Abstract
Introduction
The aim of this study was to determine the performance of axial and coronal magnetic resonance imaging (MRI) in detecting the narrowing of the cerebrospinal fluid (CSF) space at the high convexity and high midline areas, which is speculated to be one of the clinical characteristics of idiopathic normal pressure hydrocephalus (iNPH).
Methods
We retrospectively examined axial and coronal T1-weighted images of 14 iNPH patients and 12 age-matched controls. The narrowness of the CSF space at the high convexity/midline was blindly evaluated by five raters using a continuous confidence rating scale for receiver operating characteristic (ROC) analysis.
Results
Axial and coronal imaging accurately determined the presence of the narrow cisterns/sulci at the high convexity/midline and was capable of predicting probable/definite iNPH with a high degree of accuracy. there were also no significant differences in the detection of this finding between the axial and coronal images.
Conclusion
Both axial and coronal T1-weighted MRI can detect the narrow CSF space at the high convexity/midline accurately and may therefore facilitate clinicians in choosing a management strategy for iNPH patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Idiopathic normal pressure hydrocephalus (iNPH) is a relatively rare disorder that occurs in the elderly segment of the population (older than 60 years). It is considered to be of cryptogenic origin and causes dementia, gait disturbances, and incontinence. A shunt operation can successfully treat this condition [1]. While patients with iNPH show marked ventricular dilatation, narrowing of the cerebrospinal fluid (CSF) space at the high convexity and high midline areas (conflicting with a dilated sylvian fissure and basal cistern) has been reported to be one of the characteristic imaging findings in iNPH [2]. This condition has also been included in the clinical guidelines provided by the Japanese Society of Normal Pressure Hydrocephalus as a non-mandatory criterion [3]. The narrow CSF space at the high convexity/midline has generally been evaluated on coronal images because these enable comparison of the cisterns/sulci in this area with the sylvian fissure and the basal cistern on the same section. However, the diagnostic performance of this images, including sensitivity and specificity, has not been fully demonstrated. In addition, the detectability of this feature on routine axial images has not been assessed, although it would be beneficial in clinical practice if routine magnetic resonance imaging (MRI) in which only axial images are usually obtained were able to detect iNPH.
The aim of this study was to determine whether axial and coronal MRI is able to detect the narrow CSF space at the high convexity/midline in iNPH patients. We also used a receiver operating characteristic (ROC) analysis to evaluate whether it is possible to distinguish iNPH patients from healthy individuals on the basis of this finding.
Materials and methods
We examined 14 consecutive iNPH patients (eight men and six women; age range 61–91 years; mean age 77.6 years). In accordance with the Clinical Guidelines for Idiopathic Normal Pressure Hydrocephalus provided by the Japanese Society for Normal Pressure Hydrocephalus (Table 1) [3], the patients were clinically diagnosed with either probable iNPH (n = 9, five men and four women; age range 69–91 years; mean age 78.2 years), who effectively responded with a CSF tap test, or definite iNPH (n = 5, three men and two women; age range 61–82 years; mean age 75.6 years), who were successfully treated by shunt surgery. All of the patients fulfilled the mandatory MRI criterion for possible iNPH in the guidelines: the Evans’ index [4], defined as the maximum distance between the lateral margins of both the anterior horns divided by the maximum width of the inner table of the cranium, was over 30%. We also examined 12 age-matched subjects without symptoms suggestive of iNPH and without other neurological symptoms (six men and six women; age range 63–91 years; mean age 78.4 years). All examinations were carried out after obtaining permission from the institutional review board and approval and informed consent from all subjects.
