Abstract
Purpose
Cancer cachexia, a complex multifactorial syndrome associated with sarcopenia, negatively affects the quality of life and survival in patients with several cancers. We aimed to develop a new score for cachexia assessment and evaluate its effectiveness in the classification of patients undergoing radical resection for colorectal cancer.
Methods
This study included 396 patients who underwent radical resection for Stage I–III colorectal cancer. To develop the Cancer Cachexia Score (CCS), we analyzed predictive factors of cachexia status related to the development of sarcopenia and incorporated significant factors into the score. We then evaluated the relationship between CCS and survival after radical resection for colorectal cancer.
Results
As body mass index (P < 0.001), prognostic nutritional index (P = 0.005), and tumor volume (P < 0.001) were significantly associated with the development of sarcopenia, these factors were included in CCS. Using CCS, 221 (56%), 98 (25%), and 77 (19%) patients were diagnosed with mild, moderate, and severe cancer cachexia, respectively. In multivariate analysis, severe CCS (P < 0.001), N stage 1–2 (P < 0.001), and occurrence of postoperative complications (P = 0.007) were independent predictors of disease-free survival. Age ≥ 65 years (P = 0.009), severe CCS (P < 0.001), and N stage 1–2 (P < 0.001) were independent predictors of overall survival.
Conclusions
CCS may be a useful prognostic factor for predicting poor survival after radical resection in patients with Stage I–III colorectal cancer.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is the third most common malignancy and the second leading cause of cancer deaths worldwide [1]. Surgical resection is currently the only treatment offering a potential cure for patients with Stage I–III CRC. However, patients in the same TNM stage may have differences in prognosis even after undergoing radical surgery [2] [3]. Therefore, an accurate assessment is critically important for predicting the probability of survival in patients undergoing radical resection for CRC.
Cancer cachexia is a multifactorial syndrome defined by an ongoing loss of skeletal muscle mass with or without loss of fat mass [4]. As tumor progresses, patients are more likely to have cancer cachexia [5] [6] [7] [8]. It has also been correlated with functional impairment, reduced therapeutic responsiveness, and poor prognosis in cancer patients [9]. However, there is a lack of consensus on the method to be used for the evaluation of cachexia status in cancer patients.
The most important and clinically relevant phenotypic feature of cancer cachexia is sarcopenia, and the other features include body weight loss, cancer progression, and malnutrition [4] [10] [11]. The clinical measures for assessment of these features include body mass index (BMI), prognostic nutritional index (PNI), and tumor volume [10] [11] [12] [13] [14] [15]. We developed a new score called the Cancer Cachexia Score (CCS) based on these cachexia-related factors and hypothesized that the prognosis would differ according to variations in the score. In the present study, we aimed to investigate the prognostic value of cancer cachexia using CCS to predict outcomes in patients with CRC.
Materials and methods
Patient selection
Between January 2014 and December 2020, 429 patients with CRC underwent radical resection at two institutions (Department of Surgery, Tokyo General Hospital and Kasai Shoikai Hospital). Of these, 33 patients were excluded (one patient for postoperative mortality, 22 patients for additional resection after endoscopic mucosal resection, five for T stage 4b, and five for insufficient data); finally, 396 patients were included in the study. We performed a retrospective review of a prospectively maintained database of patients, and 174 of these patients had been studied previously [16]. The present study was approved by the Ethics Committees of Tokyo General Hospital (No. 22–9) and Kasai Shoikai Hospital (No. R4-1) and was conducted in accordance with the tenets of the Declaration of Helsinki.
Patient data included age, sex, BMI, American Society of Anesthesiologists Physical Status (ASA-PS) score [17], blood test results, surgical approach, tumor location, pathological findings (T and N stage), and postoperative complications. Additionally, we examined the following nutritional indices: geriatric nutritional risk index (GNRI) [18], PNI [19], and neutrophil-to-lymphocyte ratio (NLR) [20]. Blood tests were performed within 4 weeks of surgery.
