Abstract
Background
Cerebrospinal fluid (CSF) protein levels are known to increase in patients with vestibular schwannomas (VS) with concomitant hydrocephalus, however the only information available on perioperative changes in CSF in these patients comes from case reports. Here, we investigated the relation between CSF protein and hydrocephalus in a large series of patients undergoing resection of VS.
Method
We classified 376 patients undergoing resection for VS at our institute into two groups, namely VS and no hydrocephalus (control, n = 319) and VS with concomitant hydrocephalus (n = 57), and compared clinical parameters. Among the 57 patients diagnosed with hydrocephalus, hydrocephalus status was examined by lumbar puncture in 20 patients with communicative hydrocephalus, and pre- and postoperative scores in CSF properties were compared.
Results
Patients in the hydrocephalus group were significantly older than those in the control group (mean, 55.8 vs. 43.8 years), and had a longer disease duration (median, 76 vs. 12 months), larger tumors (median, 15.6 vs. 5.5 ml), and a higher protein concentration in CSF (median, 147.3 vs. 65.1 mg/dl). Perioperative CSF samples of hydrocephalus patients showed a significantly decrease in cerebrospinal pressure after tumor removal (median, -75mmH2O), followed by a decrease in CSF protein (median, -74.5 mg/dl). No patients required the placement of a shunt.
Conclusions
Extended disease duration and elevated CSF protein secondary to the presence of a tumor contribute to the occurrence of hydrocephalus. Primary maximal tumor removal for VS with coexisting hydrocephalus avoids an unnecessary shunt.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Vestibular schwannomas (VS) coexisting with hydrocephalus account for 3.7–18 % of all cases of VS. Communicative hydrocephalus is more frequent than obstructive hydrocephalus in these VS patients [1, 5–7, 19, 22, 25].
Obstructive hydrocephalus results from obstruction of the 4th ventricle or cerebral aqueduct by the mass effect of the tumor and accompanying disruption of cerebrospinal fluid (CSF) flow. Communicative hydrocephalus is reported to result from a number of mechanisms, either alone or in combination, including obstruction of CSF absorption at the arachnoid granulation by protein leakage from the tumor; a decrease in intracranial compliance due to adhesion of the subarachnoid space; meningeal adhesion due to minor hemorrhage from the tumor; and CSF malabsorption, likely due to tumor cells and high fibrinogen concentration in the CSF [7, 13]. However, the cause of communicative hydrocephalus associated with VS has not been described.
Hydrocephalus associated with VS is reported to be improved after adequate tumor resection, and recent opinion notes that hydrocephalus associated with VS is treatable by primary tumor resection alone, without the need for a CSF shunt [1, 8, 13, 19]. Although the CSF protein level is known to increase in hydrocephalus, perioperative changes in CSF in patients with VS-associated hydrocephalus have not been characterized, except for in several case reports [3, 6, 7, 13, 22].
Since 2004, we have routinely treated patients with hydrocephalus associated with VS by primary tumor resection without CSF shunt surgery or 3rd ventriculostomy. Several patients with schedule-restricted surgeries were treated by lumbar drainage or external ventricular drainage. Here, we report the relation between CSF protein level and hydrocephalus in these patients, and the improvement in hydrocephalus and CSF properties.
Materials and methods
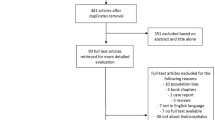
Between August 2007 and March 2012, 405 patients with VS underwent surgery for tumor resection at Tokyo Metropolitan Police Hospital. Among these patients, 29 were excluded due to VS of neurofibromatosis type 2 (14 cases); placement of a ventriculoperitoneal shunt at a different hospital (two cases); difficulty in obtaining CSF for any reason (nine cases); and limitation of the tumor to the internal auditory meatus (four cases). The remaining 376 patients were classified into two groups (control, VS with no hydrocephalus n = 319 (84.8 %); hydrocephalus group, VS with hydrocephalus, n = 57 (15.2 %)) and their clinical parameters were compared with regard to sex, age, disease duration, tumor size, CSF protein, consistency of tumor on magnetic resonance imaging (MRI), and tumor resection rate. Further, in 20 of the 57 patients with hydrocephalus whose hydrocephalus status was checked by lumbar puncture, we also compared perioperative changes in cerebrospinal pressure, CSF protein, CSF sugar, and CSF chloride.
