in the ergot DA group, compared with the non-ergot group or controls (Baseman et al. 2004; Corvol et al. 2007; Dewey et al. 2007; Junghanns et al. 2007; Kenangil et al. 2007; Peralta et al. 2006; Schade et al. 2007; Van Camp et al. 2004; Waller et al. 2005; Yamamoto et al. 2006; Zanettini et al. 2007). One paper reported a non-significant increase in the frequency of CVR of any severity in the ergot DA group, compared with healthy controls (Kim et al. 2006). Another paper, a retrospective evaluation of 234 patients who had taken an ergot-derived DA (cabergoline), found 15 suspected cases of CVR and only three with probable CVR, suggesting a low risk of fibrotic side-effects in patients with PD (Dhawan et al. 2005).
An increased risk of CVR with cabergoline treatment was reported in five of the 13 studies (Junghanns et al. 2007; Peralta et al. 2006; Schade et al. 2007; Yamamoto et al. 2006; Zanettini et al. 2007) and, in four of these studies, the increased risk was statistically significant (Peralta et al. 2006; Schade et al. 2007; Yamamoto et al. 2006; Zanettini et al. 2007). These studies also found a similar risk with pergolide (Junghanns et al. 2007; Peralta et al. 2006; Schade et al. 2007; Zanettini et al. 2007), with the exception of the Yamamoto study (Yamamoto et al. 2006). Although the mean daily dose of pergolide for the latter study was lower (1.4 mg/day) than in the other studies (between 2.8 and 3.2 mg/day). The Kenangil study reported an increased risk of CVR with pergolide or cabergoline, or a combination of the two agonists, although the relative risk of the two agents was not discussed (Kenangil et al. 2007). Five additional studies reported an increased risk of CVR with pergolide treatment (cabergoline was not assessed in these five studies) (Baseman et al. 2004; Corvol et al. 2007; Dewey et al. 2007; Van Camp et al. 2004; Waller et al. 2005). No study reported an increased risk of CVR with non-ergot DAs vs. controls.
In several of the studies, mitral tenting distances and areas were assessed, although results were inconsistent. A correlation between pergolide dose and the tenting area of the mitral valve was reported in two of the studies (Kim et al. 2006; Van Camp et al. 2004). In contrast, no correlation was found between the mitral valve tenting distance or area and risk of CVR in the Junghanns study (Junghanns et al. 2007). Corvol et al. (2007) reported significantly thickened or restrictive valves in pergolide-treated patients with moderate-to-severe CVR. An increase in leaflet thickening in the pergolide and cabergoline groups was observed by Zanettini et al. (2007). This study also reported a significantly greater mitral tenting area in the non-ergot DA group, compared with healthy controls, albeit similar to patients with trace or mild CVR. It is suggested that although this may be caused by a weak agonist effect on serotonin receptors, it is not sufficient to cause CVR (Zanettini et al. 2007). Similarly, leaflet thickening was noted in one patient taking pergolide and another taking cabergoline in another study (Peralta et al. 2006). No difference among pergolide, cabergoline or pramipexole was noted in valvular calcification or thickness by Yamamoto et al. (2006). Although thickened valves were noted in several patients by Baseman et al. (2004), this was not associated with lifetime pergolide ingestion.
Analysis of the risk of moderate-to-severe CVR
At the outset of this review, a meta-analysis was planned on a subset of studies that specifically reported moderate-to-severe CVR of any valve. Moreover, the inclusion criteria and methodology of the literature search were designed with a meta-analysis in mind. There were too few studies published that met the criteria for inclusion in a meta-analysis, however, and those studies available had methodologies too disparate to draw any reliable conclusions. Although most of the studies quantitatively assessed CVR as mild, moderate or severe, the grading of CVR was subjective in several cases, resulting in possible inter-study and inter-cardiologist variability (Antonini and Poewe 2007). When investigating the incidence of CVR in patients, this may be confounded by the presence of some form of degenerative valvular disease that also induces CVR. For example, echocardiography should exclude ischemic cardiomyopathy, a frequent cause of restrictive mitral valve disease, also leading to increased tenting areas and distances. Similarly, other diseases such as rheumatic valvular heart disease must also be excluded. In only one of the studies was ischemic cardiomyopathy carefully excluded (Van Camp et al. 2004). These limitations were partially considered in some of the other studies, in which tenting area and/or distances for the mitral valve were measured (Baseman et al. 2004; Corvol et al. 2007; Junghanns et al. 2007; Kenangil et al. 2007; Kim et al. 2006; Yamamoto et al. 2006; Zanettini et al. 2007).
