Abstract
Object
Olfactory groove meningiomas arise in the midline along the dura of the cribriform plate and may reach a large size before producing symptoms. We conducted a retrospective study of patients with these lesions focused on pre- and post-operative investigations for ophthalmological, personality and cognitive disturbances.
Methods
The authors reviewed 36 patients with giant olfactory groove meningiomas surgically treated via a bifrontal approach. Ophthalmological evaluation included visual acuity, fundoscopy and visual fields while psychological evaluation included a Mini-Mental State Examination. Data was collected before, 1 and 12 months after surgery. Formal pre- and post-operative ophthalmological examinations discovered visual deficits in 55.5% of the patients. Within the first month after surgery, improvement of visual acuity and of visual field deficits was observed. In post-operative neuropsychological testing, higher mental functions showed improvement. The most frequent post-operative complication was persistent rhinorrhoea in two patients.
Conclusions
Results at longest follow up indicate that cognitive changes and visual deficits will improve in patients with giant olfactory groove meningiomas after a bifrontal approach, without additional neurological deficits.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Olfactory groove meningiomas arise in the midline along the dura of the cribriform plate and fronto-sphenoidal suture, accounting for approximately 10% of intracranial meningiomas [1, 2, 5, 6, 24, 45, 46]. While most of these tumours occupy the floor of the anterior cranial fossa, extending from the crista galli to the tuberculum sellae [6], these slow growing lesions may reach a large size before producing symptoms.
A variety of alterations in personality and cognitive functioning may be observed in patients with meningiomas in the frontal area. However, systematic investigation of mental status changes in these patients has rarely been reported in recent years [63]. Previous studies reported neuropsychiatric symptoms and cognitive deficits in up to 51% to 78% of patients with intracranial tumours [30, 54]. Also, impairment of visual function is often unrecognised [56].
Our aim in this study was to investigate the surgical results in patients with giant olfactory groove meningioma. Special emphasis of visual and cognitive functioning was taken into consideration.
Materials and methods
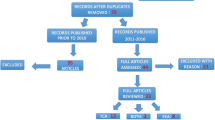
The authors conducted a retrospective analysis of 36 patients. Information on clinical history, symptoms, signs and outcome were obtained by review of the patient’s clinical notes, operative reports, histopathological records, follow-up records and radiological images.
All patients were studied pre-operatively by tri-planar contrast enhanced MRI. Ten patients had additional 3-D CT scans. Olfactory groove meningiomas were defined as those having their point of origin in the midline anterior cranial fossa, along the dura of the cribriform plate and fronto-sphenoidal suture. Anterior frontal, tuberculum sellae, clinoidal and diaphragma sellae meningiomas were excluded. A tumour was considered as a giant when the equivalent diameter was greater than 4.5 cm [53]. The equivalent diameter was calculated as (X + Y + .Z) × 1/3 1/3, where X, Y and Z are the maximum diameters in each plane. All the patients that we treated had a tumour equivalent diameter greater than 5.6 cm and in 16 it was greater than 7 cm.
All patients received peri-operative dexamethasone and anticonvulsant therapy.
Peri-tumoural oedema was evaluated by both T2-weighted and proton-weighted magnetic resonance imaging by a neuroradiologist graded according to the following scheme: Grade 0 absent or minimal oedema; Grade I moderate oedema; Grade II marked oedema.
In all patients, either digital subtraction cerebral angiography (n = 27) or angio-MRI (n = 9) was performed. All meningiomas were supplied by the anterior or posterior ethmoidal branches (n = 28) of the ophthalmic artery or the anterior branch of the middle meningeal artery (n = 4) or by all of these (n = 4). Pre-operative partial embolisation was done in two patients. Post-operative CT examinations were done in all patients within 24 h. None had post-operative cerebral angiography.
Pre-operative hydrocephalus was not present in any patient.
Microsurgical techniques were used for all patients. Simpson’s grade, complications and intra-operative findings were recorded in the operative note for each patient while surgical specimens were evaluated by a neuropathologist. All histopathology results were analysed according to the World Health Organisation (WHO) grading criteria.