Tumor size was measured on MRI images (Achieva 1.5 and 3 Tesla; Philips, Amsterdam, Netherlands) using commercially available software (Centricity PACS; GE Healthcare, Little Chalfont, UK). Tumor diameter was measured in millimeters in a plane parallel to the pyramidal bone, perpendicular to the pyramidal bone on axial MRI images, and vertically on coronal MRI images, and tumor volume was calculated (ml). Disease duration of tumors was defined as the period from the development of initial symptoms to the correct diagnosis of VS; this datum was treated as a missing value in patients whose tumors were found incidentally and in those whose onset of initial symptoms was not accurately known. Tumor consistency was classified into two types by MRI findings, a solid type consisting entirely of a solid component, and cystic type which included a cystic component. Several surgical approaches were employed, namely the lateral suboccipital approach in 371 cases, middle fossa approach in two, and translabyrinthine approach in three. Hydrocephalus was evaluated on CT images of the head using the Evans index, the ratio of the maximal width of the frontal horns to the maximal diameter of the inner table of the skull at the same level, with a ratio of 0.3 or greater defined as hydrocephalus.
CSF was obtained from the cerebellomedullary cistern or cisterna magna intraoperatively after dural incision. In this procedure, a 5-ml syringe with the external cylinder of a 20-gauge indwelling needle was used to withdraw the CSF sample under vacuum pressure immediately after opening the cerebellomedullary cistern or cisterna magna, with care taken to avoid contamination with blood. We also evaluated the shape of the 4th ventricle and aqueduct on MRI images, and classified cases showing any obstruction to the passage of CSF as obstructive hydrocephalus. Since 2009, we have performed lumbar puncture and obtained a CSF sample both before and 2 or 3 weeks after tumor resection surgery for patients with VS with communicative hydrocephalus with the consent of patients. Perioperative lumbar puncture was performed in the lateral position and cerebrospinal pressure was measured at rest. Obstructive hydrocephalus patients were excluded to avoid tonsillar herniation. This study was approved by the institutional review board (IRB) of Tokyo Metropolitan Police Hospital.
Statistical analysis
Variables were analyzed by the Chi-squared test, Mann–Whitney test and Spearman’s rank correlation coefficient, and those in subgroup analysis by Wilcoxon signed-rank sum test and the paired t test. All analyses were conducted using SPSS version 11 (SPSS INC. Chicago, IL USA).
Results
On comparison of clinical parameters with the control group, patients in the hydrocephalus group was significantly older and had a longer disease duration, larger tumors, and higher protein concentration in the CSF (Table 1). Results showed a significant correlation between tumor size and CSF protein level (r = 0.70, p < 0.01) (Fig. 1).
Subgroup analysis
Thirty-one (54.3 %) of the 57 patients with hydrocephalus had symptoms of hydrocephalus. Symptoms improved after surgery in all 31 cases, and no patient required placement of a shunt. Evaluation of hydrocephalus status at a mean of 4.0 ± 1.4 months after surgery showed a mild decrease in the Evans index, from 0.35 ± 0.03 to 0.32 ± 0.03 (p < 0.01) (Fig. 2).
