Abstract
Objective
The purpose of the study was to compare the ability of navigated 3D ultrasound to distinguish tumour and normal brain tissue at the tumour border zone in subsequent phases of resection.
Materials and methods
Biopsies were sampled in the tumour border zone as seen in the US images before and during surgery. After resection, biopsies were sampled in the resection cavity wall. Histopathology was compared with the surgeon’s image findings.
Results
Before resection, the tumour border was delineated by ultrasound with high specificity and sensitivity (both 95%). During resection, ultrasound had acceptable sensitivity (87%), but poor specificity (42%), due to biopsies falsely classified as tumour by the surgeon. After resection, sensitivity was poor (26%), due to tumour or infiltrated tissue in several biopsies deemed normal by ultrasound, but the specificity was acceptable (88%).
Conclusions
Our study shows that although glioblastomas are well delineated prior to resection, there seem to be overestimation of tumour tissue during resection. After resection tumour remnants and infiltrated brain tissue in the resection cavity wall may be undetected. We believe that the benefits of intraoperative ultrasound outweigh the shortcomings, but users of intraoperative ultrasound should keep the limitations shown in our study in mind.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Background
In the surgical treatment of glioblastomas the goal is to perform the most complete resection possible without damaging normal tissue [2, 17]. Neuronavigation systems have become part of the routine tools assisting the surgeon in achieving this goal. Intraoperative imaging appears to be necessary to maintain accuracy of neuronavigation during subsequent stages of tumour resection [19, 25, 29]. To be of value, intraoperative imaging modalities must reliably discriminate between tumour and normal tissue in the subsequent stages of surgery. At present, the alternatives for intraoperative imaging in brain tumour surgery are MRI and ultrasound [10, 11, 20, 24, 31]. Although recognized to be useful for detecting residual tumour during resection [9, 30, 35, 36], it is not known how intraoperative factors affect the ability of ultrasound to delineate tumour. The aim of the present study was to assess the ability of intraoperative 3D ultrasound in neuronavigation to distinguish tumour and normal brain tissue in the tumour border zone, before, during and after resection.
Materials and methods
Patients and biopsies
Nineteen patients (four females and 15 males, average age 59, age range 45–83 years) with the final diagnosis of glioblastoma were included in the present study. The patients were included in the period 2003–2006. A total of 301 biopsies were acquired, 186 biopsies were included in this study. The study was approved by the Regional Research Ethics Committee in medicine in Mid-Norway and the patients signed an informed consent form before the operation.
Neuronavigation equipment and intraoperative 3D ultrasound imaging
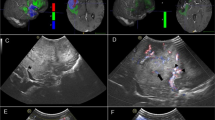
A 3D ultrasound based image guidance system was used; SonoWand®, equipped with a 5 MHz probe with tracking. The biopsy forceps used in the study was equipped with a tracking frame, which enabled image guided biopsies (Fig. 1). This system is described in further detail in other papers [8, 21, 37]. Preoperative MRI (T1 with contrast enhancement, T2 and FLAIR) was imported in the neuronavigation system and used for planning and anatomical orientation, but not during biopsy sampling. 3D ultrasound data was acquired immediately before biopsy sampling in each phase (Fig. 2). When a resection cavity had been created, the cavity was filled with saline before 3D ultrasound acquisition. The saline was removed afterwards.
