Abstract
Purpose
The results of the treatment of pial AVM provided at our neurosurgical centre are presented. Based on these results and on an overview of literary data on the efficacy and complications of each therapeutic modality, the algorithm of indications, as used at our institution, is presented.
Cohort of patients
The series comprises 195 patients, aged 9 to 87 years and treated in the years 1998–2011. The surgical group consists of 76 patients; of these, 49 patients solely received endovascular treatment, 25 were consulted and referred directly to the radiosurgical unit, and the remaining 45 were recommended to abide by the strategy of “watch and wait”.
Results
In the surgical group, serious complications were 3.9 %, at a 96.1 % therapeutic efficacy. As for AVM treated with purely endovascular methods, serious procedural complications were seen in 4.1 % of patients, with efficacy totalling 32.7 %. One observed patient suffered bleeding, resulting in death. For comparison with literary data for each modality, a survival analysis without haemorrhage following monotherapy for AVM with each particular modality was carried out.
Conclusions
Based on our analysis, we have devised the following algorithm of treatment:
-
1.
We regard surgical treatment as the treatment of choice for AVM of Spetzler-Martin (S-M) grades I and II, and only for those grade III cases that are surgically accessible.
-
2.
Endovascular intervention should mainly be used for preoperative embolisation, as a curative procedure for lower-grade AVM in patients with comorbidities, and as palliation only for higher-grade cases.
-
3.
Stereotactic irradiation with Leksell Gamma Knife (LGK) is advisable, mainly for poorly accessible, deep-seated grade-III AV malformations. In the case of lower grades, the final decision is left to the properly informed patient.
-
4.
Observation should be used as the method of choice in AVM of grades IV and V, where active therapy carries greater risk than the natural course of the disease.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Pial arteriovenous malformation (AVM) is a benign cerebrovascular disease, in which direct pathological communications between cerebral arteries and veins (bypassing the capillary system) form the morphological lesion. The malformation is surrounded by a layer of reactive gliosis. Presenting signs include haemorrhage (50 % of all cases), seizures (25 %), headache (25 %), and less often, neurological deficit caused by ischaemia due to the steal phenomenon [10]. The annual likelihood of AVM rupture was estimated at 2–4 % in Ondra’s study [61], based on a 24-year follow-up of a cohort of 166 patients with symptomatic AVM; this value is regarded as constant throughout the follow-up period [28]. While AVM-related intraparenchymal haemorrhage is associated with a more favourable prognosis compared to intraparenchymal bleeding from other causes, the intraparenchymal component of bleeding from an AVM carries with itself a worse recovery [11]. The probability of poor post-haemorrhage recovery (Rankin score greater than or equal to 2, neurological deficit) is reported at about 5–60 % [11, 19, 21, 23].
According to the commonly used Spetzler and Martin scheme, AVMs are classified into five or six groups relative to their size, localisation in eloquent areas, and the presence or absence of deep venous drainage [83] or recently published three-tier classification based on the same parameters [84]. Certain principles of treatment are also based on this AVM grading system. We currently have the choice of surgical resection, endovascular therapy and stereotactic radiosurgical treatment. Indeed, the methods can be combined—with observation being an additional, though not insignificant, modality.
We opted for an analysis of our own data and for a review of literature of published series. Using figures and graphs thus acquired, we were able to confirm the globally acknowledged principles of AVM management. In our view, the published data provide a suitable basis for discussions with our patients as, in principle, they are the ones to choose the procedure and type of treatment.
Patients and methods
Our cohort is made up of 195 patients (113 men, 82 women) treated at the Department of Neurosurgery, Charles University and Central Military Hospital, Prague. The patients received treatment between 1 January 1998 and 31 August 2011. The database was developed prospectively; the patients’ data were assessed retrospectively. The patients’ age span was between 9 and 87 years, mean age was 42 years. Enrolled were all those patients for whom we acted as the primarily consulted centre. Not included were cases where we merely provided a second opinion on documents from the Czech Republic and from abroad. Consequently, our institution-performed angiography served as the basic parameter for enrolment in the cohort. Malformations were classified according the Spetzler–Martin system. Then, following detailed discussion with each patient and his/her family, we jointly chose the therapeutical modality: surgical resection, endovascular treatment with embolisation, stereotactic radiosurgery, referral to Prague Leksell Gamma Knife (LGK) centre, or observation.
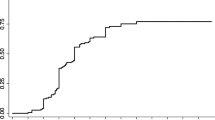
The surgical group consisted of 76 patients, all operated by the senior author; 27 of who had undergone preoperative embolisation of their AVM. Endovascular treatment alone was used for 49 patients, 25 patients were directly referred to the centre of radiosurgery, and the remaining 45 were advised to undergo a policy of “watch and wait”. However, there were also patients enrolled whose clinical condition was too serious to permit any therapeutic intervention. The distribution of AVMs according to the Spetzler–Martin grades in each group is given in Fig. 1, showing preponderance of lower-grade AVM in the surgical group compared to the endovascular group (p = 0.003, chi-square test). The basic characteristics of the patients in the surgical and endovascular groups are given in Table 1. None of the parameters under study (age distribution in each group, or presentation – haemorrhage or epileptic seizure) revealed any significant inter-group differences at the 5 % level (t-test, chi square test). The surgical and endovascular groups were studied for the rate of serious procedural complications (GOS lesser than or equal to 3 after 30 days). Correlation between AVM grade and outcome measured by GOS was assessed using Spearmann correlation coefficient, omitting patients admitted in poor clinical state, in whom poor outcome was due to severity of initial bleeding The efficacy of each therapeutic modality was assessed after complete obliteration of the AVM. The same parameters for the surgical, endovascular and radiosurgical groups were set on the basis of literary search. All larger series obtained by searching PubMed database with key words “brain avm” up to mid 2011 were included in this literature review.
