Abstract
Background
To compare the prognostic value of pulse amplitude on intracranial pressure (ICP) monitoring and disproportionately enlarged subarachnoid space hydrocephalus (DESH) on magnetic resonance imaging (MRI) for predicting surgical benefit after shunt placement in idiopathic normal pressure hydrocephalus (iNPH).
Method
Patients with suspected iNPH were prospectively recruited from a single centre. All patients received preoperative MRI and ICP monitoring. Patients were classified as shunt responders if they had an improvement of one point or more on the NPH score at 1 year post-surgery. The sensitivity, specificity, Youden index, and positive and negative predictive values of the two diagnostic methods were calculated.
Results
Sixty-four of 89 patients clinically improved at 1 year post-surgery and were classed as shunt responders. Positive DESH findings had a sensitivity of 79.4 % and specificity of 80.8 % for predicting shunt responders. Fifty-five of 89 patients had positive DESH findings: 50 of these responded to VP shunt, giving a positive and negative predictive value of 90.9 % and 61.8 %, respectively. Fifty-seven of 89 patients had high ICP pulse amplitude. High ICP pulse amplitude had a sensitivity of 84.4 %, specificity of 88 %, positive predictive value of 94.7 % and negative predictive value of 61.8 % for predicting shunt responders.
Conclusions
Both positive DESH findings and high ICP pulse amplitude support the diagnosis of iNPH and provide additional diagnostic value for predicting shunt-responsive patients; however, high ICP amplitude was more accurate than positive DESH findings, although it is an invasive test.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Idiopathic normal pressure hydrocephalus (iNPH) is a neurological degenerative disease that is a common cause of neurological impairment in older people. It manifests as progressive subcortical dementia, gait disorders and bladder or bowel incontinence, and is characterised by enlarged ventricular size in the absence of elevated opening pressure of the cerebrospinal fluid (CSF) measured by lumbar puncture [14]. Surgical diversion of the CSF is the only procedure available to treat the symptoms of iNPH [21], and some patients, especially those in the advanced stages of the disease, experience dementia despite surgical treatment.
There is significant variation in the clinical presentation, severity and progression of iNPH, and it is sometimes complicated to differentiate iNPH from other neurodegenerative disorders, especially subcortical arteriosclerotic encephalopathy and Alzheimer’s disease [4, 11]. As a consequence, diagnosis is often challenging, and identifying patients who could benefit from surgery is sometimes difficult. However, it is important to make an accurate and early diagnosis of iNPH because the symptoms can be improved with surgical treatment, but are less responsive to surgery in the advanced stages of the disease [28].
For more than 40 years, the ventricular shunt, particularly into the peritoneal cavity, has been the surgical treatment of choice for iNPH. However, ventricular shunts have a number of potential complications with serious consequences. Technical advances in the design of the valves have not substantially changed surgical outcomes, and the risks of surgery remain high [3, 21]. There is a need for a tool that will predict the outcome of surgical treatment in patients with significant comorbidities.
Supplemental tests can improve the accuracy of predicting a response to surgical treatment. Nevertheless, there is no expert consensus as to which supplemental test is optimal, and some of these procedures, such as the hydrodynamic test and intracranial pressure (ICP) monitoring, are invasive. The SHINPHONI study [12], a multi-centre prospective study in Japan, found that disproportionately expanded Sylvian fissures alongside with tight high convexity and medial subarachnoid spaces in MRI, also known as disproportionately enlarged subarachnoid space hydrocephalus (DESH), was useful for the diagnosis of iNPH and, therefore, could predict the efficacy of treatment. The Guidelines for Management of Idiopathic Normal Pressure Hydrocephalus [23] published by the Japanese Society of Normal Pressure Hydrocephalus focused on the diagnostic importance of DESH diagnosed from coronal MRI.
Other studies have highlighted the importance of ICP pulse amplitude in the diagnosis of the iNPH [5–9]. For example, Eide [7] reported that the ICP pulse amplitude predicted positive and negative responses to shunting. Despite this, the relative efficacy of and correlation between MRI DESH findings and ICP pulse amplitude is not known. The aim of this study was to compare the efficacy of MRI DESH findings and ICP pulse amplitude at predicting the success of shunt surgery.
