Abstract
Background
A small subset of patients with adult Chiari I malformation without basilar invagination (BI) and instability show ventral cervicomedullary distortion/compression and have symptoms pertaining to that. The cause of this ventral compression remains speculative. Additionally, it is unclear if these patients would require ventral decompression with posterior fusion or only posterior decompression would suffice.
Methods
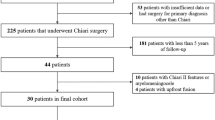
Sixteen adult patients with Chiari I malformation with significant ventral cervicomedullary compression, in the absence of BI, were included in the study. Atlantoaxial dislocation (AAD) was excluded in these patients by flexion-extension craniovertebral junction X-rays and computed tomography (CT). Their clinical profile, especially symptoms pertaining to cervicomedullary compression, i.e. dysphagia, dysarthria and spasticity, were graded. The ventral cervicomedullary compression (VCMC) was quantified using pBC2 (maximum perpendicular distance to the basion-infero posterior point of the C2 body) on sagittal magnetic resonance imaging (MRI) and only those patients with pBC2 ≥9 mm were included. Furthermore, retroversion of dens and retro odonotid tissue thickness was calculated in each patient. Fifteen patients underwent posterior decompression alone and one refused surgery. Follow-up was done every 3 months. Repeat MRI was done at 1 year following surgery to look for pBC2.
Results
The mean pBC2 was 11 ± 0.2 mm. Retroversion of dens was responsible for VCMC in three patients and periodontoid crown in 13. There was no correlation between the tonsillar descent, age and the pBC2. All patients improved in symptoms of cervicomedullary compression following surgery. One patient worsened 6 months after initial improvement. The pBC2 did not change, as seen on follow-up MRI done in five patients.
Conclusions
VCMC in adult patients with Chiari I malformation in the absence of BI and/or AAD is due to periodontoid tissue (crown) or retroverted dens. Though a long-term study is required, it appears that all patients with Chiari I malformation, irrespective of the VCMC, can be given a chance with posterior decompression alone. Transoral decompression with posterior fusion may be required in a small subset of patients who fail to improve or worsen following posterior decompression only.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
The presence of ventral cervicomedullary compression (VCMC) in patients of Chiari I malformation has been described usually due to basilar invagination (BI) [3]. There is a group of adult patients with Chiari I malformation without traditional BI and/or atlanto axial dislocation (AAD) but with the clinical features of VCMC [6]. These patients have definite signs of ventral compression in the form of severe spasticity and many have lower cranial nerve involvement with difficulty in swallowing and speaking. The role of ventral decompression is questionable. The purpose of this study was to determine (1) the cause of ventral compression in these patients and (2) whether posterior decompression alone is in itself sufficient.
Materials and methods
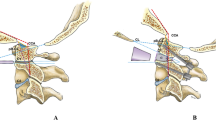
Sixteen adult patients with Chiari I malformation with VCMC (≥9 mm) were included in the study [6]. None of them had BI or AAD, as confirmed on X-rays or computed tomography (CT) of the craniovertebral junction (CVJ). Patients with syringobulbia were excluded. The clinical grading was done using a modified scale devised by us (Table 1). The clinical features suggestive of VCMC—dysarthria, spasticity, swallowing difficulty and ataxia—were graded on this scale. These were the symptoms that affected the patient’s activities of daily living. Higher grades suggested severe disability. Clinical features pertaining to syrinx (lower motor weakness, dissociate and suspended anaesthesia) were separated from those due to VCMC. Sagittal magnetic resonance imaging (MRI) of the patients was studied in detail for extent of tonsillar descent, retroversion of dens, platybasia and VCMC. The VCMC was measured using the pBC2 (maximum perpendicular distance to the basion-infero posterior point of the C2 body) [6] (Fig. 1a). Only those patients with VCMC ≥9 mm were included in the study. The VCMC was either due to the crown or posterior inclination of the odontoid. The angulation of the dens was measured as the angle between the line joining the tip of odontoid and midpoint of C2 base [10] (Fig. 1b). The periodontoid tissue (crown) was calculated separately by subtracting the bony portion (of the dens) from pBC2 (Fig. 1a). CT CVJ was obtained in all patients. Periodontoid bony changes and associated segmentation defects (occipitalised arch of atlas and C2-3 fusion) were noted.