Axial and coronal spin-echo T1-weighted images were obtained parallel and perpendicular to the anterior commissure–posterior commissure line using a 1.5-T superconductive MRI unit (Magnetom Vision, Siemens, Erlangen) for assessment of the narrow CSF space at the high convexity/midline based on prior use of a T1-weighted and not T2-weighted sequence for this purpose in a previous study [2]. We used the following scanning parameters: repetition time (ms)/echo time (ms), 550/12; matrix size, 256 × 187; field of view, 230 mm; slice thickness, 5 mm; number of slices, 20. We also obtained axial fast spin-echo T2-weighted (repetition time (ms)/effective echo time (ms), 3000/100) and fluid-attenuated inversion recovery images (repetition time (ms)/inversion time (ms)/effective echo time (ms), 10000/2500/140) in order to exclude other illnesses.
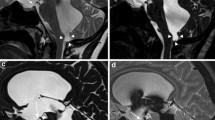
The presence or absence of a narrow CSF space at the high convexity/midline was established by a consensus between two senior neuroradiologists (MS, SH) who are familiar with the MRI findings of iNPH, and the results (positive for 12 of the 14 iNPH patients and negative for two iNPH patients, namely a 75-year-old man with definite iNPH and an 80-year-old woman with probable iNPH, and for all the controls) were used as the gold standard for the analysis. After obtaining guidance regarding the MRI findings of iNPH, two radiologists, one neurologist and two residents, all of whom were unaware of the narrowing of the CSF space at the high convexity/midline in iNPH, visually evaluated the confidence level of the presence of this finding on the axial and coronal images of the patients and controls. For image interpretation, only the two uppermost contiguous axial images through the high convexity/midline and the two contiguous coronal images through the foramen of Monro and the body of the lateral ventricle were provided on a liquid crystal display monitor in a randomized fashion under anonymized conditions by using a DICOM viewer (ExaVision Lite; Ziosoft, Tokyo) (Fig. 1). The observers used a continuous confidence rating scale comprising a line-marking method to rate their confidence levels. The experiments were performed three times at 2-week intervals using differently randomized image data sets. We also calculated the Evans’ index on the same section using a mouse-driven cursor on the same DICOM viewer in order to determine the presence of the bias caused by the difference in the ventricular size between the two groups during the interpretation using coronal images.
Axial and coronal images of idiopathic normal pressure hydrocephalus (iNPH) patients and controls. a–d Axial T1-weighted images, e–h coronal T1-weighted images. a, e An 81-year-old woman with probable iNPH (Evans’ index 0.36), b, f an 81-year-old man with definite iNPH (Evans’ index, 0.31), c, g an 86-year-old man from the control group (Evans’ index 0.31), d, h a 76-year-old man from the control group (Evans’ index 0.28). On axial and coronal images, narrowing of the cerebrospinal fluid (CSF) space at the high convexity and midline areas (arrows) is disproportional to the dilatation of the sylvian fissure (arrowheads); this is evident in iNPH patients when they are compared to the controls
The likelihood of detecting the narrow CSF space at the high convexity/midline and probable/definite iNPH on the axial and coronal images was examined by a ROC analysis using the software package LABROC designed by Metz et al. [5]. In order to evaluate observer performance in detecting the findings and diagnosing iNPH, we compared an area under the ROC curve (Az) between the axial images and coronal images by a Wilcoxon matched-pairs signed-ranks test. The sensitivity and specificity of detecting the finding on axial and coronal images by each rater was also calculated with a cutoff value of 0.50 on the continuous confidence rating scale. Intrarater and interrater agreements were evaluated using an intraclass correlation coefficient, and the difference in Evans’ index between the two groups was examined using a two-tailed t test. An alpha level of 0.05 used.
Results
The Az values of the five raters for detecting the narrow CSF space at the high convexity/midline ranged from 0.96 to 0.99 (mean 0.98) on the axial images and from 0.92 to 0.98 (mean 0.96) on the coronal images; there was no significant difference between these values (Table 2; Fig. 2a). The Az values for predicting probable/definite iNPH ranged from 0.86 to 0.90 (mean 0.89) on the axial images and from 0.85 to 0.98 (mean 0.90) on the coronal images; there was no statistically significant difference between these values (Table 2; Fig. 2b).