Biopsy sampling method. a The biopsy forceps is calibrated to the navigation system by positioning the tip of the forceps in a known reference point on the patient reference frame, in the shape of a small cone with a hole in the middle. b Two perpendicular planes are determined by the position and trajectory of the biopsy forceps. c The 3D ultrasound data volume is sliced in the two perpendicular planes, displayed on screen (bottom). The tip of the biopsy forceps is thus indicated in the two image planes, marking the site for biopsy sampling
Biopsy examples. a Screenshots from biopsy sampling before resection. Left: Biopsy sampled from area interpreted as tumour, confirmed by histopathology. Middle: Biopsy sampled from site interpreted as normal, confirmed by histopathology. Right: Biopsy sampled from site interpreted as normal, histopathology showed infiltration. b Screenshots from biopsy sampling during resection. Left: Biopsy sampled from site interpreted as tumour, confirmed by histopathology. Middle: Biopsy sampled from site interpreted as normal, confirmed by histopathology. Right: Biopsy sampled from site interpreted as tumour, but the pathologist saw no certain tumour tissue. c Screenshots from biopsy sampling after resection. Left: biopsy sampled from site interpreted as “tumour, uncertain”, tumour confirmed by histopathology. Middle: Biopsy sampled from site interpreted as normal, confirmed by histopathology. Right: Biopsy sampled from site interpreted as normal, but histopathology showed tumour
Image-guided biopsy sampling and analysis
The biopsies were sampled in three different phases of resection; (1) After opening the dura, immediately before starting the resection. (2) After most resection had been performed, but with some residual tumour left. (3) After completed resection, having removed all detected/known residual tumour (either detected visually or by use of intraoperative ultrasound) except in eloquent areas. The biopsy forceps was calibrated to the navigation system by positioning the tip of the biopsy forceps at a reference point on the patient reference frame (Fig. 1.) The position and trajectory of the biopsy forceps was displayed on two perpendicular image slices on the neuronavigation unit, marking the biopsy site. The surgeon’s assumption on whether the biopsy was sampled in tumour or normal tissue based on the ultrasound image findings was noted at the time of biopsy sampling. The surgeon classified the biopsies as “tumour”, “tumour, uncertain”, “normal uncertain” and “normal”. Images (snapshots) from the neuronavigation system taken at the time of biopsy sampling were stored for further processing and analysis.
The biopsies were collected from the border-zone of the tumour, not further from the assumed tumour border in the US images (as judged by the surgeon) than 7 mm and not closer than 2 mm. After completed resection however, biopsies were only collected from the resection cavity wall. Before and during resection, two to four biopsies were collected in assumed solid tumour tissue, while one to three biopsies were sampled from assumed normal brain tissue. All biopsies included in the study were postoperatively controlled to ensure that they were sampled in the 2–7 mm distance from the tumour border as defined from the navigation images. Biopsies outside the 2–7 mm area of interest were excluded, and this was the most frequent reason for exclusion of biopsies. In cases of doubt, the screenshots were analyzed with an edge-detection algorithm (described elsewhere [38]). The shortest distance between the tip of the biopsy forceps and the detected border was then found. Biopsies where the pathologist could not categorize the biopsy, for example, because of too small or traumatized biopsies, were also excluded.
The majority of biopsies (176 of 186 included biopsies) was fixed in buffered formalin and embedded in paraffin. Ten biopsies were prepared as frozen sections. The sections were stained with hematoxylin and eosin. A senior neuropathologist (SHT) examined the biopsies according to the WHO classification [1]. All histopathological analyses were performed without prior knowledge of the image information. The biopsies were classified as “tumour”/“infiltration zone”/“not tumour”. All but three of the patients had a postoperative MRI within 48 h.
Statistical methods
To calculate specificity, sensitivity, PPV and NPV, the cells in the original 3 × 4 result table from each phase (Table 2) were combined to create a 2 × 2 table for each phase of the operation: Biopsies deemed “normal” and “normal, uncertain” by the surgeon were combined, and likewise biopsies deemed “tumour” and “tumour, uncertain” were combined. Furthermore, biopsies that the pathologist classified as “infiltration zone” were combined with those classified as “tumour”. The ROC curves were constructed by calculating sensitivity and specificity for the three different possible cut-off points for surgeon’s judgment, one ROC curve for each phase of resection (Fig. 3).