Discussion
Incidence and outcomes with other ergot-derived drugs
A systematic review of the available data found an increased risk of CVR in patients with PD being treated with ergot-derived DAs, compared with those treated with non-ergot derived DAs or controls. Furthermore, this increased risk was reported with both cabergoline and pergolide therapy. This is in agreement with numerous reports of CVR in patients treated with pergolide (Flowers et al. 2003; Horvath et al. 2004; Pritchett et al. 2002; Van Camp et al. 2003) and with increasing concern over the use of cabergoline for the treatment of PD, due to similar reported adverse events (Horvath et al. 2004; Pinero et al. 2005).
The occurrence of CVR in patients treated with DAs is similar to events reported in patients treated for migraine with ergot-derived methysergide and ergotamine (Bana et al. 1974; Hendrikx et al. 1996; Redfield et al. 1992; Wilke et al. 1997) and in patients treated with the appetite suppressants fenfluramine and dexfenfluramine (Connolly et al. 1997; Jollis et al. 2000). Moreover, in many of the papers reviewed, similar incidences of CVR in patients taking appetite suppressants were noted (Baseman et al. 2004; Junghanns et al. 2007; Van Camp et al. 2004; Zanettini et al. 2007). Only one paper reported a lower incidence of CVR than previously reported with fenfluramine and phenteramine (Waller et al. 2005), but as already mentioned, the doses of pergolide used in this study were lower than in the other studies. These agents are ergot-derived and, similar to pergolide and cabergoline, have been found to have a higher pronounced agonist affinity to 5-HT2B receptors than the non-ergot DAs ropinirole or pramipexole (Newman-Tancredi et al. 2002).
Methodological differences among dopamine agonist studies in PD
The level of detail given for patient demographics, study design and outcome measures varied considerably among the studies. Echocardiography was used to assess the level of CVR in all studies except one (Schade et al. 2007). In this study, patient records were retrospectively reviewed; echocardiograms may have been available for some patients, but not for all. Where echocardiograms were not available, the presence of CVR was assessed by clinical records and heart catheterization (Schade et al. 2007).
In the majority of studies, patients were excluded if they had a history of CVR or other related conditions. In the Dhawan et al. (2005) and Waller et al. (2005) studies, patient records were retrospectively reviewed, but patients were not excluded based on previous history or echocardiographically-detected abnormalities unrelated to drug-induced CVR. In three of the studies, no information on exclusion criteria was available (Baseman et al. 2004, Dewey et al. 2007; Peralta et al. 2006). In all studies, echocardiograms were not available prior to treatment with a DA. Some of the studies used healthy individuals in the control group, others used patients with PD with no history of CVR, while historical controls were used in one study.
Although an echocardiogram was used to measure CVR in most of the studies, the way that CVR was scored varied between studies. The majority of studies used a semi-quantitative measure of valve disease based on recommendations by the American Society of Echocardiography (Zoghbi et al. 2003), which defines valve regurgitation as absent, 0; trace, 1; mild, 2; moderate, 3; and severe, 4. This scale was interpreted differently by different groups, however, for example in some studies, grades ranged from 0 to 3, in which case a grade of 2 or 3 indicated moderate-to-severe CVR, and lower grades were used to define absent/trace/mild regurgitation. In other studies, grades ranged from 1 to 3 or 1 to 4. Grades of moderate-to-severe CVR were considered ‘abnormal’ and thus clinically relevant. Some studies reported CVR of any severity, whereas others only reported moderate-to-severe CVR. The outcomes reported also varied among studies; in some cases the incidence of CVR was reported for each of the aortic, mitral and tricuspid valves, as well as CVR of any valve. In contrast, some studies only reported CVR at some/all individual valves or only CVR of any valve. Although in some of the early publications it appeared that the tricuspid valve was more affected than the mitral or aortic valve (Horvath et al. 2004; Pritchett et al. 2002), impairment of any valve has been reported alone or in combination in the majority of studies.
