Abstract
Endoscopic optic nerve decompression is a highly effective and reliable approach for patients with select cases of optic neuropathy. It reduces the hydrostatic pressure and helps in relieving the compressive forces within the intracanalicular portion of the optic nerve consequently preserving and arresting the deterioration of vision. The advantages of the endoscopic approach over other procedures include preservation of olfaction, quick recovery, lack of external scars and less morbidity. The objective of the study is to assess the surgical outcome of endoscopic optic nerve decompression in patients with traumatic and atraumatic optic neuropathy. The case records of consequent patients attending ENT department with defective vision due to traumatic and atraumatic causes were reviewed. The outcome was measured in terms of improvement in visual acuity by log MAR scale. Among the 14 patients studied, 57% were females and the median age of presentation was 33 years. As compared to preoperative baseline visual acuity, the overall improvement was achieved in 11 patients, with an effective rate of 78.5% postoperatively. Patients presenting with no light perception and residual vision had significant improvement in visual acuity after surgery. Trans-nasal endoscopic surgery helps in decompressing the optic nerve with proper exposure of the orbital apex and optic canal without any intracranial or intra-orbital complications. Further, being a minimally invasive procedure has great advantage in cases of optic neuropathy.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Compression of the optic nerve results in conduction block and focal demyelination, which leads to optic neuropathy and the condition is reversible to some extent by surgery or medical treatment. [1] The common modalities of managing compressive optic neuropathy include observation, corticosteroid therapy and optic nerve decompression. The main goal of surgery is to relieve the compressive forces within the intracanalicular portion of the optic nerve. The surgical outcome in patients having optic neuropathy is measured in terms of significant improvement in visual acuity. Optic nerve decompression is feasible for patients reporting indirect traumatic optic neuropathy for improved outcomes. The prognosis of patients with direct traumatic optic neuropathy is poor due to the nerve being cut or involving a fracture of the optic canal. [2].
Endoscopic optic nerve decompression is a highly reliable, delicate and minimally invasive procedure in managing patients with optic neuropathy. In comparison to the transcranial method, the transnasal endoscopic approach provides excellent visualisation of the orbital apex and optic canal, but with a compromise on trauma site exposure. [3] The advantages of the endoscopic approach over other procedures include preservation of olfaction, quick recovery, lack of external scars and less morbidity. Crucial factors like the severity of the injury, visual acuity before surgery, type of injury, and the time interval between trauma and intervention influence the outcome of optic nerve decompression. [4].
The present study was carried out with the objective to assess the surgical outcome of endoscopic optic nerve decompression in patients reporting with optic neuropathy due to traumatic and atraumatic causes.
Materials and Methods
The study was conducted in the Upgraded Institute of Otorhinolaryngology, Rajiv Gandhi Government General Hospital, Chennai, Tamil Nadu, from August 2021 to January 2023. The descriptive data was collected secondarily from the patient records maintained in the hospital and review was done. A consecutive number of fourteen patients presenting with defective vision following head trauma and sino-nasal diseases were included in the study. Patients with extensive head injury, visual defects secondary to congestive eye disorders and retinal degenerative disorders were excluded from the study. The study was approved by the Institutional Ethical Committee bearing registration number 28082023.
All patients presenting with defective vision underwent complete ophthalmologic examination including visual acuity of both eyes, extraocular movements and fundoscopic examination, before and after surgery. High resolution thin (1- 2 mm) slice CT scan of the orbits was done to look for the nature and site of injury. In a few cases, Visual evoked potential was carried out in early and subclinical stages, to characterize the electrical activity of the optic nerve.
On evaluation, those satisfying study criteria were given high-dose steroids for about 3 days (Inj. Methyl Prednisolone 30 mg/kg loading dose followed by 15 mg/kg every six hours) and patients failing to initial steroid therapy were subjected to surgery. [5, 6]
After the initial preoperative evaluation, all patients underwent optic nerve decompression under general anaesthesia through the trans-nasal route. Surgery proceeded with middle meatal antrostomy, anterior to posterior ethmoidectomy, and wide sphenoidotomy and the optic canal is visualised by a bulge on the lateral wall of the sphenoid sinus. The optic nerve was decompressed by removing the bony canal inferno-medially, thereby exposing the intracanalicular portion of the optic nerve. [7].
