Abstract
Purpose
The purpose of this study is to evaluate the results of microsurgical treatment for choroid plexus tumors (CPT) in adult patients.
Methods
From 1990 to 2008, 14 patients >18 years were treated at our institution for CPT, including seven males and seven females with a mean age of 46 years. Mean follow-up was 40 months. We reviewed the respective patients' charts, operative, and follow-up notes. Telephone interviews were performed as necessary. Neurological status was determined using the Karnofsky performance index pre- and post-operatively and at last follow-up.
Results
This series includes 12 plexus papillomas (CPP) and two atypical plexus papillomas (APP). Ten tumors were located in the fourth ventricle, two tumors in the cerebellopontine angle, one growth each in the third and lateral ventricle. In 12 cases, a complete tumor resection was achieved. No recurrence was observed in these cases. Two recurrent CPP were diagnosed 11 and 25 years after the initial surgery. Brain stem infiltration prevented a complete tumor removal in one case. In the other, the degree of resection after the first operation could not be ascertained. None of the patients received adjuvant chemo- or radiotherapy. In four patients (29%), a permanent ventricular-peritoneal shunt was necessary. Three patients initially presented with a Karnofsky index of 60 or below. During follow-up, three patients (21%) never improved beyond a Karnofsky index of 60.
Conclusions
Surgery aiming radical excision is the key to successful treatment of CPP and APP in adults. Postoperative outcomes may be less than satisfactory in some patients.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
Choroid plexus tumors (CPT) are intraventricular, papillary neoplasms derived from the choroid plexus epithelium. They account for only 0.3–0.6% of all brain tumors. The WHO classification [11] distinguishes between choroid plexus papilloma WHO grade I (CPP), atypical plexus papiloma WHO grade II (APP), and choroid plexus carcinoma WHO grade III (CPC). About 80% of CPC arise in children [5, 15, 19].
CPT typically grow in areas where choroid plexus is normally found, i.e., most CPT are intraventricular tumors. Primary manifestation of a CPT in the cerebellopontine angle (CPA) near the openings of the fourth ventricle is not uncommon [5]. The choice of the surgical procedure and the treatment of hydrocephalus pose significant challenges. As a result of their deep intraventricular location, adhesion to cranial nerves in the posterior fossa and high vascularization surgical treatment may be demanding. Brain stem infiltration may prevent total extirpation in some cases. The value of adjuvant chemotherapy and radiotherapy is unclear.
A complete resection is thought to be curative in CPP. Recurrences are infrequent and the prognosis is good [13]. APP represent a novel intermediate-grade subtype of CPT. Its clinical features and treatment outcomes have not been well delineated in the literature. Recently published data from the CPT-SIOP-2000 study support the intermediate dignity of APP [20]. The event-free-survival rate was 83% in APP, but 92% in CPP and 28% in CPC.
Because of the rarity of CPT, treatment strategies are based on the results of small case series. There are only scarce contemporary data. Most reports concentrate on pediatric patients. In the present paper, we detail our experience with these rare tumors in 14 adult patients treated at our institution between 1990 and 2008.
Methods
Fourteen adult patients with a CPT were treated between 1990 and 2008 at the Department of Neurosurgery of Bonn. One patient had his primary operation performed in another institution and was referred to our institution only at the time of recurrence. Clinical, histopathological and operative reports, as well as out-patient records, were reviewed. In cases without follow-up documentation (n = 7), a telephone interview was performed in order to determine the time point of the last MRI and the radiologists' findings (recurrence vs no recurrence) and the patient's current neurological and overall condition recorded as Karnofsky performance index (KPI) [6]. Two out of seven patients were not available for an interview. In 4/7 cases, the patient himself could be interviewed. In one case, the interview was performed with the (deceased) patient's wife.
There were seven male and seven female patients, with a mean age of 46 years (years) (range 20–79, median 43 years). During the same period, we operated on four children aged 2, 4, 5, and 6 years, respectively. Mean follow-up was 58 months (range 1–214, median 30 months). Histopathological evaluations were performed according to the WHO classification [11] in n = 12 cases. In n = 2 cases, the histopathological specimens were not available for evaluation according to the WHO guidelines. The degree of tumor resection was subdivided into subtotal vs total removal, based on the operative reports and post-operative imaging. Tumor recurrence or progression was defined as a new or progressive tumor on follow-up MRI.
