Abstract
Background
Reliable intraoperative resection control during surgery of malignant brain tumours is associated with the longer overall survival of patients. B-mode ultrasound (BUS) is a familiar intraoperative imaging application in neurosurgical procedures and supplies excellent image quality. However, due to resection-induced artefacts, its ability to distinguish between tumour borders, oedema, surrounding tissue and tumour remnants is sometimes limited. In experienced hands, this “bright rim effect” could be reduced. However, it should be determined, if contrast-enhanced ultrasound can improve this situation by providing high-quality imaging during the resection. The aim of this clinical study was to examine contrast-enhanced and three-dimensional reconstructed ultrasound (3D CEUS) in brain tumour surgery regarding the uptake of contrast agent pre- and post-tumour resection, imaging quality and in comparison with postoperative magnetic resonance imaging in different tumour entities.
Methods
Fifty patients, suffering from various brain tumours intra-axial and extra-axial, who had all undergone surgery with the support of neuronavigation in our neurosurgical department, were included in the study. Their median age was 56 years (range, 28–79). Ultrasound imaging was performed before the Dura was opened and for resection control at the end of tumour resection as defined by the neurosurgeon. A high-end ultrasound (US) device (Toshiba Aplio XG®) with linear and sector probes for B-mode and CEUS was used. Navigation and 3D reconstruction were performed with a LOCALITE SonoNavigator® and the images were transferred digitally (DVI) to the navigation system. The contrast agent consists of echoic micro-bubbles showing tumour vascularisation. The ultrasound images were compared with the corresponding postoperative MR data in order to determine the accuracy and imaging quality of the tumours and tumour remnants after resection.
Results
Different types of tumours were investigated. High, dynamic contrast agent uptake was observed in 19 of 21 patients (90 %) suffering from glioblastoma, while in 2 patients uptake was low and insufficient. In 52.4 % of glioblastoma and grade III astrocytoma patients CEUS led to an improved delineation in comparison to BUS and showed a high-resolution imaging quality of the tumour margins and tumour boarders. Grade II and grade III astrocytoma (n = 6) as well as metastasis (n = 18) also showed high contrast agent uptake, which led in 50 % to an improved imaging quality. In 5 of these 17 patients, intraoperative CEUS for resection control showed tumour remnants, leading to further tumour resection. Patients treated with CEUS showed no increased neurological deficits after tumour resection. No pharmacological side-effects occurred.
Conclusions
Three-dimensional CEUS is a reliable intraoperative imaging modality and could improve imaging quality. Ninety percent of the high-grade gliomas (HGG, glioblastoma and astrocytoma grade III) showed high contrast uptake with an improved imaging quality in more than 50 %. Gross total resection and incomplete resection of glioblastoma were adequately highlighted by 3D CEUS intraoperatively. The application of US contrast agent could be a helpful imaging tool, especially for resection control in glioblastoma surgery.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
B-mode ultrasound (BUS) has been a common technique in intraoperative neurosurgical procedures since the early 1980s. It is easy to use and is a standard acquisition tool for real-time imaging [1–5]. Real-time imaging provides the neurosurgeon with continuous guidance. However, BUS might have limitations when it comes to describing clearly tumour, tumour borders and surrounding tissue, oedema and even tumour remnants because of artefacts induced by the resection [2, 6]. Further developments in the field of ultrasound have been driven by cardiology and hepatology, and resulted in high-resolution imaging quality whose degree of detail is comparable to that of magnetic resonance imaging (MRI). Different ultrasound probes are available for different frequencies to describe the approached tumour in different depths for optimal intraoperative visualisation of the lesion. Moreover, intraoperative imaging quality and guidance have been improved by combining three-dimensional (3D) reconstruction and integrated navigation systems to minimise surgical artefacts during or after the resection [2, 3, 6–13].
Neuronavigation helps to identify the lesions at the beginning of the operation, and it can be used before craniotomy to minimise collateral damage [5]. However, as the operation proceeds, the brain shift phenomenon makes adequate intraoperative imaging essential for tumour identification and resection control [7, 13–15].