a) The methodology for measuring pBC2 (line b) and crown length (line c). Line a joins the basion to the posterior most point of the C2 body and perpendicular at the maximum indentation measures pBC2 (line b). Exclusion of bony part (cancellous) from pBC2 gives us the crown length (line c), which reflects the soft tissue. b The measurement of retroversion of the odontoid. The angle between the line joining the odontoid tip and the midpoint of the C2 body
Fifteen patients underwent posterior decompression alone and one patient refused surgery. A 2.5-cm suboccipital craniectomy from condyle to condyle was done with cervical laminectomy to expose the caudal limit of tonsillar herniation. The dura was incised obliquely across the foramen magnum, cutting the dural bands and releasing the adhesions. Duraplasty was done using nuchal fascia. Precautions were taken to avoid blood entering the subarachnoid space. The post-operative clinical grading was done at follow-up every 3 months using the same scale. Post-operative MRI of the CVJ was done at 1 year to look for adequacy of posterior decompression [defined as cerebrospinal fluid (CSF) flow across the posterior margin of foramen magnum seen on T2-weighted sagittal image] and VCMC (Fig. 2). MRI was repeated earlier if clinically indicated.
a Mid-sagittal MRI of a patient with Chiari I malformation with significant VCMC due to crown. b Post-operative image of the same patient at 1 year follow-up, showing adequate decompression as demonstrated by the CSF flow posteriorly across the foramen magnum. This patient showed significant improvement after surgery
Non-parameteric tests (Wilcoxon signed-ranks tests and Mann-Whitney U test) were used to analyse the data.
Results
The results are summarised in Table 2.The mean age was 32.7 ± 9.4 (range 17–52) years. All patients had spasticity significant enough to interfere with their daily activities and five were bedridden. Seven patients had dysarthria and dysphagia. In three of these seven patients, the dysphagia and dysarthria was so severe that the relatives could not understand their speech and they could not swallow, requiring nasogastric tube feeds. The dysarthria was mainly due to lower cranial nerve involvement. The pBC2 ranged between 9 and 17 mm with a mean of 11.5 ± 2.3 mm. Retroversion of dens ranged from 55 to 95 degrees (mean 77 ± 10.6). Seven patients had retroversion of dens <80 degrees. The pBC2 was increased mainly due to retroverted dens (crown length <50% of pBC2 ) (Fig. 3) in three patients and due to crown alone in three patients (crown length was at least 75% of pBC2). There was more retroversion of the dens and less of the periodontoid crown. Two patients with a crown showed bony changes posterior to or around the dens (Fig. 4). There was no correlation between the pBC2/crown and basal angle, tonsillar descent or preoperative disability grade due to VCMC. Additionally, there was no correlation between age and the above-mentioned factors. The follow-up ranged from 3 to 35 months (mean 10.2 months).
There was complication of surgical procedure in one patient. She had a CSF leak in the post-operative period with infection requiring antibiotics. All patients improved in respect of neck pain. Most of them could resume work or daily activities. Post-operative MRI at 1 year obtained for four patients showed no increase in the ventral compression that was seen preoperatively (Fig. 2b). One patient had increased spasticity after initial improvement that lasted for about 6 months. Repeat MRI in this patient revealed no increased compression at the cervicomedullary junction (in fact CSF flow was seen both anteriorly and posteriorly across the foramen magnum with reduction in syrinx) (Fig. 5). Another patient improved by 50%, which has been static after 6 months; MRI obtained at <1 year follow-up (because of clinical indication) revealed the same amount of ventral compression and no change in syrinx. However, posterior decompression appeared adequate. All symptoms due to cervicomedullary compression showed statistically significant improvement following foramen magnum decompression when analysed individually as well as collectively.
a, b Pre-operative mid-sagittal T1- and T2-weighted MRI images showing significant VCMC with syrinx. c Post-operative T2-weighted MRI image at 1 year of the same patient showing CSF flow both anteriorly and posteriorly across the foramen magnum with reduced syrinx. This patient worsened after an initial 6 months of improvement
Clinical features pertaining to syrinx remained largely unchanged. Post-operative MRI could be obtained in five patients. Only two of these five had syrinx on pre-operative MRI, of which it reduced significantly in one.