ROC curves. ROC curves for the ability of ultrasound to distinguish tumour from normal tissue. a ROC curve before resection, showing high accuracy (AUC = 0.94). b ROC curve during resection. Compared to the ROC curve before resection the accuracy of ultrasound is decreased. (AUC = 0.69). c ROC curve after resection. Compared to the ROC curve before and during resection, the accuracy is further decreased (AUC = 0.65)
Results
Of 301 total biopsies acquired, 186 were included in our analyses. Table 1 shows the number of biopsies included/excluded in each phase of surgery. The histopathological diagnoses of the biopsies and the corresponding ultrasound findings for each of the stages of resection are shown in Table 2. The calculated values for specificity, sensitivity, NPV and PPV are listed in Table 3. Before resection, both sensitivity and specificity were 95%, while PPV and NPV were 98% and 90%, respectively. During resection, sensitivity was 88% but specificity had dropped to 42%. PPV and NPV was 73% and 67% respectively. After resection, sensitivity was 26% and specificity was 88%, while PPV and NPV both were 62%. The ROC curve for ultrasound in each stage of surgery is displayed in Fig. 3, and the area under the curve (AUC) is stated in the figure legend.
Although comparison of ultrasound and MRI was not a part of the study protocol, 16 of the 19 patients had early postoperative MRI (within 72 h). In 13 of these 16 patients the neurosurgeon also assessed the resection grade at the end of resection using 3D ultrasound. Among these, ten patients were considered either 90–95% or >95% resected. Two of the10 patients had residual tumour on early postoperative MRI; one patient considered 90–95% resected and another considered >95% resected. The other eight patients had no residual tumour found on early postoperative MRI. In the remaining three patients (of the 13 with both early postoperative MRI and resection grade assessment), residual tumour was intentionally left behind because of unacceptable risk of neurological damage. Two of them had residual tumour on postoperative MRI, while one was considered to possibly have residual tumour.
Sixteen of the 19 patients had a good outcome with no new neurological deficits.
Two of the patients had a fair outcome with mild new neurological deficits, and one patient had a poor outcome, with hemiparesis and aphasia. None of the patients had complications related to the procedure.
Discussion
General considerations
Delineation of gliomas poses a challenge to any imaging modality, as tumour cells infiltrate the normal brain tissue beyond the solid tumour border. In this sense, definition of a specific tumour border is impossible. For practical purposes, however, to delineate a glioblastoma usually means to outline the solid part of a tumour, of which removal is the goal of surgical resection.
Several authors have evaluated different diagnostic imaging modalities for delineation of gliomas, comparing image findings with histopathology [3, 5–7, 13, 16, 22, 23, 28, 32]. Also infiltrated brain tissue may be detected by new imaging techniques [28, 32]. In neuronavigation, intraoperative imaging is now increasingly recognized as important to amend for inaccuracy due to brain shift, and facilitate detection of residual tumour. Ultrasound and MRI are the commonly used modalities in this regard [12, 15, 26, 27, 36, 39]. However, it is not entirely known to what degree intraoperative factors affect intraoperative imaging, and the studies comparing image findings with histopathology in the intraoperative setting are scarce. Reporting on intraoperative MRI, Sutherland [34], found that intraoperatively, the contrast-enhancing margin advanced beyond the preoperatively defined contrast limits, and that biopsy samples from this zone contained tumour tissue. Knauth [14] argue that surgically induced contrast enhancement may be misinterpreted as residual tumour in intraoperative MRI, but only in one case was this confirmed with a biopsy, obtained in a contrast-enhancing area which proved to contain normal tissue. Surgically induced contrast enhancement in intraoperative MRI at the resection border, mimicking residual tumour, is also mentioned by other authors [26, 33, 39]. In ultrasound, reverberations, refraction of the ultrasound beam, artefacts due to slice