Receiver operating characteristic (ROC) analysis of the visual assessment of the narrow CSF space at the high convexity/midline in iNPH a ROC curves for detecting narrow CSF space at the high convexity/midline, b ROC curves for diagnosing probable/definite iNPH. Axial as well as coronal images can accurately detect the presence of the narrow CSF space at the high convexity/midline (a); they also help to distinguish iNPH patients from controls. High Az values indicate high sensitivity and specificity (b)
At a cutoff level of 0.50 of the continuous confidence rating scale, the overall sensitivity and specificity of the detection of the narrow CSF space at the high convexity/midline were 0.80 and 0.97, respectively, on the axial images and 0.87 and 0.93, respectively, on the coronal images; the sensitivity and specificity values for detecting iNPH were 0.71 and 0.97, respectively, on the axial images and 0.74 and 0.92, respectively, on the coronal images (Table 2).
In terms of the intrarater and interrater agreements, the intraclass correlation coefficients between the raters in every combination of two of the five raters ranged from 0.58 to 0.90 (mean 0.80) on the axial images and from 0.68 to 0.89 (mean 0.80) on the coronal images, while those between sessions within each rater ranged from 0.82 to 0.98 (mean 0.87).
Evans’ indices of the iNPH patients and of the controls ranged from 0.30 to 0.38 (mean ± standard deviation, 0.34 ± 0.03) and from 0.24 to 0.33 (0.28 ± 0.03), respectively; the difference between the two groups was statistically significant (two-tailed t test, P = 0.001).
Discussion
Shunt surgery for possible iNPH is mainly indicated in patients who show an improvement in symptoms after a CSF tap test (drainage of 30–50 ml of CSF) or on continuous CSF drainage test [3, 6, 7]. Neuroimaging techniques are usually used to exclude other disorders, to consider the possibility of iNPH and to provide clinical evidence for confirming the diagnosis suggested by the CSF tap test or CSF drainage test. Among the various criteria, ventricular dilatation with an Evans’ index of 0.3 or more based on computed tomography (CT) or MR images appears to be essential but not specific to the diagnosis of iNPH [1, 3, 8]. Several imaging findings have been reported to be characteristic of iNPH, including diffuse white matter lesions on MR images, increased velocity of CSF flow at the aqueduct on MR images, backflow of the iodine contrast agents or radioisotopes into the lateral ventricle on cisternography and hypoperfusion of the cerebral white matter on positron emission tomography or single-photon emission CT images [9–12]. However, the diagnostic significance of these findings is still considered to be controversial [13–15]. The narrowing of the CSF space at the high convexity/midline, which was documented by Kitagaki et al. [2], is expected to be a noninvasive and accurate biomarker for diagnosing iNPH and predicting the outcome after shunt surgery [3]. However, its efficacy has not been fully validated.
In this study, we successfully confirmed the accuracy of the visual assessment of the narrowing of the CSF space at the high convexity/midline and demonstrated that these findings can help differentiate iNPH patients from healthy subjects with a high degree of sensitivity and specificity, thereby supporting previous results [2]. We also observed that the diagnostic performance of axial images is almost the same as that of coronal images. To the best of our knowledge, this is the first report that determines the validity of the visual interpretation and the utility of axial images.
We used a visual interpretation method to assess the narrowing of the CSF space at the high convexity/midline. This method is qualitative and may be less accurate than quantitative methods such as volumetry [3]. There should be cases that show equivocal findings in terms of the presence or absence of the findings, particularly in patients with no obvious brain atrophy. However, our results showed that even for raters who are not familiar with the MRI findings in iNPH patients, simple visual evaluation has high sensitivity, specificity and intrarater and interrater agreement in the detection of the narrowing of the CSF space at the high convexity/midline in these patients. This result suggests that visual assessment is both an easy-to-use and effective method for identifying possible iNPH cases in clinical practice.
