Abstract
To investigate whether a period of 1 Hz repetitive transcranial magnetic stimulation (rTMS) over M1 preconditioned by tDCS improves bradykinesia of the upper limb in Parkinson’s disease (PD). Fifteen patients with PD performed index finger, hand tapping and horizontal pointing movements as well as reach-to-grasp movements with either hand before (baseline conditions) and after a period of 1 Hz rTMS preconditioned by (1) sham, (2) anodal or (3) cathodal tDCS over the primary motor cortex contralateral to the more affected body side. Movement kinematics was analysed using an ultrasound-based motion analyser at baseline, immediately after and 30 min after each stimulation session. Dopaminergic medication was continued. Compared to baseline, 1 Hz rTMS significantly increased the frequency of index finger and hand tapping as well as horizontal pointing movements performed with the contralateral hand. Movement frequency increased up to 40% over 30 min after cessation of the stimulation. Preconditioning with cathodal tDCS, but not with anodal tDCS, reduced the effectiveness of 1 Hz rTMS to improve tapping and pointing movements. There was no significant increase of movement frequencies of the ipsilateral hand induced by 1 Hz rTMS preconditioned by either tDCS session. Movement kinematics of reach-to-grasp movements were not significantly influenced by either stimulation session. In PD the beneficial effects of 1 Hz rTMS over the primary motor cortex on bradykinesia of simple finger, hand and pointing movements is reduced by preconditioning with cathodal tDCS, but not with anodal tDCS. Preconditioning with tDCS is a powerful tool to modulate the behavioural effect of 1 Hz rTMS over the primary motor cortex in PD.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Neuro-imaging studies have demonstrated changes in neural activity within several brain areas during motor performance in Parkinson’s disease (PD). In particular, reduced activity in the supplementary motor area, primary motor cortex (M1) and the prefrontal cortex in association with increased activity in parietal and lateral premotor areas were found (Sabatini et al. 2000; Jahanshahi et al. 1995). PD also causes a remapping of cerebral connectivity, which changes the spatial segregation between different cortico-striatal loops (Helmich et al. 2009). Electrophysiological studies have added that the excitability of M1 is reduced during movement execution in PD (Lefaucheur 2005). In addition, plasticity in the motor cortex is deficient in PD, which has been shown by lacking increase of motor evoked potentials during paired associative stimulation (Morgante et al. 2006; Ueki et al. 2006). Reduction of neural activity, investigated by functional imaging studies, has been interpreted to reflect the motor disability caused by PD, namely bradykinesia (Palmer et al. 2009; Sabatini et al. 2000; Jahanshahi et al. 1995). l-Dopa medication or electrical stimulation of the subthalamic nucleus can, at least in part, reverse the changes in neural activity to be found in untreated PD (Brooks and Samuel 2000; Morgante et al. 2006; Ueki et al. 2006; Palmer et al. 2009).
Repetitive transcranial magnetic stimulation (rTMS) or transcranial direct current stimulation (tDCS) are powerful tools to modulate excitability of neural tissue within M1. Depending on the frequency of stimulation, rTMS generates either an increase (Pascual-Leone et al. 1994) or a decrease (Chen et al. 1997) of cortico-spinal excitability that outlasts the stimulation period for several minutes. Similarly, tDCS can produce a lasting shift in cortico-spinal excitability depending on the direction of current flow applied to M1 (Priori 2003). Given the fact that plasticity in the motor cortex is impaired in PD (Ueki et al. 2006; Morgante et al. 2006), brain stimulation techniques may help to re-store cortical plasticity and therefore improve bradykinesia. Indeed, high and low frequency rTMS (Siebner et al. 2000; Okabe et al. 2003; Khedr et al. 2003; Lefaucheur et al. 2004; Elahi et al. 2009) or anodal tDCS (Fregni et al. 2006) applied to M1 can improve bradykinesia of the upper limb in PD. The effect size is, however, generally moderate and the clinical effect short living and also quite variable after a single application of either rTMS or tDCS over M1 (Elahi et al. 2009). It has been suggested that rTMS procedures are more effective in PD when the brain is in a dopaminergic state, i.e. on dopaminergic drugs (Mir et al. 2005; Strafella et al. 2003).
In healthy humans preconditioning of cortico-spinal excitability with tDCS over M1 can modulate the direction of plasticity induced by subsequent administration of 1 Hz rTMS (Siebner et al. 2004). That is, a session of 15 min 1 Hz rTMS applied over the left M1 immediately after 10 min of preconditioning with tDCS causes an increase in cortico-spinal excitability when cathodal tDCS had been applied and a decrease in cortico-spinal excitability when anodal tDCS had been applied. The preconditioning effects of tDCS suggest the existence of intrinsic homeostatic plasticity in M1, which stabilises cortico-spinal excitability within a physiologically useful range. Preconditioning of M1 with tDCS systematically shifts cortico-spinal excitability from baseline (Siebner et al. 2004) and therefore may change the disease-inherent reduction of cortico-spinal excitability in PD.