Results
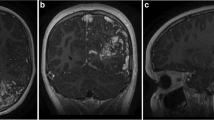
Fourteen out of the 76 surgical patients were admitted in a serious condition, marked by severe neurological deficit or a GCS of less than 9. Three patients in this group were admitted after bleeding from previously irradiated AVM. Preoperative embolisation was used in 27 cases; a total of 50 interventions were made. As an embolisation agent, Onyx was used in nine cases and NBCA in 18. In one patient, severe deficit due to intracerebral haemorrhage occurred after the procedure. The patient was surgically treated and improved markedly 6 months after his deficit. A serious complication during surgery occurred in three patients; two patients (S-M grade 3 and 4) died. One died after 1 week, the other after 8 months in a vegetative state. The cause of unfavourable results was probably normal perfusion pressure breakthrough (NPPB) phenomena [85] (in both cases we experienced uncontrollable perioperative bleeding, resulting in intracerebral hematoma in the AVM bed and severe surrounding brain edema). A third patient (SM grade 3) suffered severe hemiparesis and aphasia. Surgical morbidity and mortality was 3.9 %. Correlation between AVM grade and outcome was significant (p < 0.05) with Spearmann’s coefficient r = 0.32.
At the 1-year follow-up visit, six patients suffered from serious consequences of the initial haemorrhage. Three AVMs (3.9 %) had not been removed completely. In one patient, postoperative angiography was not done due to severe postoperative condition and ensuing death. The second unresolved case was a S-M grade-IV AVM in a 16-year old girl. Her malformation was localised in the basal ganglia and dominant frontal lobe. Embolisation attempt failed after the Brietal testing feeders were from A1 and M1 segments. The AVM was planned for only partial resection, and after this patient was twice irradiated with LGK. The AVM disappeared, but patient vision severely and permanently deteriorated after the second radiosurgical procedure. In the third case, S-M grade IV AVM was partially resected and subsequently the residual AVM was successfully embolised. The overall rate of surgical effectiveness was 96.1 %.
In the endovascular group, 49 patients had total of 87 endovascular procedures. One patient was admitted after bleeding from previously irradiated AVM. As an embolisation agent, Onyx was used in 24 cases and NBCA in 25. In addition, coils were used in nine cases, mainly for treatment of flow-related aneurysms. There was one case of unmanageable haemorrhage during embolisation; in another case, embolisation caused severe neurological deficit due to inadvertent occlusion of the major cerebral artery. Both these patients died. Consequently, the endovascular group morbidity and mortality amounted to 4.1 % (patient-related) and 2.3 % (procedure-related). Complete occlusion was achieved in 16 AVMs, which is success rate of 32.7 % per patient and 18.4 % per procedure. Four patients died within the 1-year follow-up: two after procedural complications, and the other two due to primary haemorrhage. At the annual check-up, one patient had a GOS 3 as a result of primary bleeding. Correlation between AVM grade and GOS was not significant. Table 2 sums up the results of surgical and endovascular therapy for AVM—procedural mortality and morbidity and effectiveness of obliteration—attained at our neurosurgical centre.
Thirty-nine patients were shared with the LGK unit; 25 patients were referred there primarily for treatment; 13 patients were referred after previous partial embolisation of AVM; and one after surgery. Prior to radiotherapy, one patient had coiling performed for an incidental aneurysm on the basilar artery. The only procedural complication of LGK (severe visual impairment) has already been mentioned. At the time of publication, 11 of these 39 patients had their AVM obliterated, the rest were still in latency period without angiographical proof of AVM obliteration.
The observation group consisted of 45 patients whose AVM was deemed either intractable with any of the available therapeutic techniques, or those who declined active treatment or to whom active treatment was recommended (advanced age, incidental lesion, serious comorbidity). This group included five patients whose initial haemorrhage was too serious to permit the consideration of any beneficial therapy, and four of these patients subsequently died. Six others underwent active treatment for another neurosurgical pathology; in all these cases, the AVM was an incidental finding. Three patients were examined for ACI stenosis; two of them had carotid endarterectomy performed, and the third patient underwent carotid stenting. One patient was admitted for acute subarachnoid haemorrhage following rupture of one of two aneurysms of the circle of Willis, coiling was performed on both. One patient suffered subarachnoid haemorrhage (SAH) from posterior inferior cerebellar artery (PICA) aneurysm, which was subsequently coiled. One patient had carotido-cavernous fistula successfully coiled.
In one case, AVM thrombosed spontaneously after minor bleeding. We encountered only one bleeding in the group of patients under observation: a 56-year-old patient with parieto-occipital grade IV AVM suffered fatal devastating heamorrhage after 10 years of observation.
Tables 3, 4 and 5 show the studies that helped to set the values for comparisons with our own results [1, 3, 5–8, 12–18, 20, 22, 24–27, 29–59, 62–67, 69, 70, 72, 73, 75, 77–83, 86–100].