It has not yet been determined which plane is the most suitable for assessing the narrowing of the CSF space at the high convexity/midline. Coronal images appear to be effective in evaluating the discrepancy between the narrowing of the CSF space at the high convexity/midline and the dilatation of the lateral ventricles, sylvian fissure, and basal cistern on the same section [3]. The significantly larger Evans’ indices of iNPH patients in this study may help in the interpretation of the coronal images. Sagittal images have also been proposed for the assessing the narrowing of the CSF space at the high midline [16]. However, we found that axial images through the high convexity can be used to accurately detect the presence of a narrowed CSF space and can help differentiate iNPH patients from controls, presumably because a substantially wide CSF space exists in the high convexity/midline of healthy subjects aged over 60 years. The use of axial images that can be routinely obtained is considered to be a reliable and more practical method for the assessing such patients as compared to the use of coronal or sagittal images.
In this study, we compared iNPH patients with age-matched healthy subjects but not with patients having disorders that should be differentiated from iNPH, such as Alzheimer’s disease. The narrowing of the CSF space at the high convexity/midline area was not observed in previous studies of patients with Alzheimer’s disease, vascular dementia and progressive supranuclear palsy [2, 16]. Thus, the visual assessment method that we used may possibly be able to differentiate iNPH from other related disorders, although this assessment was beyond the scope of our investigation. Another limitation of this study is that the patient cohort comprised a small number of patients, particularly those with definite iNPH, that varied widely in age, which may have affected the confidence level of the results. We assume that the finding is substantially sensitive and specific for iNPH; however, it has still not been fully determined whether the finding is found in almost all patients with iNPH or whether the same finding is occasionally observed in healthy elderly individuals and in patients with other disorders without symptoms similar to those of iNPH. Further investigation using a larger sample size comprising persons with definite iNPH is needed to confirm the sensitivity and specificity of this finding with greater accuracy.
The pathogenesis of iNPH as well as the importance of the narrow CSF space at the high convexity/midline is still unknown. Impaired CSF circulation and absorption, decreased brain tissue compliance due to age-related or cerebrovascular changes and ventriculomegaly due to brain atrophy and other causes are considered to be the principal cross-correlated factors leading to iNPH. However the relation of factors to iNPH are still controversial [1, 8, 17]. It is also unknown whether the narrow CSF space at the high convexity/midline is a cause or result of the pathophysiological mechanisms of iNPH. We speculate that the narrowing of the CSF space at the high convexity/midline can be a secondary condition caused by dilatation of the ventricle and the sylvian fissure as a result of impaired CSF circulation because this finding is not always observed in every iNPH patient, and it can be partially resolved after shunt surgery [2]. A more precise evaluation of this finding before and after the CSF tap test or shunt surgery is needed to elucidate the mechanisms and the clinical importance of the narrow CSF space at the high convexity/midline.
In conclusion, the narrow CSF space at the high convexity/midline is a clinical finding that is characteristic of iNPH patients and can be easily identified with high sensitivity, specificity, and intrarater and interrater agreement on not only coronal but also axial images. This finding may help in differentiating iNPH patients from healthy elderly patients and those with other illnesses; moreover, it will aid in determining candidates for the CSF tap test and, presumably, for the shunt operation.