A recent meta-analysis has shown that 1 Hz rTMS alone is of only limited value to (1) modulate reduced cortico-spinal excitability in PD or (2) improve bradykinesia in PD as assessed with the Unified Parkinson’s Rating Scale (Elahi et al. 2009). The idea is that a period of tDCS may enhance the effectiveness of 1 Hz rTMS over M1 to modulate cortico-spinal excitability and therefore improve bradykinesia in PD. In healthy subjects 1 Hz rTMS decreases cortico-spinal excitability, while in PD it has been shown to enhance cortico-spinal excitability (Mally and Stone 1999; Okabe et al. 2003). This “paradoxical” effect is thought to be due to the baseline reduction in cortico-spinal excitability of M1 in PD, which reduces the threshold for inducing long-term potentiation (Okabe et al. 2003). Preconditioning 1 Hz rTMS over M1 by facilitatory anodal tDCS may re-store cortico-spinal excitability in PD and therefore enhance the inhibitory effect of 1 Hz rTMS.
Patients with PD performed simple index finger, hand tapping and horizontal pointing movements as well as reach-to-grasp movements with either hand before (baseline conditions) and after 15 min of 1 Hz rTMS preconditioned by 10 min of (1) sham, (2) anodal or (3) cathodal tDCS over the M1 contralateral to the more affected body side with dopaminergic drugs. Given the fact that neural activity and cortical excitability of M1 is pathologically reduced during movement execution in PD (Helmich et al. 2009; Sabatini et al. 2000; Jahanshahi et al. 1995; Brooks and Samuel 2000), we hypothesized that facilitatory preconditioning with anodal tDCS, but not inhibitory preconditioning with cathodal tDCS, may enhance the potential benefits of 1 Hz rTMS on bradykinesia of the contralateral arm and hand for several minutes after the stimulation period.
Material and methods
Patients
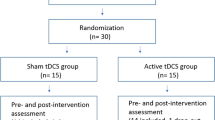
Fourteen right-handed patients and one left-handed (Crovitz and Zener 1965) patient with PD (six females, mean age 69 ± 8 years; disease duration 5 ± 3 years) participated. Clinical details regarding the patient cohort are given in Table 1. Informed consent was obtained prior to testing and all procedures had been approved by the local Ethics Committee. Patients were tested on dopaminergic drugs on three separate occasions one week apart. Patients were examined at the time of best motor response following administration of dopaminergic drugs. The Hoehn and Yahr score (1967) and the motor subscore (part III) of the Unified PD rating scale (UPDRS) were rated (Fahn and Elton 1987). Peak-dose dyskinesias were rated from involuntary movements of the face, neck, trunk, upper and lower limbs according to part IV of the UPDRS (Fahn and Elton 1987). None of the patients suffered dyskinesias in any of the experimental sessions. The levodopa equivalent daily dose (LEDD) was calculated (Krack et al. 1998). All patients were tested with the Mini Mental Status examination to exclude cognitive decline (indicated by a score ≤ 24 points; Folstein et al. 1975).
Experimental procedures
Kinematics of simple index finger tapping at the metacarpophalangeal joint, hand tapping at the wrist and horizontal pointing movements as well as more complex reach-to-grasp movements were studied at both the contralateral and ipsilateral hand (1) prior to (baseline conditions) and following 1 Hz rTMS preconditioned by (2) sham tDCS, (3) anodal tDCS and (4) cathodal tDCS over M1 contralateral to the more affected body side. The three experimental sessions were separated by one week to avoid any carry over effects after brain stimulation. The order of sessions (preconditioning with sham, anodal or cathodal tDCS) was randomly assigned to each subject and counterbalanced across subjects. Subjects were completely naïve to the experimental hypothesis and received standardized instructions. Tapping movements should be performed as fast as possible. Pointing and reach-to-grasp movements should be performed as fast and as accurate as possible.
Kinematic motion analysis
Subjects performed index finger tapping, hand tapping, horizontal pointing movements, and a reach-to-grasp task with either hand (Fig. 1). The movement kinematics were recorded using an ultrasonic motion analyzer (CMS 20S, Zebris, Isny, Germany) as described previously in detail (Nowak 2008). The total duration of motor assessment was 5 min.