Methods
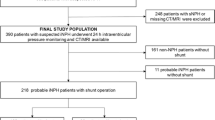
This was a prospective study involving the long-term follow-up of 89 consecutive patients (42 men and 47 women) with possible iNPH treated at University Hospital Germans Trias i Pujol (Barcelona) over a period of 46 months between February 2010 and December 2013. Inclusion criteria were as follows: age between 60 and 85 years, one or more symptoms of the clinical triad (gait disturbance, dementia and urinary incontinence), enlarged cerebral ventricles (Evans index >0.3), presence of B waves in more than 10 % of the ICP monitoring, absence of other diseases that could explain clinical symptoms, no obvious preceding diseases that may cause ventricular dilatation, and written informed consent given by the patient or patient’s representatives. Local institutional review board (IRB) approved the study.
ICP was monitored through a Codman® Microsensor™ ICP Transducer (Johnson & Johnson Medical, Raynham, MA, USA). The ICP monitoring was done from the evening of day 1 until the morning of day 2. For each patient we used the overnight ICP recording from 11 p.m. to 7 a.m., when the patient was supine in bed. Complications during ICP sensor implantation were registered. Both static and pulsatile ICP were analysed. ICP pulsatility was determined as an average of all overnight waveforms. According to previous studies [7, 24], ICP pulse amplitude >4 mmHg on ICP monitoring was considered high, and ICP pulse amplitude ≤4 mmHg was considered low. Clinical evaluation of gait, cognition, and incontinence was done pre- and 1 year post-surgery using the Normal Pressure Hydrocephalus score [25] (Table 1). Surgery consists of the implantation of a ventriculo-peritonial shunt. We placed a Codman Hakim programmable valve (Codman & Shurtleff; Medos, Le Locle, Switzerland). The opening pressure settings were selected on the basis of the results of the mean ICP (averaged overall ICP monitoring). The median opening pressure at shunt 11 cm H20 (range, 3-20 cm H20). Shunt responders were defined as patients with an improvement of one point or more on the NPH score at 1 year post-surgery.
All patients received a baseline magnetic resonance imaging (MRI) examination performed using an MX8000 IDT scanner (Philips Healthcare, Best, The Netherlands). MRI studies were carried out between 2 to 45 days before surgery. DESH positive was defined by disproportionate enlargement of the inferior subarachnoid spaces with tight high-convexity subarachnoid spaces in a coronal spin-echo T1-weighted image perpendicular to the anterior commissure. Two independent observers (one neurosurgeon (RGA) trained in assessing MRI findings of iNPH, and one experienced neuroradiologist (SD)) blinded to NPH score and ICP monitoring, established the presence of positive DESH findings.
Statistical analysis was carried out using SPSS software (SPSS for Mac, version 22.0; SPSS, Chicago, IL, USA). Numeric variables are expressed as median and interquartile range or mean and standard deviation, and categorical variables are expressed as number (percentage). A chi-squared test or Student’s t-test was used to compare the diagnostic test results (low vs high ICP pulse amplitude, and DESH positive vs DESH negative) between responders and non-responders. A p value less than 0.05 were considered statistically significant. We evaluated the inter-reader agreements between the two reviewers by using Cohen’s kappa coefficient (κ) statistical analysis.
Sensitivity, specificity, the Youden index, positive predictive values and negative predictive values, and the likelihood ratio of a positive test and negative test were determined for both diagnostic methods (ICP pulse amplitude and DESH). A positive likelihood ratio >10 and a negative likelihood ratio <0.1 was taken as reflecting a very useful test. Table 2 shows the interpretation of results on the basis of likelihood ratios. Cohen’s kappa coefficient (κ) was used also to determine the consistency of agreement between two diagnostic tests in predicting surgical results (shunt responder and shunt non-responder). The level of consistency was classified as very mild (κ, 0–0.2), mild (κ, 0.2–0.4), moderate (κ, 0.4–0.6), good (κ, 0.6–0.8), or almost perfect (κ, 0.8–1.0). All procedures were performed as part of routine clinical care, and data were anonymised.
