Abstract
Purpose
Visual failure due to optic nerve compression is a common indication for decompressive surgery. Most data only refer to the odds of improvement, deterioration or remaining the same. However, patients frequently wish to know more detail about the outcomes of surgery. Our aim was to assess the visual outcome from optic nerve decompression for visual failure in detail in order to help counsel patients pre-operatively.
Methods
Sixty-eight patients undergoing 71 operations to decompress 87 optic nerves between 1991 and 2007 were identified. Thirty-four decompressions were performed via a transzygomatic and 37 via a transbasal approach. Fifty-two patients had meningiomas, 3 pituitary adenomas, 3 craniopharyngiomas, 3 chordomas, 2 adenocarcinomas, 2 fibrous dysplasia, 1 schwannoma, 1 granular pituitary tumour and 1 olfactory neuroblastoma. Visual acuity and fields were recorded pre-operatively, immediately post-operatively, at first follow-up and at most recent follow-up.
Results
Forty-three eyes (49.4%) experienced an improvement in either acuity or fields. Twenty-four (27.5%) were unchanged and 20 (22.9%) deteriorated. Average improvement was 0.88 Snellen lines (logMAR 0.13). Improvement was seen between immediate post-operative acuity and first follow-up in 52%, but 22% suffered a late deterioration after 1 year. There was no relationship between age, duration of symptoms, pathology, approach or redo surgery and visual outcome. There was a complex relationship between pre-operative visual acuity and post-operative improvement and outcome. Better pre-operative acuity predicted better outcome and greater odds of improvement, although patients with poor pre-operative vision had a greater average magnitude of improvement.
Conclusions
Patients experience significant benefit from optic nerve decompression irrespective of pre-operative visual status. Although early decompression is desirable, good results can still be obtained in patients with severe visual failure. Detailed data on visual outcome can help counsel patients pre-operatively to aid decision-making and set expectations.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Visual failure due to optic nerve compression is one of the most distressing symptoms experienced by patients with anterior skull base tumours. As a result of this, it is a common indication for complex neuro- and craniofacial surgery.
Many approaches have been described for such surgery depending on the pathology and location of the offending lesion. There is a growing body of literature describing visual outcomes from optic nerve decompression for suprasellar meningiomas [3, 5–7, 11, 16, 21, 26, 28, 30, 31, 32, 39]. Outcomes from surgery for meningiomas arising from other locations, such as the sphenoid wing [2, 27, 34] and olfactory groove [17], and for craniopharyngiomas [12, 37, 38], have also been reported. These studies have helped to establish the rates of visual recovery, which range between 22.5 and 80% [11, 26]. It is also recognised that many patients experience deterioration in their vision following decompressive surgery. This complication occurs following 11–25% of decompressions [16, 26, 35].
Most of these reports relate to classical pterional approaches. The literature on extensive anterior approaches is more limited [14], with our previous study forming one of the larger series reporting visual outcomes [35]. Other, rarer lesions, such as fibrous dysplasia and adenocarcinoma are well recognised, but descriptions of post-operative vision consist of case reports or short case series [15, 29]. It therefore remains unclear what the prospects are for future vision in these cases and how this compares with meningioma surgery.
In view of the fact that most meningioma series to date lack detail on visual outcome (only reporting on the odds of improvement or deterioration in vision), and the small numbers of on non-meningioma cases in the literature, we find it difficult to answer many of the questions posed by our patients. Therefore, we report the detailed visual outcomes of optic nerve decompression by either orbitozygomatic or transbasal approaches. Our aim was to describe how vision evolves over time, determine the magnitude as well as the odds of change, and identify predictors of improvement. We also sought to identify how these results varied with different degrees of pre-operative impairment. By putting these in a clinically meaningful context we hope to provide valuable information for counselling patients.
Materials and methods
Patients
We performed a retrospective case note review of patients undergoing optic nerve decompression via a combined craniofacial approach in the Wessex Neurological Centre in Southampton between 1991 and 2007. Only patients with charted pre- and post-operative visual fields and acuities, as well as a pre-operative deficit, were included.
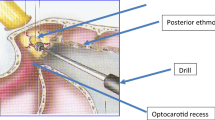
All operations were performed via either a traditional transzygomatic or a transbasal approach. We have previously described the details of both of these approaches [19, 22]. All procedures were performed by a combined maxillofacial and neurosurgical team.