The method of weighted mean was used for this purpose, the number of patients in each given study being the weight. The probability of procedural complications in radiosurgery is equal to the likelihood of bleeding during the three-year period of latency and severe adverse events of irradiation.
Due to the fact that AVM is disease of young and mid age, we have to make inferences at least 30 years ahead. On the acceptance of 3 % annual bleeding rate, a comparison of a thirty-year outlook of bleeding in patients treated with the particular techniques is given in Fig. 2. Furthermore, on the acceptance of 30 % probability of poor recovery after AVM-related bleeding, thirty-year prospective period is plotted in Fig. 3, as a determinant of the likelihood of serious mortality and morbidity. The values of mortality and morbidity, just as those of the efficacy of treatment for the surgical and endovascular groups, were used for constructing the graphs based on our centre’s data. However, the values given for radiosurgical treatment and for observation are derived from literary sources, since our LGK group is quite small and atypical.
As for radiosurgery, an 8 % probability of bleeding was used for the first three postoperative years—the period of latency. All patients treated with the given method where some AVM remnants are detectable are exposed to the yearly probability of bleeding.
Discussion
Results of surgical treatment for pial AVM at our neurosurgical department, as well as results in the rest of the studies, refer to a meticulous selection of patients. Figure 1 makes it quite obvious that most of the higher-grade malformations were dealt with by those methods other than surgical. The preponderance of lower-grade AVM in the surgical group compared to endovascular group (p = 0.003, chi-square test) is attributable to the surgical centre’s preferences. Patients a priori refusing surgical intervention often look for some other therapeutic option themselves. In contrast, patients with operable AVM who seek advice at the surgical centre are mostly well disposed to resection from the outset. Our results are comparable with the published ones [57, 71, 77]. Most of the patients with S-M Grade I and II AVMs are now indicated for surgical treatment, as all other modalities fall far short of offering such an efficacy with such a low rate of complications. Thus, the only decisive factor is the surgeon’s ability to weigh his/her own skills, as not even an operation for a small AVM is an easy task.
The efficacy and rate of complications of independent endovascular embolisation attained at our centre is fully comparable with the average quoted in the rest of the published results. However, assessed over a 30-year span of time, the position of embolisation as an independent method is debatable. An analysis of Fig. 2 will show that only after 10 years post-embolisation is the patient’s prognosis more favourable than the natural course of the disease, with regard to potential risk of bleeding due to a ruptured AVM. Analysing Fig. 3, we can see the point of intersection shifting as far as 25 years from the treatment. On the whole then, owing to its low efficacy and relatively higher rate of procedural complications in comparison with the other modalities, the benefit of independent curative embolisation is negligible, as it can never reach a significant difference assessed against the natural course of the disease. The role of endovascular treatment in the management of AVMs is yet to be established. In our view, endovascular intervention is an essential part of AVM obliteration, though solely for selective embolisation of deep branches. As for the superficial branches, embolisation is a counterproductive approach, hampering subsequent AVM resection. The superficial branches are easy to deal with after the dura is opened, there is no need for obstructive surgical glue, and in addition, anatomical orientation is better. Embolisation of those branches will distend the deep feeders; their treatment is already the hardest part of AVM surgery even without embolisation. As we have seen repeatedly, even an embolised vessel can bleed readily after being cut as a whole. Arresting such haemorrhage is no easy task, as the glue cannot be coagulated easily, nor the vessel clipped. Recently, some goups report much higher success rates [58, 70], but it is questionable whether these results are repeatable on a much broader scale. Another important finding of this study is the absence of correlation between AVM grade and clinical outcome, meaning risk of endovascular procedure is similar for all AVM grades. This result strongly favours surgery with very low morbidity as a method of choice for lower grade AVMs. New procedures, mainly the introduction of Onyx into endovascular practice, did not change efficacy of endovascular methods significantly, and only few groups of authors presents markedly better results [58, 64].
In contrast, the position of radiosurgery remains unshakeable in the treatment of AVM; objections can only be raised against its unidirectional and liberal limits of indications. What comes as a surprise in our milieu are the 20 % better results than those commonly reported [45] (Table 5). Surgical treament of grade I and II AVM is associated with 0 % probability of permanent deficit [19], at a well nigh 100 % rate of efficacy. In view of this, a solid medical substantiation is called for if the patient is to be exposed to the hazards of AVM-related haemorrhage during the period of latency at a markedly lower probability of obliteration—84 % [68]. Conversely, for deep-seated, poorly accessible small-sized malformations, radiosurgery is the method of choice. In such malformations suitable for radiotherapy, the rate of obliteration is reported at up to 70 % [42]. In the case of larger-size AVM, a similarly very high efficacy is reported after single or multiple irradiations. One study [35] mentions an efficacy of 62 % for a group of AVMs larger than 9 cm3; Sirin et al. [76] attained an efficacy of 50 % for AVMs of more than 15 cm3 in size. On the other hand, there have been cases of bleeding from an AVM, even after radiosurgical treatment and angiographic evidence of its obliteration [9, 74]. In our view, the greatest problem of radiosurgery lies in the variously high percentage of patients (reported at 10 up to 50 %) in whom the AVM is discernible even after repeated irradiation. Admittedly, ours is a limited body of experience (three patients) of surgery on AVM after LGK treatment. Nevertheless, it is a very optimistic experience; the operations were not more difficult. This prompts ideas of converting higher-grade AVM radiosurgically into AVMs of grades I and II, to make them suitable for neurosurgery. In irradiated patients, the definitive therapy is in fact postponed by more than 6 years. As follows from the above facts, the therapeutical modalities are competitive with regard to low-grade malformations. This applies mainly to surgical resection relative to stereotactic irradiation. True inter-modality cooperation has been reached in grade III AVM, where preoperative or pre-radiosurgical embolisation can facilitate obliteration and reduce the risks of subsequent therapy [60]. What is still missing, however, is clear evidence of this logical conclusion, as some authors question the effect of pre-radiosurgical embolisation [4]. It should be noted that grade III AVMs are a very heterogeneous group. Therefore, any decision must take into account the individual characteristics of each AVM.