Perioperative CSF samples were obtained by lumbar tap and suction from the cerebellomedullary cistern in 20 of the 57 patients with hydrocephalus (Table 2). Among them, perioperative cerebrospinal pressure was less than 15 mmH2O in five cases (25 %), between 15 and 20 mmH2O in 5 (25 %), and greater than 20 mmH2O in 10 (50 %), demonstrating a trend towards higher-than-normal levels. Cerebrospinal pressure decreased after tumor removal (median -75 mmH2O, p < 0.01) (Fig. 3a), as did CSF protein (median −74.5 mg/dl, p < 0.01) (Fig. 3b). In contrast, CSF sugar and chloride showed no significant perioperative changes (Fig. 3c, d). Among all 57 cases, tumor removal rate was greater than 95 % in 50 (87.7 %) cases, from 90 to 95 % in three (5.3 %) cases, and less than 90 % in four (7.0 %) cases.
Perioperative change in pressure of CSF, CSF protein, CSF sugar, and chloride. A: cerebrospinal pressure measured by lumbar puncture showed a significant postoperative decrease (p < 0.01). B: CSF protein level showed a significant decrease (p < 0.01) after tumor resection. C and D: no significant perioperative differences were seen in CSF sugar or chloride levels
No significant difference in CSF protein level was seen between CSF obtained before tumor removal by lumbar tap and that obtained from the cerebellomedullary cistern during resection (162.1 ± 113.0 mg/dl vs. 162.5 ± 125.7 mg/dl, p > 0.05).
Discussion
In this study, we confirmed that primary maximal tumor removal for VS with coexisting hydrocephalus can avoid the necessity of a CSF shunt. Patients with hydrocephalus were older and had larger tumors and significantly higher CSF protein levels than control patients. The efficacy of surgery for tumor removal in VS with coexisting hydrocephalus was confirmed by the finding of a perioperative decrease in cerebrospinal pressure and CSF protein. These findings indicate that an extended disease duration and elevated CSF protein secondary to the presence of the tumor contribute to the occurrence of communicative hydrocephalus.
Among a total of 376 patients with VS in this series, 57 (15 %) had concomitant hydrocephalus. Although 45 (79 %) of these were diagnosed with communicative hydrocephalus and 12 (21 %) with obstructive hydrocephalus, a definitive diagnosis was not usually possible because we did not perform a flow study of CSF, and some cases diagnosed as obstructive hydrocephalus may in fact have had characteristics of communicative hydrocephalus.
Results indicated that VS patients with hydrocephalus were significantly older than those without hydrocephalus, and had a longer disease duration, larger tumors, and a higher CSF protein concentration. These findings are consistent with those of previous studies [1, 7, 8, 19–22, 25, 27]. Distribution was highest in those in their 40s in the control group, and in those in their 50s and 60s in the hydrocephalus group. This age distribution of hydrocephalus towards older patients is considered due to the decreased ability of aged patients to absorb CSF, which results from the proliferation of arachnoid cells even when protein levels in CSF are only mildly increased, and longer disease duration [25]. In the present study, patients with hydrocephalus were significantly older and had a longer disease duration than controls. Nevertheless, the finding of young patients with this condition appears to discount the theory that most patients with hydrocephalus are elderly as a result of aging-dependent adhesion of the arachnoid.
In this study, hydrocephalic symptoms improved after surgery in all 31 patients and no patient required a permanent CSF shunt, although two patients required transient CSF drainage to control symptoms. One patient underwent lumbar drainage before surgery and another patient received external ventricular drainage after surgery. We therefore concluded that tumor resection should be conducted first, and that doing so should obviate the need for unnecessary shunt placement.
Among studies reporting that tumor excision contributes to the improvement of hydrocephalus associated with VS [1, 5, 8, 13, 19, 25], the incidence of patients who required shunt placement after tumor removal ranged from 3.8 % to 29.2 % [8, 19, 25]. In the present study, the high tumor removal rate may have contributed to the control of hydrocephalus, with greater than 95 % resection in 50 cases (87.7 %), 90–95 % in three (5.3 %), and less than 90 % in four (7.0 %). The 4th ventricle and cerebral aqueduct were clearly visualized on MRI images, and symptoms were improved after tumor resection in all cases.