thickness among others, may all cause imaging artefacts which may be misleading. During tumour resection, air bubbles, debris, blood, and the rough surface of the tumour cavity wall probably increase the occurrence of imaging artefacts in ultrasound. In addition other, unknown factors may affect the ultrasound images during the course of a tumour resection. Comparing ultrasound findings after (completed) resection, Chacko [4] found that biopsies taken from the tumour margins agreed with ultrasound image findings in the majority of samples, however, there were instances (16%) when the ultrasound reported tumour while the biopsies were negative. LeRoux et al. [18] used intraoperative ultrasound to facilitate gross total resection of brain tumours and obtained biopsies from the resection cavity wall after completed resection. They found that among 15 tumours not invading eloquent cortex and thus feasible for total resection, 11 cases (73%) had margins without solid tumour involvement although scattered tumour cells were found. Woydt et al. [40] published a study in 1996, to evaluate ultrasound findings after completed microsurgical resection of gliomas. Biopsies were obtained in (1) hyperechoic areas adjacent to the resection cavity and (2) the hyperechoic rim of the resection cavity. In group 1 (hyperechoic areas adjacent to resection cavity), high-grade glioma cases showed that 90% of biopsies contained tumour tissue, and the rest contained infiltrated tissue. For low-grade glioma cases 85% of biopsies in this group contained tumour tissue, the rest contained infiltrated tissue. Biopsies obtained at the hyperechoic rim (group 2) were heterogeneous, 26% revealed solid tumour tissue, 35% infiltration zone and 39% brain tissue (high-grade and low-grade gliomas combined). Our research group published a study in 2005 [38], comparing ultrasound findings with histopathology by obtaining tissue samples obtained in the tumour border zone before starting the resection. The ultrasound findings were in agreement with the histopathology in 77% of biopsies from glioblastoma cases and 83% and 74% for anaplastic astrocytomas and low-grade astrocytomas, respectively.
In the present paper we report on our results evaluating the ability of intraoperative ultrasound for delineation of gliobastomas before, during and after resection by comparing image findings from image guided biopsies with histopathology.
Discussion of findings
The conditions for ultrasound imaging before resection are probably close to optimal, and imaging artefacts should be at a minimum level. Before resection, sensitivity was 95% and specificity also was 95%. The PPV and NPV were 98% and 90%, respectively. This result shows that the ultrasound was highly accurate in delineating glioblastomas prior to resection. The sensitivity and specificity is slightly improved compared to our own study from 2005 [38]. This may be because of increased experience with ultrasound. The result also demonstrates that the sensitivity and specificity of ultrasound for predicting tumour/normal tissue, although operator dependent, is in the range of other, state of the art imaging techniques [16, 23, 28]. Thus, the sensitivity and specificity of ultrasound diagnosis in this phase serve as a baseline for comparison with subsequent phases.
During resection, a partial resection had been performed, with a resection cavity and some residual tumour left. The resection cavity wall, having a rough surface, as well as debris, small air bubbles, and blood all contribute to ultrasound imaging artefacts. The values of sensitivity and PPV were 87% and 73%; the specificity and NPV were 42% and 67%. The striking finding is a considerable decrease in specificity. This may be explained by a considerable amount of false positive biopsies; in nine biopsies, which contained normal tissue (as diagnosed by the pathologist), the diagnosis on ultrasound was “tumour”, and two were classified as “tumour, uncertain”. Several factors may explain the high false positive rate, both imaging artefacts and inherent error sources in the method of the study (discussed below). These numbers show that there may be some overestimation of tumour in this phase of surgery, but on the other hand, chances of overlooking areas with residual tumour tissue seem to be low (still high sensitivity).