Grade IV and V AVMs are complex and large malformations; straightforward surgery is too risky and radiosurgery is inefficacious. This is why we usually opt for the watch and wait strategy. In some cases, endovascular active approach can be used, depending on angioarchtecture, risk factors such as intranidal aneurysm, etc.. As a rule, complete occlusion can hardly be achieved, though it is possible to treat, e.g. an intranidal aneurysm, or to reduce the malformation blood flow. Today, most neurosurgical teams regard AVM of grades IV and V as lesions suitable for observation. Some of those lesions, however, could be managed by cooperation of all three treatment modalities. Such an option and a well thought through management plan is to be considered, especially in young patients with high rupture-risk AVMs. In patients treated by multimodal approach, each new step should be established anew, according to the results of the previous one. The team must not dogmatically follow the management plan devised at the beginning of treatment.
During the construction of the two graphs, the constant probability of AVM rupture was estimated at 3 % per annum, leaving aside the opinion that during a few post-rupture years the likelihood of AVM rerupture is prominently higher; 6 to 18 % in the first year and gradually approaching the initial value [2, 21].
The previous paragraphs discussed the decisive AVM-related factors. The most important point here is the AVM classification according to Spetzler and Martin. The decision-making process invariably involves the need to estimate the risks and efficacy of the therapy against the hazards of the natural course. Apart from assessing the AVM as such, it is necessary to weigh up a number of other variables unrelated to the AVM. These are: 1) patient-related factors—the presenting symptoms of the AVM. A patient whose AVM triggered only a single epileptic paroxysm needs an approach that is different from another patient with recurrent AVM haemorrhage. The patient’s age is important; some statistics show that any active therapy in patients over 45 years of age can no longer counteract the risks of the natural course. Other patient-related factors include concomitant diseases and ASA grade. A patient with a congenital heart defect where anaesthesia would already be dangerous should be recommended for radiosurgical treatment. 2) Institution-related factors. Is the clinical centre sufficiently experienced and equipped? Are the results comparable with those reported in literature? Have they been published? 3)Factors pertaining to the attending physician/surgeon. These are the most difficult to evaluate. As a rule, self-assessment is the least objective. However, honesty is the most important quality of any physician. Ultimately it is the patient, correctly and fairly informed, who should have the main say in deciding on the therapy.
Conclusion
Backed by our experience of AVM treatment and by our assessment of the likelihood of post-treatment haemorrhage, we have devised the following algorithm of treatment:
-
1.
Surgery is to be seen as the method of choice for AVM of S-M grades I and II; as for grade III cases—only for superficially localised lesions. Higher-grade AVMs are only suitable for surgery in exceptional cases, palliatively or in cases of recurrent haemorrhage.
-
2.
Endovascular intervention should mainly be used for preoperative embolisation (that in itself is questionable), or as a curative procedure for lower-grade AVM in polymorbid patients, and again only palliatively for higher grades—the steal phenomenon, intranidal aneurysm.
-
3.
Stereotactic radiotherapy with LGK is advisable mainly for poorly accessible, deep-seated grade-III AVM. In the case of lower grades, the final decision is left to the thoroughly informed patient.
-
4.
Observation is to be taken as the method of choice for AVM of grades IV and V, where active therapy represents a greater risk that the natural course of the disease.