Despite these limitations, all studies reported an increased incidence of CVR in patients treated with ergot DAs. In the majority of studies, the risk of CVR significantly increased with ergot DAs, compared with non-ergot DAs or controls.
Ergot vs. non-ergot dopamine agonists
As summarized in the results, 11 of the 13 studies found a significant increase in the frequency of CVR of any severity in the ergot DA group, compared with the non-ergot group (Baseman et al. 2004; Corvol et al. 2007; Dewey et al. 2007; Junghanns et al. 2007; Kenangil et al. 2007; Peralta et al. 2006; Schade et al. 2007; Van Camp et al. 2004; Waller et al. 2005; Yamamoto et al. 2006; Zanettini et al. 2007). The doses of pergolide used across the different studies varied; one paper reported a non-significant increase in the frequency of CVR of any severity in the ergot DA group, compared with the control group (Kim et al. 2006), but also reported a lower mean dose of pergolide in the study population (1.1 mg/day) in comparison to other published studies (1.8–3.2 mg/day), which may account for the apparently lower risk reported. Another study also reported lower daily doses of pergolide (mean dose 1.4 mg/day) suggesting a possible explanation for the lower risk of CVR found in this study in the pergolide group (Yamamoto et al. 2006). The median dose of pergolide in the Waller et al. (2005) study, was also low (0.71 mg/day), although this is perhaps not surprising as 64% of the patients in this study were receiving pergolide treatment for RLS, in which case a lower dose of DA was appropriate, compared with patients with PD. This study did, however, report an increased risk of aortic CVR.
In contrast, cabergoline mean doses were similar across all the studies reviewed (3.6–4.0 mg/day) and similar increased risks of CVR were reported with the exception of one study, in which a retrospective evaluation of patients treated with cabergoline found 15 suspected cases of CVR and only three with probable CVR, suggesting a low risk of fibrotic side-effects (Dhawan et al. 2005).
An association between cumulative dose and the risk of CVR was reported in five of the studies (Corvol et al. 2007; Schade et al. 2007; Van Camp et al. 2004; Yamamoto et al. 2006; Zanettini et al. 2007). A similar association was not demonstrated in the Waller et al. (2005) study, although patients in this study were on lower median daily doses of pergolide. In addition, two of the studies reported an association between the increased risk of CVR and the duration of treatment (Schade et al. 2007; Yamamoto et al. 2006). In the five studies that reported the duration of treatment for both pergolide and cabergoline, the mean duration of treatment with pergolide was 1.5 to 2.6 times longer than that for cabergoline. Despite a shorter duration of treatment, the risk of CVR was as high in the cabergoline group as in the pergolide group. To determine if the patients in the different groups were exposed to a similar dose of DA, the following dosage equivalents have been suggested: 1.0 mg pergolide = 4.0 mg cabergoline = 1.0 mg pramipexole = 4.0 mg ropinirole (Grosset et al. 2004). Taking these equivalents into consideration, the relative dose of cabergoline received by patients in these studies may be considered higher than the pergolide dose.