After resection, leaving a cavity with the solid part of the tumour removed, biopsies were sampled in the resection cavity wall only. The same sources of imaging artefacts as discussed above also apply to this phase. The calculated values of sensitivity and PPV were 26% and 62%, while the values of specificity and NPV were 88% and 62%, respectively. The specificity was acceptable; reflecting that normal tissue in the majority of cases was correctly classified on ultrasound, important for patient safety. A sensitivity of 26% is discouraging, but calls for further considerations. First, the number of biopsies deemed “tumour” and “tumour, uncertain” were low in this stage of resection for obvious reasons. Also noteworthy is the high number of biopsies deemed “normal” and “normal, uncertain”, which contained either tumour tissue (four deemed “normal” and another four considered “normal, uncertain”) or tumour-infiltrated tissue (five deemed “normal” and ten deemed “normal, uncertain”). We are not surprised to find infiltrated brain tissue and small tumour remnants in the resection cavity wall, due to the infiltrating nature of glioblastomas. In their paper from 1996, Woydt et al. [40] reported that biopsies obtained from the “hyperechoic rim” of a resection cavity contained solid tumour (26%), infiltration zone (35%) and brain tissue (39%). For comparison, biopsies taken from the resection cavity (regardless of image finding) wall after resection in this study have a similar, although slightly more favourable distribution; solid tumour 21%; infiltration zone 22% and normal tissue 58%. Comparison of 3D ultrasound findings at the end of resection and early postoperative MRI was not a part of the study. Still, the fact that two of ten patients considered either >95% or 90–95% resected had residual tumour on early postoperative MRI may likewise reflect difficulties in interpreting 3D ultrasound after resection, or limitations of the 3D ultrasound itself.
In summary, the diagnostic accuracy of ultrasound for delineating glioblastomas was lower in the subsequent phases of surgery than before resection. During surgery there seemed to be some overestimation of tumour, but residual tumour was rarely missed. After resection, small tumour remnants and infiltrated tissue appeared as normal tissue on ultrasound, lowering the sensitivity. Still in most cases biopsies containing normal tissue were correctly classified with ultrasound.
Limitations of the study
Important limitations of the study method must be recognized due to the fact that the 3D ultrasound technique used in this study still is not real time; the biopsy sampling in itself, although performed as gently as possible, may cause some motion of tissue. Furthermore, in some cases that the walls of the resection cavity seemed to collapse a little inwardly when removing the saline after 3D ultrasound image acquisition to what degree these effects have affected the results in this study is not known.
Small and traumatized biopsy specimens in some cases prevented optimal histological examination. The surgeon did not have the opportunity to classify tissue as infiltrated brain tissue, while the pathologist did: Whether this introduces a bias is unknown.
The diagnostic accuracy of ultrasound is user dependent. The majority of biopsies were assessed by a surgeon with long experience using 3D ultrasound (GU), and the rest of the biopsies were assessed by a surgeon with shorter, but significant experience using ultrasound. Interobserver variability analysis on the interpretation of 3D ultrasound images was not done, and this is an important limitation of the current study. In our view, interpreting 3D ultrasound is dependent on interactive navigation, and using 2D snapshots postoperatively may not be sufficient for analysis of interobserver variability. We were not able to record biopsy positions in the 3D ultrasound dataset for postoperative review and analysis.
Systematic comparison of 3D ultrasound at the end of the resection and postoperative MRI was not done as it was not part of the study protocol.
Ethical aspects
The ethical aspects of intentional sampling of biopsies in the outer border of the tumour, as seen in the US images, were given consideration. Biopsies from outside of the US indicated border were never sampled in eloquent areas.
We did not see any complications that could be related to the biopsy sampling procedure.
Conclusions
Our study shows that while ultrasound is highly accurate in delineating glioblastomas before resection it appears less accurate during and after resection. During resection there seem to be some overestimation of tumour, while small tumour remnants and infiltrated tissue in the cavity wall is underestimated after resection. Due to inherent error sources in the study design, the results must be interpreted with caution. Intraoperative 3D ultrasound still seems a reasonably reliable modality for guidance of the resection of glioblastomas as the sensitivity during resection and the specificity after completed resection are acceptable.