Recording of the a index finger tapping, b hand tapping, c horizontal pointing movements and d reach-to-grasp movements. Movement kinematics during each task was recorded using a three-dimensional motion analysis system based on ultrasound-emitting position markers. For the index finger tapping, hand tapping and horizontal pointing movement tasks, the position markers were fixed to the distal segments of the index finger and to the styloid process of the radius. In the horizontal pointing task additional markers were placed on the marks to be pointed at. For the reach-to-grasp task, position markers were fixed to the distal segments of the index finger and thumb and to the styloid process of the radius
Index finger tapping and hand tapping were performed as fast as possible. Movement amplitude was 2 cm in the index finger task and 4 cm in the hand tapping task as indicated by a mark (Fig. 1a, b). Three 5 s trials were performed with each hand. To quantify movement performance, the following parameters were obtained: (1) movement frequency (in Hz) and (2) peak movement amplitude (in mm). Both parameters were averaged across all three trials for each patient. For the horizontal pointing task, subjects pointed with the index finger between two marks separated in a horizontal plane in parallel to the trunk by a distance of 30 cm (Fig. 1c). Horizontal pointing should be performed fast and accurate. Three 20 s trials were performed with each hand. Motor performance was quantified by (1) the movement frequency (in Hz) and (2) the peak movement amplitude (in mm). Parameters were averaged across all trials performed by each patient. During the reach-to-grasp task, subjects placed the hand with thumb and index finger touching each other on a starting mark (Fig. 1d). Subjects reached for a cylindrical object (diameter: 9 cm; depth: 4 cm; mass: 350 g), grasped it between the tips of the index finger and thumb, lifted it 10 cm above the table (as indicated by another mark), and held it for 3 s before placing it back on the table. Ten such reach-to-grasp movements were performed by each subject with either hand. Reach-to-grasp movements should be performed fast and accurate. For each reach-to-grasp movement the following parameters were obtained: (1) peak velocity of wrist transport (in mm/s), (2) peak grasp aperture (in mm), (3) peak velocity of grasp aperture (in mm/s) and (4) time of peak grasp aperture in percent of movement time (in %). All parameters were averaged across all trials performed by each participant.
tDCS-preconditioning of 1 Hz rTMS
Continuous tDCS of M1 was applied using a battery-driven DC stimulator (NeuroConn, Ilmenau, Germany). For effective tDCS of M1, a constant current flow of 1 mA was applied for 10 min through wet sponge electrodes (size: 7 × 5 cm) positioned over the M1 contralateral to the more affected body side and the contralateral frontal pole (Fig. 2). The M1 electrode was placed at the optimal site for cortical magnetic stimulation (see below). The fronto-polar electrode was always placed over the eyebrow contralateral to the stimulated M1. The polarity of tDCS refers to the electrode placed over M1. For anodal (facilitatory) tDCS, the anode was placed over the M1, whereas for cathodal (inhibitory) tDCS the cathode was positioned over M1. During sham tDCS the DC stimulator faded off after 5 s of stimulation at the beginning of the sham session and then was turned off.
Transcranial magnetic stimulation was performed using a 70-mm figure-of-eight coil and a Magstim Super Rapid stimulator (Magstim Company, Dyfed, UK). The coil was placed tangentially over the hand area of M1 of the hemisphere contralateral to the more affected body side at the optimal site for the response of the first dorsal interosseus muscle. The handle of the coil was pointed backward and laterally at a 45° angle from the midline. The optimal site was defined as the location where stimulation at slightly supra-threshold intensity elicited the largest motor evoked potential in the contralateral first dorsal interosseus muscle. Electromyographic activity was recorded using silver–silver-chloride electrodes positioned in a belly-tendon technique on the skin overlying the first dorsal interosseus muscle of the contralateral hand. The electromyographic signal was amplified, filtered (50–2,000 z) and digitized at a sampling rate of 5,000 Hz. The resting motor threshold was defined for each patient as the lowest stimulator output that elicited motor evoked potentials with peak-to-peak amplitude of at least 50 μV in the contralateral first dorsal interosseus muscle in at least five of ten trials. The average resting motor thresholds are summarized for each patient in Table 1. RTMS was applied immediately after tDCS. RTMS was applied over M1 at a rate of 1 Hz, 90% resting motor threshold for 15 min using a 70-mm figure-of-eight coil. Immediately after application of the rTMS protocol the behavioural measurements started.
Statistical analysis
After verification of normal distribution and homogeneity of variance, repeated measures ANOVAs were calculated for each kinematic parameter with the factors “session” [levels: (1) 1 Hz rTMS preconditioned by sham tDCS, (2) 1 Hz rTMS preconditioned by anodal tDCS and (3) 1 Hz rTMS preconditioned by cathodal tDCS], “time” [levels: (1) baseline, (2) 0 min after rTMS application and (3) 30 min after rTMS application] and “hand” [levels: (1) contralateral hand and (2) ipsilateral hand]. Only significant effects are reported. Post hoc pair-wise comparisons between conditions were performed using t-tests. A P value of 0.05 was considered significant after Bonferroni correction for multiple comparisons.
