Abstract
Purpose
The prognostic significance of the cachexia index, a novel biomarker of cancer cachexia, remains unclear in colorectal cancer; we, therefore, evaluated this relationship.
Methods
This retrospective cohort study included 306 patients with stage I–III colorectal cancer who underwent R0 resection between April 2010 and March 2020. The cachexia index was calculated as (skeletal muscle index [cm2/m2] × serum albumin level [g/dL])/neutrophil-to-lymphocyte ratio. The overall and disease-free survival rates were analyzed using a Cox proportional hazards model.
Results
A low cachexia index was found in 94 patients. This group had significantly lower disease-free survival and overall survival than the high-cachexia index group (5-year survival, 86.3% vs. 63.1%, p < 0.01; 87.9% vs. 67.2%, p < 0.01). Multivariate analyses showed that T3 or T4 (hazard ratio [HR]: 2.56; 95% confidence interval CI 1.04–6.25, p = 0.039), stage III (HR: 3.77; 95% CI 1.79–7.93, p < 0.01), and a low cachexia index (HR: 2.27; 95% CI 1.31–3.90, p = 0.003) were significant independent predictors of the disease-free survival. CA19-9 ≥ 37.0 ng/mL (HR: 2.68; 95% CI: 1.37–5.24, p = 0.004), stage III (HR: 2.57; 95% CI 1.34–4.92, p = 0.004), and a low cachexia index (HR: 2.35; 95% CI 1.31–4.21, p = 0.004) were significant independent predictors of the overall survival.
Conclusion
A low cachexia index might be a long-term prognostic factor of colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third-most commonly diagnosed cancer and the fourth leading cause of death worldwide [1]. Recently, minimally invasive surgery and intensified chemotherapy have improved CRC outcomes; however, there are still patients with a poor prognosis that need to be identified.
Over time, cachexia has been recognized as a serious adverse effect of cancer. Cancer cachexia is defined as a multifactorial syndrome characterized by a persistent loss of skeletal muscle mass that cannot be fully recovered by conventional nutritional support and leads to progressive dysfunction [2, 3]. Cancer cachexia has been associated with poor clinical outcomes, such as weight loss, loss of appetite, a decreased quality of life, reduced response to chemotherapy treatment, poor compliance, increased adverse effects, and a poor prognosis [4, 5].
The diagnostic criteria for cachexia established by the European Palliative Care Research Collaborative (EPCRC) include weight loss and sarcopenia [3]; however, these diagnostic criteria are unclear and difficult to apply in clinical practice. The cachexia index (CXI), first developed by Jafri et al. in 2015, is a novel biomarker that consists of the skeletal muscle index (SMI), serum albumin level, and neutrophil–lymphocyte ratio (NLR) [6]. The CXI enables the comprehensive evaluation of sarcopenia, systemic inflammation, and nutritional status. It is an objective biomarker and can be evaluated non-invasively by daily examinations (computed tomography [CT] and blood tests).
Recently, it has been shown that the CXI can be a useful long-term prognostic indicator in non-small-cell lung cancer, small-cell lung cancer, and diffuse large B-cell lymphoma [6,7,8]. However, there have been no studies of the CXI as a prognostic index in CRC. The present study, therefore, evaluated whether or not the CXI is useful as a prognostic factor in CRC.
Materials and methods
Study population
This was a retrospective cohort study of 306 patients who underwent surgical resection for CRC at the International University of Health and Welfare Hospital (Nasushiobara, Tochigi Prefecture, Japan) between April 2010 and March 2020.
The inclusion criterion was patients who underwent laparoscopic R0 colorectal resection for CRC. Patients who had (a) stage 0 or IV CRC, (b) multiple cancers, (c) perioperative death, (d) who underwent emergency surgery, and (e) who had missing data on clinicopathological factors and follow-up were excluded. We retrospectively reviewed the primary endpoint as the disease-free survival (DFS) and overall survival (OS) using a maintained database.
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of the International University of Health and Welfare Hospital (approval no: 22-B-7).
Treatment and patient management
Surgical indications, surgical treatment, chemotherapy selection, and basic surveillance for CRC were determined according to the Japanese Society for Cancer of the Colon and Rectum guideline 2019, whereas staging and pathological diagnoses were performed in accordance with the 9th edition of the Colorectal Cancer Handling Regulations [9, 10]. Basic surveillance after surgery was performed using tumor markers every three months, whereas chest and abdominal enhanced CT and colonoscopy were performed every 6 months and every 1 or 2 years, respectively.
