Abstract
Background
Electrode fractures are known hardware problems in patients with deep brain stimulation (DBS) and require surgical revision. Short circuits, loose connections or disconnections of only single contacts of the common quadripolar stimulation electrodes are more subtle dysfunctions and can result in decreased efficacy of DBS. Measuring the impedances of electrodes helps detect such technical dysfunctions. This study evaluates the frequency and clinical implications of abnormal impedance measurements.
Methods
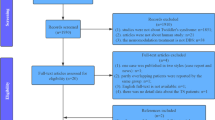
We retrospectively analyzed findings of systematic impedance checks in 591 consecutive patients with DBS for various movement disorders treated in our DBS center between 2005 and 2010.
Findings
A technical dysfunction was found in 36 out of 1,142 electrodes (3.2%). Short circuits (22 electrodes) were more frequent than disconnections of single contacts (8 electrodes) or loose contacts (6 electrodes). Moreover, after 109 replacements of impulse generators another 16 electrodes revealed technical dysfunctions, again with short circuits (9 electrodes) exceeding disconnections of single contacts (5 electrodes) and loose contacts (2 electrodes). Most of the short circuits occurred immediately after surgical interventions. In contrast, among dysfunctions occurring later during long-term DBS, disconnections and loose contacts prevailed. Surgical revision was performed in 4 of the overall 52 electrodes with dysfunctions, whereas in the other electrodes adjustment of stimulation parameters resulted in stable and satisfying symptom control.
Conclusions
Technical dysfunctions of stimulation electrodes or extension leads are rare but important sources of unsatisfying DBS efficacy. In the majority of cases DBS programming or reprogramming allows avoiding surgical revision.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Deep brain stimulation (DBS) has become an important therapeutic option for a variety of movement disorders, most notably Parkinson’s disease (PD), dystonia and tremors [3, 9, 12, 15]. More recently, DBS has also been used for epilepsy and psychiatric disorders like obsessive compulsive disorders and depression [5, 8, 11].
The principle of DBS is to implant stimulation electrodes into target areas like the subthalamic nucleus (STN), the internal pallidum (GPi) or the ventral intermediate thalamic nucleus (Vim) for chronic stimulation. The stimulation electrodes are connected to impulse generators (IPGs) via extension leads, and the IPG is programmed telemetrically to tailor the volume of tissue activated according to the clinical stimulation effects. Efficacy of DBS, therefore, strongly depends on the precise localization of the electrodes and the programming of optimal stimulation parameters. Quadripolar stimulation electrodes are the most common electrodes used for DBS. These electrodes allow the activation of single contacts or combinations of four contacts to optimally adjust the volume of tissue activated by DBS.
Efficacy and stability of DBS also depend on proper technical function to ensure a constant volume of tissue activated by stimulation. Apart from dysfunctions of the IPG the most important technical problems can be (1) disconnections of leads, (2) short circuits between leads or (3) loose contacts with significant changes of the impedance, intermittent disconnection or intermittent short circuits with other leads. The possibility to measure the impedance of leads is the most important technical feature to help detecting such dysfunctions and is further supported by the clinical evaluation of stimulation effects and side effects. DBS systems by Medtronic Co. (Minneapolis, MN) are the most common systems used worldwide, and the available IPGs provide the possibility of impedance measurements. In the following study, we analyzed the frequency of technical dysfunctions and the clinical management in 591 consecutive DBS patients and 1,142 electrodes.
Materials and methods
The Neurological Rehabilitation Center Godeshoehe is a DBS center selecting appropriate candidates for surgery and programming DBS thereafter. Control and optimization of stimulation parameters are also part of a hospital rehabilitation program for patients referred from other DBS centers [1, 2, 13]. Furthermore, patients with DBS are followed up in our movement disorder outpatient clinic.
Apart from the systematic evaluation of stimulation effects, all patients with DBS undergo a routine of technical checking of the DBS system. This check includes the measurement of all impedances to detect dysfunctions and a check of the battery capacity. The results of these checks are documented electronically. Similarly, all changes of stimulation parameters are continuously documented electronically.