Development of Cancer Cachexia Score
We analyzed the predictive factors of cachexia status, which are related to the development of sarcopenia in patients with CRC. Sarcopenia was evaluated using preoperative computed tomography (CT) findings and skeletal muscle index (SMI) [21]. SMI was calculated by measuring the cross-sectional area (cm2) of the skeletal muscle in the region of the third lumbar vertebra (L3) and normalizing the value according to the height (cm2/m2). Sarcopenia was defined as SMI below the cut-off value (≤ 43.75 cm2/m2 for men and ≤ 41.10 cm2/m2 for women) [22].
The exploratory model included the following variables as cancer cachexia-related factors: BMI, ASA-PS, GNRI, NLR, PNI, tumor volume, T stage, and N stage. On the basis of the definition of cachexia, 20 kg/m2 was selected as the cutoff value for BMI, and 40 was selected as the cutoff for PNI [4] [19]. Tumor information was recorded using surgical pathological reports, and tumor volume was estimated by calculating tumor size (larger diameter × smaller diameter) × T stage. The optimal cut-off value of tumor volume was determined using receiver operating characteristic (ROC) analysis. We incorporated statistically significant and cancer cachexia-related factors into CCS.
Statistical analysis
All statistical analyses were conducted using the EZR software version 1.51 (Saitama Medical Center, Jichi Medical University, Japan) and GraphPad Prism (version 9). All P values were two-sided, with an α level of 0.05.
Data were expressed as median values. Continuous and categorical variables were compared using the Kruskal–Wallis test or the chi-square test, as appropriate. The optimal cut-off values of clinical continuous variables were determined by analysis of ROC curves of overall survival events. Clinical continuous variables were classified into two groups based on the cut-off values and the values above or below the standard values; subsequently, analyses were conducted using the logistic regression and the Cox proportional hazards regression models.
First, we identified the cancer cachexia-related factors in patients with CRC. Univariate and multivariate logistic analyses were performed to identify the independent factors associated with the development of sarcopenia. A stepwise backward elimination approach with a threshold P value of 0.05 was used to select suitable variables for the final model. Then, a multivariate ROC curve including the cachexia-related factors was constructed to predict survival status, and the individual factors were examined.
Next, we evaluated the prognostic significance of CCS in patients with CRC. Univariate and multivariate Cox proportional hazards regression models were used to estimate hazard ratios (HRs) for disease-free and overall survival. A stepwise backward elimination approach with a threshold P value of 0.05 was used to select suitable variables for the final model. The Kaplan–Meier method was used to estimate cumulative survival probabilities, and differences between results obtained for the two groups were compared using the log-rank test.
Results
Correlation between sarcopenia and cachexia-related factors
Table 1 shows the correlation between clinical variables and sarcopenia in patients with CRC. Univariate analysis revealed that age ≥ 65 years (P = 0.004), female sex (P < 0.001), BMI < 20 (P < 0.001), NLR ≥ 3.02 (P < 0.001), PNI < 40 (P < 0.001), tumor volume ≥ 57.7 (P < 0.001), and T stage ≥ 3 (P = 0.018) were significantly associated with sarcopenia. Multivariate analysis revealed that age ≥ 65 years (P = 0.044), female sex (P = 0.014), BMI < 20 (P < 0.001), PNI < 40 (P = 0.005), and tumor volume ≥ 57.7 (P < 0.001) were significantly associated with sarcopenia in patients with CRC. On the basis of these results, CCS was developed by including statistically significant cancer cachexia-related factors (BMI, PNI, and tumor volume); however, factors like age and sex were excluded. The multivariate ROC curve showed that the area under the curve (AUC) of the integrated factors (sarcopenia, BMI, PNI, and tumor volume) was 0.717 (95% CI, 0.651–0.783), which was larger than that of the individual factors such as sarcopenia (0.639; 95% CI: 0.582–0.696), BMI (0.607; 95% CI: 0.544–0.669), PNI (0.619; 95% CI: 0.556–0.681), and tumor volume (0.592; 95% CI: 0.528–0.655) (Online Resource 1). On the basis of the sum of the scores of individual patients, the CCS values were categorized into mild (0–1 point), moderate (2 points), and severe (3–4 points) groups (Table 2).