Right-sided colon cancer refers to CRC located in the cecum, ascending colon, and transverse colon, whereas left-sided colon cancer refers to that located within the splenic flexure and beyond [11]. CRC recurrence after primary operation referred to newly detected local or distant metastatic lesions on enhanced CT or positron emission tomography with CT, regardless of whether the level of the tumor markers increased. The DFS was defined as the time from surgery to any disease recurrence in the local region, distant metastases or second primary cancer, or death from any cause. Postoperative complications, including anastomotic leakage, intraperitoneal abscess, surgical site infection, and ileus, were defined as grade ≥ III complications occurring within one month after surgery, according to the Clavien–Dindo classification.
Data collection
The clinicopathological data included sex, age, body mass index (BMI), comorbidities, tumor location, TNM staging, surgical factors (bleeding, operation time, postoperative complications), and survival duration. Other data were the preoperative values for serum albumin, C-reactive protein (CRP), white blood cells (neutrophils, lymphocyte count), carcinoembryonic antigen (CEA), and carbohydrate antigen 19–9 (CA19-9). We assessed these parameters through blood tests within seven days before surgery. The Glasgow prognostic score (GPS) using the serum CRP and albumin levels was used as the preoperative nutritional evaluation index [12].
Assessing the CXI
The CXI was calculated as previously reported: (SMI × serum albumin level [g/dL])/NLR [6]. In the previous report, the L3-SMI was used, but since this parameter is complicated to measure, we simply used the L3-psoas muscle index (PMI) as a substitute for the L3-SMI. Preoperative CT at the third lumbar vertebra was used to determine the psoas muscle area, which was calculated using the following formula: length of the major axes × length of the minor axes. The PMI was calculated as the psoas muscle area/height squared (cm2/m2) [13,14,15]. The NLR was calculated by dividing the absolute neutrophil count by the absolute lymphocyte count [16]. The cutoff values of PMI and NLR were defined as below the sex-specific median. The optimal cutoff values for PMI were 5.0 for males and 3.1 for females, and for the NLR, the cutoff level was 3.9.
As the skeletal muscle area differs by sex, the CXI cutoff values by sex were defined as the values maximizing the Youden index for predicting the 5-year survival for each sex on the receiver-operating characteristic (ROC) curve. In the ROC analysis of the 5-year survival status, the optimal cutoff values for the CXI were 8.4 for males and 5.6 for females, with an area under the curve of 0.666 (95% confidence interval [CI]: 0.56–0.77) and 0.622 (95% CI: 0.46–0.78), respectively (Supplementary Fig. 1A and 1B). Patients were stratified into two groups using these cutoff values (high- and low-CXI groups). Given the strong correlation between the CXI and SMI (r = 0.7135) or NLR (r = − 0.7041) according to Spearman’s rank correlation test (Supplementary Fig. 2A and 2B), the SMI and NLR were excluded from the multivariate analysis.
Statistical analyses
The Mann–Whitney U and Chi-square tests were used to compare the continuous and categorical variables, respectively. Kaplan–Meier curves with the log-rank test were used to estimate and compare the survival between high-CXI and low-CXI groups. The Cox proportional hazards model was used to estimate the hazard ratios (HRs) for the DFS and OS in the univariate and multivariate analyses. The cutoff values for CEA and CA19-9 were set at the level of the upper normal limit. The STATA/IC software program, version 16.0 (STATA Statistical Software; Stata Corp., College Station, TX, USA) was used for the statistical analyses. A two-sided p value < 0.05 was considered significant.
Results
A comparison of the baseline patient characteristics
The 306 total patients (males, 192; females, 114) were divided into the high-CXI and low-CXI groups, and the patient characteristics are shown in Table 1. In the univariate analysis, the low-CXI group was significantly older (73.6 vs. 70.6 years old, p = 0.02), had a lower BMI (21.6 vs. 23.1 kg/m2, p < 0.01), were more likely to have had obstructive CRC (15.9 vs. 3.3%, p < 0.01), and had poorer T factor and pathological stage (both p < 0.01) than the high-CXI group. There were no significant differences in the tumor location, histopathological type, surgical procedure, or postoperative complications between groups. The PMI (3.16 vs. 5.17 cm2/kg, p < 0.01) and NLR and GPS were significantly lower and higher in the low-CXI group, respectively, than in the high-CXI group (both p < 0.01).