Results
Tumor location and histopathology findings
Tumors were located in the fourth ventricle in 10 cases, in the CPA in two cases, and one case each in the third and the left lateral ventricles (trigonum). There were 12 CPP and two APP (for a detailed overview see Table 1).
Clinical presentation
Four patients presented with symptoms and signs of hydrocephalus (three posterior fossa CPTs and one tumor in the third ventricle). Cerebellar signs were seen in 9/12 cases of posterior fossa tumors. In two patients (11%), the tumor was a coincidental finding (one case each during neuroimaging work-up for parkinsonism and for unspecific symptoms). Symptomatic occlusive hydrocephalus (n = 1) and severe cerebellar symptoms (n = 2) resulted in a KPI ≤ 60 at diagnosis in 3/14 (21%) of cases.
Surgical treatment
Tumor removal at first operation was complete in 12 patients and incomplete in one case. Two patients underwent a second and one of them a third operation for recurrent/progressive tumor: In one case, the initial tumor resection had been incomplete, and in the second case, the degree of resection after the first operation could not be ascertained.
All surgeries were performed utilizing standard approaches. Tumors located in the fourth ventricle were operated through an osteoplastic suboccipital median craniotomy with opening of the foramen magnum. Depending on the precise location of the tumors and the surgeon's preference, splitting of the inferior vermis or a telovelar approach allowed for good visualization of the growth in all cases. CPA tumors were approached through a lateral suboccipital craniotomy. The lower cranial nerves (IX and X), as well as the vertebral artery and the PICA, had to be dissected and released from the tumor. A subtemporal transcortical approach was used for the tumor in the trigonum and a supracerebellar infratentorial approach for the tumor in the dorsal part of the third ventricle. In five patients, brain stem tissue invasion was noted intra-operatively, precluding a complete resection in one case. None of the patients received adjuvant radiation or chemotherapy.
Hydrocephalus
Four patients (29%) presented with occlusive hydrocephalus, which required external CSF drainage in three cases. Permanent CSF diversion was necessary in 4/14 cases (29%). There was no case in which the recorded CSF drainage volume suggested a hypersecretory hydrocephalus.
Functional outcomes and tumor recurrence
The KPI improved by ≥20 points in two patients early after surgery, and in 5/14 patients during further follow-up. Permanent postoperative worsening by ≥20 points was seen in one case with a tumor located in the fourth ventricle. A total of 3/14 (29%) patients never improved beyond a KPI of 60 during follow-up. Reasons for lack of improvement were caudal nerves palsy in one case, brain infarction due to vasospasm (proven by angiography) in another patient, and hydrocephalus and meningitis in an elderly woman.
There was no surgical mortality. One patient with a CPP and first tumor recurrence/progression after 25 years and tumor progression another 4 years later died of unknown causes.
Tumor recurrence or progression was noted in 2/14 (14%) patients (both diagnosed with a CPP). Time to first tumor progression was 11 and 25 years. Both APP patients remain progression-free 28 and 74 months after their initial surgery. There was no documented tumor recurrence or progression after a complete resection.
Discussion
CPT are rare lesions that occur mostly in infants and young adults. Hence, many contemporary reports on CPT focus on pediatric cases [1, 3, 4, 9, 10, 12, 14]. CPT in adults may have a different etiology than their pediatric counterparts [19]. The present paper reports our institutional experience with adult patients, which accounts for the finding that the majority of the tumors were localized in the posterior fossa (12/14, 86%) and for the mostly benign histologies (CPP 12/14, 86%). Similarly, these findings are well documented in the literature. McGirr et al. reported on 19 adult cases, all of them with a CPP and all of which were located in the posterior fossa; likewise, Talacchi et al. reported on 12 adult cases, all of them presenting with a CPP. Sampath et al. analyzed 47 cases including 19 adults. Seventy four percent of the adult cases were located in the fourth ventricle or CPA and 95% were classified as CPP [7, 13, 16, 18, 19].
Outcomes
Sampath et al. [16] compared their results in pediatric vs adult patients. They pointed out that gross total excision is more feasible in adults with better outcomes in this group. These findings are certainly influenced by the more benign characters of the tumors in the adult patient group (95% CPP). In contrast, Due-Tonessen et al. [3] reported a mostly favorable outcome in their mostly pediatric patient cohort. Eighty three percent of their cases (papilloma) presented with a KPI of 100 at follow-up. A poor outcome was seen only in a patient with CPC. This successful outcome may be based on the young population combined with non-carcinoma histologies of the series.