References
Abad JM, Alvarez F, Manrique M, Garcia-Blazquez M (1983) Cerebral arteriovenous malformations. Comparative results of surgical vs conservative treatment in 112 cases. J Neurosurg Sci 27:203–210
Al-Shahi R, Warlow C (2001) A systematic review of the frequency and prognosis of arteriovenous malformations of the brain in adults. Brain 124:1900–1926
Andrade-Souza YM, Ramani M, Scora D, Tsao MN, TerBrugge K, Schwartz ML (2006) Radiosurgical treatment for rolandic arteriovenous malformations. J Neurosurg 105:689–697
Andrade-Souza YM, Ramani M, Scora D, Tsao MN, TerBrugge K, Schwartz ML (2007) Embolization before radiosurgery reduces the obliteration rate of arteriovenous malformations. Neurosurgery 60:443–452
Andrade-Souza YM, Zadeh G, Scora D, Tsao MN, Schwartz ML (2005) Radiosurgery for basal ganglia, internal capsule, and thalamus arteriovenous malformation: clinical outcome. Neurosurgery 56:56–63, discussion 63–54
Andrews BT, Wilson CB (1987) Staged treatment of arteriovenous malformations of the brain. Neurosurgery 21:314–323
Aoki Y, Nakagawa K, Tago M, Terahara A, Kurita H, Sasaki Y (1996) Clinical evaluation of gamma knife radiosurgery for intracranial arteriovenous malformation. Radiat Med 14:265–268
Blamek S, Tarnawski R, Miszczyk L (2011) Linac-based stereotactic radiosurgery for brain arteriovenous malformations. Clin Oncol 23(8):525–531
Bradac O, Mayerova K, Hrabal P, Benes V (2010) Haemorrhage from a radiosurgically treated arteriovenous malformation after its angiographically proven obliteration: a case report. Cen Eur Neurosurg 71:92–95
Brown RDJ, Flemming KD, Meyer FB, Cloft HJ, Pollock BE, Link MJ (2005) Natural history, evaluation, and management of intracranial vascular malformations. Mayo Clin Proc 80:269–281
Choi JH, Mast H, Sciacca RR, Hartmann A, Khaw AV, Mohr JP, Sacco RL, Stapf C (2006) Clinical outcome after first and recurrent hemorrhage in patients with untreated brain arteriovenous malformation. Stroke 37:1243–1247
Coffey RJ, Nichols DA, Shaw EG (1995) Stereotactic radiosurgical treatment of cerebral arteriovenous malformations. Gamma unit radiosurgery study group. Mayo Clin Proc 70:214–222
Cohen-Gadol AA, Pollock BE (2006) Radiosurgery for arteriovenous malformations in children. J Neurosurg 104:388–391
Colombo F, Benedetti A, Pozza F, Marchetti C, Chierego G (1989) Linear accelerator radiosurgery of cerebral arteriovenous malformations. Neurosurgery 24:833–840
Debrun GM, Aletich V, Ausman JI, Charbel F, Dujovny M (1997) Embolization of the nidus of brain arteriovenous malformations with n-butyl cyanoacrylate. Neurosurgery 40:112–120, discussion 120–111
Deruty R, Pelissou-Guyotat I, Mottolese C, Bascoulergue Y, Amat D (1993) The combined management of cerebral arteriovenous malformations. Experience with 100 cases and review of the literature. Acta Neurochir (Wien) 123:101–112
Friedman WA, Bova FJ, Bollampally S, Bradshaw P (2003) Analysis of factors predictive of success or complications in arteriovenous malformation radiosurgery. Neurosurgery 52:296–307, discussion 307–298
Gao K, Yang XJ, Mu SQ, Li YX, Zhang YP, Lu M, Wu ZX (2009) Embolization of brain arteriovenous malformations with ethylene vinyl alcohol copolymer: technical aspects. Chin Med J (Engl) 122:1851–1856
Greenberg MS (2006) Handbook of Neurosurgery. Thieme Medical Publishers, New York
Hadjipanayis CG, Levy EI, Niranjan A, Firlik AD, Kondziolka D, Flickinger JC, Lunsford LD (2001) Stereotactic radiosurgery for motor cortex region arteriovenous malformations. Neurosurgery 48:70–76, discussion 76–77
Halim AX, Johnston SC, Singh V, McCulloch CE, Bennett JP, Achrol AS, Sidney S, Young WL (2004) Longitudinal risk of intracranial hemorrhage in patients with arteriovenous malformation of the brain within a defined population. Stroke 35:1697–1702
Hamilton MG, Spetzler RF (1994) The prospective application of a grading system for arteriovenous malformations. Neurosurgery 34:2–7
Hartmann A, Mast H, Mohr JP, Koennecke H-C, Osipov A, Pile-Spellman J, Duong DH, Young WL (1998) Morbidity of intracranial hemorrhage in patients with cerebral arteriovenous malformation. Stroke 29:931–934
Hartmann A, Pile-Spellman J, Stapf C, Sciacca RR, Faulstich A, Mohr JP, Schumacher HC, Mast H (2002) Risk of endovascular treatment of brain arteriovenous malformations. Stroke 33:1816–1820
Hartmann A, Stapf C, Hofmeister C, Mohr JP, Sciacca RR, Stein BM, Faultisch MS, Mast H (2000) Determinants of neurological outcome after surgery for brain arteriovenous malformation. Stroke 31:2361–2364
Hassler W, Hejazi N (1998) Complications of angioma surgery--personal experience in 191 patients with cerebral angiomas. Neurol Med Chir (Tokyo) 38(Suppl):238–244
Haw CS, TerBrugge K, Willinsky R, Tomlinson G (2006) Complications of embolization of arteriovenous malformations of the brain. J Neurosurg 104:226–232
Hernesniemi JA, Dashti R, Juvela S, Vaart K, Niemela M, Laakso A (2008) Natural history of brain arteriovenous malformations: a long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurgery 63:823–829, discussion 829–831