The survival
The median duration of follow-up was 51.9 (range: 3.6–115.2) months. During the follow-up, 58 patients (18.9%) relapsed, and 53 (17.3%) died. In all cohorts, the 5-year DFS was 80.3% (95% CI 75.1–84.5%), and the 5-year OS was 81.5% (95% CI 76.1–85.9%).
Univariate and multivariate DFS analyses of CRC patients
Table 2 shows the univariate and multivariate analyses of the association of clinicopathological characteristics with the DFS in patients with CRC. In the univariate analysis, the DFS rate was significantly worse in patients with obstructive CRC (p < 0.01), CEA level ≥ 5.0 ng/mL (p < 0.01), CA19-9 level ≥ 37.0 ng/mL (p < 0.01), T3 or T4 (p < 0.01), stage III disease (p < 0.01), lymphatic or venous invasion (p < 0.01), adjuvant chemotherapy (p < 0.01), a low PMI (p < 0.01), and a low CXI (p < 0.01) than in others.
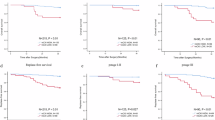
In the multivariate analysis, T3 or T4 (HR: 2.56; 95% CI 1.04–6.25, p = 0.039), stage III disease (HR: 3.77; 95% CI 1.79–7.93, p < 0.01), and low CXI (HR: 2.27; 95% CI 1.31–3.90, p = 0.003) were significant independent predictors of the DFS. Figure 1A shows the Kaplan–Meier survival curves of the DFS according to the CXI status. The low-CXI group had significantly lower DFS rates than the high-CXI group (5-year survival rates, 86.3% [95% CI 80.6–90.5%] vs. 63.1% [50.9–72.9%], log-rank: p < 0.01).
Univariate and multivariate OS and cancer-specific survival (CSS) analyses of CRC patients
Table 3 shows the univariate and multivariate analyses of the association of the clinicopathological characteristics with the OS in patients with CRC. In the univariate analysis, the OS rate was significantly worse in patients with an older age (p < 0.03), CEA level ≥ 5.0 ng/mL (p < 0.01), CA19-9 level ≥ 37.0 ng/mL (p < 0.01), T3 or T4 (p < 0.01), stage III disease (p < 0.01), lymphatic or venous invasion (p = 0.03), GPS 1 or 2 (p < 0.01), low PMI (p < 0.01), high NLR (p < 0.01), and low CXI (p < 0.01) than in others.
In the multivariate analysis, CA19-9 level ≥ 37.0 ng/mL (HR: 2.68; 95% CI 1.37–5.24, p = 0.004), stage III disease (HR: 2.57; 95% CI 1.34–4.92, p = 0.004), and a low CXI (HR: 2.35; 95% CI 1.31–4.21, p = 0.004) were significant independent predictors of the OS. Figure 1B shows the Kaplan–Meier survival curves of the OS according to the CXI status. The low-CXI group had significantly lower OS rates than the high-CXI group (5-year survival rates, 87.9% [95% CI 82.0–92.1%] vs. 67.2% [55.2–76.6%], log-rank: p < 0.01).
Furthermore, during the follow-up period, 33 patients (10.7%) suffered from cancer-specific death, and the 5-year CSS rate after laparoscopic colorectal resection for CRC was 87.9%. Supplemental Table 1 shows the univariate and multivariate analyses of the association of clinicopathological characteristics with the CSS in patients with CRC. In the multivariate analysis, CA19-9 level ≥ 37.0 ng/mL (HR: 3.05; 95% CI 1.35–6.87, p = 0.007), stage III disease (HR: 9.36; 95% CI 2.62–33.3, p = 0.001), and a low CXI (HR: 2.48; 95% CI: 1.21–5.11, p = 0.013) were significant independent predictors of the CSS. The Kaplan–Meier curve indicated that patients with a low CXI had worse CSS rates than those with a high CXI (5-year survival rates, 77.6% [65.5–85.9%] vs. 92.1% [86.9–95.2%], log-rank p < 0.01; Fig. 1C).