Vision
All patients had visual fields and acuities charted pre- and post-operatively. Post-operative visual acuities and fields were divided into three groups: those performed as an in-patient (within 7 days of surgery), those performed at the first out-patient appointment (3 months), and those performed at late follow-up (at least 12 months and up to 97 months following surgery).
Visual acuities were recorded on a Snellen chart at 6 m with correction. A change in vision was defined as an improvement or deterioration of one Snellen line. Vision worse than 6/60 was recorded as finger counting, hand movement, light perception and no light perception. For the purposes of analysis each of these were considered as a Snellen line.
For statistical analysis all Snellen values were converted to logMAR following established practices [25]. For vision worse than 6/60 logMAR values were ascribed as estimated by the Freiburg Visual Acuity Test FrACT [33]. All Snellen and logMAR equivalents are demonstrated in Table 1.
There was a planned subgroup analysis of eyes that were blind, those that were not blind but did not meet the standards for driving, and those that did meet the standards for driving. These terms usually refer to binocular vision, but for the purposes of analysis it was useful to stratify individual eyes into mild, moderate and severe visual impairment and are practical terms in which patients perceive their deficits and assess surgery. Although United Kingdom requirements for visual acuity for driving are not defined in terms of Snellen lines, it is usually approximated to 6/12 (logMAR 0.3) [9]. The World Health Organisation definition of blindness of 3/60 or worse was used [20], although legal definitions of blindness do vary.
Visual fields were recorded by Goldman perimetry. A change was defined as an expansion or constriction of 15 degrees or more in at least three sectors (one quadrant).
Statistics
Unless stated, all statistical analyses were performed using logMAR values. Correlations were calculated by linear regression and expressed as Pearson’s coefficient. Differences in mean were calculated using a two-tailed Student’s t test. Differences between categorised groups were calculated using the Chi-squared test. Any association with a probability value <0.05 was considered statistically significant.
Results
Patients
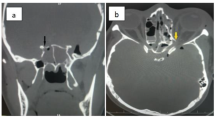
We identified 68 patients who had optic nerve decompression with documented visual failure between 1991 and 2007. Fifty-two patients had meningiomas, 3 pituitary adenomas, 3 craniopharyngiomas, 3 chordomas, 2 adenocarcinomas, 2 fibrous dysplasia, 1 granular pituitary tumour, 1 schwannoma and 1 olfactory neuroblastoma. Twenty-two meningiomas were of the sphenoid wing, 17 suprasellar, 11 subfrontal and 2 petroclival with large anterior extension (Table 2). One meningioma was atypical.
These 68 patients underwent 71 operations; 34 via a transzygomatic approach and 37 via a transbasal approach. Sixteen operations were performed to decompress both optic nerves, giving a total of 87 nerves decompressed. Of these, 76 were primary decompressions and 11 redo surgeries.
The average age of patients was 52.0 years (range 5–79 years). The average duration of visual deficit was 26.1 months (range 0.25–216 months). Forty-seven decompressions were of the right optic nerve and 40 of the left. The average follow-up was 24.4 months (range 4–97 months). There were no significant differences in age, sex, or visual function between the approaches (P = 0.464, P = 0.529, P = 0.822), pathologies (P = 0.365, P = 0.313, P = 0.911) or primary and redo surgery (P = 0.767, P = 0.292, P = 0.228).
Visual acuity
Seventy-nine of the 87 eyes had a visual acuity worse than 6/6 pre-operatively. The median pre-operative acuity was 6/24 (mean 1.13 logMAR) and the median post-operative acuity was 6/18 (mean 1.00 logMAR). The average change was 0.89 Snellen lines (0.13 logMAR). The visual acuity of 40 eyes (46.0%) improved, 27 (31.0%) were unchanged, and 20 (23.0%) deteriorated. Of the 40 improved eyes, the average change was 3.3 Snellen lines (0.87 logMAR). Of the 20 deteriorated eyes, the average change was 2.8 Snellen lines (0.71 logMAR; Fig. 1).