The IPG models provided by Medtronic for DBS include single-channel IPGs (Itrel II® Model 7424 followed by SoletraTM Model 7426) as well as dual channel IPGs (Kinetra® Model 7428, Activa PC, Model 37601 and Activa RC, Model 37612). Two models of intracranial stimulation electrodes are used for DBS in movement disorders both providing four stimulation contacts at the tip separated by either 0.5 mm (model 3389) or 1.5 mm (model 3387). These quadripolar stimulation electrodes are connected via extension leads (Model 7482 or Model 7482A for Kinetra® and SoletraTM, Model 37085 for Activa PC and Activa RC) to the IPG. The extension leads for the Activa models feature a stretch mechanism with 15% extensibility. An adaptor can be used to connect the extension leads model 7482 or 7482A to an Activa PC or RC if a Kinetra® or SoletraTM is replaced by an IPG of the Activa models.
Impedance measurements are provided by help of a programmer (N’Vision Clinician Programmer, Model 8840). A complete check of all electrode leads and contacts includes monopolar measurements of each contact as cathode against the IPG case as anode as well as bipolar measurements between all contacts. For the SoletraTM and the Kinetra® these measurements are performed by the Clinician Programmer at 30 Hz, 210 μs and 1.5 V. For the Activa-IPGs these measurements are performed at 100 Hz, 80 μs and 0.7 V.
In our study, a disconnection of stimulation contacts was assumed if (1) the monopolar impedance of a contact was >2,000 Ohm in case of a SoletraTM, >4,000 Ohm in case of a Kinetra® or >40,000 Ohm in case of an Activa; (2) in case of a SoletraTM or Kinetra® if the current flow with increasing amplitudes did not exceed the resting current (<7 μA for SoletraTM and <15 μA for Kinetra®); and (3) if stimulation with therapeutic stimulation parameters (130 Hz, 60 μs, voltages up to 10.5 V) did not induce stimulation effects of the central nervous system. A short circuit of stimulation contacts was assumed if the impedance of a bipolar measurement was <150 Ohm. This definition is rather arbitrary because the impedance of short circuited leads can vary depending on the location of the short circuit and depending on the monopolar impedances of the affected leads. In fact, the threshold to highlight “low” impedances in impedance measurements of Activa-IPGs is 250 Ohm, whereas other authors have used a limit of 50 Ohm to assume a short circuit [6]. Further evidence for a short circuit is given if monopolar therapeutic stimulation of the affected contacts results in comparable thresholds of stimulation effects and side effects. Loose contacts were assumed if disconnections or short circuits were not stable in repeated measurements and/or if impedances and stimulation effects suggested intermittent changes in the volume of tissue activated by DBS.
In our study, we retrospectively analyzed the electronic documents of stimulation parameters and impedance checks in all patients with DBS treated between 2005 and 2010 in the Neurological Rehabilitation Center Godeshoehe. Mean ± standard deviations are given for the analysis of stimulation parameters and demographical data.
Results
Five hundred ninety-one patients with DBS for various movement disorders were included. Demographical data on the different diseases and age at observation onset are given in Table 1.
In the vast majority of patients IPGs by Medtronic were used (Table 2). Only 8 out of 613 IPGs (1.3%) were from 2 other companies. These eight IPGs were excluded from the further analysis. Due to the more recent introduction the observation times of patients with Activa PC or Activa RC were shorter than those for patients with SoletraTM or Kinetra® (Table 2).
Stimulation parameters including the number of activated stimulation contacts per electrode are depicted in Table 3. Most notably, in 76% of the electrodes only one single contact was activated, and in less than 3% three or four contacts were activated.
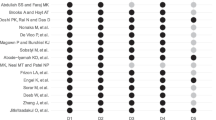
A technical dysfunction at the initial check or during long-term observation before an IPG replacement was found in 36 out of 1,142 electrodes (3.2%) (Table 4). Separated into those electrodes connected via non-extensible extension leads to the IPG models SoletraTM or Kinetra® and those connected via extensible extension leads to the IPG models Activa PC or Activa RC, a technical dysfunction in the former group was found in 2.8% and in the latter group in 4.1%.