Subgroup analyses
In the comparison between the two groups, the low-CXI group had significantly more advanced disease; therefore, we conducted a sensitivity analysis in the subgroups of stage I + II and stage III. Figure 2A, B, C shows the comparison of the survival curves of the low-CXI vs. high-CXI groups according to the stage I + II groups. The survival rate of the low-CXI group was significantly lower than that of the high-CXI group for the 5-year DFS (95.5% [95% CI 89.4–98.2%] vs. 79.4% [95% CI 61.5–89.6%]; p = 0.0081) and 5-year OS (91.7% [95% CI: 83.9–95.8%] vs. 82.9% [68.6–91.2%]; p = 0.0081). The same trend was observed for the 5-year CSS (98.8% [95% CI 92.1–99.8] vs. 92.4% [95% CI 78.0–97.5%]; p = 0.0365).
Kaplan–Meier curves for patients with low cachexia index (CXI) and high CXI. After surgery for stages I+ II colorectal cancer: A the disease-free survival; B the overall survival; C the cancer-specific survival. After surgery for stage III colorectal cancer: D the disease-free survival; E the overall survival; F the cancer-specific survival
Figure 2D, E, F shows the comparison of the low-CXI vs. high-CXI survival curves in the stage III group. The survival rate of patients with a low CXI was significantly lower than that of patients with a high CXI for the 5-year DFS (70.5% [95% CI 58.6–79.5%] vs. 42.8% [95% CI 27.0–57.7%]; p = 0.0046) and 5-year OS (81.8% [95% CI 70.6–89.0%] vs. 47.1% [95% CI 29.0–63.2%]; p = 0.0006). The same trend was observed for the 5-year CSS (81.7% [95% CI 70.6–89.0%] vs. 58.7% [95% CI 38.2–74.5%]; p = 0.0205).
Discussion
Our results suggested that a low CXI might be a long-term prognostic factor for the DFS, OS, and CSS in CRC patients, not only in advanced-stage cases but also early-stage cases. To our knowledge, this is the first report to demonstrate the impact of a low CXI on CRC mortality.
Cancer cachexia is a devastating, multifactorial, and often irreversible syndrome characterized by substantial weight loss, primarily from the loss of skeletal muscle and body fat, affecting about 50–80% of cancer patients, depending on the tumor type [4]. In cancer cachexia, increased systemic inflammation, altered skeletal muscle protein and adipose tissue metabolisms, and increased energy consumption by the tumor occur owing to complex interactions between the tumor and the host, inflammatory cytokines, reactive oxygen species, eicosanoids, adipokines, cachexia-promoting factors, and hormones [4]. These conditions cause significant morbidity and mortality and severe complications during cancer treatment in both localized and metastatic cancer patients.
In 2011, the EPCRC classified cancer cachexia into three stages: pre-cachexia, cachexia, and refractory cachexia [3]. Refractory cachexia patients do not respond to any treatment and have less than 3 months of life expectancy owing to the increased level of active catabolism and the impossibility of weight loss management. Therefore, the EPCRC emphasized the importance of early intervention in the reversible pre-cachexia and cachexia stages [3]. Previous studies showed the relationship between a low CXI and treatment response to chemotherapy or the long-term prognosis in unresectable advanced tumors [6,7,8]. In the present study, we were able to extract cachexia patients using the CXI even at stage I + II, which is less likely to cause weight loss than later stages [17], findings that may be useful for early intervention in cachexia patients.
