Abstract
Introduction
Repetitive magnetic stimulation (rMS) is a safe and well-tolerated intervention. Transcranial magnetic stimulation (TMS) is used for the treatment of depression and for the treatment and prevention of migraine. Over the last few years, several reports and randomised controlled studies of the use of rMS for the treatment of pain have been published. The aim of this systematic review was to identify the available literature regarding the use of rMS in the treatment of peripheral neuropathic pain.
Methods
After a systematic Medline search we identified 12 papers eligible to be included in this review.
Results
The majority of the studies were on patients with phantom limb pain, followed by radiculopathy, plexopathy, post-traumatic pain and peripheral neuropathy. The treatment protocols vary significantly from study to study and, therefore, pooling the results together is currently difficult. However, rMS has a definite immediate effect in pain relief which, in the majority of studies, is maintained for a few weeks.
Conclusion
rMS seems to be a promising intervention in the treatment of peripheral neuropathic pain. Further research is in the field is needed. Use of neuronavigation might increase the precision of stimulation and subsequently its effectiveness.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Both peripheral and central repetitive magnetic stimulation have been employed for the treatment of peripheral neuropathic pain. |
Repetitive magnetic stimulation has potential in the treatment of peripheral neuropathic pain. |
Use of neuronavigation might increase the precision of stimulation and subsequently the effectiveness of repetitive magnetic stimulation. |
Assessment of brain networks might be the way forward to developing an objective means of studying the effect of repetitive magnetic. stimulation. |
Introduction
Transcranial magnetic stimulation (TMS) is a neurostimulation and neuromodulation technique based on the principle of electromagnetic induction of an electric field in the brain [1]. Anthony T. Barker was the first to explore the use of magnetic fields to alter electrical signalling within the brain, in Sheffield, and the first stable TMS devices were developed in 1985 [2].
The therapeutic utility of repetitive TMS (rTMS) has been demonstrated in a variety of neurological [3] and psychiatric conditions [4] and has already been approved as a treatment for depression and migraine in many countries. TMS is a safe and well-tolerated intervention whilst serious adverse events during TMS are rare [5].
Neuropathic pain is a common presenting complaint of patients with peripheral neuropathy (PN) and is considered one of the most detrimental aspects of the condition with regards to patients’ quality of life [6,7,8,9,10,11,12,13]. It is therefore imperative for robust pain therapeutic interventions to be innovated, improved and implemented.
Over the years, increasing reports of the clinical utility of magnetic stimulation (MS) in the management of peripheral neuropathic pain and in particular rMS delivered either through a peripheral or transcranial route have been attempted with promising results.
The aim of this work was to systematically review the current literature regarding the use of rMS for the management of peripheral neuropathic pain. We aimed to describe the different treatment protocols that have been used and their efficacy in order to establish the therapeutic utility of rMS in the management of peripheral neuropathic pain.
Methods
Search Strategy
A systematic computer-based literature search was conducted on 12 June 2019 using the PubMed database. We evaluated all articles published between the dates of 1 January 1999 and 12 June 2019. For the search, we used three Medical Subject Heading (MeSH) terms that had to be present in the title or the abstract. Term A was “neuropathy” or “phantom limb” or “polyneuropathy” or “peripheral” or “neuronopathy” or “radiculopathy” or “polyradiculopathy” or “dorsal” or “low back”. Term B was “magnetic stimulation” or “magnetic therapy” or “electromagnetic”. Term C was “pain” or “painful”. No filters were applied to our search.
Inclusion and Exclusion Criteria
In order to be included in this review articles were required to meet the following criteria: (1) be original articles; (2) involve study of human subjects; (3) be written in the English language; (4) refer to transcranial magnetic stimulation or peripheral magnetic stimulation; (5) refer to pain because of peripheral nervous system involvement. The exclusion criteria for the articles were as follows: (1) book chapters, reviews, meta-analyses, systematic reviews, letters to the editor and editorials not providing new data and study protocols; (2) articles which did not discuss magnetic or electromagnetic stimulation as a management option; (3) articles with a lack of individual results for the management of painful peripheral neuropathies, even if those subjects were included in the study; (4) articles not referring to patients with painful peripheral neuropathies.