Patients’ characteristics according to Cancer Cachexia Score
The clinical characteristics of the patients according to the CCS values are shown in Table 3. Overall, 221 (56%), 98 (25%), and 77 (19%) patients were diagnosed with mild, moderate, and severe cancer cachexia, respectively, based on the CCS values. Significant differences were observed in the values obtained for factors such as age (P < 0.001), sex (P = 0.003), BMI (P < 0.001), GNRI (P = 0.005), NLR (P < 0.001), PNI (P < 0.001), sarcopenia (P < 0.001), tumor volume (P < 0.001), and T stage ≥ 3 (P < 0.001). However, there were no significant differences in the rates of occurrence of N stage 1–2 (P = 0.366).
Survival curve in patients with Stage I and II/III colorectal cancer according to Cancer Cachexia Score
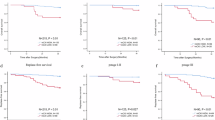
The patients were subdivided into Stage I and II/III disease groups; 26 and 69% of the patients in Stages I and II/III were categorized into the moderate or severe groups using CCS, and there was no difference in the cachexia status of Stage II and III patients categorized in the severe group (Fig. 1).
Cachexia status determined by CCS was associated with the rates of disease-free survival (Fig. 2a, P < 0.001) and overall survival (Fig. 2b, P < 0.001) in patients following radical resection for Stage I–III CRC. In Stage I, the survival rates of the mild and the moderate CCS groups were comparable, and that of the severe CCS group was worse than those of the other groups (Fig. 2c, P < 0.001). In Stage II/III, the overall survival rates decreased significantly as CCS increased (Fig. 2d, P < 0.001).
The Kaplan–Meier curves prepared using data obtained from patients who underwent radical resection for colorectal cancer. a Disease-free survival, b overall survival in patients with Stage I–III, c overall survival in patients with Stage I, and d overall survival in patients with Stage II/III colorectal cancer
Univariate and multivariate analyses of clinicopathologic variables in relation to disease-free survival after radical resection for colorectal cancer
Table 4 lists the relationship between the clinical variables and the disease-free survival rates after radical resection for CRC. The univariate analysis showed that the disease-free survival rates were significantly worse in patients with severe CCS (P < 0.001), T stage ≥ 3 (P = 0.004), N stage 1–2 (P < 0.001), and postoperative complication occurrence (P = 0.009). The multivariate analysis revealed that severe CCS (P < 0.001), N stage 1–2 (P < 0.001), and postoperative complication occurrence (P = 0.007) were independent predictors of disease-free survival.
Univariate and multivariate analyses of clinicopathologic variables in relation to overall survival after radical resection for colorectal cancer
Table 5 lists the relationship between the clinical variables and the overall survival rates after radical resection for CRC. The univariate analysis showed that the overall survival rates were significantly worse in patients with age ≥ 65 (P = 0.005), ASA-PS ≥ 3 (P = 0.031), GNRI < 96.9 (P = 0.001), severe CCS (P < 0.001), T stage ≥ 3 (P = 0.039), N stage 1–2 (P < 0.001), and postoperative complication occurrence (P = 0.032). The multivariate analysis revealed that age ≥ 65 (P = 0.009), severe CCS (P < 0.001), and N stage 1–2 (P < 0.001) were independent predictors of overall survival.
Discussion
We found a significant association between CCS values and poor prognosis in patients who underwent radical resection for CRC. Multivariate analysis revealed that the CCS value was an independent predictor of poor disease-free survival and overall survival outcomes in patients with CRC. Furthermore, the overall survival rate decreased significantly as the CCS value increased in patients with Stage II/III CRC. These findings suggest that CCS may be a strong prognostic factor and useful for predicting cachexia status, especially in cases of advanced CRC.
The pathophysiology of cancer cachexia is complex, and various definitions have been proposed because of the lack of a consensus clinical definition in clinical settings [23]. In the present study, we identified predictive factors for cachexia (BMI, PNI, and tumor volume) and combined the data obtained for these factors with that obtained for sarcopenia status. Although cancer cachexia occurs less frequently in patients with CRC than that in patients with pancreatic or gastric cancers, previous studies have shown that almost 50–60% of patients with advanced CRC are affected by cancer cachexia [9]. Our study revealed that 44 and 69% of patients in Stages I–III and II–III had severe or moderate cachexia, which is consistent with the findings mentioned in previous reports.