Results
There were 118 consecutive patients treated for possible iNPH in the study period. Twenty-nine (24.6 %) were excluded from the study because they did not meet the inclusion criteria: age >85 years, n = 5; age <60 years, n = 1; preceding diseases possibly causing ventricular dilatation, n = 23 (n = 16 previous subarachnoid haemorrhage, n = 5 previous tumour, and n = 2 other). Thus, the final series consisted of 89 participants (42 men and 47 women) with a mean ± standard deviation age of 72.5 ± 6.6 years. Table 3 summarises the demographic data and baseline clinical features of these patients. ICP catheter complications occurred in one patient (1.1 %). Wound infection occurred in one patient without clinical consequences.
One year after shunting, 64 patients (71.9 %) showed clinical improvement according to the NPH score. Gait improved in 62 (96.6 %) patients, sphincter control improved in 50 (78.7 %) and dementia improved in 48 (75.3 %). These 64 patients were classified as shunt responders, and the remaining 25 patients (28.1 %) were classified as shunt non-responders. Both groups have comparable CRF.
Fifty-six (62.9 %) patients were classified as DESH positive, and 33 (37.1 %) were classified as DESH negative. Both groups had comparable cardiovascular risk factors. There was a statistically significant difference between the proportion of DESH-positive patients among shunt responders (51 of 64, 79.7 %) and non-responders (5 of 25, 20.0 %; p < 0.001, chi-squared test) (Table 4). Similarly, there was a statistically significant difference between the proportion of patients with high ICP pulse amplitude (>4 mmHg) among shunt responders (54 of 64, 84.4 %) and non-responders (3 of 25, 12 %; p < 0.001, chi-squared test).
DESH had a sensitivity of 79.7 %, specificity of 80.0 %, Youden index of 0.60, positive predictive value of 91.07 % and negative predictive value of 60.6 % for discriminating shunt responders from shunt non-responders. ICP pulse amplitude had a sensitivity of 84.4 %, specificity of 88.0 %, Youden index of 0.72, positive predictive value of 94.7 % and negative predictive value of 68.8 %. Table 5 illustrates overall response accuracy of the two supplementary diagnostic tests. DESH had a positive likelihood ratio of 3.98 and a negative likelihood ratio of 0.25, and ICP pulse amplitude had a positive likelihood ratio of 7.0 and negative likelihood ratio of 0.18. Consistency of agreement of two supplementary diagnostic tests was mild (κ, 0.20), and inter-reader agreement between the two reviewers in the evaluation of the presence of DESH was good (κ, 0.64-0.85).
Discussion
Despite improving knowledge regarding iNPH, surgical outcomes have not significantly improved, and the rate of shunt complications remains high [3, 21]. Expert clinical evaluations performed in specialised centres can achieve up to 90 % accuracy in identifying shunt-responsive patients with iNPH [4]; however, diagnosis of iNPH in general practice is much less successful. Sensitivity and specificity of the classic triad in a reported series is 54 % and 84 % respectively [28].
Currently, there are no standard diagnostic criteria for iNPH [2, 4, 30]. Clinical practice guidelines recommend that iNPH diagnosis be based on evidence from the clinical history, the physical examination and image studies [20]. Some additional tests may help iNPH diagnosis, including neuropsychological tests, urodynamic studies, gait analysis and functional imaging evaluations, among others [1, 10, 19]. These tests may increase the diagnostic accuracy in some cases when the symptoms are subtle, although some, such as hydrodynamic tests and ICP monitoring, are invasive procedures. The sensitivity of iNPH diagnosis is low [19], due to the variability that exists in the clinical onset and the progression of the disease. Specificity is also low due to other common disorders, such as cerebrovascular diseases, Alzheimer’s disease, Parkinson’s disease and Lewy body dementia [11, 15, 16], with symptoms very similar to those of iNPH, specifically, spinal degenerative disorders and urological problems. It is important to make an accurate and early diagnosis of iNPH because the symptoms can be improved with surgical treatment. Some authors have reported that symptoms such as ataxia, dementia and incontinence in the advanced stages of the disease tend to respond worse to the treatment than mild symptoms [28].