Long-term outcomes for patients treated with ergot-derived dopamine agonists
There have been reports that the side-effects of ergot-derived agents may be reversible if therapy is stopped and an alternative non-ergot therapy is sought. Van Camp et al. (2004) reported reversibility of CVR in two of six patients in whom pergolide was discontinued. Similarly, reversibility of CVR with pergolide was reported by Calomne et al. (2004). A reduction in the frequency of CVR over time after the discontinuation of dexfenfluramine has also been reported (Shively et al. 1999). Furthermore, the reported frequency of CVR in a group of patients who had been treated with an ergot DA in the past was not significantly different from the control group, who had received no treatment with a DA (Yamamoto et al. 2006).
Further studies
Since this literature review was conducted, there has been a further report of CVR in patients treated with cabergoline (Yamashiro et al. 2008). The frequency of CVR was assessed in patients with PD taking low-dose DAs. Transthoracic echocardiographs were analyzed in 527 consecutive patients (448 patients treated with DAs and 79 age-matched controls who had never been treated with a DA). The frequency of CVR of the aortic valve was significantly higher in the cabergoline group (14%) compared with the control group (3%) (P < 0.05). Relative risk was significantly higher in patients treated with higher daily doses (P = 0.0007) and higher cumulative doses (P = 0.0006). No statistical difference was identified in the frequency of the tricuspid and mitral CVR. None of the other DA groups, including pergolide, gave higher frequency or higher OR compared with the controls. None of the patients showed severe regurgitation.
Implications of prescribing dopamine agonists in patients with PD
The original intention of this review was to include a meta-analysis of the studies reporting clinically significant moderate-to-severe total CVR, however, this would have been inappropriate for several reasons. Randomized controlled trials to test the risk of an adverse event would not be ethical, a prospective study to compare the risks among different DAs will not be carried out and, therefore, studies available for analysis are limited to observational or case-control studies. Guidelines for the reporting and evaluation of meta-analyses of observational studies have been assembled by an expert panel (Stroup et al. 2000), but it has also been noted that potential bias may exist in observational studies, in terms of publication, location and inclusion (Egger and Smith 1998). The diversity of study design, patient population and outcome measures also make meta-analysis of such studies challenging (Stroup et al. 2000). Although for this study, strict inclusion criteria were defined a priori and every effort was made to obtain as many published studies as possible in this area, there were too few studies published that met the inclusion criteria and those studies available had methodologies too disparate to draw any reliable conclusions from a subsequent meta-analysis. Furthermore, it has been reported that a meta-analysis based on a small number of studies should often be taken as inconclusive, regardless of the significance of the result (Davey Smith and Egger 1998).
Although a meta-analysis of the current literature seems scientifically inappropriate, the review of the published literature permits us to conclude that the symptomatic treatment of PD with ergot-derived DAs can lead to valvular heart disease. The frequency of CVR observed with ergot-derived DAs is not low, and is seen far more frequently than previously presumed, a frequency comparable to that observed with appetite-suppressant drugs. Indeed, fibrosis is a known side-effect when taking a drug with an ergotaminic structure on a regular basis and, due to safety concerns such as the development of fibrotic complications, pergolide was voluntarily withdrawn from the US market by the manufacturer in March 2007.
No significant statistical correlation was observed between the use of non-ergot-derived DAs and CVR, suggesting less risk of CVR with non-ergot-derived DAs than with ergot-derived DAs. These results should be interpreted with caution, however, as the number of patients taking non-ergot DAs included in these studies is low. Although current literature suggests that the risks of CVR with ergot-derived DAs may be dose-dependent and sometimes reversible, alternate treatment options, such as non-ergot DAs are available. Non-ergot DAs are now, together with l-dopa, the cornerstones of the symptomatic medical treatment of PD, due to their efficacy and favorable adverse event profile. In Europe, cabergoline and pergolide are now indicated as second-line therapy in patients who are intolerant or fail treatment with a non-ergot DA, accompanied by regular clinical and echocardiographic monitoring. However, further research in this field is needed; we still know little of the natural history of valvular heart disease in a large cohort of patients with PD, or whether patients with PD are pre-disposed to degenerative CVR as compared with age-matched controls. Animal studies can further enhance our knowledge in this field.