Our data confirm that survival after CPT surgery in adults is usually good. However, functional outcomes in three of our 14 cases (21%) were not satisfactory and only 5/14 cases (36%) presented with a KPI of 100 at last follow-up. This may be a chance finding due to the small sample size. This may also reflect, in part, the risks of posterior fossa surgery, particularly in elderly patients.
A poorer outcome in surgically treated CPP was reported by Tacconi et al. [17]. An overall favorable outcome was documented in only 51.5% of their cases. This may be related to the fact that 30% of the cases were treated in the pre-microsurgical era. If these cases were excluded, the percentage of favorable outcomes rose up to 73.9% and is comparable with other reports [3, 16]. A review of the literature is illustrated in Table 2.
Factors influencing recurrence and surgical management
Total surgical excision has been identified as the key to the successful management of most CPT in various studies [7, 12, 14, 17, 19]. Our data support this view. We observed only two recurrent tumors. Tumor recurrence was diagnosed in one case following an incomplete resection (the only patient who had incomplete surgery in our series). In the other case, the operative notes and/or early postoperative neuroimaging data were lacking, i.e., the degree of resection at the first operation remained unknown. There was no documented true recurrence after complete tumor removal.
Adherence to the brain stem may prevent a complete tumor resection. Kumabe et al. reported that resection results in cases with brain stem infiltration were not satisfactory in a number of CPT cases of the fourth ventricle [8]. In contrast, invasion of brain parenchyma by nests of tumor cells did not confer a poor prognosis in the series reported by Sampath et al. [16]. Brain stem infiltration was seen in five of our cases but prevented a complete resection in one patient. This case was diagnosed with recurrent/progressive CPP 11 years after surgery.
Hydrocephalus
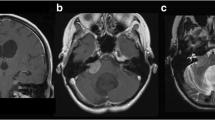
Treatment of CPT-associated hydrocephalus is an important aspect of surgical management as reported in several series [2, 3, 14, 17]. Obstruction of the CSF pathways and hypersecretion of CSF by the tumor are causes that can be treated by tumor removal. However, patients may develop persistent hydrocephalus. Due-Tonnessen et al. reported that 50% of their 16 CPT patients required CSF shunting after tumor resection. In contrast, in the series of Pencalet et al., permanent hydrocephalus was diagnosed in only 24% of their patients. Tacconi et al. [17] reported that, in 17 out of 23 cases (74%), the hydrocephalus resolved after insertion of a ventricular drain during tumor surgery, which was kept in place for 2–3 days (Fig. 1). Hydrocephalus requiring permanent shunting was seen in four cases (29%) in our series, including two cases with slow onset of symptoms after surgery, who did not have a prior external CSF drainage. Nevertheless, the overall rate of patients requiring CSF shunting procedures leaves room for improvement.
a CT of a 35-year-old woman who presented with headache, nausea and vomiting, gait disturbance, and diplopia. An infratentorial tumor with calcification resulting in obstructive hydrocephalus was diagnosed. An MRI obtained after urgent insertion of an external ventricular drain showed a highly vascularized well-defined tumor located in the fourth ventricle. b Gadolinium enhanced axial and c coronal T1 weighted scans. The histopathological diagnosis was choroid plexus papilloma WHO grade I (CPP)
Conclusions
Surgery is the key to the successful management of CPTs in adults. A complete removal of the tumor will likely cure most patients. A significant number of patients require shunting procedures after CPT surgery, and postoperative functional outcomes can be less than satisfactory in some cases.