Over the past 10–15 years, the use of intraoperative MRI has demonstrated that resection control and the extent of resection are factors leading to a longer survival of glioma patients [16]. However, intraoperative MRI systems are too expensive for most neurosurgical departments. Furthermore, it is a time-consuming imaging acquisition.
For many years, 2D and 3D intraoperative BUS has been an established imaging tool for tumour visualisation and resection. In 2008/2009, trials began to test the effectiveness of 3D reconstructed and contrast-enhanced ultrasound (CEUS) in the neurosurgical resection of brain tumours by using ultrasound contrast agent [2, 10, 11, 13]. This led to a protocol for tumour and tumour remnant visualisation in which 3D BUS and 3D CEUS datasets were compared with MRI before and after tumour resection [17]. Actually no prospective study showed the effectiveness of 3D CEUS in brain tumour surgery. We performed this prospective study to investigate 3D CEUS before and after resection in surgery of different brain tumour entities regarding contrast agent uptake as well as a comparison to 3D BUS and MRI (preoperative and postoperative) and the feasibility of resection control and improved real-time imaging.
Methods
A prospective phase IIb mono-centre study was conducted funded by the German Research Foundation (Deutsche Forschungsgemeinschaft [DFG]). The study was approved and monitored by the Federal Institute for Drugs and Medical Devices (Bundesagentur für Arzneimittelsicherheit [BfArM]) and the University of Leipzig’s ethics committee. The contrast agent used was SonoVue® (Bracco, Milan, Italy). This agent is not certified for intraoperative use in brain tumour surgery in Germany, which was why we initiated this phase IIb trial. The inclusion criteria were consistent with ICH good clinical practice (GCP) in clinical trials. All patients signed an informed consent form and were insured throughout the study period. All side-effects, adverse events (AEs) and severe adverse events (SAEs) were recorded.
From April 2011 to January 2013, we included 50 patients suffering from a brain tumour. Preoperative and postoperative (within 48 h postoperatively) T1-weighted 3D MRI with gadolinium (slice thickness 0.5–1 mm) was performed on all patients. The neuronavigation system used during the surgery was LOCALITE (Sankt Augustin, Germany) with SonoNavigator® software. Landmark and surface registration led to a maximum deviation of up to 1.5 mm in each case.
The Aplio XG® (Toshiba Medical Systems Europe, Zoetermeer, The Netherlands) high-end system was used as the ultrasound device. Depending on the size of the craniotomy and the depth of the lesion, one of three different ultrasound probes was employed. All probes were tracked, enabling integration into neuronavigation. A large linear array transducer (probe PLT704SBT; contact area, 13 × 46 mm; frequency range, 4.8–11.0 MHz; Fig. 1), a small convex transducer (probe PVT-745BTV; frequency range, 4.0–11.0 MHz) and a small phased array transducer (probe PST-65AT; frequency range, 4.2–8.5 MHz) were used. All ultrasound probes can work in contrast-enhanced mode with the Aplio XG preset for contrast agent use.
The ultrasound contrast agent SonoVue (Bracco, Milan, Italy) consists of micro-bubbles with a diameter of 1 μm containing an echoic gas (sulphur hexafluoride [SF6]). In total, 4.8 ml SonoVue was applied at the start of imaging. At first, a bolus dose of 1.5 ml SonoVue was applied to describe the ultrasound perfusion features of the tumour. Then a continuous rotating infusion system (ACIST VueJect®, 3 ml/h) was used for intravenous application before and after tumour resection. The continuous injection is needed because of the short half-life of the contrast agent of 2–5 min. Afterwards it decomposes spontaneously into gas, which is excreted over the lungs and the lipid shell. In other medical disciplines, such as cardiology and hepatology, the contrast agent has been used for many years without known complications besides an allergic reaction in a very small number of cases (<1/1,000 patients). Actually no negative effects were reported in CNS administration like in stroke patients [9, 18–20] .
The 3D BUS and 3D CEUS scans before tumour resection were performed after craniotomy and before opening the dura. Therefore, different ultrasound probes were available for different sized craniotomies and different depths. The craniotomy was not fitted to the ultrasound probe because the study design did not allow changing the operation steps in this particular case.