Abbreviations
- US:
-
ultrasound
- 3D:
-
three dimensional
- MHz:
-
megahertz
- PPV:
-
positive predictive value
- NPV:
-
negative predictive value
- ROC:
-
receiver operating characteristics
- AUC:
-
area under curve
References
Albert FK, Forsting M, Sartor K, Adams HP, Kunze S (1994) Early postoperative magnetic resonance imaging after resection of malignant glioma: objective evaluation of residual tumour and its influence on regrowth and prognosis. Neurosurgery 34:45–60 discussion 60–41
Burger PC, Heinz ER, Shibata T, Kleihues P (1988) Topographic anatomy and CT correlations in the untreated glioblastoma multiforme. J Neurosurg 68:698–704
Chacko AG, Kumar NKS, Chacko G, Athyal R, Rajshekhar V (2003) Intraoperative ultrasound in determining the extent of resection of parenchymal brain tumours—a comparative study with computed tomography and histopathology. Acta Neurochirurgica 145:743–748
Croteau D, Scarpace L, Hearshen D, Gutierrez J, Fisher JL, Rock JP, Mikkelsen T (2001) Correlation between magnetic resonance spectroscopy imaging and image-guided biopsies: semiquantitative and qualitative histopathological analyses of patients with untreated glioma. Neurosurgery 49:823–829
Daumas-Duport C, Monsaigneon V, Blond S, Munari C, Musolino A, Chodkiewicz JP, Missir O (1987) Serial stereotactic biopsies and CT scan in gliomas: correlative study in 100 astrocytomas, oligo-astrocytomas and oligodendrocytomas. J Neurooncol 4:317–328
Ganslandt O, Stadlbauer A, Fahlbusch R, Kamada K, Buslei R, Blumcke I, Moser E, Nimsky C (2005) Proton magnetic resonance spectroscopic imaging integrated into image-guided surgery: correlation to standard magnetic resonance imaging and tumor cell density. Neurosurgery 56:291–298 discussion 291–298
Grønningsæter Å, Kleven A, Ommedal S, Årseth TE, Lie T, Lindseth F, Langø T, Unsgård G (2000) SonoWand, an ultrasound-based neuronavigation system. Neurosurgery 47:1373–1380
Hammoud MA, Ligon BL, elSouki R, Shi WM, Schomer DF, Sawaya R (1996) Use of intraoperative ultrasound for localizing tumors and determining the extent of resection: a comparative study with magnetic resonance imaging. J Neurosurg 84:737–741
Hirschberg H, Samset E, Hol PK, Tillung T, Lote K (2005) Impact of intraoperative MRI on the surgical results for high-grade gliomas. Minim Invasive Neurosurg 48:77–84
Iseki H, Muragaki Y, Nakamura R, Ozawa N, Taniguchi H, Hori T, Takakura K (2005) Intelligent operating theater using intraoperative open-MRI. Magn Reson Med Sci 4:129–136
Katisko JP, Koivukangas JP (2007) Optically neuronavigated ultrasonography in an intraoperative magnetic resonance imaging environment. Neurosurgery 60:373–380 discussion 380–371
Kelly PJ, Daumas-Duport C, Scheithauer BW, Kall BA, Kispert DB (1987) Stereotactic histologic correlations of computed tomography- and magnetic resonance imaging-defined abnormalities in patients with glial neoplasms. Mayo Clin Proc 62:450–459
Kleihues P, Cavenee WK (eds) (2000) Pathology and genetics of tumours of the nervous system: world health organization classification of tumours. IARC, Lyon
Knauth M, Aras N, Wirtz CR, Dorfler A, Engelhorn T, Sartor K (1999) Surgically induced intracranial contrast enhancement: potential source of diagnostic error in intraoperative MR imaging. AJNR Am J Neuroradiol 20:1547–1553
Koivukangas J, Louhisalmi Y, Alakuijala J, Oikarinen J (1993) Ultrasound-controlled neuronavigator-guided brain surgery. J Neurosurg 79:36–42
Kracht LW, Miletic H, Busch S, Jacobs AH, Voges J, Hoevels M, Klein JC, Herholz K, Heiss WD (2004) Delineation of brain tumor extent with [11C]l-methionine positron emission tomography: local comparison with stereotactic histopathology. Clin Cancer Res 10:7163–7170