Synthesis of Results
The study is reported in accordance with the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines [6]. Where studies did not provide raw values in graphically displayed results, an open-source programme was used to extract raw data (Engauge Digitizer, http://markummitchell.github.io/engauge-digitizer). A database was developed using the Statistical Package for Social Sciences, version 24 for Mac. Pooled frequencies and descriptive characteristics of demographic parameters were extracted.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Results
Our literature search strategy identified 332 articles. Of these, 12 met the inclusion criteria and were included and analysed in this review. Of them five were randomised controlled trials (RCTs), two were small case series and five single case reports. The majority of the papers (50%) tested the use of rMS in phantom limb pain, followed by radiculopathy (17%), brachial plexopathy (17%), post-traumatic pain (8%) and peripheral neuropathy (8%).
The PRISMA chart displays the process of article selection (Fig. 1). Table 1 summarizes the characteristics of the papers included and gives a detailed summary of the treatment protocols and outcomes.
Phantom Limb Pain
Phantom limb pain (PLP) is difficult to treat and often responds poorly to conventional pain management [15, 16]. Phantom limb sensations can be experienced following amputation. Phantom limb-like sensations can also be seen in patients with spinal cord injury, nerve avulsions and with congenital limb aplasia [17]. In PLP, maladaptive plasticity and reduced connectivity in interhemispherical and sensorimotor networks play a major role in pain. rTMS has been tested in PLP as a tool for blocking maladaptive plasticity in the sensorimotor cortex and has shown analgesic effects when used on the motor cortex, through modulating cortical reorganisation [18]. One particular study has shown that amputees with PLP have a significantly greater activation in the primary motor cortex and supplementary motor cortex of the affected hemisphere compared to those without pain, likely due to increased excitability after limb amputation [19].
Malavera et al. studied the effects of rTMS in the treatment of PLP in a randomised double-blinded placebo-controlled study [16]. Fifty-four patients underwent real or sham rTMS of the primary motor area contralateral to the amputated limb. The analgesic effect of the treatment was significant for the first 15 days; however, it was not after 30 days. The analgesic effect found in this study can possibly be explained by the effect of rTMS over the central pathophysiological mechanisms relating to PLP. After a traumatic amputation, maladaptive reorganisation of the sensorimotor cortex involves a reduction in intracortical inhibition mechanisms, an imbalance between γ-aminobutyric acid (GABA) and glutamate and an increase in excitability of corticospinal neurons. High frequency rTMS over the motor cortex enhances its excitability leading to the indirect activation of inhibitory projections towards the thalamus, resulting in the modulation of pain signalling pathways [16].
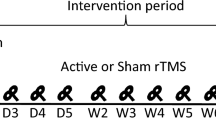
In contrast to the RCT conducted by Malavera et al., a study by Ahmed et al. showed a significant and prolonged reduction of pain in patients with PLP receiving real rTMS versus sham. The authors randomised patients to receive either real rTMS (n = 17) or sham rTMS (n = 10). Sham rTMS involved elevating and angling the magnetic coil away from the cortex. The authors found a 55% reduction in pain in the treatment group immediately following the fifth session. This effect was still seen at 2 months follow-up [20]. Interestingly the percentage of pain reduction was higher in patients with upper limb phantom pain compared to patients with lower limb phantom pain. Whilst the results reported are positive, there are multiple drawbacks in the methodology within this study including non-standard randomisation criteria, small sample size and unequal group allocation. Additionally, the study recruited a heterogenous population of patients affected by PLP, in both upper (n = 11) and lower limbs (n = 16).
Navigated TMS employs conventional TMS combined with sophisticated neuronavigational software providing precise anatomical information necessary for anatomically controlled cortical stimulation. It can be used to stimulate highly selected areas in the brain in PLP. It promotes the modulation of brain connectivity to induce its rearrangement in chronic pain syndromes. In a patient with PLP, Scibilia et al. used high frequency stimulation (10 Hz) of the primary motor area and the dorsolateral frontal cortex contralateral to the pain, and low frequency (1 Hz) stimulation of the primary somatosensory area contralateral to the pain, using navigated TMS [21]. Using resting state functional magnetic resonance, they showed that rTMS promoted cortical and subcortical plasticity, which led to an associated pain reduction. After treatment, the patient experienced a significant reduction of 5 points on the visual analogue scale (VAS) in terms of pain. This suggests that high frequency stimulation of the motor cortex contralateral to site of PLP can induce an analgesic effect. As this was a single case report, larger cohort studies are warranted to validate these findings.