References
Relkin N, Marmarou A, Klinge P, Bergsneider M, Black PM (2005) Diagnosing idiopathic normal-pressure hydrocephalus. Neurosurgery 57[Suppl]:4–16
Kitagaki H, Mori E, Ishii K, Yamaji S, Hirono N, Imamura T (1998) CSF spaces in idiopathic normal pressure hydrocephalus: morphology and volumetry. Am J Neuroradiol 19:1277–1284
Ishikawa M (2004) Clinical guidelines for idiopathic normal pressure hydrocephalus. Neurol Med Chir 44:222–223
Evans WA (1942) An encephalographic ratio for estimating ventricular and cerebral atrophy. Arch Neurol Psychiatr 47:931–937
Metz CE, Herman BA, Shen JH (1998) Maximum-likelihood estimation of receiver operating characteristic (ROC) curves from continuously-distributed data. Stat Med 17:1033–1053
Walchenbach R, Geiger E, Thomeer RT, Vanneste JA (2002) The value of temporary external CSF drainage in predicting the outcome of shunting on normal pressure hydrocephalus. J Neurol Neurosurg Psychiatr 72:503–506
Kahlon B, Sundbarg G, Rehncrona S (2002) Comparison between the lumbar infusion and CSF tap tests to predict outcome after shunt surgery in suspected normal pressure hydrocephalus. J Neurol Neurosurg Psychiatr 73:721–726
Vassilouthis J (1984) The syndrome of normal-pressure hydrocephalus. J Neurosurg 61:501–509
Krauss JK, Regel JP, Vach W, Orszaph M, Jungling FD, Bohus M, Droste DW (1997) White matter lesions in patients with idiopathic normal pressure hydrocephalus and in an age-matched control group: a comparative study. Neurosurgery 40:491–495
Jack CR, Mokri B, Laws ER, Houser OW, Baker HL, Petersen RC (1987) MR findings in normal-pressure hydrocephalus: significance and comparison with other forms of dementia. J Comput Assist Tomogr 11:923–931
Luetmer PH, Huston J, Friedman JA, Dixon GR, Petersen RC, Jack CR, McClelland RL, Ebersold MJ (2002) Measurement of cerebrospinal fluid flow at the cerebral aqueduct by use of phase-contrast magnetic resonance imaging: technique and validation and utility in diagnosing idiopathic normal pressure hydrocephalus. Neurosurgery 50:534–543
Kristensen B, Malm J, Fagerland M, Hietala SO, Johansson B, Eksttedt J, Karlsson T (1996) Regional cerebral blood flow, white matter abnormalities, and cerebrospinal fluid hydrodynamics in patients with idiopathic adult hydrocephalus syndrome. J Neurol Neurosurg Psychiatr 60:282–288
Tullberg M, Jensen C, Ekholm S (2001) Normal pressure hydrocephalus: vascular white matter changes on MR images must not exclude patients from shunt surgery. Am J Neuroradiol 22:1665–1673
Vanneste J, Augustijn P, Davies GA, Dirven C, Tan WF (1992) Normal-pressure hydrocephalus; is cisternograpphy still useful in selecting patients for a shunt? Arch Neurol 49:366–370
Bateman GA, Levi CR, Schofield P, Wang Y, Lovett EC (2005) The pathophysiology of the aqueduct stroke volume in normal pressure hydrocephalus: can co-morbidity with other forms of dementia be excluded? Neuroradiology 47:741–748
Adachi M, Kawanami T, Ohshima F, Kato T (2006) Upper midbrain profile sign and cingulate sulcus sign: MRI findings on sagittal images in idiopathic normal-pressure hydrocephalus, Alzheimer’s disease, and progressive supranuclear palsy. Radiat Med 24:568–572
Bradley WG, Bahl G, Alksne JF (2006) Idiopathic normal pressure hydrocephalus may be a “two hit” disease: benign external hydrocephalus in infancy followed by deep white matter ischemia in late adulthood. J Magn Reson Imaging 24:747–755
Acknowledgements
This work was partly supported by a Research Grant from the Ministry of Health, Labour and Welfare of Japan (2005-Nanchi-17) and by a Grant-in-Aid for Advanced Medical Science Research from the Ministry of Education, Culture, Sports, Science and Technology of Japan.
Conflict of interest statement
We declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Sasaki, M., Honda, S., Yuasa, T. et al. Narrow CSF space at high convexity and high midline areas in idiopathic normal pressure hydrocephalus detected by axial and coronal MRI. Neuroradiology 50, 117–122 (2008). https://doi.org/10.1007/s00234-007-0318-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00234-007-0318-x