Cognitive and ophthalmological assessments
During the initial evaluation, cognitive function was assessed using the Mini-Mental State Examination (MMSE) [18]. The MMSE consists of seven subtests designed to measure orientation, memory, attention, naming, and the ability to follow verbal and written commands, write a sentence spontaneously and design copying. Each task is scored individually and the scores are added to yield a score ranging from 0 to 30, with the higher scores representing best cognitive functioning. As in the original MMSE description, we considered scores less than 24 to be indicative of cognitive impairment. Although this cut-off score is conventional, it is an approximation since this test is strongly affected by age and level of education. Our primary aim in performing the MMSE before and after surgery was to evaluate whether the bifrontal approach had a negative impact on cognitive functioning in these patients. The patients repeated the MMSE at follow up after 1 month and then after 12 months. The neuropsychological tests used in all patients at 30 days follow up and in 25 patients at 12 months follow up included also the following: (1) Brief Psychiatric Rating Scale (BPRS) version 4.0 translated into Italian by Morosini [40]; (2) Neuropsychiatric Inventory (NPI) (in 20 patients); (3) Phonemic Verbal Fluency Test [43]; (4) preferred hand test for assessment of handedness; (5) Verbal Memory Test. The results of the tests for attention, verbal memory and disconnection were analysed in detail by a neuropsychologist.
Formal pre- and post-operative ophthalmological examinations were performed by the Ophthalmology Department and included testing for visual acuity, fundoscopy and Goldmann perimetry for visual fields. Visual acuity was tested with a Snellen chart at 6 m in all patients. The presence of concomitant eye pathology was also taken into account.
Results
From 1990 to 2004 a total of 36 patients were treated for olfactory groove meningioma at the Department of Neurosurgery at San Filippo Neri Hospital in Rome. All the patients were surgically treated by the senior author (G.G.). The mean patient age was 56.4 years (range 28 to 78) and 66.7% of the patients were women (including one transsexual with male genotype and female phenotype) [19]. The demographic data is indicated in Table 1.
The most common presenting symptom was headache seen in 18 patients (50%) and the other signs and symptoms are as summarised in Table 2. On admission, 25 patients (69.4%) had mental status changes with intellectual deterioration; major psychological changes included confusion (15 patients, 41.6%), and depression (ten patients, 27.7%) as shown in Table 3. Twenty patients (55.5%) presented with associated visual complaints, and ten patients (27.7%) had epilepsy at presentation. All but six patients had anosmia on presentation and unilateral preservation of olfactory function was possible only in two patients. Pre-operative urinary incontinence was reported in seven patients and had improved urinary function after surgery.
The size of the tumour was calculated on the basis of measurements obtained from CT scans or MR images. The tumour equivalent diameter varied from 5.6 to 8 cm, with a median of 6.4 cm. Meningiomas were broad based with symmetrical bilateral growth in all but one patient; pre-operative ethmoidal extension of the tumour was demonstrated in one patient. Peri-tumoural oedema on pre-operative MRI studies was absent in 25 (69.4%), moderate in eight (22.2%) and severe in three (8.3%) patients.
Thirty five patients were operated on by a bifrontal approach (Figs. 1, 2 and 3). When the frontal sinus was entered, the mucous membranes were exenterated and the duct was tamponaded with iodine-soaked cottonoids and covered with pericranium. One patient with unilateral extension of the tumour was operated on by a fronto-temporal approach.
Pre-operative sagittal (a) and coronal (c) MRI scans after gadolinium injection of a 52-year-old woman with a giant olfactory groove meningioma. c Coronal MRI scan demonstrating the ethmoidal extension of the tumour (grade I). d Post-operative CT scan demonstrating tumour removal with bifrontal craniotomy
Total macroscopic surgical resection of the mass lesion was achieved in 31 patients (Simpson grade I removal in 11 patients, and Simpson grade II in 20 patients); three patients had a non-radical removal (Simpson grade III), while two patients had a subtotal resection (Simpson grade IV). Radical tumour removal was avoided in elderly patients. In all patients, there was an intact arachnoidal plane between the tumour and the optic nerve, chiasm and anterior cerebral artery complex, thus facilitating tumour dissection from these structures. Recurrence occurred in one patient who had subtotal resection and was re-operated 24 months after the first intervention; another recurrence after subtotal resection was operated elsewhere 7 years later. The follow-up period of patients ranged from 34 to 187 months (mean: 111 months). None of the other patients showed radiological progression of the tumour during their follow-up and their clinical condition remained stable. All the patients had WHO grade I tumours (15 transitional, 41.7 %; 12 meningothelial, 33.4 %; five psammomatous 13.9%; two syncitial 5.5%; two angioblastic, 5.5%).