Heros RC, Korosue K, Diebold PM (1990) Surgical excision of cerebral arteriovenous malformations: late results. Neurosurgery 26:570–577, discussion 577–578
Huang Z, Dai Q, Suo J, Liu F, Wang C, Yin W (1995) Percutaneous endovascular embolization of intracerebral arteriovenous malformations. Experience in 72 cases. Chin Med J (Engl) 108:413–419
Izawa M, Hayashi M, Chernov M, Nakaya K, Ochiai T, Murata N, Takasu Y, Kubo O, Hori T, Takakura K (2005) Long-term complications after gamma knife surgery for arteriovenous malformations. J Neurosurg 102(Suppl):34–37
Javalkar V, Pillai P, Vannemreddy P, Caldito G, Ampil F, Nanda A (2009) Gamma knife radiosurgery for arteriovenous malformations located in eloquent regions of the brain. Neurol India 57:617–621
Jayaraman MV, Marcellus ML, Hamilton S, Do HM, Campbell D, Chang SD, Steinberg GK, Marks MP (2008) Neurologic complications of arteriovenous malformation embolization using liquid embolic agents. AJNR Am J Neuroradiol 29:242–246
Jomin M, Lesoin F, Lozes G (1985) Prognosis for arteriovenous malformations of the brain in adults based on 150 cases. Surg Neurol 23:362–366
Karlsson B, Jokura H, Yamamoto M, Soderman M, Lax I (2007) Is repeated radiosurgery an alternative to staged radiosurgery for very large brain arteriovenous malformations? J Neurosurg 107:740–744
Karlsson B, Lindquist C, Steiner L (1997) Prediction of obliteration after Gamma Knife surgery for cerebral arteriovenous malformations. Neurosurgery 40:425–431
Katsaridis V, Papagiannaki C, Aimar E (2008) Curative embolization of cerebral arteriovenous malformations (AVMs) with Onyx in 101 patients. Neuroradiology 50:589–597
Kim HY, Chang WS, Kim DJ, Lee JW, Chang JW, Kim DI, Huh SK, Park YG, Chang JH (2010) Gamma Knife surgery for large cerebral arteriovenous malformations. J Neurosurg 113(Suppl):2–8
Kim LJ, Albuquerque FC, Spetzler RF, McDougall CG (2006) Postembolization neurological deficits in cerebral arteriovenous malformations: stratification by arteriovenous malformation grade. Neurosurgery 59:53–59
Kiran NA, Kale SS, Vaishya S, Kasliwal MK, Gupta A, Sharma MS, Sharma BS, Mahapatra AK (2007) Gamma Knife surgery for intracranial arteriovenous malformations in children: a retrospective study in 103 patients. J Neurosurg 107:479–484
Kobayashi T, Tanaka T, Kida Y, Oyama H, Niwa M, Maesawa S (1996) Gamma knife treatment of AVM of the basal ganglia and thalamus. No To Shinkei 48:351–356
Kurita H, Kawamoto S, Sasaki T, Shin M, Tago M, Terahara A, Ueki K, Kirino T (2000) Results of radiosurgery for brain stem arteriovenous malformations. J Neurol Neurosurg Psychiatry 68:563–570
Lawton MT, Du R, Tran MN, Achrol AS, McCulloch CE, Johnston SC, Quinnine NJ, Young WL (2005) Effect of presenting hemorrhage on outcome after microsurgical resection of brain arteriovenous malformations. Neurosurgery 56:485–493, discussion 485–493
Ledezma CJ, Hoh BL, Carter BS, Pryor JC, Putman CM, Ogilvy CS (2006) Complications of cerebral arteriovenous malformation embolization: multivariate analysis of predictive factors. Neurosurgery 58:602–611
Liščák R, Vladyka V, Šimonová G, Urgošík D, Novotný J, Janoušková L, Vymazal J (2007) Arteriovenous malformations after Leksell Gamma Knife radiosurgery: rate of obliteration and complications. Neurosurgery 60:1005–1016
Liu HM, Huang YC, Wang YH (2000) Embolization of cerebral arteriovenous malformations with n-butyl-2-cyanoacrylate. J Formos Med Assoc 99:906–913
Lundqvist C, Wikholm G, Svendsen P (1996) Embolization of cerebral arteriovenous malformations: part II—aspects of complications and late outcome. Neurosurgery 39:460–467, discussion 467–469
Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Jungreis CA, Maitz AH, Horton JA, Coffey RJ (1991) Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg 75:512–524
Lv X, Wu Z, Jiang C, Li Y, Yang X, Zhang Y, Zhang N (2010) Complication risk of endovascular embolization for cerebral arteriovenous malformation. Eur J Radiol
Maimon S, Strauss I, Frolov V, Margalit N, Ram Z (2010) Brain arteriovenous malformation treatment using a combination of Onyx and a new detachable tip microcatheter, SONIC: short-term results. AJNR Am J Neuroradiol 31:947–954
Malik GM, Seyfried DM, Morgan JK (1996) Temporal lobe arteriovenous malformations: surgical management and outcome. Surg Neurol 46:106–114, discussion 114–105
Maruyama K, Kawahara N, Shin M, Tago M, Kishimoto J, Kurita H, Kawamoto S, Morita A, Kirino T (2005) The risk of hemorrhage after radiosurgery for cerebral arteriovenous malformations. N Engl J Med 352:146–153
Massager N, Regis J, Kondziolka D, Njee T, Levivier M (2000) Gamma knife radiosurgery for brainstem arteriovenous malformations: preliminary results. J Neurosurg 93(Suppl 3):102–103
Meisel HJ, Mansmann U, Alvarez H, Rodesch G, Brock M, Lasjaunias P (2002) Effect of partial targeted N-butyl-cyano-acrylate embolization in brain AVM. Acta Neurochir (Wien) 144:879–887, discussion 888