During the initial period after electrode implantation 21 malfunctioning electrodes were observed: 16 electrodes with short circuits (11 connected to Activa PC or RC, 5 connected to SoletraTM or Kinetra®), 3 electrodes with disconnections of single contacts (1 connected to an Activa RC, 1 connected to a SoletraTM and 1 connected to a Kinetra®) and 2 electrodes with loose contacts (1 connected to Activa RCs, 1 connected to a Kinetra®). During long-term follow-up another eight electrodes (connected to SoletraTM or Kinetra®) developed dysfunctions: disconnections of single contacts were found in four electrodes and loose contacts in three electrodes; one electrode had to be replaced because of a wound dehiscence 9 months after surgery and showed a stable short circuit of contacts thereafter. Another seven electrodes with technical dysfunctions (short circuits in 5 electrodes, a disconnection of a single contact in 1 electrode and loose contacts in 1 electrode) were observed in patients with already longer time periods of DBS before first presentation to our center so that the time of occurrence could not be determined. However, it is of note that two out of these seven cases had a previous IPG replacement, and in one case an extension lead had been replaced before first presentation.
One hundred nine IPG replacements were performed in patients with long-term follow-up in our center because of battery failures or hardware failures. After the IPG replacement a new technical dysfunction was found in 16 electrodes (Table 5). In 13 electrodes the malfunction was observed immediately after IPG replacement (short circuits in 8 electrodes, disconnections of single contacts in 4 electrodes and loose contacts in 1 electrode). Another three electrodes developed a technical dysfunction (short circuit in 1 electrode, disconnections in 2 electrodes) during long-term follow-up after IPG replacement, one after additional surgical transfer of the IPG from a thoracic to an abdominal position (see case 4).
Most of the dysfunctions remained stable during long-term observation and did not extend to other contacts. Among those cases with observation times of at least 3 months, 14 electrodes with short circuits remained stable during 85 ± 71 weeks follow-up. Similarly, eight electrodes with disconnections remained stable during 182 ± 91 weeks follow-up.
Only 3 of the 52 malfunctioning electrodes resulted in a surgical revision. A fourth electrode with a short circuit between contacts was replaced primarily because of a significant dislocation. In one case the IPG was repositioned because of tension between the extension lead and the abdominally placed IPG case (Activa RC), which resulted in progressive disconnection of contacts 10 and 11 of the right hemispheric electrode during hospital rehabilitation 2 weeks after implantation (monopolar impedances of contacts 10 and 11 at admission 975 Ohm and 955 Ohm, respectively, and 2 weeks later both >40,000 Ohm). In a second case a PD patient 6 months after an IPG replacement (Kinetra® for Kinetra®) and 4½ years after DBS implantation noticed that pressure on the connection between electrodes and extension leads resulted in sudden double vision and dysaesthesia of the left arm, suggesting intermittent short circuit of the activated dorsal contact 3 to more ventral contacts. An X-ray demonstrated a deviation of the third of four setscrews at the connection between extension lead and electrode. Intraoperatively a defect of both the extension lead and the electrode was found, and both were successfully replaced. In a third case a lead fracture of the stimulation electrode was found, necessitating the replacement of this electrode (see case 4).
In all other cases programming or reprogramming allowed avoiding surgical revision. In case of disconnected or loose contacts neighboring contacts were activated for chronic DBS, resulting in satisfying symptom control. In case of short circuits either neighboring contacts were activated or the short-circuited contacts were programmed together as cathode. Short-circuited contacts characteristically show comparable thresholds of stimulation effects/side effects if one of the respective contacts is activated alone or both together as cathode. The advantage of activating them together was that in case of an only intermittent short circuit, a sudden change of the volume of tissue activated and consequently the stimulation effects was avoided (see case 3 below).
The following four cases illustrate different presentations of technical dysfunctions and the clinical management.
Case 1: A female patient was operated on at the age of 63 years because of an 11-year history of PD complicated by severe fluctuations and levodopa-induced dyskinesias. STN DBS resulted in a significant improvement of motor symptoms and a reduction of the levodopa equivalent dosage from 1,670 mg/day to 750 mg at the 1-year follow-up. Impedances of all contacts were normal after surgery, and a monopolar stimulation of contacts 1 for the left STN (130 Hz, 60 μs, 4.5 V) and 5 for the right STN (130 Hz, 60 μs, 4.3 V) was programmed. After 1½ years of DBS, she noticed a significant increase in motor symptoms. The impedance check revealed a disconnection of the active contact 1 for the left hemispheric STN: monopolar impedance >4,000 Ohm (Kinetra®), increase of the voltage at 130 Hz and 60 μs up to 8 V without stimulation effects and without increase of the resting current (<15 μA). All other impedances were normal. DBS was reprogrammed, resulting in satisfying symptom control at a monopolar stimulation of contacts 0 and 2 (130 Hz, 60 μs, 3.0 V). The disconnection of contact 1 remained stable during the next 1½-year follow-up period.