Cognitive function
The mean MMSE score on admission was 16.4 (SD ± 7.99). Twenty eight patients (80%) had an MMSE score lower than 24, consistent with cognitive impairment. Post-operative psychometric assessment was available in 35 patients. The mean MMSE score at 1 month follow up evaluation was 24.4 (SD ± 4.79), with 18 (51.4%) patients having an MMSE score lower than 24. There was no further significant mean score change at 12 months of follow up (mean MMSE score, 24.8; SD ± 4.83). On admission, the MMS was normal [24–30] in six patients and grossly impaired (severe) in 11 patients.
After 1 month follow up, 17 patients were in the normal MMSE group, while no patient was still in the severe group. Further cognitive evaluation of the 23 surviving patients was carried out during this manuscript formulation (mean follow up 111 months, range 34–187). The mean MMSE score was 23.9 (SD ± 4.97), and 12 (52.1%) patients had an MMSE score lower than 24; the mean MMSE score was lower than MMSE score at 12 months after surgery, probably secondary to further aging of the patients (Table 4).
At 30 days after surgery, patients were assessed with other neuropsychological tests. Post-operative clinical assessment performed using the Brief Psychiatric Rating Scale (BPRS) and the Neuropsychiatric Inventory (NPI) showed a mean value of 54.7 (SD ± 10.4) and 9.7 (SD ± 1.3). The performance data on the Phonemic Verbal Fluency Test showed a mean value of 31.3 (SD ± 9.34). Data analysis of the Verbal Memory Test revealed a mean value of 27.9 (SD ± 5.2). Although anxiety and depression was present in some patients, all the patients had a good psychosocial adjustment following surgery, most of them returning to work or to their previous social activities in daily life.
Ophthalmological findings
Twenty patients (55.5%) presented with visual deficits: the mean duration of visual symptoms was 27.4 months (range 3–125). Visual acuity was decreased bilaterally in six patients and unilaterally in ten patients. Fundoscopy revealed optic disc pallor in 16 patients (ten right eye, four left eye and two bilateral) and disc swelling in three patients (two right eye, one left eye). A Foster–Kennedy syndrome was present in two patients. Visual field defects (Table 5) were found in 14 patients. Chiasmal compression produced bitemporal hemianopia in seven and a temporal hemianopia in one eye in seven patients (involving the right eye in two and the left eye in five).
Within the first month after surgery, the post-operative visual acuity improved in nine patients, while in 26 it remained unchanged. In eight patients visual field defects improved and in two cases the defects resolved completely. In three patients, visual field defects were unchanged and became worse in one patient. No patient had post-operative deterioration of visual acuity (Table 6).
Post-operative recovery of visual deficits was poor in five patients with a deficit of more than 24 months and none of these patients had improvement of visual function.
In general, vision improved rapidly within the first month, with little further improvement within the first year of follow up.
Complications
Complications were seen in six patients (16.6%). The most frequent post-operative complication was persistent rhinorrhoea, which occurred in two patients (5.5%): all CSF leaks stopped after insertion of a lumbar drain. Persistent post-operative seizures were present in one patient. As discussed above, in one there was post-operative visual field deterioration. One patient with symptomatic delayed frontal pneumocephalus had surgical repair 1 month after tumour resection, with subsequent resolution of the symptoms. There was one mortality on the 17th post-operative day secondary to massive pulmonary embolism after an uneventful early post-operative course (Table 7). No other clinical complications were observed.
Discussion
The surgical principles of the management of olfactory groove meningiomas were first described by Cushing and Eisenhardt in 1938 [11]. He emphasised the importance of tumour decompression before capsule dissection, thus preserving the anterior cerebral arteries that may be adherent. Yet, the correct approach to use in the resection of giant olfactory groove meningiomas remains controversial [4, 8, 12, 14, 15, 17, 20, 22–25, 29, 31, 38, 48, 49, 53, 58, 66].