Lacroix M, Abi-Said D, Fourney DR, Gokaslan ZL, Shi W, DeMonte F, Lang FF, McCutcheon IE, Hassenbusch SJ, Holland E, Hess K, Michael C, Miller D, Sawaya R (2001) A multivariate analysis of 416 patients with glioblastoma multiforme: prognosis, extent of resection, and survival. J Neurosurg 95:190–198
LeRoux PD, Winter TC, Berger MS, Mack LA, Wang K, Elliott JP (1994) A comparison between preoperative magnetic resonance and intraoperative ultrasound tumor volumes and margins. J Clin Ultrasound 22:29–36
Letteboer MM, Willems PW, Viergever MA, Niessen WJ (2005) Brain shift estimation in image-guided neurosurgery using 3-D ultrasound. IEEE Trans Biomed Eng 52:268–276
Lindner D, Trantakis C, Renner C, Arnold S, Schmitgen A, Schneider J, Meixensberger J (2006) Application of intraoperative 3D ultrasound during navigated tumor resection. Minim Invasive Neurosurg 49:197–202
Lindseth F, Lango T, Bang J, Nagelhus Hernes TA (2002) Accuracy evaluation of a 3D ultrasound-based neuronavigation system. Comput Aided Surg 7:197–222
Lunsford LD, Martinez AJ, Latchaw RE (1986) Magnetic resonance imaging does not define tumor boundaries. Acta Radiol Suppl 369:154–156
McKnight TR, von dem Bussche MH, Vigneron DB, Lu Y, Berger MS, McDermott MW, Dillon WP, Graves EE, Pirzkall A, Nelson SJ (2002) Histopathological validation of a three-dimensional magnetic resonance spectroscopy index as a predictor of tumor presence. J Neurosurg 97:794–802
Nimsky C, Ganslandt O, Buchfelder M, Fahlbusch R (2006) Intraoperative visualization for resection of gliomas: the role of functional neuronavigation and intraoperative 1.5 T MRI. Neurol Res 28:482–487
Nimsky C, Ganslandt O, Cerny P, Hastreiter P, Greiner G, Fahlbush R (2000) Quantification of, visulaization of, and compensating for brain shift using intraoperative magnetic resonance imaging. Neurosurgery 47:1070–1080
Nimsky C, Ganslandt O, Hastreiter P, Fahlbusch R (2001) Intraoperative compensation for brain shift. Surg Neurol 56:357–364 discussion 364–355
Nimsky C, Ganslandt O, von Keller B, Romstock J, Fahlbusch R (2004) Intraoperative high-field-strength MR imaging: implementation and experience in 200 patients. Radiology 233:67–78
Price SJ, Jena R, Burnet NG, Hutchinson PJ, Dean AF, Pena A, Pickard JD, Carpenter TA, Gillard JH (2006) Improved delineation of glioma margins and regions of infiltration with the use of diffusion tensor imaging: an image-guided biopsy study. AJNR Am J Neuroradiol 27:1969–1974
Reinges MHT, Nguyen HH, Krings T, Hutter BO, Rohde V, Gilsbach JM (2004) Course of brain shift during microsurgical resection of supratentorial cerebral lesions: limits of conventional neuronavigation. Acta Neurochirurgica 146:369–377
Rubin JM, Dohrmann GJ (1985) Efficacy of intraoperative US for evaluating intracranial masses. Radiology 157:509–511
Sergeeva O, Uhlemann F, Schackert G, Hergeth C, Morgenstern U, Steinmeier R (2006) Integration of intraoperative 3D-ultrasound in a commercial navigation system. Zentralbl Neurochir 67:197–203
Stadlbauer A, Ganslandt O, Buslei R, Hammen T, Gruber S, Moser E, Buchfelder M, Salomonowitz E, Nimsky C (2006) Gliomas: histopathologic evaluation of changes in directionality and magnitude of water diffusion at diffusion-tensor MR imaging. Radiology 240:803–810
Steinmeier R, Fahlbusch R, Ganslandt O, Nimsky C, Buchfelder M, Kaus M, Heigl T, Lenz G, Kuth R, Huk W (1998) Intraoperative magnetic resonance imaging with the magnetom open scanner: concepts, neurosurgical indications, and procedures: a preliminary report. Neurosurgery 43:739–747 discussion 747–738