Several studies have reported hydrocephalus secondary to procedures using gamma knife for VS [6, 11, 15]. Gamma knife procedures may exacerbate hydrocephalus in cases with a previously enlarged ventricle. Considering the possibility of complications with a CSF shunt, we consider that primary tumor resection is the first choice of hydrocephalus associated with VS, even in aged patients.
Several theories have been proposed to explain the mechanism of hydrocephalus associated with VS, including obstruction of absorption of CSF at the arachnoid granulation by protein leakage from the tumor; adhesion of the subarachnoid space causing a decrease in intracranial compliance; malabsorption of CSF due to tumor-induced arachnoiditis; meningeal adhesions due to recurrent tumor bleeding; and malabsorption due to tumor cells and a high fibrinogen concentration in CSF [7, 13, 22]. No definitive explanation has yet been proposed, however.
Several recent studies have reported that CSF protein levels are elevated in patients with VS and concomitant hydrocephalus [3, 6, 7, 13, 22], and the theory that elevated CSF protein obstructs the absorption of CSF at the arachnoid granulation is widely accepted. Spinal tumors, consisting mainly of schwannomas and gliomas, are also associated with hydrocephalus, and we consider that the mechanism of this hydrocephalus is the same as that with VS, on the basis that CSF protein level is similarly elevated to that with VS, and because the hydrocephalus improves after tumor resection. These studies reported that glioma-associated hydrocephalus requires CSF shunting after tumor removal in all cases due to the dissemination of tumor cells, a finding that does not occur with spinal schwannoma [24]. Several studies reported that elevated CSF protein obstructs absorption of CSF, and that spinal tumors decrease compliance of the caudal spinal portion, which in turn decreases overall compliance of the CSF space [16, 17, 24]. Against this, however, malabsorption of CSF at the arachnoid granulations does not explain enlargement of the ventricles without dilatation of the subarachnoid space; nor does it explain normal pressure hydrocephalus, given that obstruction at the arachnoid granulations should increase intracranial pressure. Further, CSF protein levels were not particularly high in some of our patients with hydrocephalus, but were relatively high in some patients in the control group (Table 1). Greitz et al. therefore consider that enlargement of the ventricles cannot simply be explained by reference to disturbed absorption at the arachnoid granulations alone without dilatation of the subarachnoid space [9]. Protein levels in CSF obtained from the cerebellomedullary cistern were significantly higher in the communicative hydrocephalus group than in the controls. Preoperative cerebrospinal pressure with communicative hydrocephalus was somewhat higher than normal, at greater than 200 mmH2O in ten cases (50 %), from 150 to 200 mmH2O in five (25 %), and less than 150 mmH2O in five (25 %). A number of these cases (n = 10) were categorized as normal-pressure hydrocephalus.
Postoperative lumbar puncture showed a significant decrease in cerebrospinal pressure and CSF protein below normal in all cases (Fig. 3a). Thirty-one (54.3 %) of the 57 patients with hydrocephalus had symptoms of hydrocephalus, all of whom experienced a postoperative improvement in symptoms and significant shrinkage of ventricular size. This finding indicates a relationship between ventricular enlargement and increased CSF protein. Regarding the temporal relationship of these two findings, we speculate that protein elevation precedes ventricular enlargement, on the basis that median CSF protein of the control group was slightly higher (65.1 mg/dl) than normal. With regard to mechanism, protein elevation in CSF is considered due to protein leakage from the tumor or produced by the tumor [2, 4]. The strong correlation between CSF protein and tumor size indicates that enlargement of the tumor is a factor in increased CSF protein.