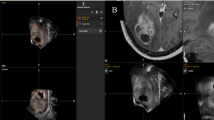
When the neurosurgeon stopped tumour resection, a 3D BUS and a 3D CEUS scan were carried out. The ultrasound data were transferred to the neuronavigation system via DVI® (Digital Visual Interface) without loss of quality or information. A 3D volume was calculated by the SonoNavigator software and superimposed on the corresponding MRI data (Figs. 2 and 3). Whenever tumour remnants were observed in the resection control, a further navigated tumour resection was performed if gross total resection or more tumour debulking was possible.
Postoperatively, the segmentation of the US and MR datasets was mainly carried out with the open-source software ITK-SNAP (http://www.itksnap.org/). Preoperative and postoperative MRI data were registered in a two-step procedure (anatomical landmarks followed by a mutual information algorithm) in the SonoNavigator (LOCALITE). The overlapping 3D tumour volumes were visualised with the open-source MITK® software (http://www.mitk.org/wiki/The_Medical_Imaging_Interaction_Toolkit_(MITK)).
An ultrasound scoring system was defined to describe the quality of tumour imaging at the beginning of tumour removal in order to compare 3D B-mode and 3D CEUS.
-
Good: tumour margins are clearly distinguishable from the surrounding brain structures and tumour details are accurately represented
-
Middle: although tumour intensities differ from the healthy brain, the tumour boundary is not well defined and hard to delineate
-
Bad: the tumour is poorly or not visible
Comparison of 3D B-mode and 3D CEUS data from the same patient led to assignment to one of the following three groups:
-
Group A: the use of contrast agent improved the image of the brain tumour
-
Group B: the quality of the tumour image was the same in the 3D intraoperative US and the 3D CEUS data
-
Group C: the representation of the tumour was worse in the 3D CEUS data than in the 3D intraoperative US data
To verify the specificity and sensitivity of 3D CEUS at the end of resection, navigated biopsies were taken. At least three biopsies were planned on the LOCALITE Workstation. All biopsies were planned in the area of a contrast agent absorbing remnant or at the resection border without harming eloquent areas.
Results
The histological findings of the 50 patients included are shown in Table 1. There were 21 patients with glioblastoma (including 2 with recurrent tumours), 2 with astrocytoma grade III (1 recurrent tumour), 4 with astrocytoma grade II, 2 with oligodendroglioma grade II, 18 with metastasis (1 recurrent tumour) and 3 with meningioma (1 grade I meningioma, 1 grade II meningioma, 1 recurrent grade III meningioma).
The imaging quality for each histology finding is shown in Tables 2 and 3.
During the study period, no pharmacological side-effects occurred during the application of contrast agent. We observed no SAEs or SUSARs, as defined in the study protocol, to draw inferences from the contrast agent. As might be considered, the use of CEUS led to no further neurological worsening after the operation. We noticed nearly the same numbers of neurological deficits as in patients treated without CEUS. In four of the GBM and in five of the metastasis patients, a neurological worsening occurred. This was defined as new or deteriorated hemiparesis, aphasia, seizure or confusion. In five GBM patients, an amendment of a neurological deficit was observed.
Tumour segmentation was performed by a neurosurgeon and a scientific assistant to minimise deviations. For the different tumour entities the results are represented in Table 4. The mean tumour volume for glioblastoma patients was 30.4 cm3 (standard deviation [SD], 23.1) and 19.4 cm3 for metastasis (SD, 16.9) measured in MRI. In 3D CEUS, the mean tumour volume was 25.2 cm3 (SD, 21.2) and in BUS 24.1 cm3 (SD, 17.3) for glioblastoma patients. For metastasis the mean tumour volume was 19.8 cm3 (SD, 14.7) in CEUS and 16.6 cm3 (SD, 12.9) in BUS. In astrocaytoma grade II and III the US volumes were larger than the MRI volume. No statistical significance could be shown in the volumetric data between MRI, CEUS and BUS in glioblastoma, astrocytoma and metastasis patients.