References
Chow E, Reardon DA, Shah AB, Jenkins JJ, Langston J, Heideman RL, Sanford RA, Kun LE, Merchant TE (1999) Pediatric choroid plexus neoplasms. Int J Radiat Oncol Biol Phys 44:249–254
Di Rocco C, Iannelli A (1997) Poor outcome of bilateral congenital choroid plexus papillomas with extreme hydrocephalus. Eur Neurol 37:33–37
Due-Tonnessen B, Helseth E, Skullerud K, Lundar T (2001) Choroid plexus tumors in children and young adults: report of 16 consecutive cases. Childs Nerv Syst 17:252–256
Gupta N (2003) Choroid plexus tumors in children. Neurosurg Clin N Am 14:621–631
Janisch W, Staneczek W (1989) Primary tumors of the choroid plexus. Frequency, localization and age. Zentralbl Allg Pathol 135:235–240
Karnofsky D, Burchenal J (1949) The clinical evaluation of chemotherapeutic agents in cancer. In: MacLeod C (ed) Evaluation of chemotherapeutic agents. Columbia Univ Press, p 196
Krishnan S, Brown PD, Scheithauer BW, Ebersold MJ, Hammack JE, Buckner JC (2004) Choroid plexus papillomas: a single institutional experience. J Neurooncol 68:49–55
Kumabe T, Fujimura M, Jokura H, Tominaga T (2008) Surgical treatment for choroid plexus tumors in the fourth ventricle: brain stem infiltration hinders total extirpation. Neurosurg Rev 31:165–172, discussion 172
Kumar R, Singh S (2005) Childhood choroid plexus papillomas: operative complications. Childs Nerv Syst 21:138–143
Levy ML, Goldfarb A, Hyder DJ, Gonzales-Gomez I, Nelson M, Gilles FH, McComb JG (2001) Choroid plexus tumors in children: significance of stromal invasion. Neurosurgery 48:303–309
Louis DN, Ohgaki H, Wiestler OD, Cavenee WK (2007) WHO classification of tumours of the central nervous system. International Agency for Research on Cancer (IARC), Lyon
McEvoy AW, Harding BN, Phipps KP, Ellison DW, Elsmore AJ, Thompson D, Harkness W, Hayward RD (2000) Management of choroid plexus tumours in children: 20 years experience at a single neurosurgical centre. Pediatr Neurosurg 32:192–199
McGirr SJ, Ebersold MJ, Scheithauer BW, Quast LM, Shaw EG (1988) Choroid plexus papillomas: long-term follow-up results in a surgically treated series. J Neurosurg 69:843–849
Pencalet P, Sainte-Rose C, Lellouch-Tubiana A, Kalifa C, Brunelle F, Sgouros S, Meyer P, Cinalli G, Zerah M, Pierre-Kahn A, Renier D (1998) Papillomas and carcinomas of the choroid plexus in children. J Neurosurg 88:521–528
Rickert CH, Paulus W (2001) Tumors of the choroid plexus. Microsc Res Tech 52:104–111
Sampath S, Nitin G, Yasha TC, Chandramouli BA, Devi BI, Kovoor JM (2008) Does choroid plexus tumour differ with age? Br J Neurosurg 22:373–388
Tacconi L, Delfini R, Cantore G (1996) Choroid plexus papillomas: consideration of a surgical series of 33 cases. Acta Neurochir (Wien) 138:802–810
Talacchi A, De Micheli E, Lombardo C, Turazzi S, Bricolo A (1999) Choroid plexus papilloma of the cerebellopontine angle: a 12 patient series. Surg Neurol 51:621–629
Wolff JE, Sajedi M, Brant R, Coppes MJ, Egeler RM (2002) Choroid plexus tumours. Br J Cancer 87:1086–1091
Wrede B, Hasselblatt M, Peters O, Thall PF, Kutluk T, Moghrabi A, Mahajan A, Rutkowski S, Diez B, Wang X, Pietsch T, Kortmann RD, Paulus W, Jeibmann A, Wolff JE (2009) Atypical choroid plexus papilloma: clinical experience in the CPT-SIOP-2000 study. J Neurooncol 95(3):383–392
Conflicts of interest
None.
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The group from Bonn provided us with an excellent review of their surgical experience on CPT. This is a contemporary series including a relatively large number of adult patients affected by choroid plexus papillomas and a few even rarer cases of atypical plexus papillomas. The take-home message from this paper is straightforward and convincingly discussed: aggressive surgery is the key to successful treatment of such tumors in adults. In this respect, the information that patients with atypical plexus papillomas remain progression-free at 28 and 74 months after their initial surgery emphasizes the role of an operative strategy aimed at complete resection. Nevertheless, the authors do not underscore the problems inherent to this difficult pathology, including post-operative shunt-dependent hydrocephalus in almost one third of cases and a less-than-optimal functional outcome in one fourth. This series will serve as a reference for future investigations on this rare group of tumors.
Domenico d’Avella
Giorgio Perilongo
Padova, Italy
Rights and permissions
About this article
Cite this article
Boström, A., Boström, J.P., von Lehe, M. et al. Surgical treatment of choroid plexus tumors. Acta Neurochir 153, 371–376 (2011). https://doi.org/10.1007/s00701-010-0828-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-010-0828-x