Results
All subjects performed the motor tasks according to the instructions and tolerated 1 Hz rTMS preconditioned by tDCS well without side-effects.
Index finger tapping, hand tapping and horizontal pointing movements
Importantly, the peak amplitudes of index finger tapping, hand tapping and horizontal pointing were not significantly influenced by the factors “session”, “hand”, “time” or their interactions. Thus, differences in movement frequency induced by 1 Hz rTMS preconditioned by any of the tDCS sessions are unlikely to be simply the result of a change in movement amplitude. Figure 3a provides average percentage changes from baseline of the frequencies of index finger tapping, hand tapping and horizontal pointing performed with either hand after 1 Hz rTMS applied to the M1 contralateral to the more affected body side preconditioned by (1) sham, (2) anodal and (3) cathodal tDCS. The frequencies of index finger tapping, hand tapping and horizontal pointing increase relative to baseline immediately after and 30 min after 1 Hz rTMS preconditioned by sham and anodal tDCS, but not by cathodal tDCS. This effect is most pronounced at the hand contralateral to the stimulated M1. Index finger and hand tapping performance as well as horizontal pointing at individual maximum speed are highly over-learned motor behaviours both in healthy subjects and in PD (Hermsdörfer et al. 1999; De Frias et al. 2007). That is no relevant intra-individual variability of movement frequency is found for repeated performance over time (Hermsdörfer et al. 1999; De Frias et al. 2007). Thus, the change in tapping frequency observed at both the hand ipsi- and contralateral to the stimulated M1 should represent a “real effect” induced by the stimulation procedure rather than a training effect.
a Percentage changes (± one standard error of the mean) of the frequency of index finger tapping, hand tapping and horizontal pointing movements performed with either hand after 1 Hz rTMS preconditioned by sham, anodal or cathodal tDCS in relation to the baseline condition of each session. b Percentage changes (± one standard error of the mean) of peak velocity of wrist transport, peak velocity of grasp aperture and time of peak grasp aperture after 1 Hz rTMS preconditioned by sham, anodal or cathodal tDCS in relation to the baseline condition of each session
Frequencies of index finger tapping (F 2,28 = 5.3; P < 0.01), hand tapping (F 2,28 = 5.6; P < 0.01) and horizontal pointing movements (F 2,28 = 6.5; P < 0.01) were significantly influenced by the factor “time”, suggesting that movement frequencies increased over 30 min after the stimulation session has ceased. A significant effect of the factor “hand” on index finger tapping (F 1,14 = 5.6; P < 0.05), hand tapping (F 1,14 = 4.5; P = 0.05) and horizontal pointing movement frequencies (F 1,14 = 5.6; P < 0.01) indicates that the improvement in performance induced by the stimulation session was most pronounced at the hand contralateral to the stimulated M1. A significant effect of the interaction “session” × ”time” on the frequencies of index finger tapping (F 4,56 = 2.7; P < 0.05), hand tapping (F 4,56 = 2.8; P < 0.05) and horizontal pointing movements (F 4,56 = 2.9; P < 0.05), implies that the increase in movement frequency over 30 min after the stimulation session was evident only when 1 Hz rTMS was preceded by sham tDCS or anodal tDCS, but not by cathodal tDCS. Indeed, a significant effect of “time” on index finger tapping (1 Hz rTMS preconditioned by sham tDCS: P < 0.01; 1 Hz rTMS preconditioned by anodal tDCS: P < 0.01), hand tapping (1 Hz rTMS preconditioned by sham tDCS: P < 0.05; 1 Hz rTMS preconditioned by anodal tDCS: P < 0.05) and horizontal pointing movement frequencies (1 Hz rTMS preconditioned by sham tDCS: P < 0.001; 1 Hz rTMS preconditioned by anodal tDCS: P < 0.01) was only evident after 1 Hz rTMS preconditioned by sham and anodal tDCS, but not by cathodal tDCS. None of the other factors or interactions between factors reached significant effects on index finger tapping, hand tapping or horizontal pointing movement frequencies.
Reach-to-grasp movements
Peak velocity of wrist transport refers to the performance of more proximal muscles of the arm and shoulder. Peak grasp aperture and the velocity of peak grasp aperture are measures of performance of more distal muscles of the arm. The time of peak grasp aperture measures the temporal coupling between the reach and grasp components of the reach-to-grasp task. Figure 3b summarizes the average percentage change of peak velocity of wrist transport, peak velocity of grasp aperture and time of peak grasp aperture from baseline. Data obtained from reach-to-grasp movements performed with either hand after 1 Hz rTMS preconditioned by (1) sham, (2) anodal and (3) cathodal tDCS are shown. None of these measures was systematically influenced by any of the stimulation sessions.