Visual fields
Fifty-one of the 78 patients with Goldman perimetry pre- and post-operatively had a pre-operative field deficit. The visual fields of 22 eyes (28.2%) improved, 43 (55.1%) were unchanged, and 13 (16.7%) deteriorated (Table 3).
The number of eyes that experienced an improvement in either acuity or fields was 43 (49.4%). Twenty-four (27.5%) were unchanged and 20 (22.9%) deteriorated.
Age and symptom duration
There was no correlation between age and pre-operative acuity (r = 0.074, P = 0.493), or post-operative change in vision (r = 0.147, P = 0.172; Fig. 2a). The duration of visual symptoms (time from the initial onset of visual symptoms to surgery) showed no correlation with pre-operative acuity (r = 0.021, P = 0.853), or post-operative change in vision (r = 0.097, P = 0.400; Fig. 2b).
Pre-operative acuity
The relationships between pre-operative acuity and post-operative acuity and improvement are demonstrated in Fig. 3. The pre-operative acuity correlated with post-operative acuity (r = 0.656, P < 0.001). Pre-operative acuity also correlated with the magnitude of the post-operative change in vision (r = 0.301, P = 0.004). Linear regression of post-operative change in vision against pre-operative acuity yielded an x intercept at logMAR 0.64 (Snellen 6/24) with gradient 0.26 (P = 0.005). This represents the pre-operative visual acuity at which on average there is no change in acuity post-operatively.
The numbers of eyes meeting criteria for driving or blindness that improved or deteriorated are demonstrated in Table 4. There was no statistical difference in the likelihood of improving or deteriorating between eyes that met driving requirements and those that did not (χ2 = 2.848, P = 0.241). There was a difference between those registered blind and those who were not (χ2 = 31.815, P < 0.001). The numbers of affected eyes in patients who were driving or who were blind post-operatively is shown in Table 5.
Approach, pathology and redo surgery
Although age and symptom duration were statistically the same in the transzygomatic and transbasal groups, there was a significantly higher number of meningiomas in the transzygomatic group (χ2 = 9.221, P = 0.002). There was no difference in pre-operative acuity (P = 0.821), post-operative acuity (P = 0.694) or magnitude of change (P = 0.809) in the t test, and no difference in the odds of improvement, remaining the same or deterioration with the Chi-squared test (χ2 = 0.277, P = 0.877).
The patients were divided into two groups according to pathology: meningioma and non-meningioma. There was no difference in pre-operative acuity (P = 0.911), post-operative acuity (P = 0.185) or magnitude of change (P = 0.071) with the t test, and no difference in the odds of improvement, remaining the same or deterioration with the Chi-squared test (χ2 = 3.476, P = 0.176).
Eleven decompressed eyes had undergone previous surgery. Amongst these eyes there was no difference in pre-operative acuity (P = 0.228), post-operative acuity (P = 0.582) or magnitude of change (P = 0.508) in the t test, and no difference in the odds of improvement, remaining the same or deterioration in the Chi-squared test (χ2 = 0.184, P = 0.912).
Time course of visual change
Charted visual acuities as in-patient and at first follow-up were available for 25 decompressed eyes. Thirteen eyes (52%) continued to improve after discharge, although one eye (4%) deteriorated. On average there was an improvement of 1.8 Snellen lines (logMAR 0.48), or 3.6 Snellen lines (logMAR 0.90) in the subgroup of eyes that improved. The immediate post-operative vision was also subdivided into driving, not driving and not blind, and blind, and the outcome of these are demonstrated in Table 6.
There were 50 eyes with more than 12 months’ follow-up. Of these, 11 (22%) deteriorated and none improved after the first year. On average, eyes deteriorated by 0.5 Snellen lines (logMAR 0.14), or 2.2 Snellen lines (logMAR 0.43) in the subgroup that deteriorated.
Discussion
We report the detailed visual outcomes of a large series of optic nerve decompressions. Although direct comparisons can be difficult to make due to the heterogeneous pathology and approaches, there are several reasons to believe it is representative. First, rates of recovery are similar to those reported in other series. Second, within this series there are homogeneous subgroups that in themselves are large enough to represent a significant case series. Third, all the subgroups irrespective of pathology or approach have the same results provided optic nerve decompression was achieved.
