Abstract
Background
The optimal targets for deep brain stimulation (DBS) in patients with refractory chronic pain are not clearly defined. We applied sensory functional MRI (fMRI)- and diffusion tensor imaging (DTI)-based DBS in chronic pain patients into 3 different targets to ascertain the most beneficial individual stimulation site.
Methods
Three patients with incapacitating chronic pain underwent DBS into 3 targets (periventricular gray (PVG), ventroposterolateral thalamus (VPL), and posterior limb of the internal capsule according to fMRI and DTI (PLIC). The electrodes were externalized and double-blinded tested for several days. Finally, the two electrodes with the best pain reduction were kept for permanent stimulation. The patients were then followed up for 12 months. Outcome measures comprised the numerical rating scale (NRS), short-form McGill’s score (SF-MPQ), and health-related quality of life (SF-36).
Results
Continuous pain (mean NRS 6.6) was reduced to NRS 3.6 after 12 months. Only with stimulation of the PLIC pain attacks, that occurred at least 3 times a week (mean NRS 9.6) resolved in 2 patients and improved in one patient concerning both intensity (NRS 5) and frequency (twice a month). The mean SF-MPQ decreased from 92.7 to 50. The health-related quality of life improved considerably.
Conclusion
fMRI- and DTI-based DBS to the PLIC was the only target with a significant effect on pain attacks and seems to be the most promising target in chronic pain patients after brachial plexus injury. The combination with PVG or VPL can further improve patients’ outcome especially in terms of reducing the continuous pain.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Chronic pain is a challenging healthcare issue, affecting approximately 5% of the population [4]. Apart from insufficient relief with conventional treatment [19], it is associated with impairment in cognition and attention [13] as well as decline of social functioning due to dependence on opioids [7]. Particularly severe, pharmacotherapy-refractory neuropathic pain occurs in 25% of patients after brachial plexus injury [14]. These patients often suffer from continuous burning or throbbing pain which has shown to be associated with thalamic neuroplasticity and shooting pain attacks due to hyperactivity of the dorsal horn [15, 16]. After failure of pharmacotherapy, neuromodulative treatment options such as spinal cord stimulation, motor cortex stimulation, and deep brain stimulation (DBS) may have a favorable effect [5].
DBS is an established therapy for movement disorders and has been performed in patients with chronic pain since the early 1970s [6]. Till now, this indication for DBS is performed in off-label use, since none of the manufacturers of DBS equipment has an FDA or CE approval for pain treatment. Several studies reported inconsistent pain reduction and adverse effects following DBS (for review, see Farrell et al. [5]). Target regions vary, whereby the sensory nuclei of the thalamus [12] (VPL); the periventricular gray (PVG) [9] and the posterior limb of the internal capsule (PLIC) [2] seem to be promising regions. Target adjustments of VPL and PVG can be performed considering the third ventricle or the border of the internal capsule. In the past, target localization of the internal capsule was determined according to standardized atlas coordinates with no correction pertaining to the individual anatomy. While the optimal target within the internal capsule cannot be reliably determined through anatomical MRI (T1 or T2), newer developments like diffusion tensor imaging (DTI) and functional MRI (fMRI) may allow for better targeting of individual pain processing regions.
Therefore, we compared 2 standard DBS targets (VPL and PVG) with a new individualized fMRI- and DTI-based targeting of the PLIC to ascertain the most beneficial individual stimulation site.
Methods
Patients
Three patients with therapy-refractory severe chronic neuropathic pain after brachial plexus injury were selected for DBS through expanded access with off-label use. All three patients suffered from continuous burning pain (mean NRS 7.3) and pain attacks (mean NRS 9.6) at least 3 times a week despite extensive pharmacotherapy (3 patients), spinal cord stimulation (3 patients), and intrathecal morphine pump (2 patients). These pain attacks persisted for several hours detaining the patients from taking part in normal social interactions (for patient characteristics see Table 1). The pain region were the right hand, wrist, and the distal lower arm (patient 1), the left wrist (patient 2), and the left hand and distal arm (patient 3). Psychiatric evaluation revealed no underlying psychiatric disorders. Patients 1 and 2 were injured due to a motorcycle accident. Patient 3 suffered from brachial plexus injury after a car accident. All patients were retirees since 2–4 years after their accidents.