In cases such as motor function recovery post stroke, stimulation with low frequency rTMS in the unaffected hemisphere has shown beneficial results [22]. Di Rollo et al. reported the effect of stimulating the hemisphere ipsilateral to the PLP in a single patient [15]. The patient showed a 33% reduction in pain at the end of the third week of treatment and a decrease of 17% at the follow-up visit which was 3 weeks after the last session.
Lee et al. described a case report of PLP treated with rTMS of the supplementary motor cortex and the primary motor cortex, using neuronavigation. Magnetic therapy dramatically reduced the pain intensity when directed over the supplementary motor cortex; however, there was no reduction in pain with therapy directed over the primary motor cortex [23]. The authors postulate that this is due to a reported greater activation of the supplementary motor cortex in amputees with PLP than those without [24]. These results, however, are to be taken with caution, owing to the patient receiving one round of treatment to the primary motor cortex, versus five rounds to the supplementary motor cortex.
Grammer et al. reported a patient with upper extremity PLP. Over 6 weeks they delivered 28 sessions of rTMS to the dorsolateral prefrontal cortex and primary sensory area contralateral to the side of pain. The sessions were of low frequency (1 Hz) for the first five sessions, thereafter alternating between low frequency (1 Hz) and high frequency (10 Hz). This protocol led to an 80% decrease in pain as rated on the VAS [25].
Radiculopathy
Attal et al. studied the efficacy of rTMS in patients suffering from neuropathic pain secondary to unilateral lower lumbar radiculopathy in an RCT. In tandem with this they compared the efficacy of rTMS to transcranial direct current stimulation (tDCS), which applies low intensity electrical currents directly, rather than the magnetic field employed in rTMS [26]. In an altered crossover methodology, they randomised 36 patients to receive either active rTMS and tDCS or sham rTMS and tDCS, with a 3-week period between either modality. Results showed that rTMS was more effective than tDCS and sham (tDCS and rTMS), after the third and final stimulation session. Repetitive magnetic stimulation maintained its efficacy over sham when pain was measured 5 days after the final session, but not in comparison to tDCS. The study was limited by its relatively short treatment and follow-up period.
Töpper et al. evaluated the use of rTMS in two patients with PLP-like syndrome who had suffered cervical nerve root (C7 and C8) injuries secondary to road traffic collisions [27]. The authors investigated two separate protocols of rTMS directed over the posterior parietal cortex contralateral to the symptomatic side. The first included high frequency stimulation (10 Hz) and the second low frequency (1 Hz). The two protocols were separated by at least 4 weeks. Whilst the authors reported a significant reduction in pain measured with VAS during the rTMS treatment, this effect was seen only for up to 15 min after therapy. The study is, however, limited by its small number of participants.
Brachial Plexopathy
In an RCT of 34 patients with traumatic brachial plexopathy, Khedr et al. evaluated the efficacy of rTMS as an adjuvant intervention to physical therapy, consisting of electrical stimulation, ultrasound, heat therapy and therapeutic/active exercises [28]. Magnetic stimulation was directed over the superior trapezius muscle, using stimulation at both 3 Hz (aiming to increase strength) and 15 Hz (aiming to relieve pain). The authors reported a significant reduction in the VAS score in patients receiving real therapy compared to sham therapy. This effect was seen both at the end of the therapy and at 1-month follow-up. The study is limited by the fact that the sham protocol was substandard as the authors used an active coil that was elevated away from the muscle, rather than a sham coil applied directly over the muscle [29].
In a case report of a 37-year-old patient with brachial plexopathy, Lefaucheur et al. assessed the efficacy of high frequency rTMS targeting the precentral gyrus [30]. Over a treatment period of 16 months, they found that rTMS provided a statistically significant reduction in VAS scores. Whilst the study provides evidence of long-term use of rTMS, it is limited by being a single patient report with no matched control.