References
Adler CH, Sethi KD, Hauser RA, Davis TL, Hammerstad, JP, Bertoni et al (1997) Ropinirole for the treatment of early Parkinson’s disease. The Ropinirole Study Group. Neurology 49:393–399
Antonini A, Poewe W (2007) Fibrotic heart-valve reactions to dopamine agonist treatment in Parkinson’s disease. Lancet Neurol 6:826–829
Bana DS, MacNeal PS, LeCompte PM, Shah Y, Graham JR (1974) Cardiac murmurs and endocardial fibrosis associated with methysergide therapy. Am Heart J 88:640–655
Baseman DG, O’Suilleabhain PE, Reimold SC, Laskar SR, Baseman JG, Dewey RB Jr (2004) Pergolide use in Parkinson disease is associated with cardiac valve regurgitation. Neurology 63:301–304
Brunt ER, Brooks DJ, Korczyn AD, Montastruc JL, Stocchi F (2002) A six-month multicentre, double-blind, bromocriptine-controlled study of the safety and efficacy of ropinirole in the treatment of patients with Parkinson’s disease not optimally controlled by l-dopa. J Neural Transm 109:489–502
Calomne V, Dupuis MJ, Muller T, Kempinere F (2004) Reversible cardiac valve abnormalities with pergolide treatment. Rev Neurol (Paris) 160:81–82
Clarke CE, Guttman M (2002) Dopamine agonist monotherapy in Parkinson’s disease. Lancet 360:1767–1769
Connolly HM, Crary JL, McGoon MD, Hensrud DD, Edwards BS, Edwards WD et al (1997) Valvular heart disease associated with fenfluramine-phentermine. N Engl J Med 337:581–588
Corvol J-C, Anzouan-Kacou J-B, Fauveau E, Bonnet A-M, Lebrun-Vignes B, Girault C et al (2007) Heart valve regurgitation, pergolide use, and Parkinson disease. Arch Neurol 64:1721–1726
Cotzias GC, Van Woert MH, Schiffer LM (1967) Aromatic amino acids and modification of parkinsonism. N Engl J Med 276:374–379
Davey Smith G, Egger M (1998) Meta-analysis. Unresolved issues and future developments. BMJ 316:221–225
Dewey RBII, Reimold SC, O’Suilleabhain PE (2007) Cardiac valve regurgitation with pergolide compared with nonergot agonists in Parkinson disease. Arch Neurol 64:377–380
Dhawan V, Medcalf P, Stegie F, Jackson G, Basu S, Luce P et al (2005) Retrospective evaluation of cardio-pulmonary fibrotic side effects in symptomatic patients from a group of 234 Parkinson’s disease patients treated with cabergoline. J Neural Transm 112:661–668
Egger M, Smith GD (1998) Bias in location and selection of studies. BMJ 316:61–66
Flowers CM, Racoosin JA, Lu SL, Beitz JG (2003) The US Food and Drug Administration’s registry of patients with pergolide-associated valvular heart disease. Mayo Clin Proc 78:730–731
Grosset K, Needleman F, Macphee G, Grosset D (2004) Switching from ergot to nonergot dopamine agonists in Parkinson’s disease: a clinical series and five-drug dose conversion table. Mov Disord 19:1370–1374
Hendrikx M, Van Dorpe J, Flameng W, Daenen W (1996) Aortic and mitral valve disease induced by ergotamine therapy for migraine: a case report and review of the literature. J Heart Valve Dis 5:235–237
Holloway RG, Shoulson I, Fahn S, Kieburtz K, Lang A, Marek K et al (2004) Pramipexole vs levodopa as initial treatment for Parkinson disease: a 4-year randomized controlled trial. Arch Neurol 61:1044–1053
Horvath J, Fross RD, Kleiner-Fisman G, Lerch R, Stalder H, Liaudat S et al (2004) Severe multivalvular heart disease: a new complication of the ergot derivative dopamine agonists. Mov Disord 19:656–662
Jollis JG, Landolfo CK, Kisslo J, Constantine GD, Davis KD, Ryan T (2000) Fenfluramine and phentermine and cardiovascular findings: effect of treatment duration on prevalence of valve abnormalities. Circulation 101:2071–2077