Overall, 49.4% improved, 27.5% were unchanged and 22.9% deteriorated. This is in keeping with reports for both suprasellar and sphenoid wing meningiomas. The figures quoted vary considerably (Table 7). This is likely to be not only due to the surgeon, approach and case selection, but also to study design and outcome measures.
Visual scales
A significant problem when making comparisons between studies is in the use of different visual acuity scales. The Snellen chart has been the universally accepted visual scale since its inception by the Dutch ophthalmologist Herman Snellen in 1862. It has therefore been included in this analysis to give clinical meaning to results. One limitation of this scale is that it follows an arithmetic and not geometric progression. This is an impediment to statistical analysis as it makes averaging techniques invalid [18]. LogMAR is a logarithmic scale, developed to address some of these issues [4], and is now widely used in research. We therefore also employed this scale. Although the use of two scales may appear to cause confusion, it makes statistical analysis possible while producing results in clinically meaningful terms. It is also worth noting that similar results were obtained through both methods of analysis.
Vision poorer than 6/60 poses special problems [24]. By most definitions this is blindness. Many neurosurgical studies have considered them all in one category. However, even if outcomes worse than 6/60 seem disappointing, differences between categories can actually make a significant functional difference to patients [13]. This is particularly so if the contralateral eye also has poor function and cannot compensate.
Although attempts have been made to approximate finger counting and hand movements to both Snellen and logMAR charts [18], light perception and no light perception pose further problems. These do not refer to angles of resolution, which are intrinsic to all acuity scales. Fortunately, recent low visual acuity research with the Freiburg Visual Acuity Test (FrACT) has produced robust estimates of logMAR equivalents, which we have used allowing analysis of all grades of vision [33].
Visual outcome
Although it is encouraging to see a large percentage of patients improving, the magnitude of improvement varies. This detail is less frequently reported and there is rarely much differentiation between a small improvement and normalisation of vision, despite its clinical relevance to the patient. In our series the average change was 0.89 Snellen lines (7% improvement in Snellen lines), and 3.3 Snellen lines (47% improvement in Snellen lines) in the subgroup of 40 patients with improved acuity. Thus, although a large number of patients experience an improvement, not all achieve normality (31/87 or 35.6% achieved an acuity of 6/6 or better).
These data will help to counsel patients pre-operatively. However, there are little data in the literature to guide what happens to vision between the immediate post-operative phase and late follow-up, despite being of great interest to patients. We show that visual change is not limited to the peri-operative period. In the initial months there is a significant improvement in acuity, often following a small deterioration immediately peri-operatively, although severe immediate deterioration is rarely followed by any improvement, as has been observed elsewhere [30].
Unfortunately, this visual improvement is not always maintained and in the long term 22% of patients suffered a significant deterioration. This was excluding deterioration due to recurrence and not related to post-operative radiotherapy or redo surgery. It can only be postulated that this relates to a reduced redundancy within the optic nerve and hence increased sensitivity to any future neuronal loss [35].
Pathology and approach
Previous reports have suggested that visual outcome following trans-cranial approaches depends on tumour location [3, 27]. It is surprising that we found no such relationship. Nor did we find a relationship with pathology or approach. We therefore believe the most important factor relating to post-operative improvement is the decompression itself—that tumour location does not influence visual outcome directly, but only through the adequacy of that decompression. This supports the traditional surgical view that approach should be tailored to the lesion to achieve maximal decompression with minimal risk and the approach in itself does not determine outcome. This will have to be evaluated against new transsphenoidal–transethmoidal–transnasal approaches being used [8, 10, 23], when larger series reporting on visual outcome are available.
Transsphenoidal procedures were excluded from this study. We felt these represented a significantly different group, as soft pituitary tumours were liable to lead to better debulking, without the need to visualise and potentially injure the optic nerve. This hypothesis is supported by better results reported in other studies [36]. Unfortunately, the number of pituitary adenomas in our series decompressed trans-cranially is too small to draw conclusions.
Other groups have found that the plane between the nerve and tumour (and measures of this such as the presence of the arachnoid plane and nerve encasement) correlates with visual outcome [5, 11, 26, 28, 39] and that redo surgery is associated with worse outcome [27].