Many authors [4, 18, 19, 21, 26, 29, 30] have highlighted the need for a diagnostic tool that will help to make a prediction of the outcome after surgical treatment of patients with significant comorbidities. The present study compared the results of two complementary diagnostic tools, one invasive (ICP pulse amplitude) and one non-invasive (MRI), between iNPH patients who responded to CSF shunt surgery and those who did not.
Recently, a DESH finding has been validated as a useful feature in the diagnosis of iNPH, and has been included in the clinical guidelines of the Japanese Society of Normal Pressure Hydrocephalus [23]. This characteristic, which was reported by Kitagaki et al. [17], might be a non-invasive biomarker for predicting shunt surgery results.
ICP pulsatility was correlated with clinical improvement after shunt surgery [5–9], and may also be a biomarker for shunt surgery results, but this test is invasive and can cause complications [8]. In our study, the rate of complications related to the implantation and monitoring of ICP was low. Although some studies reported potentially serious complications, such as bleeding (1.1 %), epidural haematoma (0.47 %), contusion (0.47 %) and intraparenchymal haematoma (0.15 %) [2], the majority reported few complications that are generally mild in nature and include technical complications such as a dislocation of the fixation screw, disconnection of the transducer, breakage of the fibreoptic cable, probe defects and monitor-related infections [9].
In this study, we demonstrate that a high ICP pulse amplitude (>4 mmHg) determined by ICP monitoring was more sensitive (84.4 % vs 79.7 %) and more specific (88.0 % vs 80.0 %) than a positive DESH finding for predicting shunt response in symptomatic patients. Moreover Youden index values were higher for high ICP amplitude than for positive DESH findings. On the basis that the Youden index captures the performance of a diagnostic test, we suggest that ICP amplitude may be more useful than DESH findings. Nevertheless, the positive predictive values indicated that both diagnostic tests were highly accurate at predicting shunt response (91.1 % and 94.7 % for high ICP amplitude and positive DESH, respectively). This means that improvement after surgery can be anticipated in approximately nine of ten symptomatic patients with positive DESH findings or high ICP amplitude.
Eide and Brean [8] reported comparable findings, with clinical improvement in 103 (79 %) of the 130 surgically treated patients, and a sensitivity of 98 %, specificity of 70 % and a PPV of 93 % for mean ICP amplitude >4 mmHg. DESH findings in a previous report also agree with our results, with a high positive predictive value (80 %) [12], indicating that MRI-based diagnosis is useful for diagnosis of iNPH. Accordingly, we theorise that the two diagnostic methods can be considered with equal weighting when a test is positive in symptomatic patients. However, negative predictive values were low, 68.8 % and 60.6 %, and neither test achieved good accuracy. Therefore, a negative result on the two tests may not exclude the possibility that the patient will improve with surgery. These rates differed somewhat to those made by Eide and Brean [8], who reported a high NPV (91 %) for high ICP pulse amplitude in 130 surgically treated patients. The positive and negative predictive values of an external lumbar drainage test (draining 10 ml of CSF per hour for a period of 72 h) were 87 % and 36 %, respectively [19, 20, 30], and agree with our results reached with both diagnostic tests (high ICP amplitude and positive DESH). However, the lumbar drainage test has an increased risk of complications in comparison to other tests, such as overdrainage and bacterial meningitis. Complications with this test occurred in approximately 5 % of cases [20, 30]. Another supplemental test, cerebrospinal pulse pressure amplitude determined during a lumbar infusion test was reported to achieve a sensitivity of 88 % for predicting shunt response with a specificity of 60 % and a positive predictive value and negative predictive value of 89 % and 60 %, respectively [8]. These values are lower than those found for high ICP pulse amplitude in this study. This discrepancy may be because the ICP pulse amplitude was evaluated at different anatomical sites. One may speculate that this variation is due to a difference in the compliance in the different compartments, as reported by Eide and Brean [8]; however, this assumption remains to be confirmed.