The outcome of the surgery was assessed based on the change in visual acuity after surgery compared to pre-operative vision. The baseline visual acuity was taken before the surgery and the post-operative visual acuity was taken during the follow-up period of one month. The visual acuity measured using the Snellen chart is converted to quantitative figures as logarithmic minimum Angle Resolution (log MAR) Equivalent units as per referenced literature. [8].
Data Collection and Analysis
The collected patient data were entered in the Microsoft Excel Sheet and analysed using SPSS software (v.17) The quantitative parameters were described in Mean and Standard Deviation and Quantitative values in proportions. The student ‘t’ test was used to compare the mean visual outcomes, before and after surgery. The test of significance is kept at p-value < 0.05.
Results
In the study among the 14 patients studied, 57% were females and 43% were males. Most of the patients belonged to the age group of 26–45 years (57.1%) with the median age of presentation being 33 years. Among the study subjects, 71% of the cases had optic neuropathy secondary to sinonasal disease and 29% had a history of trauma. Compressive lesions due to tumours contributed to 50% of the sino-nasal diseases and the rest due to infectious optic neuritis.
As given above, initially the patients were given high-dose steroids for about 3 days and those not responding to initial steroid therapy were subjected to surgery. The interval between the onset of injury and surgery in traumatic neuropathy is 6–12 days with an average of 8 days, and in compressive optic neuropathy, the duration was 10–120 days with an average of 56 days. The patients with long-standing vision loss responded poorly to decompression, implying probable degeneration of the optic nerve. The summary of patient characteristics is given in detail in Table 1:
Visual Outcome After Surgery
In synopsis, the Postoperative visual acuity (VA) improvement was achieved in 11 patients and the total effective rate is 78.5% (33–90%). About 62.5% of patients who had no light perception (NLP) before surgery saw improvement in visual acuity after surgery, while 37.5% showed no improvement. Prior to surgery, 83.3% of patients who had residual vision saw an improvement in their vision and 16.7% did not have any benefit.
From the study results, it is observed that there was an improvement in visual acuity following endoscopic optic nerve decompression in all types of patients. There was a substantial improvement in vision among patients reporting with no perception of light showing a decline from 57.1 to 21.4%, which was found to be statistically significant. The improvement in VA after surgery is depicted in Table 2:
The visual acuity was assessed using LogMAR equivalent values of Snellen’s chart and the improvement in visual acuity is taken as efficacy of overall surgical outcome. The surgical intervention was found to be highly significant for the majority of the patients. The statistical analysis of the visual acuity is presented in Table 3:
A sample of selected cases history of presentation and management are illustrated in detail for further understanding and review:
Case 1
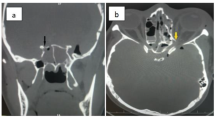
A 24-year-old male with a history of road traffic accident was admitted to our ENT department with no light perception in his left eye for three days. After the evaluation of the patient for injuries, he underwent a thorough ophthalmic examination. The patient was started on high-dose steroids, injection of Methylprednisolone IV 30 mg/kg loading dose followed by 15 mg/kg every 6 h for 3 days. He did not respond to steroid therapy and hence was taken for endoscopic optic nerve decompression after getting emergency surgical fitness. Intraoperative findings clearly showed fracture fragments impinging on the left optic nerve and the same was carefully removed, achieving optic nerve decompression without damaging the nearby vital structures. Postoperative period was uneventful without complications and the visual acuity after surgery was 6/12, which was highly rewarding for the patient. The photographic images are shown below in Figs. 1 and 2:
Case 2
A 38-year-old female presented with defective vision in her right eye for one month. After a complete history and ruling out trauma, an ophthalmic examination was done. Visual acuity was 6/24 in the right eye. Computed tomography of the paranasal sinus revealed spheno-orbito ethmoidal mass compressing the optic nerve. It was planned for elective functional endoscopic sinus surgery and the mass was seen occupying the posterior ethmoid and sphenoid compressing the optic nerve. Mass was removed in toto and optic nerve decompression was done. The Postoperative visual acuity was 6/9 and the biopsy of the specimen turned out to be adenoid cystic carcinoma. The MRI image and endoscopic view are depicted below in Figs. 3 and 4:
Discussion
The objective of the study was to assess the surgical outcome of endoscopic optic nerve decompression in patients presenting with optic neuropathy due to compressive and traumatic aetiology. A total of 14 patients admitted with defective vision in the Department of Otorhinolaryngology were evaluated and the study results were presented.