We believe that the risk of post-operative deterioration is largely determined by vascular injury, which itself is related to the adequacy of the plane between the nerve and the tumour. We therefore expected some subgroups with different degrees of adherence to the optic nerve to have higher rates of post-operative deterioration. Redo surgery was one such group. We did not observe any difference, however. We believe this is either due to the small sample size or as a result of our practice to be more conservative in our decompression in the face of adherent tumour at redo surgery and that if we pursued more aggressive surgery in these cases we may have had poorer results. Our data, therefore, suggest that although it requires careful judgement, the results from redo surgery can be satisfying and indeed similar to those obtained after primary surgery.
A number of studies have found that other intra-operative observations predict worse outcome. These include encased anterior cerebral arteries [16], vertical growth [28], severe oedema [28] and cavernous sinus involvement [27]. These are likely to reflect the surgical difficulty in achieving adequate decompression rather than the intrinsic capacity for recovery of the nerve itself. This is supported by previous studies demonstrating lower rates of recovery associated with subtotal removal [28]. However, what constitutes adequate decompression is unclear, as other studies have found no difference between complete and incomplete removal [30].
In our experience one of the best predictors of visual outcome is the appearance of the optic nerve at surgery. This is in keeping with reports that an atrophic optic nerve at surgery predicts poor outcome [5] and unlike other factors is likely to reflect the degree of injury already sustained by the optic nerve and its capacity to regain function.
Age and duration of symptoms
So far, the main associations with outcome are intra-operative findings. These are not available pre-operatively. For pre-operative counselling we considered factors such as age, symptom duration and pre-operative acuity. The literature is conflicting on all three of these issues (Table 7).
Some papers suggest that age predicts a poor recovery. We found that it did not. Although a bias could have been introduced if only the fittest elderly patients with the most favourable tumours were offered surgery, we excluded any relationship between age and pre-operative acuity. Therefore, in the absence of any other associations with outcome, this is unlikely.
We also found no relationship to the duration of symptoms. One reason for conflicting reports on this subject may be due to the definition of the term. At one extreme, this could be considered to start from the first onset of any visual symptom, and at the other extreme, from when the symptoms reached their pre-operative level. We opted for the former, as this was relatively easier to obtain and more reproducible. However, it could be argued that if outcome is related to the severity of deficit in acuity, then it may also be related to the duration of the worst deficit and not the duration of any deficit. We can therefore only conclude that outcome is not related to the time since the first onset of visual failure. Although there could still be a relationship with the duration of the most severe symptoms, clinically this can be difficult to define and probably not relevant.
Pre-operative acuity
The relationship of outcome to pre-operative visual acuity is complex. Previously, we have reported that there is no relationship between pre-operative acuity and the change in acuity achieved [35]. However, in the continuation of our series there is a clear relationship between pre- and post-operative acuity, with patients with good vision faring best post-operatively. This demonstrates the dangers of the interpretation of small numbers.
However, when viewed as the magnitude of improvement, the picture is different again. We observed that patients with worse vision, on average, had a larger improvement in vision than those with good vision. This can easily be explained by the fact that patients with worse vision simply have more to gain. We therefore looked at the rates of improvement in subgroups with good, moderate or poor vision. This was more in keeping with the accepted view that patients with worse vision are less likely to improve. However, this was only seen amongst patients registered blind. Patients with pre-operative acuities better than 6/60, all had the same frequency of improvement, as has been observed in some other studies [27].
While this is very useful for patient information, our data also provide useful information regarding the timing of surgery. It is clear we should be operating before blindness is reached (although we should not be deterred from surgery if patients present severely impaired, as significant and worthwhile improvements were seen in our series). The relationship between pre- and post-operative acuity suggests that we should operate at the earliest possible stage, before there is significant visual deterioration, as this will result in the best visual outcomes. However, this ignores the risk of visual deterioration. If we consider the ideal time to operate to be when the average improvement (as opposed to the probability of improvement) is larger than the average deterioration, then linear regression demonstrates that this is reached at logMAR 0.64 or a Snellen equivalent of 6/24.