Post-traumatic Neuropathic Pain
Peripheral nerve injury can lead to the formation of a neuroma which results from abnormal nerve regeneration, which is often refractory to medications and invasive interventions. In a small case series reported by Leung et al., five patients tolerated well low frequency TMS over the site of the neuroma formation and showed long-term pain relief [31]. This is in line with other studies demonstrating that low frequency rTMS provides an inhibitory effect on neuronal activities. However, this study is limited by its small sample size, lack of control and unclear frequency of treatment sessions.
Peripheral Neuropathy
Peripheral neuropathy is common amongst the diabetic population [32]. In a cross-over RCT Onesti et al. were the first to investigate the effect of deep rTMS, achieved by using the H-coil in 25 patients with diabetic neuropathic pain. The H-coil allows safe access to deep cortical areas which otherwise could not be accessed [33] and has been proven to be effective in the management of major depressive disorder, bipolar disorder and focal dystonias [34,35,36]. In this study the authors used deep real or sham rTMS of the lower limb motor cortex. The authors reported that real rTMS at 20 Hz reduces chronic drug-resistant distal diabetic neuropathic pain for 3 weeks.
Conclusions
Chronic pain perception has been found to propagate through central brain sensitisation, particularly involving the prefrontal cortex and the thalamus, in comparison to acute pain scenarios primarily recruiting the spinothalamic pathways [37]. This presents an opportunity to identify therapeutic interventions that are able to target this central processing of pain. Magnetic stimulation exerts its effect by the magnetic field generated inducing a subsequent electrical field that is able to depolarise axons and therefore modulate active neural networks within the cortex [38]. This effect may differ depending on factors such as the magnetic pulse waveform, the intensity, frequency and pattern of stimulation [38]. There is consensus in the literature that low frequency stimulation (< 1 Hz) and high frequency stimulation (> 5 Hz) are responsible for suppression and facilitation of corticospinal excitability, respectively [39]. There is some consensus that high frequency rather than low frequency stimulation is able to illicit an analgesic effect in neuropathic pain [38]. Indeed, a similar conclusion may be drawn from the studies that have been included in this review.
On a molecular level, rTMS has been reported to induce endogenous opioid release, with one study demonstrating a reduction of the analgesic effect when stimulating the primary motor cortex in subjects administered naloxone. The authors did not find this to be the case when rTMS was applied to the dorsolateral prefrontal cortex [40]. It is important to note, however, that naloxone is known to play a role in reducing the perceived analgesic effect derived through placebo [41]. Various other neurochemicals have been reported to be implicated during rTMS therapy, including GABA, glutamate and dopamine. Glutamate N-methyl-d-aspartate (NMDA) receptors are known to be responsible for synaptic plasticity and have been reported to be associated with the long-term analgesic effect of rTMS [42]. In the context of PLP in particular, high frequency rTMS may indirectly activate inhibitory thalamic projections, thereby modulating ascending nociceptive pathways [43]. Neuropathic pain of diverse aetiologies has been shown to be associated with decreased intracortical inhibition (ICI) and interestingly rTMS therapy has been correlated with increased ICI in tandem with pain relief, particularly in patients with drug-resistant neuropathic pain [44]. Functional magnetic resonance imaging has revealed that rTMS of the motor cortex results in subsequent activity within the ipsilateral thalamus and putamen, structures known to be linked to the sensorimotor cortex, implicated in the centralisation of pain [45].
This review identified five RCTs, highlighting a paucity in the literature of well-designed placebo-controlled trials evaluating rMS for relief of peripheral neuropathic pain. Although the majority of the studies included in this review show that rMS has potential for the treatment of peripheral neuropathic pain, there is a need for further studies in the field. Whilst its efficacy is still debated, rMS has been demonstrated to be a safe and tolerated intervention, with no serious adverse effects noted in the studies included in this review. Furthermore, there is a need to create consensus regarding optimum stimulation protocols and procedures [46]. The use of neuronavigation might increase the precision of stimulation and subsequently its effectiveness; however, this requires further robust assessment as current evidence is lacking. Finally, assessment of brain network function, with techniques such as functional magnetic resonance or appropriate TMS-compatible EEG recordings, with various quantitative EEG metrics, might be the way forward to developing an objective means of studying the effect of rMS on widely distributed brain network constituents involved in the generation and persistence of neuropathic pain.