Before resection
Glioblastoma multiforme and anaplastic astrocytoma (grade III)
In 19 of 21 patients (90 %) suffering from glioblastoma, high, dynamic contrast agent uptake was measured, whereas in two patients uptake was low and insufficient. In 86 % of patients with glioblastoma, 3D CEUS resulted in equivalent or better tumour imaging than BUS (Figs. 4 and 5). In 52.4 %, delineation and imaging were improved by CEUS. We observed a fast arterial and venous phase after bolus injection. The tumour was always well distinguished from the normal brain tissue. The contrast pattern in CEUS could hence be predictive for malignant brain tumours when used for intraoperative imaging.
Both anaplastic astrocytoma were assigned to group A and B (recurrent tumour) and completely removed according to MRI criteria.
Astrocytoma and oligodendroglioma (grade II)
All six patients with astrocytoma or oligodendroglioma (grade II) showed an uptake of contrast agent (Fig. 6). Improved image quality was observed in 50 % of cases (group A). Both oligodendrogliomas showed no better imaging in 3D CEUS than B-mode and were assigned to group B. Resection control using 3D CEUS was not possible.
Metastasis and meningioma
In 89 % of all patients with metastasis, 3D CEUS showed equivalent or better tumour imaging than B-mode. In 44.4 %, delineation and presentation were improved by CEUS.
All patients with meningioma showed completely different contrast agent uptake in comparison to gadolinium uptake in MRI. Grade II meningeoma showed no contrast agent uptake in CEUS, while grade I and grade III tumours showed high delineation after US contrast agent application.
After resection
Intraoperative biopsies
Forty-five navigated biopsies from resection margins in 15 glioblastoma patients were taken. In 6 of 21 patients, no biopsies after tumour resection were performed because of intraoperative brain swelling and eloquent localisation or poor imaging quality.
In 45 biopsies, 27 were located in areas of contrast agent uptake, 12 of them showed tumour (44 %), 11 samples showed tumour infiltration (41 %) and 4 samples were tumour-negative. Eighteen biopsies were not located in an area of contrast agent uptake, 5 showed no tumour (28 %), in 3 samples tumour was detected and 10 samples showed tumour infiltration. A sensitivity of 85 % and a specificity of 28 % for tumour in areas of contrast agent uptake were calculated (Table 5).
Resection control
We analysed 21 patients with a glioblastoma. In 13 of the 21 patients, a gross total resection (GTR) and in 8 cases a subtotal resection was planned before the operation. We achieved in 8 of these 13 patients a GTR (62 %) with no tumour remnant in the postoperative MRI. In 5 of the 13 patients, no GTR was achieved according to MRI criteria. In three of these cases, 3D CEUS showed tumour remnants as did postoperative MRI. In two cases, intraoperative 3D CEUS showed no tumour remnant, whereas postoperative MRI did; in these cases the tumour remnant volume was >0.175 cm3.
In 7 of the 13 patients, 3D CEUS demonstrated a tumour remnant after the surgeon had stopped resection. Additional resection was performed in five of these cases after 3D CEUS had shown tumour remnants (Fig. 6). In four of these cases, postoperative MRI showed complete resection; in one case, a small tumour remnant was demonstrated. In the remaining two cases, no further resection was performed owing to localisation near an eloquent area.
No gross total resection was planned in 8 of the 21 glioblastoma patients. In seven patients, a subtotal resection (>90 % tumour mass) and in one case a tumour biopsy was planned. In seven cases, 3D CEUS as well as postoperative MRI showed tumour remnants; in one of these cases, complete resection was achieved.
Discussion
During the study period, we did not observe side-effects caused by SonoVue. Its application is safe and does not harm the patient. The short pharmacological half-life indicated no negative effect for the central nervous system, such as micro-embolisms or minimal strokes. The postoperative MRI also showed no hints of any negative effects. Despite the fact of a more radical resection, caused by intraoperative CEUS for visualisation of tumour remnants, we observed no increased number of severe and continuing postoperative neurological deficits in comparison to patients treated without CEUS.