Peak velocity of wrist transport (F 1,14 = 7.2; P < 0.05) and peak velocity of grasp aperture (F 1,14 = 4.2; P < 0.05) were significantly influenced by the factor “hand”, suggesting that patients produced smaller velocities of wrist transport and smaller velocities of grasp aperture with the contralateral (more affected) hand indicative of pronounced bradykinesia. Also the time of peak grasp aperture was significantly influenced by the factor “hand” (F 1,14 = 10; P < 0.01), indicating that the peak of grasp aperture occurred later, that is closer to the end of the reach movement, when performing with the contralateral (more affected) hand. Thus, the timing between the reach and grasp component of the reach-to-grasp task differed in between the less affected (ipsilateral) and more affected (contralateral) hand. The time of peak grasp aperture was significantly influenced by the factor “time” (F 2,28 = 7.3; P < 0.01), implying that it occurred closer to the end of the movement in dependence of time from the stimulation session. None of the other factors or interactions between factors reached significant effects on any of the kinematic parameters analysed for the reach-to-grasp task.
Discussion
Our data add the following important information to the current knowledge about the effectiveness of brain stimulation techniques on bradykinesia in PD: (1) 1 Hz rTMS over M1 preconditioned by sham or anodal tDCS improves movement kinematics primarily at the hand contralateral to the stimulated M1 for at least 30 min; (2) movement kinematics at the hand contralateral to the stimulated M1 was equally improved by either 1 Hz rTMS alone (preconditioned by sham tDCS) or 1 Hz rTMS preconditioned by anodal tDCS, (3) 1 Hz rTMS improves simple finger, hand and pointing movements, but not reach-to-grasp movements; (4) the beneficial effects of 1 Hz rTMS are reduced by preconditioning with cathodal tDCS.
The effects of rTMS, in particular low frequency rTMS, on bradykinesia in PD have been found to be quite variable (Okabe et al. 2003; Lefaucheur et al. 2004; Mally and Stone 1999; Tergau et al. 1999). Quantitative improvement of motor performance, as assessed by the motor subscore of the Unified Parkinson’s Disease Rating scale (UPDRS; Fahn and Elton 1987), varied between 0 and 20% after a single session of low frequency (0.5 and 1 Hz) rTMS applied over M1 (Lefaucheur et al. 2004; Tergau et al. 1999). Repeated sessions of low frequency (0.2 and 1 Hz) rTMS delivered over 10 days (once or twice a day; Mally and Stone 1999) or 8 weeks (once a week; Okabe et al. 2003) improved motor performance, as assessed by the motor subscore of the UPDRS, by 15–48%. Differences in the stimulation procedures, patient selection and outcome measures may explain some of the inconsistencies between studies and the overall limited value of 1 Hz rTMS over M1 to enhance motor performance in PD (Elahi et al. 2009).
Our methodological approach included the kinematic investigation of both simple tapping and pointing movements, involving both distal (index finger and hand) and proximal (shoulder and upper arm) segments of the upper limb, and more complex reach-to-grasp movements, representing a motor behaviour most relevant for daily life. We found that 1 Hz rTMS preconditioned by sham (no) tDCS improved index finger tapping frequency by up to 9% at the contralateral hand (5% at the ipsilateral hand), hand tapping frequency by up to 28% at the contralateral hand (6% at the ipsilateral hand) and the frequency of pointing movements by up to 38% at the contralateral hand (10% at the ipsilateral hand) within 30 min after stimulation has ceased. 1 Hz rTMS preconditioned by anodal tDCS caused an improvement of index finger tapping frequency by up to 10% at the contralateral hand (6% at the ipsilateral hand), hand tapping frequency by up to 13% at the contralateral hand (5% at the ipsilateral hand) and the frequency of pointing movements by up to 24% at the contralateral hand (6% at the ipsilateral hand) 30 min after stimulation.
An interesting observation was that 1 Hz rTMS over M1 produced similar effects on movement kinematics of the contralateral hand when preceded by sham (no) or anodal tDCS. The question is why anodal tDCS did not enhance the effect of 1 Hz rTMS over M1 in PD. It has been demonstrated that cortical plasticity in the motor system is lacking in PD subjects off dopaminergic medication, but is evident in PD subjects on dopaminergic drugs (Ueki et al. 2006; Morgante et al. 2006). In addition, there is evidence that rTMS procedures are more effective in PD when the brain is in a dopaminergic state (Mir et al. 2005; Strafella et al. 2003). We therefore tested PD subjects on dopaminergic drugs and assumed that cortical plasticity per se should be intact in our study sample. To reduce intra-individual variability in between stimulation sessions PD subjects were examined at the time of best motor response following administration of dopaminergic drugs. Indeed, the fact that cathodal tDCS reduces the beneficial effects of 1 Hz rTMS over M1 on motor performance of the contralateral hand implies that cortical excitability in principle could be modulated in our PD subjects. Consequently, other reasons for the lacking effectiveness of anodal tDCS preconditioning must be considered.