Merland JJ, Rufenacht D, Laurent A, Guimaraens L (1986) Endovascular treatment with isobutyl cyano acrylate in patients with arteriovenous malformation of the brain. Indications, results and complications. Acta Radiol Suppl 369:621–622
Miyawaki L, Dowd C, Wara W, Goldsmith B, Albright N, Gutin P, Halbach V, Hieshima G, Higashida R, Lulu B, Pitts L, Schell M, Smith V, Weaver K, Wilson C, Larson D (1999) Five year results of LINAC radiosurgery for arteriovenous malformations: outcome for large AVMS. Int J Radiat Oncol Biol Phys 44:1089–1106
Morgan MK, Rochford AM, Tsahtsarlis A, Little N, Faulder KC (2004) Surgical risks associated with the management of grade I and II brain arteriovenous malformations. Neurosurgery 54:832–839
Mounayer C, Hammami N, Piotin M, Spelle L, Benndorf G, Kessler I, Moret J (2007) Nidal embolization of brain arteriovenous malformations using Onyx in 94 patients. AJNR Am J Neuroradiol 28:518–523
O’Laoire SA (1995) Microsurgical treatment of arteriovenous malformations in critical areas of the brain. Br J Neurosurg 9:347–360
Ogilvy CS, Stieg PE, Awad I, Brown RD Jr, Kondziolka D, Rosenwasser R, Young WL, Hademenos G (2001) Recommendations for the management of intracranial arteriovenous malformations: a statement for healthcare professionals from a special writing group of the stroke council, American Stroke Association. Stroke 32:1458–1471
Ondra SL, Troupp H, George ED, Schwab K (1990) The natural history of symptomatic arteriovenous malformations of the brain: a 24-year follow-up assessment. J Neurosurg 73:338–339
Pan DH, Guo WY, Chung WY, Shiau CY, Chang YC, AWang LW (2000) Gamma knife radiosurgery as a single treatment modality for large cerebral arteriovenous malformations. J Neurosurg 93(Suppl 3):113–119
Panagiotopoulos V, Gizewski E, Asgari S, Regel J, Forsting M, Wanke I (2009) Embolization of intracranial arteriovenous malformations with ethylene-vinyl alcohol copolymer (Onyx). AJNR Am J Neuroradiol 30:99–106
Pierot L, Januel AC, Herbreteau D, Barreau X, Drouineau J, Berge J, Sourour N, Cognard C (2009) Endovascular treatment of brain arteriovenous malformations using onyx: results of a prospective, multicenter study. J Neuroradiol 36:147–152
Pik JHT, Morgan MK (2000) Microsurgery for small arteriovenous malformations of the brain: results in 110 consecutive patients. Neurosurgery 47:571–577
Pikus HJ, Beach ML, Harbaugh RE (1998) Microsurgical treatment of arteriovenous malformations: analysis and comparison with stereotactic radiosurgery. J Neurosurg 88:641–646
Pollock BE, Gorman D, Coffey RJ (2003) Patient outcomes after arteriovenous malformation radiosurgical management: results based on a 5- to 14-year follow-up study. Neurosurgery 52:1291–1297
Pollock BE, Lunsford LD, Kondziolka D, Maitz A, Flickinger JC (1994) Patient outcomes after stereotactic radiosurgery for “operable” arteriovenous malformations. Neurosurgery 35:1–8
Reyns N, Blond S, Gauvrit J-Y, Touzet G, Coche B, Pruvo J-P, Dhellemmes P (2007) Role of radiosurgery in the management of cerebral arteriovenous malformations in the pediatric age group: data from a 100-patient series. Neurosurgery 60:268–276
Saatci I, Geyik S, Yavuz K, Cekirge HS (2011) Endovascular treatment of brain arteriovenous malformations with prolonged intranidal Onyx injection technique: long-term results in 350 consecutive patients with completed endovascular treatment course. J Neurosurg
Schaller C, Schramm J (1997) Microsurgical results for small arteriovenous malformations accessible for radiosurgical or embolization treatment. Neurosurgery 40:664–672
Schaller C, Schramm J, Haun D (1998) Significance of factors contributing to surgical complications and to late outcome after elective surgery of cerebral arteriovenous malformations. J Neurol Neurosurg Psychiatry 65:547–554
Schlienger M, Atlan D, Lefkopoulos D, Merienne L, Touboul E, Missir O, Nataf F, Mammar H, Platoni K, Grandjean P, Foulquier JN, Huart J, Oppenheim C, Meder JF, Houdart E, Merland JJ (2000) Linac radiosurgery for cerebral arteriovenous malformations: results in 169 patients. Int J Radiat Oncol Biol Phys 46:1135–1142
Shin M, Kawahara N, Maruyama K, Tago M, Ueki K, Kirino T (2005) Risk of hemorrhage from an arteriovenous malformation confirmed to have been obliterated on angiography after stereotactic radiosurgery. J Neurosurg 102:842–846
Shin M, Maruyama K, Kurita H, Kawamoto S, Tago M, Terahara A, Morita A, Ueki K, Takakura K, Kirino T (2004) Analysis of nidus obliteration rates after gamma knife surgery for arteriovenous malformations based on long-term follow-up data: the University of Tokyo experience. J Neurosurg 101:18–24
Sirin S, Kondziolka D, Niranjan A, Flickinger JC, Maitz A, Lunsford LD (2006) Large arteriovenous malformations: indications and outcomes in otherwise untreatable patients. Neurosurgery 58:17–27
Sisti MB, Kader A, Stein BM (1993) Microsurgery for 67 intracranial arteriovenous malformations less than 3 cm in diameter. J Neurosurg 79:653–660