The prime indications of endoscopic optic nerve decompression are post-traumatic optic neuropathy, infectious optic neuropathy caused by inflammation secondary to sinus infection, and compressive optic neuropathy. The conditions causing compressive neuropathy are expansile lesions of sinuses (mucocele, polyposis, etc.,), tumours of sinuses (chondrosarcoma, fibrous dysplasia, adenoid cystic carcinoma, cavernous haemangioma etc.,), and intracranial expansile lesions. [9] As per published literature, the overall incidence of traumatic optic neuropathy is about 0.7 to 2.5% [9] and compressive optic neuropathy is 1.14/ 100,000 per year. [10].
Though some cases of traumatic optic neuropathy have certain chances of spontaneous resolution with medical management, the cases of nontraumatic optic neuropathy need stabilization for improvement of visual acuity by optic nerve decompression despite varied outcomes [11]. In cases of traumatic neuropathy, removal of direct compression by fractured bony fragments has a good prognosis after surgery.
The level of compression dictates the efficacy of the surgical procedure. The optic nerve may be compressed at the level of the optic nerve head, intraorbital, intracanalicular and orbital apex region. The main aim of endoscopic optic nerve decompression in optic neuropathy is to relieve the compressive forces within the intracanalicular segment of the optic nerve since it is tightly adherent to the orbital periosteum. Optic neuropathy sets in after a rise in intracanalicular pressure which initiates a cascade of secondary events like intraneural oedema, hematoma, altered microvasculature or CSF circulation and interrupted axoplasmic transport. [2] However, these changes get reversed partially by medical or surgical treatment.
Decompressive surgery does not hold good and is mostly contraindicated in cases where there is direct damage to the optic nerve, optic nerve atrophy or carotid cavernous fistula. There occurs a probable delay in the diagnosis in cases of sinonasal masses causing compressing due to the insidious nature of onset. Initially, the symptoms are vague and nonspecific with mild blurring of vision. In the early stages, visual acuity and fundus examination may be normal and with gradual progression of the disease, signs of scotoma, colour vision defect and afferent pupillary defect are observed. In the later stages, visual acuity is reduced and may eventually lead to loss of vision.
The residual vision is the most important independent prognostic factor for postoperative visual acuity improvement. Endoscopic Surgical decompression of the optic nerve can be visualized around 270 degrees, and the lateral 90 degrees is inaccessible. Hence the pathology corresponding to those inaccessible areas cannot be addressed and this could be a probable reason for reduced outcomes in cases of optic neuropathy.
In our study, overall visual acuity improvement was seen in 78.5% of patients with varying degrees of visual impairment. Following surgery, an improvement in visual acuity was seen in about 83.3% of the patients with residual vision and 62.5% of patients with NLP. Around 21.5% had no improvement in visual acuity, implying potential ganglionic cell death and degeneration of the optic nerve. [12] A study by Yu B and Chen et al., showed an overall effective visual improvement in 54.84% of patients, with 69.70% gaining significant improvement with residual vision and 37.9% improvement in patients with NLP. [2].
Similarly, Devang Gupta et al. in their study showed a significant improvement in visual acuity in about 80% of cases following surgical decompression, which is comparable to our study results. [7] In a study by Jingwen Sun et al., patients with residual vision showed better results compared to patients with complete blindness. [13] In 2023, Xiang Tu et al., conducted a study on nine patients with traumatic optic neuropathy and observed an overall effective rate of 69.2%. In the same study, patients with NLP before surgery had an effective rate of 50% and those with residual vision had a success rate of 85.7%. [14] Likewise, Levin et al., has reported that, patients with NLP before surgery had less improvement in visual acuity compared to patients with residual vision preoperatively [6].
The above studies quoted, clearly indicate that the decompression of the optic canal is effective for lesions involving optic neuropathy leading to vision loss. The surgical procedure allows the nerve to expand and lessens the detrimental effects of compression, thereby helping in restoring optic nerve function. Though all patients have not equally benefitted from optic nerve decompression, the majority of the cases had favourable outcomes implying timing of surgery and residual vision playing a significant role in restoring vision. [15].
Conclusion
Endoscopic Optic nerve decompression is a minimally invasive, less morbid and highly advantageous procedure in restoring or preventing the deterioration of vision in select cases of optic neuropathy. In addition, this procedure also provides excellent visualization of the orbital apex and the bony structures covering the neurovascular complex and helps in the preservation of olfaction. The key advantage of the procedure is the significant improvement in visual acuity with minimal associated complications. The critical factor influencing the outcome of optic nerve decompression is the timing of surgery, and once the optic atrophy has set in it has very minimal favourable outcomes.