Parkinson’s disease is associated with changes of both inhibitory and facilitatory motor cortical mechanisms, suggesting deficient motor cortex activation and deactivation (Lefaucheur 2005; Buhmann et al. 2004; Soysal et al. 2008). Low frequency rTMS over M1 or premotor cortex has been found to enhance intracortical inhibition of M1 in PD (Lefaucheur et al. 2004; Buhmann et al. 2004), however, the effectiveness of low frequency rTMS regarding clinical improvement of motor disability has been found to vary considerably (Okabe et al. 2003; Lefaucheur et al. 2004; Mally and Stone 1999; Tergau et al. 1999). The plastic changes induced by 1 Hz rTMS critically depend on the functional state of cortical excitability of the stimulated M1 before and at the time of stimulation (Siebner et al. 2004). The sensitivity of the motor cortex to brain stimulation techniques in an individual with PD depends on both intrinsic factors, such as disease progression (Buhmann et al. 2004) and genetic status (Bäumer et al. 2007), and extrinsic factors, such as levodopa depletion (Lefaucheur 2005; Mir et al. 2005; Strafella et al. 2003). Consequently, inter-individual variability of motor cortex sensitivity to brain stimulation may have contributed to the differential behavioural effects found after low frequency rTMS administered to M1 alone or after preconditioning with anodal tDCS in our PD subjects. Future studies should address this issue by the application of electrophysiological measures to test the effects of brain stimulation on cortico-spinal excitability in PD.
Most importantly, however, neither stimulation session produced any behavioural changes of reach-to-grasp movements, which are more relevant for daily life motor activities in PD. This finding fits well with previous data suggesting a lacking effect of inhibitory brain stimulation on global motor function in PD subjects (Elahi et al. 2009). One possible explanation for the dissociation of behavioural responses induced by brain stimulation for single joint movements and reach-to-grasp movements may be differential changes in motor cortex excitability induced by single and multi-joint movements. It has been shown that the excitability maps of motor output within the primary motor cortex change in dependence of the number of joints and muscles involved during pointing and grasping movements (Devanne et al. 2002; Ginanneschi et al. 2006). Within the context of the Bienenstock–Cooper–Munro (BCM) theory stabilization of cortical excitability is ensured by a dynamic adaptation of the threshold of postsynaptic activity (Bienenstock et al. 1982). The differential activation of multiple motor maps within M1 during multi-joint movements may cause reduction of postsynaptic activity for inactive muscle representation areas and enhancement of postsynaptic activity for active muscle representation areas. The changes in cortical excitability induced by either 1 Hz rTMS alone or 1 Hz rTMS preconditioned by tDCS may be blurred and less directed towards inhibition or facilitation when multiple motor output maps work in concert, compared to the well circumscribed motor cortex activation induced by single joint movements. In other words enhancement of cortical excitability in multiple motor maps induced by multi-joint movements (such as reach-to-grasp movements) may taint (1) the directed shift of cortical excitability and therefore (2) the behavioural change induced by 1 Hz rTMS alone or after preconditioning with tDCS. Given the fact that changes in cortical excitability were not measured in the current study additional data are necessary to support this interpretation.
In the context of the BCM doctrine reduction in postsynaptic activity favours the induction of long-term potentiation and enhancement of postsynaptic activity favours the induction of long-term depression (Bienenstock et al. 1982). In PD cortico-spinal excitability of the motor cortex is usually reduced (Lefaucheur 2005; Lefaucheur et al. 2004). Within the BCM theory we hypothesized that a period of facilitatory anodal tDCS may “normalize” cortico-spinal excitability and therefore enhance the inhibitory effects of 1 Hz rTMS over M1 in PD. This should improve bradykinesia of the contralateral upper limb (Mally and Stone 1999; Okabe et al. 2003). Indeed, we observed that 1 Hz rTMS alone or preconditioned by anodal tDCS significantly improved simple index finger and hand tapping movements as well as horizontal pointing performed with the arm and hand contralateral to the stimulated M1. However, our data suggest that the amount of improvement of upper limb bradykinesia to be achieved by 1 Hz rTMS preconditioned by anodal tDCS does not differ from that achieved by administration of 1 Hz rTMS alone (in conjunction with sham tDCS). Preconditioning with cathodal tDCS, on the other hand, significantly reduced the effectiveness of 1 Hz rTMS to improve motor performance of single joint movements of the index finger, hand and arm. We have not probed the changes in cortical excitability using electrophysiological measures. To understand the mechanisms underlying the differential behavioural effects of 1 Hz rTMS alone and preconditioned by tDCS it appears essential to do so in future studies. Although preconditioning rTMS by tDCS in PD patients appears to be a safe procedure, the practical impact of our work is that tDCS preconditioning with tDCS does not significantly enhance the beneficial effects of 1 Hz rTMS over M1 in an attempt to improve upper limb bradykinesia in PD.