Target determination
All patients received a 3 Tesla DTI and sensory fMRI (Siemens Magnetom Verio, Siemens Healthineers, Erlangen, Germany). For preoperative planning, fMRI and EPI BOLD sequences were used with an in-plane resolution of 1.6 mm and slice thickness of 3.36 mm. The diffusion images were acquired using a readout-segmented echo-planar (RESOLVE) diffusion sequence with TE = 64 ms and TR = 8500 ms. A total of 20 diffusion sampling directions were acquired. The b value was 800 s/mm2. The in-plane resolution was 2.7 mm and the slice thickness was 2.5 mm. To visualize the cortical sensory region, the pain regions of the patients were stimulated with a surgical brush during the fMRI acquisition.
Tractography was performed using a multi-ROI approach. The fMRI activation obtained as described above was used as a primary region of interest (ROI) for the fiber tracking of the spino-thalamo-cortical tract, with manually defined thalamus segmentation serving as the second targeted ROI. The third ROI was defined within the brain stem. The PLIC was targeted within the displayed portion of the spino thalamo-cortical tract (17–19 mm lateral, about 6 mm anterior to the posterior commissure (PC) and at the dorsoventral level of the PC). The VPL was targeted approximately 2–3 mm medial to the border of the internal capsule and at the level of the PC (z = 0). The PVG was targeted 2–3 mm lateral to the wall of the third ventricle, at the level of the PC (z = 0). BrainLab iPlan 3.0 (BrainLab AG, Feldkirchen, Germany) was used for fMRI analysis, fibertracking, and trajectory planning. The image processing method is shown in Fig. 1.
a Postcentral sensory fMRI activation of the pain region (hand, distal arm) of patient 3. b Three ROIs were used to display the spino-thalamo-cortical tract (blue and violet): the postcentral fMRI activation (red) was used to define the cortical ROI, the thalamus (light blue) was segmented manually and a box ROI in brain stem was used. Planned electrode trajectory for the PLIC - spino-thalamo-cortical electrode (light blue). c Postoperative CT shows the planned electrode projected inside of the displayed spino-thalamo-cortical tract (CT registered to the tractography result and encircled). From above in clockwise direction, the PLIC electrode as well as the VPL and PVG electrodes are visible in the axial CT plane
Operating procedure and data acquisition
The surgery was done as an expanded access in off-label use. Accordingly, the patients gave their consent for the surgery and for publication of possible results. Because of the observational manner with a treatment as expanded access, ethical approval was not necessary.
The MRI was merged with a computer tomography (CT) with a stereotactic frame. The operation was performed under general anesthesia. All three patients received lead placement into the PVG, VPL, and PLIC contralateral to their affected limb (Vercise Cartesia directional leads, Vercise PC, Boston Scientific). Thereby, lead ring contact 2 (first directional contact) was placed in the target region. The entry point for PVG and VPL was the coronal suture. The lead trajectory for the PLIC stimulation was chosen regarding the pathway of the DTI in the center of the projected fiber tract at the height of the AC-PC line. Thereby, the planned trajectory covered over 10 mm along the fibers. This resulted in a deviation of the target coordinates of 2–3 mm latetal and 0–0.5 mm anterior. The extrapolation of the trajectory to the skull defined the entry point at the postcentral gyrus. To avoid vessels and sulci, the entry points of all electrodes were shifted gradually.
The leads were connected to extensions and externalized for trial stimulation. Lead placement was conformed through stereotactic CT. After the surgery, double-blinded trial-stimulations during two consecutive days were performed in order to identify the most beneficial targets. Thereby, every target was tested separately without combinations for several hours. First, the test stimulation was done with 130 Hz and 90 μs to determine the individual lead contact for pain modulation. During this high frequency stimulation, patients reported on burning pain in various body regions. Thereby, all patients were programmed for directional stimulation, to enable a highly selective activation of the individual pain region. Afterwards, the frequency was reduced to 40 Hz and the impulse width was increased to 400 μs. With these stimulation parameters, patients were tested whether an acute pain reduction/modulation of the continuous pain or the pain attacks could be achieved. The period of the test stimulation was so short because of rapid and pronounced effects during the test stimulation. The effect with reduced pain was observed immediately after turning on the stimulation for pain attacks and after 1 h for continuous pain. After pain reduction, the therapeutic window was determined till stimulation-dependent side effects occurred. Thereby, side effects were paresthesia in other body regions than the pain region, double vision, speech arrest, or dizziness. The test stimulation of every contact was done for 3 h per day. Within this time, stimulation-dependent side-effects and pain-reducing effects were recorded. After turning the stimulation off, there was a rebound effect regarding the pain attacks and the continuous pain. The two most effective electrodes were selected and connected to new extensions and a stimulator for permanent treatment in a second procedure. The remaining third electrode was removed together with the externalized extensions. Afterwards, further optimization of the stimulation parameters was performed during 1 week. For the stimulation parameters, see Table 1. Follow-up visits took place at 1, 3, 6, 9, and 12 months after the surgery and comprised recordings of the numerical rating scale (NRS), short-form McGill Pain Questionnaire (SF-MPQ), and health-related quality of life (SF-36).