The circulation theory describes the dynamic state of CSF circulation and is now widely accepted. This theory states that CSF is produced mainly by the choroid plexus and then flows through the ventricles along specific pathways to the subarachnoid space where it is absorbed through Pacchionian granulations into venous sinuses. In recent years, however, accumulating evidence has suggested that the cerebral parenchyma is permeable and exchanges water with the vascular system via aquaporin 4 (AQP4) channels [9, 12, 18]. The AQP4 channel is a membrane protein that promotes the transfer of water by an osmotic pressure gradient, and is expressed on ependymal cells lining the lateral ventricles, the end feet of astrocytes that contact microvessels, and endothelial cells of capillary vessels [10, 23, 26]. Elevation of intraventricular osmotic pressure causes water movement into the ventricles, resulting in their enlargement [14]. We speculate that the osmotic pressure gradient is enlarged by elevation of CSF protein, which then increases water movement from the brain parenchyma to ventricles via AQP4 channels to thereby result in ventricular enlargement. The osmotic pressure gradient decreases after tumor removal, suppressing water movement into the ventricles and thereby improving the hydrocephalus.
Several limitations of this study warrant mention. First, CSF protein was not analyzed. Investigation of the consistency of CSF protein would help answer why CSF protein increases in VS. Second, as a clinical study, we did not investigate the mechanism of occurrence of communicative hydrocephalus. A more comprehensive understanding of this mechanism requires additional research.
Conclusions
We demonstrated the efficacy of tumor resection in VS with concomitant hydrocephalus by examining perioperative decreases in cerebrospinal pressure and CSF protein. Our patients with hydrocephalus were older than the control group, and had larger tumors and significantly higher CSF protein levels. We consider that an extended disease duration and elevated CSF protein levels secondary to the presence of the tumor contribute to the occurrence of hydrocephalus. Primary maximal tumor resection in VS with concomitant hydrocephalus avoids an unnecessary CSF shunt.
References
Atlas MD, Perez de Tagle JR, Cook JA, Sheehy JP, Fagan PA (1996) Evolution of the management of hydrocephalus associated with acoustic neuroma. Laryngoscope 106:204–206
Bamford CR, Labadie EL (1967) Reversal of dementia in normotensive hydrocephalus after removal of a cauda equina tumor. Case report. J Neurosurg 45:104–107
Bloch J, Vernet O, Aube M, Villemure JG (2003) Non-obstructive hydrocephalus associated with intracranial schwannomas: hyperproteinorrhachia as an etiopathological factor? Acta Neurochir (Wien) 145:73–78
Borgesen SE, Sorensen SC, Olesen J, Gjerris F (1997) Spinal tumours associated with increased intracranial pressure. Report of two cases and a discussion on the pathophysiology. Acta Neurol Scand 56:263–268
Briggs RJ, Shelton C, Kwartler JA, Hitselberger W (1993) Management of hydrocephalus resulting from acoustic neuromas. Otolaryngol Head Neck Surg 109:1020–1024
Cauley KA, Ratkovits B, Braff SP, Linnell G (2009) Communicating hydrocephalus after gamma knife radiosurgery for vestibular schwannoma: an MR imaging study. AJNR Am J Neuroradiol 30:992–994
Fukuda M, Oishi M, Kawaguchi T, Watanabe M, Takao T, Tanaka R, Fujii Y (2007) Etiopathological factors related to hydrocephalus associated with vestibular schwannoma. Neurosurgery 61:1186–1192, discussion 1192–1183
Gerganov VM, Pirayesh A, Nouri M, Hore N, Luedemann WO, Oi S, Samii A, Samii M (2011) Hydrocephalus associated with vestibular schwannomas: management options and factors predicting the outcome. J Neurosurg 114:1209–1215