Junghanns S, Fuhrmann JT, Simonis G, Oelwein C, Koch R, Strasser RH et al (2007) Valvular heart disease in Parkinson’s disease patients treated with dopamine agonists: a reader-blinded monocenter echocardiography study. Mov Disord 22:234–238
Kenangil G, Ozekmekci S, Koldas L, Sahin T, Erginoz E (2007) Assessment of valvulopathy in Parkinson’s disease patients on pergolide and/or cabergoline. Clin Neurol Neurosurg 109:350–353
Kim JY, Chung EJ, Park SW, Lee WY (2006) Valvular heart disease in Parkinson’s disease treated with ergot derivative dopamine agonists. Mov Disord 21:1261–1264
Lieberman A, Ranhosky A, Korts D (1997) Clinical evaluation of pramipexole in advanced Parkinson’s disease: results of a double-blind, placebo-controlled, parallel-group study. Neurology 49:162–168
Lieberman A, Olanow CW, Sethi K, Swanson P, Waters CH, Fahn S et al (1998) A multicenter trial of ropinirole as adjunct treatment for Parkinson’s disease. Ropinirole Study Group. Neurology 51:1057–1062
Marsden CD, Parkes JD (1977) Success and problems of long-term levodopa therapy in Parkinson’s disease. Lancet 1:345–349
Millan MJ, Maiofiss L, Cussac D, Audinot V, Boutin JA, Newman-Tancredi A (2002) Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. I. A multivariate analysis of the binding profiles of 14 drugs at 21 native and cloned human receptor subtypes. J Pharmacol Exp Ther 303:791–804
Miyasaki JM, Martin W, Suchowersky O, Weiner WJ, Lang AE (2002) Practice parameter: initiation of treatment for Parkinson’s disease: an evidence-based review: report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 58:11–17
Mizuno Y, Yanagisawa N, Kuno S, Yamamoto M, Hasegawa K, Origasa H et al (2003) Randomized, double-blind study of pramipexole with placebo and bromocriptine in advanced Parkinson’s disease. Mov Disord 18:1149–1156
Newman-Tancredi A, Cussac D, Quentric Y, Touzard M, Verriele L, Carpentier N et al (2002) Differential actions of antiparkinson agents at multiple classes of monoaminergic receptor. III. Agonist and antagonist properties at serotonin, 5-HT(1) and 5-HT(2), receptor subtypes. J Pharmacol Exp Ther 303:815–822
Nutt JG (1990) Levodopa-induced dyskinesia: review, observations, and speculations. Neurology 40:340–345
Obeso JA, Grandas F, Vaamonde J, Luquin MR, Artieda J, Lera G et al (1989) Motor complications associated with chronic levodopa therapy in Parkinson’s disease. Neurology 39:11–19
Pahwa R, Factor SA, Lyons KE, Ondo WG, Gronseth G, Bronte-Stewart H et al (2006) Practice parameter: treatment of Parkinson’s disease with motor fluctuations and dyskinesia (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology 66:983–995
Peralta C, Wolf E, Alber H, Seppi K, Muller S, Bosch S et al (2006) Valvular heart disease in Parkinson’s disease vs. controls: an echocardiographic study. Mov Disord 21:1109–1113
Pinero A, Marcos-Alberca P, Fortes J (2005) Cabergoline-related severe restrictive mitral regurgitation. N Engl J Med 353:1976–1977
Pritchett AM, Morrison JF, Edwards WD, Schaff HV, Connolly HM, Espinosa RE (2002) Valvular heart disease in patients taking pergolide. Mayo Clin Proc 77:1280–1286
Rascol O, Brooks DJ, Korczyn AD, De Deyn PP, Clarke CE, Lang AE (2000) A five-year study of the incidence of dyskinesia in patients with early Parkinson’s disease who were treated with ropinirole or levodopa. 056 Study Group. N Engl J Med 342:1484–1491