Discussion
Ventral brain stem compression with Chiari I malformation without traditional BI has been described in the paediatric population [6]. The pBC2 was used to quantify ventral compression. The same index was used in our group of adult patients with Chiari I malformation with VCMC. This index has been used as it directly measures the ventral cervicomedullary encroachment by the odontoid and its investing tissues into the rostral spinal canal. Additionally, it is unaffected by flexion-extension. A pBC2 ≥9 mm was taken as a cut-off, as it was shown as significant by Grabb et al. [6].
The pBC2 was increased either due to periodontoid crown or retroversion of the dens. The genesis of the crown has been described previously as exuberant granulation secondary to instability in non-rheumatoid arthritis and pannus formation in inflammatory lesions [7]. This periodontoid tissue disappears on stabilising posteriorly [11]. However, there was no instability in our cases, as confirmed on flexion-extension X-rays and CT scans. Also, a biopsy sent from one patient in whom ventral decompression was done revealed no inflammation or evidence of granulation. In fact it revealed degenerative changes alone. However, this patient was not included in the study as he had BI.
Menezes et al. [8] pointed out that atlas assimilation and segmentation failures of the upper cervical spine may contribute to ligamentous laxity and proliferation of granulation tissue at the craniocervical junction that eventually leads to BI and irreducibility. In the series by Grabb et al. [6], segmentation defects correlated with the pBC2. However, in our series, only six patients had segmentation failure (occipitalised C1 or C2-3 fusion or both) that did not correlate with the VCMC.
Calcification may develop around the odontoid process, synovial membrane, articular capsule and ligaments and 90% of these deposits are posteriorly. It has been usually reported in the elderly and without the predisposing inflammation it is thought to be due to degenerative changes [5]. When such a lesion becomes symptomatic with neck pain with or without myelopathy it constitutes ‘crowned dens syndrome’ [5].
The aforementioned causes do not explain the genesis of a periodontoid crown in patients with Chiari I malformation without instability or segmentation defects. The tonsils move up and down across the foramen magnum, as proved on cine MR, blocking the CSF flow intermittently [9]. This produces a relative instability between the neural tissue and the foramen magnum. To avoid this, there is a hypertrophy of the ligaments or possible osteophyte formation from the posterior edge of the dens as evident on the thin CT images. After the posterior decompression, the space for medulla and cord increases, thereby improving the symptoms. The movement of soft tissue across the new (decompressed) foramen magnum edge is only of CSF, thereby taking care of the relative soft tissue-bony instability. The osteophyte/crown does not increase any further as is evident in follow-up MRI of our patients. Such a crown is usually not seen in cases where the odontoid is inclined posteriorly. Retroverted dens may be a part of compensatory mechanism where in the lordosis of the cervical spine is increased so as to restrict the tonsillar movements across the foramen magnum, or it represents a mere congenital deformity. It is also possible that the periodontoid soft tissue actually represents folding of the ligaments, including the tectorial membrane, which remains lax and thick (due to infolding of the ligaments) in the absence of dens retroversion but becomes taut and thin when the retroverted dens stretches it.
The conventional treatment for Chiari I malformation includes foramen magnum decompression alone. Symptoms from cervicomedullary compression improve dramatically with posterior decompression alone [1]. A subset of patients with Chiari I malformation (without BI and AAD) have significant VCMC/kink as seen on imaging. Does this subset of patients require ventral decompression? Delayed neurological worsening after posterior decompression despite initial good response has been mentioned only in two patients (one of them had BI) [1, 2].