References
Bäumer T, Pramstaller PP, Siebner HR, Schippling S, Hagenah J, Peller M, Gerloff C, Klein C, Münchau A (2007) Sensorimotor integration is abnormal in asymptomatic Parkin mutation carriers: a TMS study. Neurology 69:1976–1981
Bienenstock EL, Cooper LN, Munro PW (1982) Theory for the development of neuron selectivity: orientation specificity and binocular interaction in visual cortex. J Neurosci 2:32–48
Brooks DJ, Samuel M (2000) The effects of surgical treatment of Parkinson’s disease on brain function: PET findings. Neurology 55:S52–S59
Buhmann C, Gorsler A, Baumer T, Hidding U, Demiralay C, Hinkelmann K, Weiler C, Siebner HR, Münchau A (2004) Abnormal excitability of premotor-motor connections in de novo Parkinson’s disease. Brain 127:2246–2732
Chen R, Classen J, Gerloff C, Celnik P, Wassermann EM, Hallett M, Cohen LG (1997) Depression of motor cortex excitability by low-frequency transcranial magnetic stimulation. Neurology 48:1398–1403
Crovitz HF, Zener K (1965) A group for assessing hand and eye dominance. Am J Psychol 75:271–276
De Frias CM, Dixon RA, Fisher N, Camicioli R (2007) Intraindividual variability in neurocognitive speed: a comparison of Parkinson’s disease and normal older adults. Neuropsychologia 45:2499–2507
Devanne H, Cohen LG, Kouchtir-Devanne N, Capaday C (2002) Integrated motor cortical control of task-related muscles during pointing in humans. J Neurophysiol 87:3006–3017
Elahi B, Elahi B, Chen R (2009) Effect of transcranial magnetic stimulation on Parkinson motor function-systematic review of controlled clinical trials. Mov Disord 24:357–363
Fahn S, Elton RL, Members of the UPDRS Development Committee (1987) The Unified Parkinson’s disease Rating Scale. In: Fahn S, Marsden CD, Calne DB, Goldstein M (eds) Recent developments in Parkinson’s disease, vol. 2. McMillan Healthcare Information, Florham Park, pp 153–163, 293–304
Folstein MF, Folstein SE, McHugh PR (1975) Mini-Mental State (a practical method for grading the state of patients for the clinician). J Psychiatr Res 12:189–198
Fregni F, Boggio PS, Santos MC, Lima M, Vieira AL, Rigonatti SP, Silva MT, Barbosa ER, Nitsche MA, Pascual-Leone A (2006) Noninvasive cortical stimulation with transcranial direct current stimulation in Parkinson’s disease. Mov Disord 21:1693–1702
Ginanneschi F, Dominici F, Biasella A, Gelli F, Rossi A (2006) Changes in corticomotor excitability of forearm muscles in relation to static shoulder positions. Brain Res 1073:332–338
Helmich RC, Derikx LC, Bakker M, Scheeringa R, Bloem BR, Toni I (2009) Spatial remapping of cortico-striatal connectivity in Parkinson’s disease. Cereb Cortex [Epub ahead of print]
Hermsdörfer J, Marquardt C, Wack S, Mai N (1999) Comparative analysis of diadochokinetic movements. J Electromyogr Kinesiol 9:283–295
Hoehn M, Yahr M (1967) Parkinsonism: onset, progression and mortality. Neurology 17:427–442
Jahanshahi M, Jenkins IH, Brown RG, Marsden CD, Passingham RE, Brooks DJ (1995) Self-initiated versus externally triggered movements. I. An investigation using measurement of regional cerebral blood flow with PET and movement-related potentials in normal and Parkinson’s disease subjects. Brain 118:913–933
Khedr EM, Farweez HM, Islam H (2003) Therapeutic effect of repetitive transcranial magnetic stimulation on motor function in Parkinson’s disease patients. Eur J Neurol 10:567–572
Krack P, Pollak P, Limousin P, Hoffmann D, Xie J, Benazzouz A (1998) Subthalamic nucleus or internal pallidal stimulation in young onset Parkinson’s disease. Brain 121:141–147
Lefaucheur JP (2005) Motor cortex dysfunction revealed by cortical excitability studies in Parkinson’s disease: influence of antiparkinsonian treatment and cortical stimulation. Clin Neurophysiol 116:244–253
Lefaucheur JP, Drouot X, Von Raison F, Ménard-Lefaucheur I, Cesaro P, Nguyen JP (2004) Improvement of motor performance and modulation of cortical excitability by repetitive transcranial magnetic stimulation of the motor cortex in Parkinson’s disease. Clin Neurophysiol 115:2530–2541