Limitations
-
As in all studies measuring pain with the VAS, a self-reported questionnaire, there is potential for an inherent response bias when reporting the nature and extent of the pain.
-
The variations in treatment protocols between studies and the limited number of studies eligible for inclusion make it impossible to use a meta-analytic approach.
-
A more comprehensive search using databases other than PubMed alone might have identified a greater number of articles suitable for analysis.
References
Rossi S, Hallett M, Rossini PM, et al. Safety, ethical considerations, and application guidelines for the use of transcranial magnetic stimulation in clinical practice and research. Clin Neurophysiol. 2009;120(12):2008–39.
Barker AT, Jalinous R, Freeston IL. Non-invasive magnetic stimulation of human motor cortex. Lancet. 1985;325(8437):1106–7.
Eldaief MC, Press DZ, Pascual-Leone A. Transcranial magnetic stimulation in neurology. A review of established and prospective applications. Neurol Clin Pract. 2013;3(6):519–26.
Aleman A. Use of repetitive transcranial magnetic stimulation for treatment in psychiatry. Clin Psychopharmacol Neurosci. 2013;11(2):53–9.
Zis P, Shafique F, Hadjivassiliou M, et al. Safety, tolerability, and nocebo phenomena during transcranial magnetic stimulation: a systematic review and meta-analysis of placebo-controlled clinical trials. Neuromodul Technol Neural Interface. 2019. https://doi.org/10.1111/ner.12946.
Girach A, Julian TH, Varrassi G, Paladini A, Vadalouka A, Zis P. Quality of life in painful peripheral neuropathies: a systematic review. Pain Res Manag. 2019;2019:2091960.
Zis P, Sarrigiannis PG, Rao DG, Sanders DS, Hadjivassiliou M. Small fiber neuropathy in coeliac disease and gluten sensitivity. Postgrad Med. 2019;131(7):496–500.
Michaelides A, Hadden RDM, Sarrigiannis PG, Hadjivassiliou M, Zis P. Pain in chronic inflammatory demyelinating polyradiculoneuropathy: a systematic review and meta-analysis. Pain Ther. 2019;8(2):177–85.
Zis P, Sarrigiannis PG, Rao DG, Hewamadduma C, Hadjivassiliou M. Chronic idiopathic axonal polyneuropathy: prevalence of pain and impact on quality of life. Brain Behav. 2019;9(1):e01171.
Zis P, Sarrigiannis PG, Rao DG, Hadjivassiliou M. Gluten neuropathy: prevalence of neuropathic pain and the role of gluten-free diet. J Neurol. 2018;265(10):2231–6.
Zis P, Sarrigiannis P, Rao D, Hadjivassiliou M. Quality of life in patients with gluten neuropathy: a case-controlled study. Nutrients. 2018;10(6):662.
Brozou V, Vadalouca A, Zis P. Pain in platin-induced neuropathies: a systematic review and meta-analysis. Pain Ther. 2018;7(1):105–19.
Zis P, Paladini A, Piroli A, McHugh PC, Varrassi G, Hadjivassiliou M. Pain as a first manifestation of paraneoplastic neuropathies: a systematic review and meta-analysis. Pain Ther. 2017;6(2):143–51.
Moher D, Liberati A, Tetzlaff J, Altman DG. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol. 2009;62(10):1006–12.
Di Rollo A, Pallanti S. Phantom limb pain: low frequency repetitive transcranial magnetic stimulation in unaffected hemisphere. Case Rep Med. 2011;2011:130751.
Malavera A, Silva FA, Fregni F, Carrillo S, Garcia RG. Repetitive transcranial magnetic stimulation for phantom limb pain in land mine victims: a double-blinded, randomized, sham-controlled trial. J Pain. 2016;17(8):911–8.