Out of 40 paediatric patients in series by Grabb et al. [6], 11 patients had VCMC ≥9 mm. However, operative details of only four out of these 11 patients were mentioned. These four patients had other procedures in addition to posterior decompression (transoral in one and posterior fusion in three). Of these three patients, one worsened neurologically and required additional transoral decompression [6].
There is a group of patients who have incurving of the basion with adult Chiari I malformation and have BI according to Chamberlain’s/McGregor’s line but not according to McRae’s line. Goel [4] has described this as Type B BI with adult Chiari I malformation. The ventral indentation on the brain stem is smooth and there is no kinking. The odontoid process and clivus remains anatomically aligned. Simple posterior foramen magnum decompression has been suggested for type B patients [4]. This is similar to our group of patients who had increased pBC2 due to retroverted odontoid.
In our series, one patient worsened after initial improvement and another patient had partial improvement. Repeat MRI in the first patient revealed a good flow of CSF across the foramen magnum, both anteriorly and posteriorly, with reduction of syrinx. Repeat flexion-extension X-rays of the CVJ showed no instability. The second patient had retroverted dens and the kinking of the cord remained the same. This patient has been advised transoral decompression.
Short follow-up is the limitation of this study and it is possible that after the initial improvement a subset of patients might require a transoral decompression at a later stage. However, sudden post-operative worsening was not noted in any of our patients. Thus it appears that all patients with Chiari I malformation without atlanto-axial instability and BI, irrespective of the amount of ventral compression, benefit following posterior decompression alone. Transoral decompression and posterior fusion may be considered in select cases without improvement or worsening of symptoms following posterior fossa decompression.
References
Bindal AK, Dunsker SB, Tew JM Jr (1995) Chiari I malformation: classification and management. Neurosurgery 37:1069–1074
Dyste GN, Menezes AH, VanGilder JC (1989) Symptomatic Chiari malformations. An analysis of presentation, management, and long-term outcome. J Neurosurg 71(2):159–168
Elster AD, Chen MY (1992) Chiari I malformations: clinical and radiologic reappraisal. Radiology 183(2):347–353
Goel A (2009) Basilar invagination, Chiari malformation, syringomyelia: a review. Neurol India 57(3):235–246
Goto S, Umehara J, Aizawa T, Kokubun S (2007) Crowned dens syndrome. J Bone Joint Surg Am 89(12):2732–2736
Grabb PA, Mapstone TB, Oakes WJ (1999) Ventral brain stem compression in pediatric and young adult patients with Chiari I malformations. Neurosurgery 44(3):520–528
Grob D, Würsch R, Grauer W, Sturzenegger J, Dvorak J (1997) Atlantoaxial fusion and retrodental pannus in rheumatoid arthritis. Spine (Phila Pa 1976) 22(14):1580–1583, discussion 1584
Menezes AH (1995) Primary craniovertebral anomalies and the hindbrain herniation syndrome (Chiari I): data base analysis. Pediatr Neurosurg 23(5):260–269
Pujol J, Roig C, Capdevila A, Pou A, Martí-Vilalta JL, Kulisevsky J, Escartín A, Zannoli G (1995) Motion of the cerebellar tonsils in Chiari type I malformation studied by cine phase-contrast MRI. Neurology 45(9):1746–1753
Tubbs RS, Wellons JC 3rd, Blount JP, Grabb PA, Oakes WJ (2003) Inclination of the odontoid process in the pediatric Chiari I malformation. J Neurosurg 98(1 Suppl):43–49
Young WF, Boyko O (2002) Magnetic resonance imaging confirmation of resolution of periodontoid pannus formation following C1/C2 posterior transarticular screw fixation. J Clin Neurosci 9(4):434–436
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Salunke, P., Sura, S., Futane, S. et al. Ventral compression in adult patients with Chiari 1 malformation sans basilar invagiantion: cause and management. Acta Neurochir 154, 147–152 (2012). https://doi.org/10.1007/s00701-011-1215-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1215-y