Our study presents a homogeneous cohort of patients with giant olfactory meningiomas surgically treated via a bifrontal approach with only one patient treated with a fronto-temporal craniotomy. The bifrontal approach has been described in detail in numerous studies [1, 11, 13, 15, 45, 55, 59], while the subfrontal route without resection of frontal lobe tissue, was first described by Tonnis in 1938, and later used by several authors [15, 21, 32, 33, 39, 42, 44–46, 50, 51, 52, 60, 61]. This approach provides direct access to the tumour without excessive brain retraction, reaching the primary tumour attachment and the vascular feeders of the meningioma, thus first dividing the ethmoidal arteries and small meningeal feeding vessels, devascularising and debulking the tumour from the inferior aspect. In those with extensive bone involvement, it may be appropriate to drill the anterior cranial base and provide a secondary reconstruction with a vascularised pericranial flap [14]. Disadvantages are the inevitable opening of the frontal sinus with the risk of CSF leakage and meningitis. We used pericranial flaps to cover the defect in the floor of the anterior fossa. Two patients had rhinorrhoea without meningitis and both stopped after insertion of a lumbar drain.
In our experience, it is fundamental to perform pre-operative angiography or angio-MRI to visualise the neurovascular structures that may be encased by the meningioma. We have done so in all patients and had no operative vascular complications. We constantly found an intact arachnoidal plane between the tumour, the optic apparatus and the anterior communicating complex, thus facilitating dissection.
One of the major criticisms against this approach is the risk of new cognitive deficits as a result of excision of a basal portion of the frontal lobe [44, 52, 63]. In our study, we examined cognitive function outcome after the bifrontal approach and comparing pre- and post-operative evaluation we found no increased deficits after surgery, while some had improved function (Table 5). Similarly, Hunter et al. [25] and Tucha et al. [63, 64] reported a remarkable improvement of cognitive status and attention function after resection of frontal meningiomas. We suggest that peri-tumoural oedema played an important role in causing cognitive function deficits and post-surgical improvement in attention and memory disturbances may be related also to diminished frontal lobe oedema. Changes of mental capacity are frequently observed and the diagnosis of dementia is still applied to patients who have not been adequately evaluated. Indeed, it was difficult for us to determine the duration of such changes, because of their insidious onset. Also, in many patients personality changes were even unrecognised by relatives. In the case of the transsexual patient, the personality changes were noted in the last 4 months before admission but were correlated by family members to the new gender identity of the patient [19].
Assessment of cognitive outcome is important when brain tumours and neurosurgical brain interventions can affect cognitive functioning. First described by Folstein et al. [18] in 1975, the MMSE is routinely used by clinicians as the criterion screening test for cognitive impairment. The MMSE is relatively insensitive to cognitive changes typically caused by frontal lobe lesions and does not substitute for other formal and more extensive neurocognitive testing. Also, it does not take into consideration what role depression plays in the patient's score. However, we have used this screening tool in the initial encounter and in the subsequent interviews because of its easy administration. There is actually very little published regarding objective assessment of cognitive function pre- and post-operatively in olfactory groove meningiomas.
Only few studies have focused on pre- and post-operative testing for cognitive disturbances [63, 64]. Bakay [5] reported that these disturbances improved in 47% of his patients post-operatively, while Ojemann [45] stated that pre-operative changes recovered completely in all patients after surgery. In the series from Solero et al. [57] 43.3% of cognitive disturbances completely recovered after removal of the meningioma. Our results indicate that cognitive functioning in patients with olfactory groove meningioma may improve markedly after bifrontal surgical approach at 1 month follow up, with no further improvement at 1 year follow up.
Urinary incontinence was present in seven patients. This symptom may be caused by the pressure of the meningioma on the micturition centre [3] or by personality deterioration with loss of social sense [25]. In five patients urinary function improved after surgery. Two patients had persisting nocturia without any symptoms of dementia.