This should, of course, not be used as a criterion for surgery in itself, as this does not take into account the natural history of the disease. Many of these patients face inevitable progression of their visual symptoms. Therefore, even a small immediate deterioration following surgery may be better than a severe progressive deficit. Nor does the question take into account the plenitude of patient and tumour factors that have bearing on this decision. We may have demonstrated that age, duration of symptoms, pathology or approach do not independently influence outcome, but this does not mean that they do not have an influence on decision-making. Many of these factors are related to the progression of symptoms. Thus, although they do not influence the visual outcome following surgery, they do influence what surgery is measured against—conservative management, or in some cases, radiosurgery.
Radiosurgery represents an interesting new option. Traditionally, it was not considered due to the risk to the optic apparatus. There are a number of recent reports on safe treatment with increasingly conformal therapy [1]. While these do not appear to provide much relief from visual symptoms (16%) they do provide some tumour control with low complication rates (6%) and perhaps provide a good option for patients before visual disturbance has occurred where the risks of surgery are felt to be unacceptable.
Ultimately, it comes down to how patients perceive their risk. Should they choose an immediate risk of deterioration with the best overall outcome, or should they wish to wait until the chances of improving from surgery are better than the chances of deterioration. These are choices that can only be made after careful consultation between patient and surgeon.
References
Adler JR, Gibbs IC, Puataweepong P, Chang SD (2006) Visual field preservation after multisession cyberknife radiosurgery for perioptic lesions. Neurosurgery 59(2):244–254
Al-Mefty O (1990) Clinoidal meningiomas. J Neurosurg 73:840–849
Andrews BT, Wilson CB (1988) Suprasellar meningiomas: the effect of tumor location on postoperative visual outcome. J Neurosurg 69:523–528
Bailey IL, Lovie JE (1980) The design and use of a new near-vision chart. Am J Optom Physiol Opt 57(6):378–387
Bassiouni H, Asgari S, Stolke D (2006) Tuberculum sellae meningiomas: functional outcome in a consecutive series treated microsurgically. Surg Neurol 66:37–45
Chi JH, McDermott MW (2002) Tuberculum sellae meningiomas. Neurosurg Focus 14(6):1–6
Chicani CF, Miller NR (2003) Visual outcome in surgically treated suprasellar meningiomas. J Neuroophthalmol 23(1):3–10
Cook SW, Smith Z, Kelly DF (2004) Endonasal transsphenoidal removal of tuberculum sellae meningiomas: technical note. Neurosurgery 55(1):239–244
Currie Z, Bhan A, Pepper I (2000) Reliability of Snellen charts for testing visual acuity for driving: prospective study and postal questionnaire. BMJ 321(7267):990–992
De Divitiis E, Cavallo LM, Cappabianca P, Esposito F (2007) Extended endoscopic endonasal transsphenoidal approach for the removal of suprasellar tumours. II. Neurosurgery 60(1):46–58
Fahlbusch R, Schott W (2002) Pterional surgery of meningiomas of the tuberculum sellae and planum sphenoidale: surgical results with special consideration of ophthalmological and endocrine outcomes. J Neurosurg 96:235–243
Fahlbusch R, Honegger J, Paulus W, Huk W, Buchfelder M (1999) Surgical treatment of craniopharyngiomas: experience with 168 patients. J Neurosurg 90:237–250
Faye EE (1976) Clinical low vision. Little, Brown, Boston
Feiz-Erfan I, Han PP, Spetzler RF et al (2005) The radical transbasal approach for resection of anterior and midline skull base lesions. J Neurosurg 103:485–490
Giosis M, Bigioli F, Guareschi M, Frigerio A, Mortini P (2005) Fibrous dysplasia of the orbital region: current clinical perspectives in ophthalmology and cranio-maxillofacial surgery. Ophthal Plast Reconstr Surg 22(5):383–387
Goel A, Muzamdar D, Desai KI (2002) Tuberculum sellae meningioma: a report on management on the basis of a surgical experience with 70 patients. Neurosurgery 51(6):1358–1364