Although the mechanisms underlying cancer cachexia are not fully understood, they are related to the local and systemic immune response to the tumor [2]. The tumor microenvironment (TME), as a complex cellular network, consists of cancer cells, various stromal cells (e.g., infiltrating immune cells such as lymphocytes and macrophages), neutrophils, fibroblasts, and adipocytes, as well as extracellular-matrix components, soluble factors, and signaling molecules produced by these cells [2, 18, 19]. Accumulating evidence demonstrates that TME-associated tumor-host interactions contribute to plasma cytokine levels and proteome alterations, possibly aiding in the development of cancer cachexia and tumor progression through the production of multiple pro-cachectic factors [20]. The most important role in CRC-associated cachexia is played by pro-inflammatory cytokines, including the proteolysis-inducing factor (PIF), tumor necrosis factor α (TNFα), interleukin (IL)-1, IL-6, and certain chemokines (e.g., IL-8) [21, 22]. The role of CRC cells, especially in cooperation with other TME cells, is also crucial in cancer cachexia. In fact, CRC cells are the products of classic cachexia-inducing factors, including PIF, IL-6, and TNF-α, as well as novel factors known as “cachexokines” (e.g., ataxin-10, bridging integrator 1, syntaxin 7, and multiple inositol-polyphosphate 1) [23, 24]. The first pro-cachectic factors are mainly responsible for increasing skeletal muscle catabolism, accelerating weight loss, and shortening the survival time [23]. Furthermore, CRC cell products (mainly IL-6) mediate the recruitment of immunosuppressive cells (e.g., myeloid-derived suppressor cells and regulatory T cells) and reduce T-cell infiltration, resulting mainly in cell-mediated response suppression and CRC progression [25].
In the present study, the difference in the method compared with that in previous studies lies in the fact that the L3-PMI was used instead of the L3-SMI. Previous studies have reported the usefulness of the CXI determined using the L3-SMI [6,7,8]; however, the measurement of the L3-SMI, including the psoas muscle, lumbar muscle, erector spinae, transversus abdominis muscle, internal and external oblique muscles, and rectus abdominis, is complicated and requires time and effort [26]. A previous study showed a high correlation between the L3-SMI and L3-PMI (r = 0.70) [27], suggesting that the L3-PMI can be a substitute for the L3-SMI. We used the L3-PMI to calculate the CXI because it can be calculated easily in clinical practice and has been widely used to calculate the sarcopenia index [13,14,15]. The present study showed that the modified CXI using L3-PMI, which is easier to measure, is also a useful prognostic factor.
Currently, there are few clinical studies on interventional treatment for cancer cachexia. However, several drug therapies (including corticosteroids, non-steroidal anti-inflammatory agents, eicosapentaenoic acid, ghrelin agonists, and selective androgen receptor modulator) have potential anti-inflammatory, metabolic improvement, and appetite improvement benefits in cancer cachexia patients [28,29,30]. Early multidisciplinary treatment with drug therapy, high-quality nutrition therapy, and appropriate exercise, prescribed according to the patient’s physical function can be expected to increase the skeletal muscle mass, restore the physical function, and contribute to improving the prognosis of cancer cachexia patients [31, 32].
Several limitations associated with the present study warrant mention. Most importantly, this retrospective study was conducted at a single institution with a small number of patients. In addition, the cutoff value of the CXI using the SMI and NLR is controversial and might vary by ethnicity and underlying disease. Furthermore, in this study, genetic mutations and weight loss were not investigated; therefore, their relationship with the prognosis could not be evaluated. There are still few clinical studies on the CXI, and further large-scale studies with the CXI calculated using the same method in CRC patients are thus necessary to determine the optimal cutoff value.
Conclusion
In this study, we showed that a low CXI is a long-term prognostic factor in CRC patients, including those in the early stage. We believe that appropriate interventional treatments of cancer cachexia in CRC patients stratified by CXI have the potential to improve the prognosis of CRC patients further.
Data availability
The data that support the findings of this study are available from the corresponding author upon reasonable request.
References
Bray F, Ferlay J, Soerjomataram I, Siegel RL, Torre LA, Jemal A. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin. 2018;68:394–424. https://doi.org/10.3322/caac.21492.
Kasprzak A. The role of tumor microenvironment cells in colorectal cancer (CRC) cachexia. Int J Mol Sci. 2021;22:1565. https://doi.org/10.3390/ijms22041565.
Fearon K, Strasser F, Anker SD, Bosaeus I, Bruera E, Fainsinger RL, et al. Definition and classification of cancer cachexia: an international consensus. Lancet Oncol. 2011;12:489–95. https://doi.org/10.1016/S1470-2045(10)70218-7.
Argilés JM, Busquets S, Stemmler B, López-Soriano FJ. Cancer cachexia: understanding the molecular basis. Nat Rev Cancer. 2014;14:754–62. https://doi.org/10.1038/nrc3829.