Anosmia is an early symptom of olfactory groove meningiomas, but only few patients complain of it. The decline of olfactory function is gradual, similar to that seen in the elderly, and only one side is affected in the early stage. Lateralised testing of olfactoy function seems to be necessary to achieve an early diagnosis. Preservation of olfaction during surgery is difficult. Even if the olfactory tract is in anatomical continuity after resection of the meningioma [7, 66], post-operative anosmia may be induced by ischaemia caused by loss of blood supply to the olfactory nerves or a functional lesion of the fila olfactoria during surgery. In the series of Bassiouni et al. [7] there was no difference in the preserving of olfaction comparing various surgical approaches. To prevent further damage of the olfactory nerves, frontal lobe retraction should be minimal. Our findings indicate that 83% had anosmia on presentation. In those with pre-operative unilateral normal olfactory function, only two of the six patients had preserved olfaction after surgery.
The most common reason for seeking medical attention in patients with olfactory meningiomas is failing vision. Vision deficits often progress asymmetrically: the commonest early visual complaint is blurred vision in one eye secondary to a central scotoma, but partial loss of vision in one eye proceeds almost unnoticed by the patient [50]. Pre-operative visual deficits on clinical examination are reported in 15.3–58.1% of patients [6, 11, 16, 23, 35, 57, 62, 65]. Visual impairment, including optic disc swelling and pallor, was found in 55.5% of our patients on clinical examination. Classical Foster–Kennedy syndrome was reported to occur in 0–5.5% of patients in recent studies [6, 65] and was found in 5.5% of our patients. Patients with visual impairment longer than 1 year have a worse chance of improved vision [47]. Also, our findings suggest that visual outcome was better in patients with symptoms shorter than 24 months. Post-operatively, visual function improved in 22.8% of our patients, while in 74.2% it was unchanged. There was no deterioration of visual acuity after bifrontal excision but in one patient the visual field defect worsened.
The percentage of recovery of visual fields in our series was less than that reported by other authors in patients with frontal meningiomas [41]. Larger mean tumour diameter and longer duration of visual deterioration in our series compared with patients in other reports with tumours smaller than 3 cm and a shorter history of symptoms may have an influence on the differences in visual outcome. Nakamura et al. [41] reported worse improvement rates of post-operative visual outcome in tuberculum sellae meningiomas treated with a bifrontal approach than those treated with a fronto-lateral approach. However, in their series clinical and radiological data were not matched in the two groups. Larger tumour diameter in the bifrontal group and the fact that this approach was performed in earlier years may have influenced the visual outcome.
Complete resection of olfactory meningiomas has been reported in 67–100% of patients [6, 23, 44, 46, 51, 57, 59, 61, 62, 65]. Recurrence rates of these tumours range from 5% to 41%, although several authors have reported a very low or no recurrence rate after a mean follow up period ranging from 4.4 to 9 years [9, 34, 36, 45, 51, 59]. Recurrence of meningioma may be the result of incomplete resection or occur after even radical resection after a long follow up [6, 10, 28, 33, 34, 37, 42, 56, 65]. The approach for tumour resection seems not to influence tumour recurrence [42]. The rate of recurrence in our series was 5.5% after a mean follow up period of 111 months. Mortality rates in the literature vary from 0% [24, 44, 46] to 17% [57] in recent literature. In our series, we had one death after a massive pulmonary embolism on the 17th postoperative day; but none directly related to surgery.
Conclusions
Our results at longest follow up indicate that there is a good prospect that cognitive changes and visual deficits will improve in patients with giant olfactory groove meningiomas after a bifrontal approach, without additional neurological deficits. This approach may be considered the most appropriate for these tumours.