Statistics
The values are expressed as means; standard deviations were not regarded as helpful given the small sample size. As no normal distribution was to be expected and a Wilcoxon signed-rank test could not be calculated with only three subjects, we chose a Mann-Whitney U test. The significance level was set at 0.05. The statistical calculations were performed in SPSS Version 24 (IBM, Amonk, NY, USA).
Results
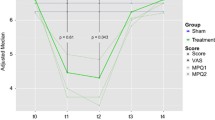
Directional stimulation of VPL (patients 1 and 2), PVG (patient 3), and PLIC (all 3 patients) reduced the pain with low-frequency stimulation. Utilizing the directional properties of the segmented lead poles in order to shape the electrical field was helpful in all three patients in order to maximize desired stimulation effects while avoiding adverse effects. While the stimulation of the PVG or VPL reduced the burning continuous pain, both targets had no immediate effect on the severe pain attacks. Up to 12 months after combined DBS, the continuous pain was reduced significantly to a mean of NRS 3.0 (p = 0.0053; Fig. 2a). Stimulation of the PLIC resolved the pain attacks in 2 patients and reduced them in one patient resulting in weaker attacks (NRS 4) less frequently (twice a month vs. three times a week) (Fig. 2b). During adjustments of the stimulation at follow-up visits, deactivation of the electrode stimulating the PLIC was not tolerated for a period longer than a few days, since the severe pain attacks returned shortly after deactivation. In contrast, deactivation of the PVG- or VPL-lead for 2 weeks revealed an only a slight increase of the continuous pain up to mean NRS 4.7.
During combined stimulation for 12 months, mean SF-MPQ decreased from 92.7 to 50 (p = 0.0466; Fig. 2c). Likewise, the health-related quality of life improved considerably (Fig. 3). The most pronounced improvements were observed in the subsections pain (mean 0 vs. 73.3; p = 0.000022), social functioning (mean 16.6 vs. 69.2; p = 0.000925), emotional well-being (mean 22.7 vs. 77.3; p < 0.00001), and role limitation due to emotional problems (mean 22.2 vs. 100; p = 0.012451). No complications occurred.
Discussion
We hereby describe initial experience of the combination of DTI- and sensory fMRI-based individual targeting of directional DBS in three patients with chronic neuropathic pain after brachial plexus injury. While targeting of PVG and VPL is possible regarding the local anatomy [17], the target localization of the PLIC is more challenging due to the passing fiber tracts and may be associated with undesired effects of stimulation. With the combination of DTI and sensory fMRI with directional leads which allow altering of the shape of the stimulation fields, all three patients experienced significant reduction of both continuous pain and pain attacks combined with an improved quality of life and social participation. Importantly, this was achieved without any stimulation-dependent side effects. Regarding the reconstructed lead coordinates within the PLIC, the stimulation seems to modulate fibers of the spinothalamocortical tract (STC) as identified with DTI [8]. Stimulation of this region has been shown to alleviate thalamic pain [10]. The STC exerts an enhanced descending influence on ventroposterior thalamic nuclei during pain processing [18]. Particularly, it is involved in the sensory discriminative aspect of pain [11]. But in contrast to thalamic pain which affects the entire contralateral half of the body and thus requires stimulation that does not discriminate for somatotopy, patients with plexus injury need a precisely selected stimulation site. Combined stimulation of the STC and the VPL/PVG adds further pain relief, whereas the exact pathomechanisms remains unclear.
With this presented approach, the therapeutic effects with reduction of continuous pain (59.1%) and pain attacks (86.2%) are very promising. Comparable preexisting studies revealed a general pain reduction of only 40% [1] and 43% [3]. However, the differentiation between continuous pain and pain attacks so far is described unsatisfactorily in the available literature.