Martin L, Senesse P, Gioulbasanis I, Antoun S, Bozzetti F, Deans C, et al. Diagnostic criteria for the classification of cancer-associated weight loss. J Clin Oncol. 2015;33:90–9. https://doi.org/10.1200/JCO.2014.56.1894.
Jafri SH, Previgliano C, Khandelwal K, Shi R. Cachexia index in advanced non-small-cell lung cancer patients. Clin Med Insights Oncol. 2015;9:87–93. https://doi.org/10.4137/CMO.S30891.
Go SI, Park MJ, Lee GW. Clinical significance of the cachexia index in patients with small cell lung cancer. BMC Cancer. 2021;21:563. https://doi.org/10.1186/s12885-021-08300-x.
Go SI, Park MJ, Park S, Kang MH, Kim HG, Kang JH, et al. Cachexia index as a potential biomarker for cancer cachexia and a prognostic indicator in diffuse large B-cell lymphoma. J Cachexia Sarcopenia Muscle. 2021;12:2211–9. https://doi.org/10.1002/jcsm.12837.
Hashiguchi Y, Muro K, Saito Y, Ito Y, Ajioka Y, Hamaguchi T, et al. Japanese society for cancer of the colon and rectum (JSCCR) guidelines 2019 for the treatment of colorectal cancer. Int J Clin Oncol. 2020;25:1–42. https://doi.org/10.1007/s10147-019-01485-z.
Japanese Society for Cancer of the Colon and Rectum. Japanese classification of colorectal, appendiceal, and anal carcinoma: the 3rd. English ed. J Anus Rectum Colon 2019 3 175–95
Cremolini C, Antoniotti C, Lonardi S, Bergamo F, Cortesi E, Tomasello G, et al. Primary tumor sidedness and benefit from FOLFOXIRI plus bevacizumab as initial therapy for metastatic colorectal cancer Retrospective analysis of the TRIBE trial by GONO. Ann Oncol. 2018. https://doi.org/10.1093/annonc/mdy140.
Forrest LM, McMillan DC, McArdle CS, Angerson WJ, Dunlop DJ. Evaluation of cumulative prognostic scores based on the systemic inflammatory response in patients with inoperable non-small-cell lung cancer. Br J Cancer. 2003;89:1028–30. https://doi.org/10.1038/sj.bjc.6601242.
Hamaguchi Y, Kaido T, Okumura S, Kobayashi A, Hammad A, Tamai Y, et al. Proposal for new diagnostic criteria for low skeletal muscle mass based on computed tomography imaging in Asian adults. Nutrition. 2016;32:1200–5. https://doi.org/10.1016/j.nut.2016.04.003.
Durand F, Buyse S, Francoz C, Laouénan C, Bruno O, Belghiti J, et al. Prognostic value of muscle atrophy in cirrhosis using psoas muscle thickness on computed tomography. J Hepatol. 2014;60:1151–7.
Masuda T, Shirabe K, Ikegami T, Harimoto N, Yoshizumi T, Soejima Y, et al. Sarcopenia is a prognostic factor in living donor liver transplantation. Liver Transpl. 2014;20:401–7.
Malietzis G, Giacometti M, Kennedy RH, Athanasiou T, Aziz O, Jenkins JT. The emerging role of neutrophil to lymphocyte ratio in determining colorectal cancer treatment outcomes: a systematic review and meta-analysis. Ann Surg Oncol. 2014;21:3938–46. https://doi.org/10.1245/s10434-014-3815-2.
Meyerhardt JA, Kroenke CH, Prado CM, Kwan ML, Castillo A, Weltzien E, et al. Association of weight change after colorectal cancer diagnosis and outcomes in the Kaiser permanente Northern California population. Cancer Epidemiol Biomarkers Prev. 2017;26:30–7. https://doi.org/10.1158/1055-9965.EPI-16-0145.
Catalano V, Turdo A, Di Franco S, Dieli F, Todaro M, Stassi G. Tumor and its microenvironment: a synergistic interplay. Semin Cancer Biol. 2013;23:522–32. https://doi.org/10.1016/j.semcancer.2013.08.007.
Roma-Rodrigues C, Mendes R, Baptista PV, Fernandes AR. Targeting tumor microenvironment for cancer therapy. Int J Mol Sci. 2019;20:840. https://doi.org/10.3390/ijms20040840.