Case 2: A female patient was operated on at the age of 58 years because of a 5-year history of a severe right-sided PD tremor. Left hemispheric Vim DBS resulted in almost complete tremor reduction. Impedances of all contacts were normal after surgery, and a bipolar stimulation of contacts 0 and 1 as anode and 2 as cathode with 130 Hz, 60 μs and 5.4 V was programmed. After 4 months she noticed a reoccurrence of the right-sided tremor. The impedance check of contact 0 was >2,000 Ohm (1,511 Ohm in the previous measurement), and, most notably, the threshold of side effects (dysaesthesias) in a monopolar stimulation setting with contact 0 alone increased from 2.0 V during the initial programming to 7.0 V. Reprogramming to a bipolar setting with 1 as cathode and 2 as anode, later extended to 1 and 2 as cathode and 3 as anode (130 Hz, 6.0 V), resulted in satisfying and stable tremor reduction during the next 1½-year follow-up period.
Case 3: A male patient was operated on at the age of 69 years because of an 11-year history of PD complicated by fluctuations with a significant off-tremor and levodopa-induced dyskinesias. STN DBS during the first 3 months resulted in unstable symptom control with periods of severe dyskinesias and periods of increased tremor. Repeated impedance checks revealed intermittent short circuits (impedances <100 Ohm) between contacts 4 and 5, 4 and 6, 4 and 7 as well as 5 and 6. An unusual monopolar stimulation with all contacts 4 to 7 as cathode against the case as anode at 130 Hz, 60 μs and 1.5 V resulted in satisfying and stable symptom control during the following 2½-year follow-up. Although symptom control was stable throughout the follow-up period, the impedance checks continued to show changing results with short circuits between variable contacts.
Case 4: A PD patient was operated on at the age of 64 years because of a 5-year history of tremor-dominant PD. After 3½ years of STN DBS the IPG was replaced because of battery failure (Kinetra® for Kinetra®). Seven months later the IPG was transferred from a thoracic to an abdominal position because of discomfort. Four months later she complained of a significant tremor increase at the left extremities. The impedance check of the right hemispheric electrode only revealed an abnormally low impedance between contacts 0 and 3 of 214 Ohm. The main finding, however, was that test stimulation at contacts 0 and 1 with 130 Hz and 60 μs up to 8 V only elicited dysesthesia at the site of the connection between the electrode and extension lead, but not the tetanic facial contraction observed after the initial DBS surgery 4 years earlier at thresholds of 4 V. An X-ray demonstrated a lead fracture of the stimulation electrode near the connection to the extension lead. The electrode was successfully replaced thereafter.
Discussion
This retrospective clinical study in a large population of patients with various movement disorders treated by DBS demonstrates that the overall frequency of technical dysfunctions was low (3.2%). However, short circuits, disconnections or loose connections can have significant impact on DBS efficacy and need to be excluded particularly in those patients with unsatisfactory symptom control. Most importantly, in the majority of cases surgical revision can be avoided by adequate programming or reprogramming of stimulation parameters.
Technical support to identify electrode dysfunctions, therefore, is an important feature for DBS systems. In our study we focused on DBS systems by Medtronic because they are the most commonly applied systems worldwide. Impedance measurements have been improved in the more recent models Activa PC and Activa RC. Most notably, the range of measurable impedances has been increased to 40,000 Ohm. The upper limit of both the SoletraTM (2,000 Ohm) and the Kinetra® (4,000 Ohm) are not sufficient to indicate an electrode disconnection. Although the monopolar impedance of a single contact is usually between 900 and 1,500 Ohm, impedances above 2,000 Ohm or even above 4,000 Ohm are not rare, and can still serve for stable and satisfying DBS efficacy. Therefore, disconnections or significant changes in electrode impedances need further clinical evaluation of stimulation effects/side effects and the respective thresholds. The importance of additional clinical evaluation of stimulation effects is further demonstrated by the patient of case report 4. The lead fracture in this case was not detected by impedance measurements but by stimulation effects: local dysesthesias at the site of the fracture.