References
Al-Mefty O (1993) Tuberculum sellae and olfactory groove meningioma. In: Sekhar LN, Janecka IP (eds) Surgery of cranial base tumours. Raven, New York, pp 507–519
Al-Mefty O, Smith R (1991) Tuberculum sellae meningiomas. In: Al-Mefty O (ed) Meningiomas. Raven, New York, p 395–411, 630
Andrew J, Nathan PW (1964) Lesions on the anterior frontal lobes and disturbances of micturition and defaecation. Brain 87:233–262
Babu R, Barton A, Kasoff SS (1995) Resection of olfactory groove meningiomas: technical note revisited. Surg Neurol 44:567–572
Bakay L (1984) Olfactory meningiomas. The missed diagnosis. JAMA 251(1):53–55, Jan 6
Bakay L, Cares HL (1972) Olfactory meningiomas: report on a series of twenty-five cases. Acta Neurochir (Wien) 26:1–12
Bassiouni H, Asgari S, Stolke D (2007) Olfactory groove meningiomas: functional outcome in a series treated microsurgically. Acta Neurochir (Wien) 149(2):109–121
Bricolo A: Commentary on Babu R, Barton A, Kasoff SS (1995) Resection of olfactory groove meningiomas: technical note revisited. Surg Neurol 44:567–572
Chan RC, Thompson GB (1984) Morbidity, mortality, and quality of life following surgery for intracranial meningiomas. A retrospective study in 257 cases. J Neurosurg 60:52–60
Christensen D, Laursen H, Klinken L (1983) Prediction of recurrence in meningiomas after surgical treatment. A quantitative approach. Acta Neuropathol (Berl) 61(2):130–134
Cushing H, Eisenhardt L (1938) The olfactory meningiomas with primary anosmia. In: Cushing H, Eisenhardt L (eds) Meningiomas: their classification, regional behaviour, life history, and surgical results. Thomas, Springfield, p 250–282
Delashaw JB Jr, Jane JA, Kassell NF, Luce C (1993) Supraorbital craniotomy by fracture of the anterior orbital roof: technical note. J Neurosurg 79:615–618
DeMonte F (1996) Surgical treatment of anterior basal meningiomas. J Neurooncol 29(3):239–248
Derome PJ, Guiot G (1978) Bone problems in meningiomas invading the base of the skull. Clin Neurosurg 25:435–451
El Gindi S (2000) Olfactory groove meningioma: surgical techniques and pitfalls. Surg Neurol 54:415–417
Finn JE, Mount LA (1974) Meningiomas of the tuberculum sellae and planum sphenoidale. A review of 83 cases. Arch Ophthalmol 92(1):23–27
Fliss D, Zucker G, Amir A, Gatot A, Cohen M, Spektor S (2000) The subcranial approach for anterior skull base tumours. Otolaryngol Head Neck Surg 11:238–253
Folstein MF, Folstein SE, McHugh PR (1975) “Mini-mental state”. A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 12(3):189–198
Gazzeri R, Galarza M, Gazzeri G (2007) Growth of a meningioma in a transsexual patient after oestrogen–progestin therapy. N Engl J Med 357(23):2411–2412
Goffin J, Fossion E, Plets C, Mommaerts M, Vrielinck L (1991) Craniofacial resection for anterior skull base tumours. Acta Neurochir (Wien) 110:33–37
Guthrie BL, Ebersold MJ, Scheithauer BW (1990) Neoplasms of the intracranial meninges. In: Youmans JR (ed) Neurological surgery vol 5. 3rd edn. Saunders, Philadelphia, pp 3250–3315
Hallacq P, Moreau JJ, Fischer G, Beziat JL (1999) Frontal sinus approach to olfactory groove meningiomas [in French]. Neurochirurgie 45:329–337
Hassler W, Zentner J (1989) Pterional approach for surgical treatment of olfactory groove meningiomas. Neurosurgery 25:942–947
Hentschel S, DeMonte F (2003) Olfactory groove meningiomas. Neurosurg Focus 14(6):e4
Hunter R, Blackwood W, Bull J (1968) Three cases of frontal meningiomas presenting psychiatrically. Br Med J 3(5609):9–16
Jallo GI, Benjamin V (2002) Tuberculum sellae meningiomas: microsurgical anatomy and surgical technique. Neurosurgery 51:1432–1440
Jho HD, Alfieri A (2002) Endoscopic glabellar approach to the anterior skull base: a technical note. Minim Invasive Neurosurg 45:185–188