It has been postulated that positive DESH findings may be caused by defective CSF absorption as a result of suprasylvian subarachnoidal block. Patients with iNPH have a greater volume of CSF within the ventricular system than patients with Alzheimer’s disease or vascular dementia, and have narrower subarachnoid spaces of the upper and medial convexity [13, 17, 22]. We hypothesise that positive DESH findings in MRI as a result of blocked suprasylvian CSF subarachnoidal flow may be an indirect measure of a decrease in brain compliance, i.e. pressure-volume reserve capacity, and may be inversely correlated with ICP pulse amplitude. Although not documented in the literature, compartmentalisation of pulse amplitude is possible. The blockage of the suprasylvian CSF subarachnoid space may produce a compartmentalised gradient of pressure in this space. That issue may alter the compensatory reserve and the CSF pressure reactivity, subsequently impairing the brain compliance. In this situation the brain elastance behaves in a linear manner and the variations of intracranial volume correlate well with changes in ICP wave amplitude. Saehle and Eide [27] reported an association between ventricular volume measures and pulsatile and static ICP scores in non-communicating hydrocephalus. However, there are no studies that support this hypothesis in communicating hydrocephalus, and we found that the agreement between DESH findings and high ICP amplitude was very mild (κ, <0.2). It is likely that the two tests measure different but related aspects of iNPH and provide complementary information, but are not directly associated.
Finally, our study has several limitations. First, this was a single-centre study, and the patient sample was too small to draw any definite conclusions. Second, the classification of DESH from MRI was subjective, although having two assessors minimised the effects of this on results and, third, the supposition (association between ICP pulse and DESH findings) was very simplistic in a disease whose pathophysiology is not completely understood.
Conclusions
Despite the fact that the agreement between DESH findings and ICP amplitude was mild, and despite the superiority of ICP pulse amplitude over DESH findings for predicting shunt effectiveness, given the non-invasive nature and high sensitivity and specificity of DESH findings, DESH may be useful as a first test for identifying iNPH patients who will respond to a shunt. However, when there are no identifying DESH findings, an invasive test such as an ICP monitoring or a hydrodynamic test is likely to provide valuable additional information, and seems to be indicated regarding the effectiveness of a shunt.
References
Alperin N, Vikingstad EM, Gomez-Anson B, Levin DN (1996) Hemodynamically independent analysis of cerebrospinal fluid and brain motion observed with dynamic phase contrast MRI. Magn Reson Med 35:741–754
Bech-Azeddine R, Waldemar G, Knudsen GM, Høgh P, Bruhn P, Wildschiødtz G, Gjerris F, Paulson OB, Juhler M (2001) Idiopathic normal-pressure hydrocephalus: evaluation and findings in a multidisciplinary memory clinic. Eur J Neurol 8:601–611
Black PM (1980) Idiopathic normal-pressure hydrocephalus. Results of shunting in 62 patients. J Neurosurg 52:371–377
Boon AJ, Tans JT, Delwel EJ, Egeler-Peerdeman SM, Hanlo PW, Wurzer HA, Hermans J (1999) Dutch normal-pressure hydrocephalus study: the role of cerebrovascular disease. J Neurosurg 90:221–226
Czosnyka M, Czosnyka Z, Keong N, Lavinio A, Smielewski P, Momjian S, Schmidt EA, Petrella G, Owler B, Pickard JD (2007) Pulse pressure waveform in hydrocephalus: what it is and what it isn’t. Neurosurg Focus 22:E2
Di Rocco C, Maira G, Rossi GF, Vignati A (1976) Cerebrospinal fluid pressure studies in normal pressure hydrocephalus and cerebral atrophy. Eur Neurol 14:119–128