Similarly, the detection of short circuits cannot solely rely on a single lower impedance threshold in bipolar impedance measurements between contacts. In our study, we used a threshold of 150 Ohm, although the impedances in detected cases were mostly well below 100 Ohm, with 2 Ohm being the lowest impedance measured. A short circuit between contacts means that in monopolar settings the current is directed to all short-circuited contacts no matter whether chosen as cathode alone or together. In our experience, a successful way to cope with this situation has been either by activating alternative contacts or by immediately activating the short-circuited contacts as cathode together. This approach prevents clinical changes of DBS efficacy in case of loose contacts with only intermittent short circuits, as demonstrated in case 3 of the case reports.
Short circuits between contacts were the most frequent immediate dysfunction noticed after electrode implantation or surgical revisions, whereas among the dysfunctions developed during long-term stimulation, loose connections and disconnections of single contacts were more frequent. Interestingly, complete lead fractures that have been reported as long-term complications by other authors in up to 5% of the patients have been rare in our own study [4, 7, 10, 14]. The main reason is probably that the connector of the electrode and extension lead in all patients in our study was located at the calvarium, whereas higher rates of lead fractures were primarily reported in cases with the connection below the mastoid [4]. In cases of complete lead fractures surgical replacement is necessary [10]. In contrast, disconnection of single leads in our study could be managed by appropriate programming/reprogramming of stimulation parameters in most cases. From these experiences we further conclude that short circuits or disconnections of single contacts do not routinely require workup by X-ray examination of the DBS. X-ray can be restricted to those patients in whom DBS efficacy after programming/reprogramming remains unsatisfactory, particularly if impedances or clinical data point to a lead breakage.
Surgical interventions (implantation, revision, IPG replacement) bear a risk of damage to the DBS leads. Accordingly, most of the dysfunctions were found immediately after implantation of the DBS system and also after IPG replacements. In fact, such technical dysfunctions have been previously reported to be a source of reduced DBS efficacy after IPG replacements [2]. Intraoperative handling of electrodes and extension leads, therefore, requires particular care to avoid such damage. Moreover, electrodes should be carefully checked after all surgical interventions. All unnecessary surgical interventions should be avoided, most notably too frequent IPG replacements. This can be achieved by adjustment of appropriate stimulation parameters, for example, the activation of single contacts for monopolar stimulation, the use of rather short impulse widths and the avoidance of unnecessarily high frequencies. Furthermore, the time of IPG replacement should be appropriately anticipated. In patients with particularly high energy consumption and, consecutively, short battery lifetimes, rechargeable IPGs (Activa RC) can further reduce surgical interventions during long-term follow-up.
Although this was not a prospective study, it is interesting to note that the incidence of technical dysfunctions immediately after implantation seems to be higher in IPGs of the new models of Activa PC and Activa RC, which are connected to the stimulation electrodes via extension leads with 15% extensibility. These observations suggest a higher vulnerability of extensible extension leads and call for an increased alertness for dysfunctions in these models. Long-term observations are needed to evaluate the risk of technical dysfunctions during long-term follow-up of these models.
Conclusions
Electrode dysfunctions with stable or intermittent short circuits, changes of impedances or even disconnections of single leads of the quadripolar stimulation electrodes and extension leads are rare but important sources of unsatisfactory DBS efficacy. Most dysfunctions occur immediately after surgical interventions (initial implantation, surgical revision or IPG replacement), and remain stable thereafter. Programming/reprogramming in the majority of cases allows avoiding further surgical revision. DBS systems should allow impedance measurements in a sufficient range to help clinicians identify such dysfunctions.