Kallio M, Sankila R, Hakulinen T, Jaaskelainen J (1992) Factors affecting operative and excess long-term mortality in 935 patients with intracranial meningioma. Neurosurgery 31(1):2–12, Jul
Kawakami K, Yamanouchi Y, Kawamura Y, Matsumura H (1991) Operative approach to the frontal skull base: extensive transbasal approach. Neurosurgery 28:720–725
Keschner M, Bender MB, Strauss I (1938) Mental symptoms associated with brain tumour. A study of 530 verified cases. J Am Med Assoc 110:714–718
Lagares A, Lobato RD, Castro S, Alday R, De la Lama A, Alen JF, Gonzalez P (2001) Meningioma of the olfactory groove: review of a series of 27 cases [in Spanish]. Neurochirurgica (Astur) 12:17–22
Long DM (1989) Meningiomas of the olfactory groove and anterior fossa. Atlas of operative neurosurgical technique, cranial operations, vol 1. Lippincott Williams & Wilkins, Baltimore, pp 238–241
Maiuri F, Salzano FA, Motta S, Colella G, Sardo L (1998) Olfactory groove meningioma with paranasal sinus and nasal cavity extension: removal by combined subfrontal and nasal approach. J Craniomaxillofac Surg 26:314–317
Mathiesen T, Linquist C, Kihlstrom L, Karlsson B (1996) Recurrence of cranial meningiomas. Neurosurgery 39:2–9
Mayfrank L, Gilsbach JM (1996) Interhemispheric approach for microsurgical removal of olfactory groove meningiomas. Br J Neurosurg 10:541–545
Melamed S, Sahar A, Beller AJ (1979) The recurrence of intracranial meningiomas. Neurochirurgia (Stuttg) 22(2):47–51
Mirimanoff RO, Dosoretz DE, Linggood RM, Ojemann RG, Martuza RL (1985) Meningioma: analysis of recurrence and progression following neurosurgical resection. J Neurosurg 62:18–24
Moore CE, Ross DA, Marentette LJ (1999) Subcranial approach to tumours of the anterior cranial base: analysis of current and traditional surgical techniques. Otolaryngol Head Neck Surg 120:387–390
Morley T (1973) Tumours of the cranial meninges. In: Youmans J (ed) Neurological surgery. Saunders, Philadelphia, p 1388–1411
Morosini PL, Casacchia M (1985) Traduzione Italiana della Brief Psychiatric Rating Scale, versione 4.0 ampliata (BPRS 4.0). Riv Riabilitaz Psichiatr Psicosocial 3:199–228
Nakamura M, Roser F, Struck M, Vorkapic P, Samii M (2006) Tuberculum sellae meningiomas: clinical outcome considering different surgical approaches. Neurosurgery 59(5):1019–1028
Nakamura M, Struck M, Roser F, Vorkapic P, Samii M (2007) Olfactory groove meningiomas: clinical outcome and recurrence rates after tumour removal through the fronto-lateral and bifrontal approach. Neurosurgery 60(5):844–852
Novelli G, Papagno C, Capitani E, Laiacona M, Vallar G, Cappa SF (1986) Three clinical tests for the assessment of lexical retrieval and production. Norms from 320 normal subjects. Arch Psicol Neurol Psichiatr 47:477–506
Obeid F, Al-Mefty O (2003) Recurrence of olfactory groove meningiomas. Neurosurgery 53:534–543
Ojemann RG (1991) Olfactory groove meningiomas. In: Al-Mefty O (ed) Meningiomas. Raven, New York, p 383–392
Ojemann RG, Swan K (1988) Surgical management of olfactory groove, suprasellar and medial sphenoid ridge meningiomas. In: Schmidek HH, Sweet WH (eds) Operative neurosurgical techniques. Grune & Stratton, Orlando, p 531–545
Pamir MN, Ozduman K, Belirgen M, Kilic T, Ozek MM (2005) Outcome determinants of pterional surgery for tuberculum sellae meningiomas. Acta Neurochir (Wien) 147(11):1121–1130
Paterniti S, Fiore P, Levita A, La Camera A, Cambria S (1999) Venous saving in olfactory meningioma surgery. Clin Neurol Neurosurg 101:235–237
Persky MS, Som ML (1978) Olfactory groove meningioma with paranasal sinus and nasal cavity extension: a combined approach. Otolaryngology 86:ORL-714–ORL-720
Poppen JL (1964) Operative techniques for removal of olfactory groove and suprasellar meningiomas. Clin Neurosurg 11:1–7
Ransohoff J, Nockels R (1993) Olfactory groove and planum meningiomas. In: Apuzzo M (ed) Brain surgery: complication avoidance and management. Churchill Livingstone, New York, p 177–185