The visualisation and comparison to the MRI as the standard imaging application were realised by a reconstruction of the tracked US slices, superimposed on the corresponding MRI data. This navigated reconstruction allows resection to be verified in real time intraoperatively and as well as offline analysis.
This enabled additional tumour resection in different types of operations where a gross total resection was demonstrated in the postoperative MRI. In glioma surgery, this method seems to be an effective technique to approach the goal of gross total resection. Although this has already been shown in the literature, our study is the first prospective and monitored controlled trial [21–26].
In the majority of cases in our study, 3D CEUS reliably detected the tumour before and after resection in malignant brain tumours. Thus, this technique could be used for intraoperative resection control. In meningeomas, the contrast agent behaved very differently and did not match the WHO grades.
To compare MRI and CEUS, an understanding of the different principles and pathophysiological modes of action of MRI contrast agent and US contrast agent is essential. MRI contrast agent shows areas were the blood–brain barrier is damaged, whereas US contrast agent shows tumour vascularisation. The exact effect on our data remains unclear. Areas of contrast agent uptake seem to be very similar in MRI and CEUS. Also, we can state that a contrast uptake in MRI predicts a contrast agent uptake in CEUS. Even tumours not taking up MRI contrast agent showed in most of the cases an uptake in CEUS; for example, astrocytomas grade II and III. This supports our suggestion that in these tumours the blood–brain barrier is intact but we find tumour vascularisation with a higher number of vessels.
Modern intraoperative US during neurosurgical surgery achieved imaging quality comparable to MRI with high resolution [1, 6, 9]. After the application of contrast agent, the delineation of the tumour borders and adjacent vessels is even better than in MRI. Moreover, the neurosurgeon has a dynamic, real-time view. Different US probes are available and most of the devices can handle contrast agent in different presets with low energy to avoid damaging the micro-bubbles. In our opinion, linear probes with mid-to-high frequencies are most suitable for brain tumour surgery. With such a probe, lesions near the surface as well as deep tumours could be visualised with a high imaging quality. Another advantage of CEUS is the better delineation of the tumour boarders and the reduction of artefacts due to reduced power. This is necessary because otherwise the contrast agent bubbles will be destroyed. In this manner such artefacts, like in cystic tumours in BUS, are reduced or even absent (see Fig. 4).
In this study the size of the craniotomy was defined by the surgeon without consideration for the size of the probe. So in some cases no linear probe could be used, which might have had an influence on the imaging quality. In future, the craniotomy should be large enough to ensure the use of linear probes, which provide the best imaging quality.
To achieve a good imaging quality, even at the end of the resection, the position of the patient is crucial. By changing the position of the operating table, in most cases the BUS and CEUS could be performed without losing imaging quality.
Developing scoring systems to estimate the quality of BUS and CEUS helps these two imaging applications to be compared. CEUS is rarely used in neurosurgery and few relevant papers are available [17, 21–26]. Prada et al. found CEUS to be a useful tool in real-time imaging during neurosurgical operations, and different brain tumours were characterised in this CEUS study. Description after contrast agent application in this study was mainly qualitative. In another clinical study, both low-grade and high-grade gliomas were characterised intraoperatively [27]. High ultrasound contrast agent uptake after bolus injection was observed even in malignant brain tumours.
In contrast, in our prospective study we focused on describing the behaviour of US contrast agent in different brain tumour entities and evaluating the possibility for resection control as an intraoperative imaging application. We compared US data to preoperative and postoperative MRI data. For this purpose, the 3D datasets of the MRI, BUS and CEUS were segmented offline after resection, enabling quantitative analysis.
The segmentation allows the comparison of the different tumour volumes in different imaging modalities. In glioblastoma and metastasis, the tumour volumes in MRI were slightly larger than in the US volumes. BUS and CEUS volumes were nearly equal, whereas the CEUS volume was a little larger. In astrocytomas, the US volumes were enlarged in comparison to MRI volumes. This might be explained because the CEUS showed tumour vascularisation that is apparently greater than the T2-weighted areas in MRI.
Additionally, the areas of US contrast agent uptake were examined by navigated biopsies which showed high sensitivity of 85 %. The low specificity could be explained by the well-known tissue infiltration of malignant brain tumours.