Smyth MD, Sneed PK, Ciricillo SF, Edwards MS, Wara WM, Larson DA, Lawton MT, Gutin PH, McDermott MW (2002) Stereotactic radiosurgery for pediatric intracranial arteriovenous malformations: the University of California at San Francisco experience. J Neurosurg 97:48–55
Solomon RA, Connolly ES Jr, Prestigiacomo CJ, Khandji AG, Pile-Spellman J (2000) Management of residual dysplastic vessels after cerebral arteriovenous malformation resection: implications for postoperative angiography. Neurosurgery 46:1052–1060, discussion 1060–1052
Song JK, Eskridge JM, Chung EC, Blake LC, Elliott JP, Finch L, Niakan C, Maravilla KR, Winn HR (2000) Preoperative embolization of cerebral arteriovenous malformations with silk sutures: analysis and clinical correlation of complications revealed on computerized tomography scanning. J Neurosurg 92:955–960
Sorimachi T, Koike T, Takeuchi S, Minakawa T, Abe H, Nishimaki K, Ito Y, Tanaka R (1999) Embolization of cerebral arteriovenous malformations achieved with polyvinyl alcohol particles: angiographic reappearance and complications. AJNR Am J Neuroradiol 20:1323–1328
Spears J, TerBrugge KG, Moosavian M, Montanera W, Willinsky RA, Wallace MC, Tymianski M (2006) A discriminative prediction model of neurological outcome for patients undergoing surgery of brain arteriovenous malformations. Stroke 37:1457–1464
Spetzler RF, Martin NA (1986) A proposed grading system for arteriovenous malformations. J Neurosurg 65:476–483
Spetzler RF, Ponce FA (2011) A 3-tier classification of cerebral arteriovenous malformations. Clinical article. J Neurosurg 114:842–849
Spetzler RF, Wilson CB, Weinstein P, Mehdorn M, Townsend J, Telles D (1978) Normal perfusion pressure breakthrough theory. Clin Neurosurg 25:651–672
Stapf C, Connolly ES, Schumacher HC, Sciacca RR, Mast H, Pile-Spellman J, Mohr JP (2002) Dysplastic vessels after surgery for brain arteriovenous malformations. Stroke 33:1053–1056
Sun DQ, Carson KA, Raza SM, Batra S, Kleinberg LR, Lim M, Huang J, Rigamonti D (2011) The radiosurgical treatment of arteriovenous malformations: obliteration, morbidities, and performance status. Int J Radiat Oncol Biol Phys 80:354–361
Taylor CL, Dutton K, Rappard G, Pride GL, Replogle R, Purdy PD, White J, Giller C, Kopitnik TA Jr, Samson DS (2004) Complications of preoperative embolization of cerebral arteriovenous malformations. J Neurosurg 100:810–812
Tew JM Jr, Lewis AI, Reichert KW (1995) Management strategies and surgical techniques for deep-seated supratentorial arteriovenous malformations. Neurosurgery 36:1065–1072
Valavanis A, Yasargil MG (1998) The endovascular treatment of brain arteriovenous malformations. Adv Tech Stand Neurosurg 24:131–214
van Rooij WJ, Sluzewski M, Beute GN (2007) Brain AVM embolization with Onyx. AJNR Am J Neuroradiol 28:172–177
Veznedaroglu E, Andrews DW, Benitez RP, Downes MB, Werner-Wasik M, Rosenstock J, Curran WJ, Rosenwasser MH (2004) Fractionated stereotactic radiotherapy for the treatment of large arteriovenous malformations with or without previous partial embolization. Neurosurgery 55:519–531
Vinuela F, Fox AJ, Pelz D, Debrun G (1986) Angiographic follow-up of large cerebral AVMs incompletely embolized with isobutyl-2-cyanoacrylate. AJNR Am J Neuroradiol 7:919–925
Weber W, Kis B, Siekmann R, Kuehne D (2007) Endovascular treatment of intracranial arteriovenous malformations with onyx: technical aspects. AJNR Am J Neuroradiol 28:371–377
Xu F, Ni W, Liao Y, Gu Y, Xu B, Leng B, Song D (2011) Onyx embolization for the treatment of brain arteriovenous malformations. Acta Neurochir (Wien) 153:869–878
Yamamoto M, Hara M, Ide M, Ono Y, Jimbo M, Saito I (1998) Radiation-related adverse effects observed on neuro-imaging several years after radiosurgery for cerebral arteriovenous malformations. Surg Neurol 49:385–397, discussion 397–388
Yen CP, Monteith SJ, Nguyen JH, Rainey J, Schlesinger DJ, Sheehan JP (2010) Gamma Knife surgery for arteriovenous malformations in children. J Neurosurg Pediatr 6:426–434
Zabel A, Milker-Zabel S, Huber P, Schulz-Ertner D, Schlegel W, Debus J (2005) Treatment outcome after linac-based radiosurgery in cerebral arteriovenous malformations: retrospective analysis of factors affecting obliteration. Radiother Oncol 77:105–110
Zhou D, Liu Z, Yu X, Qi S, Du J (2000) Rotating Gamma System radiosurgery for cerebral arteriovenous malformations. Stereotact Funct Neurosurg 75:109–116
Zipfel GJ, Bradshaw P, Bova FJ, Friedman WA (2004) Do the morphological characteristics of arteriovenous malformations affect the results of radiosurgery? J Neurosurg 101:390–392
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bradac, O., Charvat, F. & Benes, V. Treatment for brain arteriovenous malformation in the 1998–2011 period and review of the literature. Acta Neurochir 155, 199–209 (2013). https://doi.org/10.1007/s00701-012-1572-1
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-012-1572-1