Bókkon I, Till A, Grass F, Erdöfi Szabó A. Phantom pain reduction by low-frequency and low-intensity electromagnetic fields. Electromagn Biol Med. 2011;30(3):115–27.
Nardone R, Versace V, Sebastianelli L, et al. Transcranial magnetic stimulation in subjects with phantom pain and non-painful phantom sensations: a systematic review. Brain Res Bull. 2019;148:1–9.
Dettmers C, Adler T, Rzanny R, et al. Increased excitability in the primary motor cortex and supplementary motor area in patients with phantom limb pain after upper limb amputation. Neurosci Lett. 2001;307(2):109–12.
Ahmed MA, Mohamed SA, Sayed D. Long-term antalgic effects of repetitive transcranial magnetic stimulation of motor cortex and serum beta-endorphin in patients with phantom pain. Neurol Res. 2011;33(9):953–8.
Scibilia A, Conti A, Raffa G, et al. Resting-state fMR evidence of network reorganization induced by navigated transcranial magnetic repetitive stimulation in phantom limb pain. Neurol Res. 2018;40(4):241–8.
Khedr EM, Abdel-Fadeil MR, Farghali A, Qaid M. Role of 1 and 3 Hz repetitive transcranial magnetic stimulation on motor function recovery after acute ischaemic stroke. Eur J Neurol. 2009;16(12):1323–30.
Lee J-H, Byun J-H, Choe Y-R, Lim S-K, Lee K-Y, Choi I-S. Successful treatment of phantom limb pain by 1 Hz repetitive transcranial magnetic stimulation over affected supplementary motor complex: a case report. Ann Rehabil Med. 2015;39(4):630–3.
Diers M, Christmann C, Koeppe C, Ruf M, Flor H. Mirrored, imagined and executed movements differentially activate sensorimotor cortex in amputees with and without phantom limb pain. Pain. 2010;149(2):296–304.
Grammer GG, Williams-Joseph S, Cesar A, Adkinson DK, Spevak C. Significant reduction in phantom limb pain after low-frequency repetitive transcranial magnetic stimulation to the primary sensory cortex. Mil Med. 2015;180(1):e126–8.
Attal N, Ayache SS, De Andrade DC, et al. Repetitive transcranial magnetic stimulation and transcranial direct-current stimulation in neuropathic pain due to radiculopathy: a randomized sham-controlled comparative study. Pain. 2016;157(6):1224–31.
Töpper R, Foltys H, Meister IG, Sparing R, Boroojerdi B. Repetitive transcranial magnetic stimulation of the parietal cortex transiently ameliorates phantom limb pain-like syndrome. Clin Neurophysiol. 2003;114(8):1521–30.
Khedr EM, Ahmed MA, Alkady EAM, Mostafa MG, Said HG. Therapeutic effects of peripheral magnetic stimulation on traumatic brachial plexopathy: clinical and neurophysiological study. Neurophysiol Clin. 2012;42(3):111–8.
Loo CK, Taylor JL, Gandevia SC, McDarmont BN, Mitchell PB, Sachdev PS. Transcranial magnetic stimulation (TMS) in controlled treatment studies: are some “sham” forms active? Biol Psychiatry. 2000;47(4):325–31.
Lefaucheur J-P, Drouot X, Ménard-Lefaucheur I, Nguyen J. Neuropathic pain controlled for more than a year by monthly sessions of repetitive transcranial magnetic stimulation of the motor cortex. Neurophysiol Clin Neurophysiol. 2004;34(2):91–5.
Leung A, Fallah A, Shukla S. Transcutaneous magnetic stimulation (tMS) in alleviating post-traumatic peripheral neuropathic pain states: a case series. Pain Med. 2014;15(7):1196–9.
Callaghan BC, Cheng HT, Stables CL, Smith AL, Feldman EL. Diabetic neuropathy: clinical manifestations and current treatments. Lancet Neurol. 2012;11(6):521–34.
Onesti E, Gabriele M, Cambieri C, Ceccanti M, Raccah R, Di Stefano G, et al. H-coil repetitive transcranial magnetic stimulation for pain relief in patients with diabetic neuropathy. Eur J Pain. 2013;17(9):1347–56.