References
Lal D, Stankiewicz JA (2009) Endoscopic optic nerve decompression. Oper Tech Otolaryngol Head Neck Surg 20(2):96–100. https://doi.org/10.1016/j.otot.2009.01.004
Yu B, Chen Y, Ma Y et al (2018) Outcome of endoscopic trans-ethmosphenoid optic canal decompression for indirect traumatic optic neuropathy in children. BMC Ophthalmol 18:152. https://doi.org/10.1186/s12886-018-0792-4
Wang DH, Zheng C, Qian J, Barr JJ (2008) Endoscopic optic nerve decompression for the treatment of traumatic optic nerve neuropathy. Oto-Rhino-Laryngol 70(2):130–133. https://doi.org/10.1159/000114537
Welkoborsky HJ, Kuestermeyer J, Steinke KV et al (2019) Endoscopic optic nerve decompression: indications, technique, results. Curr Otorhinolaryngol Rep 7:153–164. https://doi.org/10.1007/s40136-019-00235-z
Marks Steven C (2000) Nasal and sinus surgery. W.B. Saunders Company, USA, p 434 (ISBN 0-7216-7804-1)
Levin LA, Beck RW, Joseph MP, Seiff S, Kraker R (1999) The treatment of traumatic optic neuropathy: the international optic nerve trauma study. Ophthalmology. 106(7):1268–1277. https://doi.org/10.1016/s0161-6420(99)00707-1
Gupta D, Gadodia M (2018) Transnasal endoscopic optic nerve decompression in post traumatic optic neuropathy. Indian J Otolaryngol Head Neck Surg 70(1):49–52. https://doi.org/10.1007/s12070-017-1211-5
Holladay JT (1997) Proper method for calculating average visual acuity. J Refract Surg 13:388–391
Karimi S, Arabi A, Ansari I, Shahraki T, Safi S (2021) A systematic literature review on traumatic optic neuropathy. J Ophthalmol 2021:5553885. https://doi.org/10.1155/2021/5553885
Liu A, Craver EC, Bhatti MT, Chen JJ (2022) Population-based incidence and outcomes of compressive optic neuropathy. Am J Ophthalmol 236:130–135. https://doi.org/10.1016/j.ajo.2021.10.018. (Epub 2021 Oct 22. PMID: 34695397; PMCID: PMC9605817)
Pletcher SD, Metson R (2007) Endoscopic optic nerve decompression for non-traumatic optic neuropathy. Arch Otolaryngol Head Neck Surg 133:780–783. https://doi.org/10.1001/archotol.133.8.780
Levin LA (1999) Intrinsic survival mechanisms for retinal ganglion cells. Eur J Ophthalmol 9:S12–S16. https://doi.org/10.1177/112067219900901s08
Sun J, Cai X, Zou W, Zhang J (2021) Outcome of endoscopic optic nerve decompression for traumatic optic neuropathy. Ann Otol Rhinol Laryngol 130(1):56–59. https://doi.org/10.1177/0003489420939594
Tu X, Xiong C, Qi H, Ou YM, Rao J, Sun YQ, Fan YP, Liu GQ (2023) Diagnosis and treatment of transnasal endoscopic optic canal decompression for traumatic optic neuropathy. Front Neurosci 17:1168962. https://doi.org/10.3389/fnins.2023.1168962
Berhouma M, Jacquesson T, Abouaf L, Vighetto A, Jouanneau E (2014) Endoscopic endonasal optic nerve and orbital apex decompression for nontraumatic optic neuropathy: surgical nuances and review of the literature. Neurosurg Focus 37(4):E19. https://doi.org/10.3171/2014.7. (FOCUS14303. PMID: 25270138)
Funding
NIL.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of Interest
NIL.
Additional information
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Muthukumar, R., Mahesh Kumari, R., Shenbagavalli, S. et al. Surgical Outcome in Patients with Traumatic and Atraumatic Optic Neuropathy Following Endoscopic Optic Nerve Decompression. Indian J Otolaryngol Head Neck Surg 76, 1569–1574 (2024). https://doi.org/10.1007/s12070-023-04361-5
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s12070-023-04361-5