Our study is limited by the small sample size and its open design. However, in view of the impressive pain reduction in chronic pain patients after brachial plexus injury, fMRI- and DTI-based targeting of the PLIC should be considered in these patients. In this respect, our study may serve to enhance the methods employed in DBS for chronic pain, and further studies should evaluate if the described targeting method can lead to comparable outcome in other chronic pain patients.
In summary, fMRI- and DTI-based DBS within the PLIC combined with PVG or VPL showed promising results in patients with chronic neuropathic pain after brachial plexus injury. Stimulation of the PVG and VPL reduced permanent pain, but had no effect on pain attacks, while the stimulation of the PLIC was highly efficient for the pain attacks, that were described by the patients as the worst burden for quality of life. However, larger trials are needed to substantiate the evidence.
References
Abreu V, Vaz R, Rebelo V, Rosas MJ, Chamadoira C, Gillies MJ, Aziz TZ, Pereira EAC (2017) Thalamic deep brain stimulation for neuropathic pain: efficacy at three years follow-up. Neuromodulation 20:504–513
Adams JE, Hosobuchi Y, Fields HL (1974) Stimulation of internal capsule for relief of chronic pain. J Neurosurg 41:740–744
Boccard SGJ, Prangnell SJ, Pycroft L, Cheeran B, Moir L, Pereira EAC, Fitzgerald JJ, Green AL, Aziz TZ (2017) Long-term results of deep brain stimulation of the anterior cingulate cortex for neuropathic pain. World Neurosurg 106:625–637
Bouhassira D, Lanteri-Minet M, Attal N, Laurent B, Touboul C (2008) Prevalence of chronic pain with neuropathic characteristics in the general population. Pain 136:380–387
Farrell SM, Green A, Aziz T (2018) The current state of deep brain stimulation for chronic pain and its context in other forms of neuromodulation. Brain Sci 8
Gol A (1967) Relief of pain by electrical stimulation of the septal area. J NeurolSci 5:115–120
Gureje O, Von KM, Simon GE, Gater R (1998) Persistent pain and well-being: a World Health Organization study in primary care. JAMA 280:147–151
Hong JH, Son SM, Jang SH (2010) Identification of spinothalamic tract and its related thalamocortical fibers in human brain. Neurosci Lett 468:102–105
Hosobuchi Y, Adams JE, Linchitz R (1977) Pain relief by electrical stimulation of the central gray matter in humans and its reversal by naloxone. Science 197:183–186
Hunsche S, Sauner D, Runge MJ, Lenartz D, El MF, Treuer H, Sturm V, Maarouf M (2013) Tractography-guided stimulation of somatosensory fibers for thalamic pain relief. Stereotact Funct Neurosurg 91:328–334
Marchand S (2008) The physiology of pain mechanisms: from the periphery to the brain. Rheum Dis Clin N Am 34:285–309
Mark VR, ERVIN FR (1965) Role of thalamotomy in treatment of chronic severe pain. Postgrad Med 37:563–571
Moriarty O, McGuire BE, Finn DP (2011) The effect of pain on cognitive function: a review of clinical and preclinical research. Prog Neurobiol 93:385–404
Narakas A (1978) Surgical treatment of traction injuries of the brachial plexus. Clin Orthop Relat Res 71–90
Parry CB (1980) Pain in avulsion lesions of the brachial plexus. Pain 9:41–53
Parry CB (1984) Pain in avulsion of the brachial plexus. Neurosurgery 15:960–965
Pereira EA, Aziz TZ (2014) Neuropathic pain and deep brain stimulation. Neurotherapeutics 11:496–507
Wang JY, Chang JY, Woodward DJ, Baccala LA, Han JS, Luo F (2007) Corticofugal influences on thalamic neurons during nociceptive transmission in awake rats. Synapse 61:335–342
Wilkinson HA (2000) Bilateral anterior cingulotomy for chronic noncancer pain. Neurosurgery 46:1535–1536
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
The surgery of the three patients was done as an expanded access in off-label use.
Informed consent
Informed consent was obtained from all individual participants included in the surgery and for publication of the results.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
This article is part of the Topical Collection on Functional Neurosurgery - Pain
Rights and permissions
About this article
Cite this article
Polanski, W.H., Zolal, A., Klein, J. et al. Somatosensory functional MRI tractography for individualized targeting of deep brain stimulation in patients with chronic pain after brachial plexus injury. Acta Neurochir 161, 2485–2490 (2019). https://doi.org/10.1007/s00701-019-04065-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-019-04065-2