Hentschel SJ, DeMonte F (2003) Olfactory groove meningiomas. Neurosurg Focus 14(6):1–5
Holloday JT (2004) Visual acuity measurements. J Cataract Refract Surg 30:287–290
Honeybull S, Neil-Dwyer G, Evans BT, Lang DA (1997) Transzygomatic approach: an anatomical study. Br J Oral Maxillofac Surg 35:334–340
ICD-10 (1990) International statistical classification of diseases and related health problems: tenth revision, 2nd edn. WHO, Geneva
Jallo GI, Benjamin V (2002) Tuberculum sellae meningiomas: microsurgical anatomy and surgical technique. Neurosurgery 51(6):1432–1440
Lang DA, Honeybull S, Neil-Dwyer G, Evans BT, Weller RO, Gill J (1999) The extended transbasal approach: clinical applications and complications. Acta Neurochir (Wien) 141:579–585
Laufer I, Anand VK, Schwartz TH (2007) Endoscopic, endonasal extended approach for resection of suprasellar lesions. J Neurosurg 106:400–406
Lim LT, Frazer DG, Jackson AJ (2007) Clinical studies: visual acuities beyond Snellen. Br J Ophthalmol 92:153
Lovie-Kitchen JE (1988) Validity and reliability of visual acuity measurements. Ophthalmic Physiol Opt 8:363–370
Margalit NS, Lesser JB, Moche J, Sen C (2003) Meningiomas involving the optic nerve: technical aspects and outcomes for a series of 50 patients. Neurosurgery 33(3):523–533
Nakamura M, Roser F, Jacobs C, Vorkapic P, Samii M (2006) Medial sphenoid wing meningiomas: clinical outcome and recurrence rate. Neurosurgery 58(4):626–639
Pamir MN, Özduman K, Belirgen M, Kilic T, Özec MM (2005) Outcome determinants of pterional surgery for tuberculum sellae meningiomas. Acta Neurochir (Wien) 147:1121–1130
Papay FA, Morales L, Flaharty P et al (1995) Optic nerve decompression in cranial base fibrous dysplasia. J Craniofac Surg 6(1):5–10
Park CK, Jung HW, Yang SY, Seol HJ, Paek SH, Kim DG (2006) Surgically treated tuberculum sellae and diaphragma sellae meningiomas: the importance of short-term visual outcome. Neurosurgery 59(2):238–243
Puchner MJA, Fisher-Lampsatis RCM, Hermann HD, Freckman N (1998) Suprasellar meningiomas—neurological and visual outcome at long term follow-up in a homogeneous series of patients treated microsurgically. Acta Neurochir (Wien) 140:1231–1238
Schick U, Hassler W (2005) Surgical management of tuberculum sellae meningiomas: involvement of the optic canal and visual outcome. J Neurol Neurosurg Psychiatry 76:977–983
Schulze-Bonsel K, Feltgen N, Burau H, Hansen L, Bach M (2006) Visual acuities “hand motion” and “counting fingers” can be quantified with the Freiburg visual acuity test. Invest Ophthalmol Vis Sci 47:1236–1240
Shrivastava RK, Sen C, Costantino PD, Rocca RD (2005) Sphenoorbital meningiomas: surgical limitations and lessons learned in their long-term management. J Neurosurg 103:491–497
Sleep TJ, Hodgkins PR, Honeybul S, Neil-Dwyer G, Lang D, Evans B (2003) Visual function following neurosurgical optic nerve decompression for compressive optic neuropathy. Eye 17:571–578
Suri A, Narang KS, Sharma BS, Mahapatra AK (2008) Visual outcome after surgery in patients with suprasellar tumours and preoperative blindness. J Neurosurg 108:19–25
Van Effentere R, Boch AL (2002) Craniopharyngioma in adults and children: a study of 122 surgical cases. J Neurosurg 97:3–11
Yaşargil MG, Curcic M, Kis M, Siegenthaler G, Teddy PJ, Roth P (1990) Total removal of craniopharyngiomas. J Neurosurg 73:3–11
Zevgaridis D, Medele RJ, Müller A, Hischa AC, Steiger HJ (2001) Meningiomas of the sellar region presenting with visual impairment: impact of various prognostic factors on surgical outcome in 62 patients. Acta Neurochir (Wien) 143:471–476
Conflicts of interest
None.
Disclosure of funding
None.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Bulters, D.O., Shenouda, E., Evans, B.T. et al. Visual recovery following optic nerve decompression for chronic compressive neuropathy. Acta Neurochir 151, 325–334 (2009). https://doi.org/10.1007/s00701-009-0192-x
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-009-0192-x