Eide PK (2006) Intracranial pressure parameters in idiopathic normal pressure hydrocephalus patients treated with ventriculo-peritoneal shunts. Acta Neurochir (Wein) 148:21–29, discussion 29
Eide PK, Brean A (2010) Cerebrospinal fluid pulse pressure amplitude during lumbar infusion in idiopathic normal pressure hydrocephalus can predict response to shunting. Cerebrospinal Fluid Res 7:5
Eide PK, Sorteberg W (2010) Diagnostic intracranial pressure monitoring and surgical management in idiopathic normal pressure hydrocephalus: a 6-year review of 214 patients. Neurosurgery 66:80–91
Enzmann DR, Pelc NJ (1993) Cerebrospinal fluid flow measured by phase-contrast cine MR. AJNR Am J Neuroradiol 14:1301–1307, discussion 1309–10
Golomb J, Wisoff J, Miller DC, Boksay I, Kluger A, Weiner H, Salton J, Graves W (2000) Alzheimer’s disease comorbidity in normal pressure hydrocephalus: prevalence and shunt response. J Neurol Neurosurg Psychiatry 68:778–781
Hashimoto M, Ishikawa M, Mori E, Kuwana N (2010) Study of INPH on neurological improvement (SINPHONI) Diagnosis of idiopathic normal pressure hydrocephalus is supported by MRI-based scheme: a prospective cohort study. Cerebrospinal Fluid Res 7:18
Holodny AI, George AE, de Leon MJ, Golomb J, Kalnin AJ, Cooper PR (1998) Focal dilation and paradoxical collapse of cortical fissures and sulci in patients with normal-pressure hydrocephalus. J Neurosurg 89:742–747
Höglund M, Tisell M, Wikkelsø C (2001) Incidence of surgery for hydrocephalus in adults surveyed: same number afflicted by hydrocephalus as by multiple sclerosis]. Lakartidningen 98:1681–1685
Kiefer M, Unterberg A (2012) The differential diagnosis and treatment of normal-pressure hydrocephalus. Dtsch Arztebl Int 109:15–25, quiz 26
Kim MJ, Seo SW, Lee KM, Kim ST, Lee JI, Nam DH, Na DL (2011) Differential diagnosis of idiopathic normal pressure hydrocephalus from other dementias using diffusion tensor imaging. AJNR Am J Neuroradiol 32:1496–1503
Kitagaki H, Mori E, Ishii K, Yamaji S, Hirono N, Imamura T (1998) CSF spaces in idiopathic normal pressure hydrocephalus: morphology and volumetry. AJNR Am J Neuroradiol 19:1277–1284
Klassen BT, Ahlskog JE (2011) Normal pressure hydrocephalus: how often does the diagnosis hold water? Neurology 77:1119–1125
Marmarou A, Bergsneider M, Klinge P, Relkin N, Black PM (2005) The value of supplemental prognostic tests for the preoperative assessment of idiopathic normal-pressure hydrocephalus. Neurosurgery 57:S17–S28, discussion ii–v
Marmarou A, Bergsneider M, Relkin N, Klinge P, Black PM (2005) Development of guidelines for idiopathic normal-pressure hydrocephalus: introduction. Neurosurgery 57:S1–S3, discussion ii–v
Marmarou A, Young HF, Aygok GA, Sawauchi S, Tsuji O, Yamamoto T, Dunbar J (2005) Diagnosis and management of idiopathic normal-pressure hydrocephalus: a prospective study in 151 patients. J Neurosurg 102:987–997
Moore DW, Kovanlikaya I, Heier LA, Raj A, Huang C, Chu K-W, Relkin NR (2012) A pilot study of quantitative MRI measurements of ventricular volume and cortical atrophy for the differential diagnosis of normal pressure hydrocephalus. Neurol Res Int 2012:718150–718156
Mori E, Ishikawa M, Kato T, Kazui H, Miyake H, Miyajima M, Nakajima M, Hashimoto M, Kuriyama N, Tokuda T, Ishii K, Kaijima M (2012) Guidelines for management of idiopathic normal pressure hydrocephalus: second edition. Neurol Med Chir (Tokyo) 52:775–809
Park E-H, Eide PK, Zurakowski D, Madsen JR (2012) Impaired pulsation absorber mechanism in idiopathic normal pressure hydrocephalus: laboratory investigation. J Neurosurg 117:1189–1196
Sahuquillo J, Rubio E, Codina A, Molins A, Guitart JM, Poca MA, Chasampi A (1991) Reappraisal of the intracranial pressure and cerebrospinal fluid dynamics in patients with the so-called “normal pressure hydrocephalus” syndrome. Acta Neurochir (Wein) 112:50–61