Mally J, Stone TW (1999) Improvement in Parkinsonian symptoms after repetitive transcranial magnetic stimulation. J Neurol Sci 162:179–184
Mir P, Matsunaga K, Gilio F, Quinn NP, Siebner HR, Rothwell JC (2005) Dopaminergic drugs restore facilitatory premotor–motor interactions in Parkinson disease. Neurology 64:1906–1912
Morgante F, Espay AJ, Gunraj C, Lang AE, Chen R (2006) Motor cortex plasticity in Parkinson’s disease and levodopa-induced dyskinesias. Brain 129:1059–1069
Nowak DA (2008) The impact of stroke on the performance of grasping: usefulness of kinetic and kinematic motion analysis. Neurosci Biobehav Rev 32:1439–1450
Okabe S, Ugawa Y, Kanazawa I (2003) Effectiveness of rTMS on Parkinson’s Disease Study Group. 0.2-Hz repetitive transcranial magnetic stimulation has no add-on effects as compared to a realistic sham stimulation in Parkinson’s disease. Mov Disord 18:382–388
Palmer SJ, Ng B, Abugharbieh R, Eigenraam L, McKeown MJ (2009) Motor reserve and novel area recruitment: amplitude and spatial characteristics of compensation in Parkinson’s disease. Eur J Neurosci 29:2187–2196
Pascual-Leone A, Valls-Sole J, Wassermann EM, Hallett M (1994) Responses to rapid-rate transcranial magnetic stimulation of the human motor cortex. Brain 117:847–858
Priori A (2003) Brain polarization in humans: a reappraisal of an old tool for prolonged non-invasive modulation of brain excitability. Clin Neurophysiol 114:589–595
Sabatini U, Boulanouar K, Fabre N, Martin F, Carel C, Colonnese C, Bozzao L, Berry I, Montastruc JL, Chollet F, Rascol O (2000) Cortical motor reorganization in a kinetic patients with Parkinson’s disease: a functional MRI study. Brain 123:394–403
Siebner HR, Rossmeier C, Mentschel C, Peinemann A, Conrad B (2000) Short-term motor improvement after sub-threshold 5-Hz repetitive transcranial magnetic stimulation of the primary motor hand area in Parkinson’s disease. J Neurol Sci 178:91–94
Siebner HR, Lang N, Rizzo V, Nitsche MA, Paulus W, Lemon RN, Rothwell JC (2004) Preconditioning of low-frequency repetitive transcranial magnetic stimulation with transcranial direct current stimulation: evidence for homeostatic plasticity in the human motor cortex. J Neurosci 24:3379–3385
Soysal A, Sobe I, Atay T, Sen A, Arpaci B (2008) Effect of therapy on motor cortical excitability in Parkinson’s disease. Can J Neurol Sci 35:166–172
Strafella AP, Paus T, Fraraccio M, Dagher A (2003) Striatal dopamine release induced by repetitive transcranial magnetic stimulation of the human motor cortex. Brain 126:2609–2615
Strafella AP, Ko JH, Monchi O (2006) Therapeutic application of transcranial magnetic stimulation in Parkinson’s disease: the contribution of expectation. Neuroimage 31:1666–1672
Tergau F, Wassermann EM, Paulus W, Ziemann U (1999) Lack of clinical improvement in patients with Parkinson’s disease after low and high frequency repetitive transcranial magnetic stimulation. Electroencephalogr Clin Neurophysiol (Suppl) 51:281–288
Ueki Y, Mima T, Kotb MA, Sawada H, Saiki H, Ikeda A, Begum T, Reza F, Nagamine T, Fukuyama H (2006) Altered plasticity of the human motor cortex in Parkinson’s disease. Ann Neurol 59:60–71
Acknowledgment
The study was supported by a stipend of the Deutsche Forschungsgemeinschaft (DFG NO737/4-1) to Dennis A. Nowak.
Conflict of interest statement
None of the authors has any financial disclosures regarding the present manuscript. The study was supported by a grant of the Deutsche Forschungsgemeinschaft (DFG) to Dennis A. Nowak (NO 737/4-1).
Author information
Authors and Affiliations
Corresponding author
Additional information
U. Grüner and C. Eggers have contributed equally to the study.
Rights and permissions
About this article
Cite this article
Grüner, U., Eggers, C., Ameli, M. et al. 1 Hz rTMS preconditioned by tDCS over the primary motor cortex in Parkinson’s disease: effects on bradykinesia of arm and hand. J Neural Transm 117, 207–216 (2010). https://doi.org/10.1007/s00702-009-0356-0
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00702-009-0356-0