Samii M, Ammirati M (1992) Olfactory groove meningiomas. In: Samii M (ed) Surgery of the skull base: meningiomas. Springer, Berlin, p 15–25
Schaller C, Veit R, Hassler W (1994) Microsurgical removal of olfactory groove meningiomas via the pterional approach. Skull Base Surg 4:189–192
Schlesinger B (1950) Mental changes in intracranial tumours and related problems. Confin Neurol 10:225–263
Sekhar LN, Nanda A, Sen CN, Snyderman CN, Janecka IP (1992) The extended frontal approach to tumours of the anterior, middle, and posterior skull base. J Neurosurg 76:198–206
Snyder WE, Shah MV, Weisberger EC, Campbell RL (2000) Presentation and patterns of late recurrence of olfactory groove meningiomas. Skull Base Surg 10(3):131–139
Solero CL, Giombini S, Morello G (1983) Suprasellar and olfactory meningiomas: report on a series of 153 personal cases. Acta Neurochir (Wien) 67:181–194
Spektor S, Valarezo J, Fliss DM, Gil Z, Cohen J, Goldman J, Umansky F (2005) Olfactory groove meningiomas from neurosurgical and ear, nose, and throat perspectives: approaches, techniques, and outcomes. Neurosurgery 57(4 Suppl):268–280
Symon L (1983) Olfactory groove and suprasellar meningioma. In: Krayenbühl H (ed) Advances and technical standards in neurosurgery. Springer, New York, p 67
Tamaki N, Yin D (1999) Giant olfactory groove meningiomas: advantages of the bilateral fronto-orbitonasal approach. J Clin Neurosci 6(4):302–305
Tonnis W (1938) Zur Operation der Meningeome der Siebbeinplatte. Zentralbl Neurochir 1:1–7
Tsikoudas A, Martin-Hirsch DP (1999) Olfactory groove meningiomas. Clin Otolaryngol 24:507–509
Tucha O, Smely C, Preier M, Lange KW (2000) Cognitive deficits before treatment among patients with brain tumours. Neurosurgery 47(2):324–333
Tucha O, Smely C, Preier M, Becker G, Paul GM, Lange KW (2003) Pre-operative and post-operative cognitive functioning in patients with frontal meningiomas. J Neurosurg 98:21–31
Turazzi S, Cristofori L, Gambin R, Bricolo A (1999) The pterional approach for the microsurgical removal of olfactory groove meningiomas. Neurosurgery 45:821–826
Welge-Luessen A, Temmel A, Quint C, Moll B, Wolf S, Hummel T (2001) Olfactory function in patients with olfactory groove meningioma. J Neurol Neurosurg Psychiatry 70:218–221
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
The patients described here are remarkable for several reasons: the size of the tumours that have developed (often over many years), the fact that removal even at a late stage produces an improvement in function, and the relatively good prognosis after operation. This paper nicely describes this neurosurgical success story; the authors are to be particularly commended for including a routine assessment of cognitive function.
Lindsay Wilson
University of Stirling
Comment
The authors present their visual and cognitive results for the bifrontal approach (except one patient) to giant olfactory groove meningiomas. The 36 patients were accrued over a 14 year period ending in 2004. The primary message of the article is that visual and cognitive dysfunction does improve after surgery and that the majority of the improvement occurs within the first month. In addition, chronicity of visual deficits predicts a worse visual outcome. This is a very reasonably written article and one that adds to the literature.
John A. Jane, Jr.
University of Virginia
The Author’s didn’t receive any financial support in conjunction with the generation of their submission.
Rights and permissions
About this article
Cite this article
Gazzeri, R., Galarza, M. & Gazzeri, G. Giant olfactory groove meningioma: ophthalmological and cognitive outcome after bifrontal microsurgical approach. Acta Neurochir (Wien) 150, 1117–1126 (2008). https://doi.org/10.1007/s00701-008-0142-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-008-0142-z