Sasaki M, Honda S, Yuasa T, Iwamura A, Shibata E, Ohba H (2008) Narrow CSF space at high convexity and high midline areas in idiopathic normal pressure hydrocephalus detected by axial and coronal MRI. Neuroradiology 50:117–122
Sæhle T, Eide PK (2015) Association between ventricular volume measures and pulsatile and static intracranial pressure scores in non-communicating hydrocephalus. J Neurol Sci 350:33–39
Thomsen AM, Børgesen SE, Bruhn P, Gjerris F (1986) Prognosis of dementia in normal-pressure hydrocephalus after a shunt operation. Ann Neurol 20:304–310
Vanneste J, Augustijn P, Tan WF, Dirven C (1993) Shunting normal pressure hydrocephalus: the predictive value of combined clinical and CT data. J Neurol Neurosurg Psychiatry 56:251–256
Walchenbach R, Geiger E, Thomeer RTWM, Vanneste JAL (2002) The value of temporary external lumbar CSF drainage in predicting the outcome of shunting on normal pressure hydrocephalus. J Neurol Neurosurg Psychiatry 72:503–506
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
No funding was received for this research.
Conflict of interest
All authors certify that they have no affiliations with or involvement in any organisation or entity with any financial interest (such as honoraria; educational grants; participation in speakers’ bureaus; membership, employment, consultancies, stock ownership, or other equity interest; and expert testimony or patent-licensing arrangements), or non-financial interest (such as personal or professional relationships, affiliations, knowledge or beliefs) in the subject matter or materials discussed in this manuscript.
Ethical approval
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent
Informed consent was obtained from all individual participants included in the study.
Additional information
Comment
Despite technical and knowledge improving, the surgical outcomes and the clinical indication to shunting for iNPH have not improved in the last decades. After the well-known multi-center prospective study SHINPHONI of 2010, the neurosurgical community is aware that disproportionately expanded Sylvian fissures alongside with tight high convexity and medial subarachnoid spaces in MRI - also known as disproportionately enlarged subarachnoid space hydrocephalus (DESH) -is very useful for the diagnosis of iNPH, and therefore could predict the efficacy of treatment.
In this manuscript, the Authors report a prospective study involving long-term follow-up of 89 patients with iNPH over a mean period of 46 months in order to compare the prognostic value of DESH and pulse amplitude ICP. One year after shunting 71,9 % of patients had a clinical improvement and could be classified as shunt responders. 62,9 were DESH positive. DESH had a sensitivity and specifity of around 80 %, with a positive predict value of 91 % and negative predictive value of 60 % for discriminating shunt responders. If associated with ICP amplitude the accuracy of predicting shunt responses reaches globally the > 90 %.
A very intriguing issue is the theory, that positive DESH findings may be caused by defective CSF absorption as a result of suprasylvian subarachnoidal block. This question is worthy to be clarified by appropriate research.
The topic is of neurosurgical relevance, and the study well conducted. Overall, the data are convincing that DESH may be useful as a first test for identifying iNPH patients who will respond to a shunt.
Alex Alfieri
Francesco Ferri
Neuruppin, Germany
Rights and permissions
About this article
Cite this article
Garcia-Armengol, R., Domenech, S., Botella-Campos, C. et al. Comparison of elevated intracranial pressure pulse amplitude and disproportionately enlarged subarachnoid space (DESH) for prediction of surgical results in suspected idiopathic normal pressure hydrocephalus. Acta Neurochir 158, 2207–2213 (2016). https://doi.org/10.1007/s00701-016-2858-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2858-5