A new scoring system was defined for the qualitative imaging description of different tumour entities in order to compare BUS and CEUS before resection. This showed improved imaging quality after contrast agent application even in high-grade gliomas. The delineation of tumour borders and visualisation of tumour remnants after resection was enhanced. Quantitative analyses to compare BUS, CEUS and MRI (preoperative and postoperative) were also performed based on postoperative data segmentation.
To confirm the effectiveness of this advanced ultrasound imaging technique, the number of investigated patients must be increased. In our opinion, a multicentre study could help us to evaluate the impact of this technique on brain tumour surgery. Moreover, US-based real-time neuronavigation could be improved by further technical developments, such as the integration of functional data like fMRI or neurophysiological monitoring. The combined application of CEUS and 5-ALA in malignant brain tumour surgery could improve the extent of resection as well.
References
Coburger J, König RW, Scheuerle A, Engelke J, Hlavac M, Thal DR, Wirtz CR (2014) Navigated high frequency ultrasound: description of technique and clinical comparison with conventional intracranial ultrasound. World Surg 82:366–75
Lindner D, Trantakis C, Arnold S, Schmitgen A, Schneider J, Meixensberger J (2005) Neuronavigation based on intraoperative 3D-ultrasound during tumor resection. Proceedings of computer assisted radiology and surgery. CARS. 815–820
Selbekk T, Jakola AS, Solheim O (2013) Ultrasound imaging in neurosurgery: approaches to minimize surgically induced image artefacts for improved resection control. Acta Neurochir (Wein) 155:973–980
Unsgaard G, Gronningsaeter A, Ommedal S, Nagelhus Hernes TA (2002) Brain operations guided by real-time two-dimensional ultrasound: new possibilities as a result of improved image quality. Neurosurgery 51:402–412
Willems PW, Taphoorn MJB, Burger H, van der Sprenkel JWB, Tulleken CAF (2006) Effectiveness of neuronavigation in resecting solitary intracerebral contrast-enhancing tumors: a randomized controlled trial. J Neurosurg 104:360–368
Unsgaard G, Ommedal S, Muller T, Gronningsaeter A, Nagelhus Hernes TA (2002) Neuronavigation by intraoperative three-dimensional ultrasound: initial experience during brain tumor resection. Neurosurgery 50:804–812
Busse H, Schmitgen A, Trantakis C, Schober R, Kahn T, Moche M (2006) Advanced approach for intraoperative MRI guidance and potential benefit for neurosurgical applications. J Magn Reson Imaging 24:140–151
Chalopin C, Krissian K, Meixensberger J, Müns A, Arlt F, Lindner D (2013) Evaluation of a semi-automatic segmentation algorithm in 3D intraoperative ultrasound brain angiography. Biomed Tech 58:293–30
Kaps M, Legemate DA, Ries F, Ackerstaff RG, Markus H, Pezzoll C, Llull JB, Spinazzi A (2001) SonoVue in transcranial Doppler investigations of the cerebral arteries. J Neuroimaging 11:261–7
Mert A, Buehler K, Sutherland GR, Tomanek B, Widhalm G, Kasprian G, Knosp E, Wolfsberger S (2012) Brain tumor surgery with 3-dimensional surface navigation. Neurosurgery 71:286–94
Müns A, Mühl C, Haase R, Möckel H, Chalopin C, Meixensberger J, Lindner D (2014) A neurosurgical phantom-based training system with ultrasound simulation. Acta Neurochir (Wein) 156:1237–43
Renovanz M, Hickmann AK, Henkel C, Nadji-Ohl M, Hopf NJ (2014) Navigated versus non-navigated intraoperative ultrasound: is there any impact on the extent of resection of high-grade gliomas? A retrospective clinical analysis. Neurol Surq A Centr Eur Neurosurq 75:224–30
Trantakis C, Meixensberger J, Lindner D, Strauss G, Grunst G, Schmidtgen A, Arnold S (2002) Iterative neuronavigation using 3D ultrasound. A feasibility study. Neurol Res 24:666–670