Greitz D (2004) Radiological assessment of hydrocephalus: new theories and implications for therapy. Neurosurg Rev 27:145–165, discussion 166–167
Hasegawa H, Ma T, Skach W, Matthay MA, Verkman AS (1994) Molecular cloning of a mercurial-insensitive water channel expressed in selected water-transporting tissues. J Biol Chem 269:5497–5500
Jeon CJ, Kong DS, Nam DH, Lee JI, Park K, Kim JH (2010) Communicating hydrocephalus associated with surgery or radiosurgery for vestibular schwannoma. J Clin Neurosci 17:862–864
Johnston M, Papaiconomou C (2002) Cerebrospinal fluid transport, a lymphatic perspective. News Physiol Sci 17:227–230
Kanayama S, Kohno M, Okamura K, Yoshino M, Segawa H, Saito I, Sano K (2006) Case of hydrocephalus associated with vestibular schwannoma, treated by tumor removal. No Shinkei Geka 34:391–395 (Jpn)
Krishnamurthy S, Li J, Schultz L, McAllister JP 2nd (2009) Intraventricular infusion of hyperosmolar dextran induces hydrocephalus: a novel animal model of hydrocephalus. Cerebrospinal Fluid Res 6:16
Mohammed TA, Ahuja MS, Ju SS, Thomas J (2010) Normal pressure hydrocephalus after gamma knife radiosurgery for vestibular schwannoma. J Postgrad Med 56:213–215
Morandi X, Amlashi SF, Riffaud L (2006) A dynamic theory for hydrocephalus revealing benign intraspinal tumours: tumoural obstruction of the spinal subarachnoid space reduces total CSF compartment compliance. Med Hypotheses 67:79–81
Nishida K, Ueda S, Matsumoto K, Kusaka K, Takeuchi R (1990) Cauda equina neurinoma associated with normal pressure hydrocephalus–case report. Neurol Med Chir (Tokyo) 30:258–262
Oi S, Di Rocco C (2006) Proposal of “evolution theory in cerebrospinal fluid dynamics” and minor pathway hydrocephalus in developing immature brain. Childs Nerv Syst 22:662–669
Pirouzmand F, Tator CH, Rutka J (2001) Management of hydrocephalus associated with vestibular schwannoma and other cerebellopontine angle tumors. Neurosurgery 48:1246–1253, discussion 1253–1244
Roche PH, Khalil M, Soumare O, Régis J (2008) Hydrocephalus and vestibular schwannomas: considerations about the impact of gamma knife radiosurgery. Prog Neurol Surg 21:200–206
Roche PH, Ribeiro T, Soumare O, Robitail S, Pellet W, Régis J (2004) Hydrocephalus and vestibular schwannomas treated by gamma knife radiosurgery. Neurochirurgie 50:345–349 (French)
Rogg JM, Ahn SH, Tung GA, Reinert SE, Noren G (2005) Prevalence of hydrocephalus in 157 patients with vestibular schwannoma. Neuroradiology 47:344–351
Sobue K, Yamamoto N, Yoneda K, Fujita K, Miura Y, Asai K, Tsuda T, Katsuya H, Kato T (1999) Molecular cloning of two bovine aquaporin-4 cDNA isoforms and their expression in brain endothelial cells. Biochim Biophys Acta 1489:393–398
Sun H, Tian H (2011) Intraspinal tumors accompanied by hydrocephalus: case report, systematic review, and discussion of treatment strategy. Neurologist 17:342–345
Tanaka Y, Kobayashi S, Hongo K, Tada T, Sato A, Takasuna H (2003) Clinical and neuroimaging characteristics of hydrocephalus associated with vestibular schwannoma. J Neurosurg 98:1188–1193
Venero JL, Vizuete ML, Machado A, Cano J (2001) Aquaporins in the central nervous system. Prog Neurobiol 63:321–336
Wada K, Nawashiro H, Shimizu A, Shima K (2003) MRI analysis of hydrocephalus associated with acoustic neurinoma. Acta Neurochir Suppl 86:549–551
Acknowledgments
The authors thank the neurosurgeons, medical engineers, and medical technologists at Tokyo Metropolitan Police Hospital for their assistance in the surgeries for vestibular schwannomas.
Conflicts of interest
The authors declare that they have no conflicts of interest.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Miyakoshi, A., Kohno, M., Nagata, O. et al. Hydrocephalus associated with vestibular schwannomas: perioperative changes in cerebrospinal fluid. Acta Neurochir 155, 1271–1276 (2013). https://doi.org/10.1007/s00701-013-1742-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-013-1742-9