Redfield MM, Nicholson WJ, Edwards WD, Tajik AJ (1992) Valve disease associated with ergot alkaloid use: echocardiographic and pathologic correlations. Ann Intern Med 117:50–52
Ruzicka E, Linkova H, Penicka M, Ulmanova O, Novakova L, Roth J (2007) Low incidence of restrictive valvulopathy in patients with Parkinson’s disease on moderate dose of pergolide. J Neurol 254:1575–1578
Schade R, Andersohn F, Suissa S, Haverkamp W, Garbe E (2007) Dopamine agonists and the risk of cardiac-valve regurgitation. N Engl J Med 356:29–38
Schwarz J (2003) Rationale for dopamine agonist use as monotherapy in Parkinson’s disease. Curr Opin Neurol 16(Suppl 1):S27–S33
Serratrice J, Disdier P, Habib G, Viallet F, Weiller PJ (2002) Fibrotic valvular heart disease subsequent to bromocriptine treatment. Cardiol Rev 10:334–336
Shively BK, Roldan CA, Gill EA, Najarian T, Loar SB (1999) Prevalence and determinants of valvulopathy in patients treated with dexfenfluramine. Circulation 100:2161–2167
Singh JP, Evans JC, Levy D, Larson MG, Freed LA, Fuller DL et al (1999) Prevalence and clinical determinants of mitral, tricuspid, and aortic regurgitation (the Framingham Heart Study). Am J Cardiol 83:897–902
Stroup DF, Berlin JA, Morton SC, Olkin I, Williamson GD, Rennie D et al (2000) Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283:2008–2012
Van Camp G, Flamez A, Cosyns B, Goldstein J, Perdaens C, Schoors D (2003) Heart valvular disease in patients with Parkinson’s disease treated with high-dose pergolide. Neurology 61:859–861
Van Camp G, Flamez A, Cosyns B, Weytjens C, Muyldermans L, Van Zandijcke M et al (2004) Treatment of Parkinson’s disease with pergolide and relation to restrictive valvular heart disease. Lancet 363:1179–1183
Waller EA, Kaplan J, Heckman MG (2005) Valvular heart disease in patients taking pergolide. Mayo Clin Proc 80:1016–1020
Wilke A, Hesse H, Hufnagel G, Maisch B (1997) Mitral, aortic and tricuspid valvular heart disease associated with ergotamine therapy for migraine. Eur Heart J 18:701
Yamamoto M, Uesugi T, Nakayama T (2006) Dopamine agonists and cardiac valvulopathy in Parkinson disease: a case-control study. Neurology 67:1225–1229
Yamashiro K, Komine-Kobayashi M, Hatano T, Urabe T, Mochizuki H, Hattori N et al (2008) The frequency of cardiac valvular regurgitation in Parkinson’s disease. Mov Disord 23:935–941
Zanettini R, Antonini A, Gatto G, Gentile R, Tesei S, Pezzoli G (2007) Valvular heart disease and the use of dopamine agonists for Parkinson’s disease. N Engl J Med 356:39–46
Zoghbi WA, Enriquez-Sarano M, Foster E, Grayburn PA, Kraft CD, Levine RA et al (2003) Recommendations for evaluation of the severity of native valvular regurgitation with two-dimensional and Doppler echocardiography. J Am Soc Echocardiogr 16:777–802
Acknowledgments
This review was supported by GlaxoSmithKline Research and Development. The authors take full responsibility for the content of the paper, but thank Sarah Brown for assistance with preparing the initial draft of the manuscript and collating author comments.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Steiger, M., Jost, W., Grandas, F. et al. Risk of valvular heart disease associated with the use of dopamine agonists in Parkinson’s disease: a systematic review. J Neural Transm 116, 179–191 (2009). https://doi.org/10.1007/s00702-008-0179-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-008-0179-4