Hanash SM, Pitteri SJ, Faca VM. Mining the plasma proteome for cancer biomarkers. Nature. 2008;452:571–9. https://doi.org/10.1038/nature06916.
Pinto I, Carnier N, Oyama J, Otoch JP, Alcântara PS, Tokeshi F, et al. Cancer as a pro-inflammatory environment: metastasis and cachexia. Mediat Inflam. 2015. https://doi.org/10.1155/2015/791060.
Onesti JK, Guttridge DC. Inflammation based regulation of cancer cachexia. BioMed Res Int. 2014. https://doi.org/10.1155/2014/168407.
Cabal-Manzano R, Bhargava P, Torres-Duarte A, Marshall J, Bhargava P, Wainer IW. Proteolysis-inducing factor is expressed in tumours of patients with gastrointestinal cancers and correlates with weight loss. Br J Cancer. 2001;84:1599–601. https://doi.org/10.1054/bjoc.2001.1830.
Schäfer M, Oeing CU, Rohm M, Baysal-Temel E, Lehmann LH, Bauer R, et al. Ataxin-10 is part of a cachexokine cocktail triggering cardiac metabolic dysfunction in cancer cachexia. Mol Metab. 2016;5:67–78. https://doi.org/10.1016/j.molmet.2015.11.004.
Toyoshima Y, Kitamura H, Xiang H, Ohno Y, Homma S, Kawamura H, et al. IL6 modulates the immune status of the tumor microenvironment to facilitate metastatic colonization of colorectal cancer cells. Cancer Immunol Res. 2019;7:1944–57. https://doi.org/10.1158/2326-6066.CIR-18-0766.
Wang S, Xie H, Gong Y, Kuang J, Yan L, Ruan G, et al. The value of L3 skeletal muscle index in evaluating preoperative nutritional risk and long-term prognosis in colorectal cancer patients. Sci Rep. 2020;10:8153. https://doi.org/10.1038/s41598-020-65091-0.
Abbass T, Tsz Ho YT, Horgan PG, Dolan RD, McMillan DC. The relationship between computed tomography derived skeletal muscle index, psoas muscle index and clinical outcomes in patients with operable colorectal cancer. Clin Nutr ESPEN. 2020;39:104–13. https://doi.org/10.1016/j.clnesp.2020.07.010.
Temel JS, Abernethy AP, Currow DC, Friend J, Duus EM, Yan Y, et al. Anamorelin in patients with non-small-cell lung cancer and cachexia (ROMANA 1 and ROMANA 2): results from two randomised, double-blind, phase 3 trials. Lancet Oncol. 2016;17:519–31. https://doi.org/10.1016/S1470-2045(15)00558-6.
Crawford J. Clinical results in cachexia therapeutics. Curr Opin Clin Nutr Metab Care. 2016;19:199–204. https://doi.org/10.1097/MCO.0000000000000274.
Takiguchi S, Murakami K, Yanagimoto Y, Takata A, Miyazaki Y, Mori M, et al. Clinical application of ghrelin in the field of surgery. Surg Today. 2015;45:801–7. https://doi.org/10.1007/s00595-014-1040-z.
Naito T, Mitsunaga S, Miura S, Tatematsu N, Inano T, Mouri T, et al. Feasibility of early multimodal interventions for elderly patients with advanced pancreatic and non-small-cell lung cancer. J Cachexia Sarcopenia Muscle. 2019;10:73–83. https://doi.org/10.1002/jcsm.12351.
Hammad A, Kaido T, Uemoto S. Perioperative nutritional therapy in liver transplantation. Surg Today. 2015;45:271–83. https://doi.org/10.1007/s00595-014-0842-3.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflicts of interest. The authors have full control of all primary data and agree to allow the journal to review our data if requested.
Ethical approval
This study was conducted in accordance with the Declaration of Helsinki and was approved by the Institutional Review Board of the International University of Health and Welfare Hospital (approval no: 22-B-7).
Consent to participate
Written informed consent was obtained from each patient.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Kamada, T., Haruki, K., Nakashima, K. et al. Prognostic significance of the cachexia index in patients with stage I–III colorectal cancer who underwent laparoscopic surgery. Surg Today 53, 1064–1072 (2023). https://doi.org/10.1007/s00595-023-02646-4
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-023-02646-4