Harel EV, Rabany L, Deutsch L, Bloch Y, Zangen A, Levkovitz Y. H-coil repetitive transcranial magnetic stimulation for treatment resistant major depressive disorder: an 18-week continuation safety and feasibility study. World J Biol Psychiatry. 2014;15(4):298–306.
Kranz G, Shamim EA, Lin PT, Kranz GS, Hallett M. Transcranial magnetic brain stimulation modulates blepharospasm: a randomized controlled study. Neurology. 2010;75(16):1465–71.
Zangen A, Roth Y, Voller B, Hallett M. Transcranial magnetic stimulation of deep brain regions: evidence for efficacy of the H-coil. Clin Neurophysiol. 2005;116(4):775–9.
Apkarian AV, Bushnell MC, Treede R-D, Zubieta J-K. Human brain mechanisms of pain perception and regulation in health and disease. Eur J Pain. 2005;9(4):463.
Lefaucheur J-P, André-Obadia N, Antal A, et al. Evidence-based guidelines on the therapeutic use of repetitive transcranial magnetic stimulation (rTMS). Clin Neurophysiol. 2014;125(11):2150–206.
Siebner H, Rothwell J. Transcranial magnetic stimulation: new insights into representational cortical plasticity. Exp Brain Res. 2003;148(1):1–16.
de Andrade DC, Mhalla A, Adam F, Texeira MJ, Bouhassira D. Neuropharmacological basis of rTMS-induced analgesia: the role of endogenous opioids. Pain. 2011;152(2):320–6.
Girach A, Aamir A, Zis P. The neurobiology under the placebo effect. Drugs Today. 2019;55(7):469.
DosSantos MF, Ferreira N, Toback RL, Carvalho AC, DaSilva AF. Potential mechanisms supporting the value of motor cortex stimulation to treat chronic pain syndromes. Front Neurosci. 2016;10:18.
Bolognini N, Olgiati E, Maravita A, Ferraro F, Fregni F. Motor and parietal cortex stimulation for phantom limb pain and sensations. Pain. 2013;154(8):1274–80.
Lefaucheur JP, Drouot X, Ménard-Lefaucheur I, Keravel Y, Nguyen JP. Motor cortex rTMS restores defective intracortical inhibition in chronic neuropathic pain. Neurology. 2006;67(9):1568–74.
Bestmann S, Baudewig J, Siebner HR, Rothwell JC, Frahm J. Functional MRI of the immediate impact of transcranial magnetic stimulation on cortical and subcortical motor circuits. Eur J Neurosci. 2004;19(7):1950–62.
O’Connell NE, Marston L, Spencer S, DeSouza LH, Wand BM. Non-invasive brain stimulation techniques for chronic pain. Cochrane Database Syst Rev. 2018;4(4):CD008208.
Acknowledgements
Funding
No funding or sponsorship was received for this study or publication of this article.
Authorship
All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this article, take responsibility for the integrity of the work as a whole, and have given their approval for this version to be published.
Authorship Contributions
Abdullah Aamir and Ayesha Girach contributed equally to this study and share first authorship.
Disclosures
Antonela Paladini is a member of the journal’s Editorial Board. Giustino Varrassi is a Section Editor of this journal. Abdullah Aamir, Ayesha Girach, Ptolemaios Georgios Sarrigiannis, Marios Hadjivassiliou and Panagiotis Zis have nothing to disclose.
Compliance with Ethics Guidelines
This article is based on previously conducted studies and does not contain any studies with human participants or animals performed by any of the authors.
Data Availability
Data sharing is not applicable to this article as no datasets were generated or analysed during the current study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Enhanced Digital Features
To view enhanced digital features for this article go to https://doi.org/10.6084/m9.figshare.11568846.
Rights and permissions
About this article
Cite this article
Aamir, A., Girach, A., Sarrigiannis, P.G. et al. Repetitive Magnetic Stimulation for the Management of Peripheral Neuropathic Pain: A Systematic Review. Adv Ther 37, 998–1012 (2020). https://doi.org/10.1007/s12325-020-01231-2
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12325-020-01231-2