Lindseth F, Kaspersen JH, Ommedal S (2003) Multimodal image fusion in ultrasound-based neuronavigation: improving overview and interpretation by integrating preoperative MRI with intraoperative 3D ultrasound. Comput Aided Surg 8:49–69
Reinertsen I, Lindseth F, Askeland C, Iversen DH, Unsgård G (2014) Intra-operative correction of brain-shift. Acta Neurochir (Wein) 156:1301–10
Senft C, Bink A, Franz K, Vatter H, Gasser T, Seifert V (2011) Intraoperative MRI guidance and extent of resection in glioma surgery: a randomised, controlled trial. Lancet Oncol 12:997–1003
Prada F, Perin A, Martegani A (2014) Intraoperative contrast enhanced ultra-sound (iCEUS) for brain surgery. Neurosurgery 74:542–552
Kate GL, van Dijk AC, van den Oord SC, Hussain B, Verhagen HJ, Sijbrands EJ, van der Steen AF, van der Lugt A, Schinkel AF (2013) Usefulness of contrast-enhanced ultrasound for detection of carotid plaque ulceration in patients with symptomatic carotid atherosclerosis. Am J Cardiol 112:292–8
Nanda NC, Wistran DC, Karlsberg RP, Hack TC, Smith WB, Foley DA, Picard MH, Cotter B (2002) Multicenter evaluation of SonoVue for improved endocardial border delineation. Echocardiography 19:27–36
Park KH, Kwon SH, Lee YS, Jeong SW, Jang JY, Lee SH, Kim SG, Cha SW, Kim YS, Cho YD, Kim HS, Kim BS, Kim YJ (2015) Predictive factors of contrast-enhanced ultrasonography for the response to transarterial chemoembolization in hepatocellular carcinoma. Clin Mol Hepatol 21:158–64
Bogdahn U, Fröhlich T, Becker G (1994) Vascularization of primary central nervous system tumors: detection with contrast-enhanced transcranial color-coded real-time sonography. Radiology 192:141–148
Claudon M, Cosgrove D, Albrecht T (2008) Guidelines and good clinical practice recommendations for contrast enhanced ultrasound (CEUS)—update 2008. Ultraschall Med 29:28–44
Engelhardt M, Hansen C, Eyding J (2007) Feasibility of contrast-enhanced sonography during resection of cerebral tumours: initial results of a prospective study. Ultrasound Med Biol 33:571–575
He W, Jiang X-Q, Wang S (2008) Intraoperative contrast-enhanced ultrasound for brain tumors. Clin Imaging 32:419–424
Prada F, Mattei L, DelBene M, Aiani L, Saini M (2014) Intraoperative cerebral glioma characterization with contrast enhanced ultrasound. Biomed Res Int. 484261
Quaia E (2011) Assessment of tissue perfusion by contrast-enhanced ultrasound. Eur Radiol 21:604–615
Woydt M, Krone A, Becker G, Schmidt K, Roggendorf W, Roosen K (1996) Correlation of intra-operative ultrasound with histopathologic findings after tumour resection in supratentorial gliomas. A method to improve gross total tumour resection. Acta Neurochir (Wein) 138:1391–1398
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Funding
DFG (Deutsche Forschungsgemeinschaft) provided financial support in the form of hardware and personal costs funding. The sponsor had no role in the design or execution of this research.
Human and Animal Rights and Informed Consent
All procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards.
Informed consent was obtained from all individual participants included in the study.
Conflicts of interest
None.
Additional information
This study was supported by a DFG grant (Deutsche Forschungsgemeinschaft).
Registered in the EU Clinical Trials Register: https://www.clinicaltrialsregister.eu/ctr-search/search?query=eudract_number:2010-022057-42
Rights and permissions
About this article
Cite this article
Arlt, F., Chalopin, C., Müns, A. et al. Intraoperative 3D contrast-enhanced ultrasound (CEUS): a prospective study of 50 patients with brain tumours. Acta Neurochir 158, 685–694 (2016). https://doi.org/10.1007/s00701-016-2738-z
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00701-016-2738-z