Sutherland GR, Kaibara T, Louw D, Hoult DI, Tomanek B, Saunders J (1999) A mobile high-field magnetic resonance system for neurosurgery. J Neurosurg 91:804–813
Unsgaard G, Gronningsaeter A, Ommedal S, Nagelhus Hernes TA (2002) Brain operations guided by real-time two-dimensional ultrasound: new possibilities as a result of improved image quality. Neurosurgery 51:402–411 discussion 411–402
Unsgaard G, Ommedal S, Muller T, Gronningsaeter A, Nagelhus Hernes TA (2002) Neuronavigation by intraoperative three-dimensional ultrasound: initial experience during brain tumor resection. Neurosurgery 50:804–812 discussion 812
Unsgaard G, Rygh OM, Selbekk T, Muller TB, Kolstad F, Lindseth F, Hernes TA (2006) Intra-operative 3D ultrasound in neurosurgery. Acta Neurochir (Wien) 148:235–253
Unsgaard G, Selbekk T, Brostrup Muller T, Ommedal S, Torp SH, Myhr G, Bang J, Nagelhus Hernes TA (2005) Ability of navigated 3D ultrasound to delineate gliomas and metastases–comparison of image interpretations with histopathology. Acta Neurochir (Wien) 147:1259–1269 discussion 1269
Wirtz CR, Knauth M, Staubert A, Bonsanto MM, Sartor K, Kunze S, Tronnier VM (2000) Clinical evaluation and follow-up results for intraoperative magnetic resonance imaging in neurosurgery. Neurosurgery 46:1112–1120 discussion 1120–1112
Woydt M, Krone A, Becker G, Schmidt K, Roggendorf W, Roosen K (1996) Correlation of intra-operative ultrasound with histopathologic findings after tumour resection in supratentorial gliomas. A method to improve gross total tumour resection. Acta Neurochir (Wien) 138:1391–1398
Author information
Authors and Affiliations
Corresponding author
Additional information
Comment
There are only few papers analyzing the validity of intraoperative ultrasound findings. One possibility is to correlate the intraoperative ultrasound images with early postoperative MR images to see whether there are any discrepancies in the evaluation of tumour resection. This does not account for that a tumour margin in MR images does not exactly reflect the biological tumour margin, which actually does not exist. Morten et al. correlated histopathology findings with intraoperative ultrasound to analyze whether intraoperative ultrasound is able to distinguish tumour and normal brain. Navigated tissue samples were taken at various stages of surgery at the tumour border. This study clearly shows that intraoperative ultrasound is a reliable tool to evaluate the extent of a tumour at the beginning of surgery. However, after resection of major tumour parts sensitivity dramatically decreased, surgically induced changes at the tumour border led to false image interpretation, reducing the value of intraoperative ultrasound being used for resection control. To which extent this effect also depends on the ultrasound technology is an open question. Ultrasound imaging has undergone impressive improvements in the last years, so that these shortcomings might be solved in the near future. The authors are to be encouraged to continue their innovative work; the combination of intraoperative ultrasound with histology compared with early postoperative MR images will result in further information on the validity of intraoperative ultrasound.
Christopher Nimsky
Erlangen, Germany
Rights and permissions
About this article
Cite this article
Rygh, O.M., Selbekk, T., Torp, S.H. et al. Comparison of navigated 3D ultrasound findings with histopathology in subsequent phases of glioblastoma resection. Acta Neurochir (Wien) 150, 1033–1042 (2008). https://doi.org/10.1007/s00701-008-0017-3
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-008-0017-3