References
Allert N, Dohle C, Horn JW, Kelm S, Kirsch H, Nolte PN, Weirich W, Karbe H (2011) Rehabilitation of Parkinson patients with deep brain stimulation—Experiences of the Neurological Rehabilitation Center Godeshoehe. Nervenarzt 82:462–467
Allert N, Kirsch H, Weirich W, Karbe H (2009) Stability of symptom control after replacement of impulse generators for deep brain stimulation. J Neurosurg 110:1274–1277
Benabid AL, Chabardes S, Mitrofanis J, Pollak P (2009) Deep brain stimulation of the subthalamic nucleus for the treatment of Parkinson's disease. Lancet Neurol 8:67–81
Blomstedt P, Hariz MI (2005) Hardware-related complications of deep brain stimulation: a ten year experience. Acta Neurochirurgica 147:1061–1064
Burdick AP, Foote KD (2011) Advancing deep brain stimulation for obsessive-compulsive disorder. Expert Rev Neurother 11:341–344
Butson CR, Maks CB, McIntyre CC (2006) Sources and effects of electrode impedance during deep brain stimulation. Clin Neurophysiol 117:447–454
Fernández FS, Alvarez Vega MA, Antuña Ramos A, Fernández González F, Lozano Aragoneses B. Lead fractures in deep brain stimulation during long-term follow-up (2010) Parkinsons Dis 2010:409356
Fisher R, Salanova V, Witt T, Worth R, Henry T, Gross R, Oommen K, Osorio I, Nazzaro J, Labar D, Kaplitt M, Sperling M, Sandok E, Neal J, Handforth A, Stern J, DeSalles A, Chung S, Shetter A, Bergen D, Bakay R, Henderson J, French J, Baltuch G, Rosenfeld W, Youkilis A, Marks W, Garcia P, Barbaro N, Fountain N, Bazil C, Goodman R, McKhann G, Babu Krishnamurthy K, Papavassiliou S, Epstein C, Pollard J, Tonder L, Grebin J, Coffey R, Graves N, SANTE Study Group (2010) Electrical stimulation of the anterior nucleus of thalamus for treatment of refractory epilepsy. Epilepsia 51:899–908
Flora ED, Perera CL, Cameron AL, Maddern GJ (2010) Deep brain stimulation for essential tremor: a systematic review. Mov Disord 25:1550–1559
Hamani C, Lozano AM (2006) Hardware-related complications of deep brain stimulation: a review of the published literature. Stereotact Funct Neurosurg 84:248–251
Holtzheimer PE 3rd, Mayberg HS (2010) Deep brain stimulation for treatment-resistant depression. Am J Psychiatry 167:1437–44
Kupsch A, Benecke R, Müller J, Trottenberg T, Schneider GH, Poewe W, Eisner W, Wolters A, Müller JU, Deuschl G, Pinsker MO, Skogseid IM, Roeste GK, Vollmer-Haase J, Brentrup A, Krause M, Tronnier V, Schnitzler A, Voges J, Nikkhah G, Vesper J, Naumann M, Volkmann J, Deep-Brain Stimulation for Dystonia Study Group (2006) Pallidal deep-brain stimulation in primary generalized or segmental dystonia. N Engl J Med 355:1978–90
Moro E, Allert N, Eleopra R, Houeto JL, Phan TM, Stoevelaar H, International Study Group on Referral Criteria for DBS (2009) A decision tool to support appropriate referral for deep brain stimulation in Parkinson's disease. J Neurol 256:83–88
Oh MY, Kim SH, Lang AE, Lozano AM (2002) Long-term hardware-related complications of deep brain stimulation. Neurosurgery 50:1268–1276
Schuurman PR, Bosch DA, Bossuyt PM, Bonsel GJ, von Soeren EJ, de Bie RM, Merkus MP, Speelman JD (2000) A comparison of continuous thalamic stimulation and thalamotomy for suppression of severe tremor. N Engl J Med 342:461–468
Acknowledgments
We gratefully acknowledge the excellent support in the management and follow-up of DBS patients by Caroline Mehnert (PD nurse).
Conflicts of interest
Dr. Niels Allert has received honoraria from Medtronic for lecturing and consulting services.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Allert, N., Markou, M., Miskiewicz, A.A. et al. Electrode dysfunctions in patients with deep brain stimulation: a clinical retrospective study. Acta Neurochir 153, 2343–2349 (2011). https://doi.org/10.1007/s00701-011-1187-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-011-1187-y