BMI is a standard method of assessing body composition, and a low BMI has been associated with sarcopenia [10]. In fact, an international consensus has included weight loss of > 5% in the preceding 6 months or > 2% in individuals showing depletion according to their BMI (< 20 kg/m2) and sarcopenia status in the definition of cancer cachexia [4]. PNI is a classical nutritional marker associated with sarcopenia [12]. Several studies have demonstrated the prognostic importance of PNI in patients with CRC [24] [25]. Tumor volume is an alternative parameter for tumor burden, which has been associated with poor prognosis in gastrointestinal cancers [15] [26] [27]. Interestingly, the multivariate analysis revealed that tumor volume was associated with sarcopenia, whereas T and N stages were not. Given the value of each factor, the combination of CCS with the data obtained on these factors would be a powerful prognostic factor in patients with cancer.
Cancer cachexia is a process of chronic inflammation mediated by the tumor microenvironment and the inflammatory immune response of the host [9]. As the tumor burden increases, inflammatory cytokines such as tumor necrosis factor-α (TNF-α) and interleukins-6 (IL-6) released from cancer cells contribute to muscle wasting by inducing oxidative stress and suppress autoimmunity, resulting in cancer cachexia [5] [6] [7] [8] [28]. These inflammatory cascades block the synthesis of albumin in favor of acute-phase protein synthesis and contributed to body weight loss and malnutrition [29] [30]. These lines of evidence may support the value of CCS as a predictor of the cancer cachexia status.
Since CCS is a simple and comprehensive marker for cachexia status, the score may be useful for early identification and targeted management of patients at high risk of poor survival. Several clinical studies have shown a significant increase of body weight and skeletal muscle mass in cancer cachexia patients treated with nutritional and anti-inflammatory therapies such as eicosapentaenoic acid (EPA), β-hydroxy-beta-methyl butyrate (β-HMB), arginine, glutamine or marine phospholipids (MPL), and ghrelin agonists [31] [32]. Therefore, patients diagnosed with severe CCS would be applicable for these therapies, that may improve the quality of life and prognosis in patients with CRC.
The present study had several limitations. First, it was a retrospective study with a limited sample size. The influence of confounding factors may not be fully excluded. Cachexia and sarcopenia might have been confounded by several factors such as age and comorbidities, which may have influenced the results. Second, in the present study, we explored predictive factors of cachexia based on sarcopenia status. The definition of sarcopenia using SMI values remains a controversial topic, and a variety of diagnostic cut-off values have been reported by several authors. Third, the tumor volume was estimated using pathological test results and was not based on preoperative 3D-CT measurements. In addition, the cut-off value of tumor volume was selected using our patient data and needs to be validated using other datasets. Therefore, further multicenter prospective studies are required to validate our results.
Conclusion
CCS may be a strong predictor of poor survival in patients with CRC, suggesting the usefulness of CCS for classifying patients according to their cachexia status and predicting postoperative prognosis.
Data availability
The datasets analyzed during the current study are available from the corresponding author on reasonable request.
References
Sung H, Ferlay J, Siegel RL et al (2021) Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA Cancer J Clin 71:209–249
van Gestel YR, de Hingh IH, van Herk-Sukel MP et al (2014) Patterns of metachronous metastases after curative treatment of colorectal cancer. Cancer Epidemiol 38:448–454
Neki K, Eto K, Kosuge M et al (2019) Identification of the risk factors for recurrence of Stage III colorectal cancer. Anticancer Res 39:5721–5724
Fearon K, Strasser F, Anker SD et al (2011) Definition and classification of cancer cachexia: an international consensus. Lancet Oncol 12:489–495
Anderson LJ, Albrecht ED, Garcia JM (2017) Update on management of cancer-related cachexia. Curr Oncol Rep 19:3
Ábrigo J, Elorza AA, Riedel CA et al (2018) Role of oxidative stress as key regulator of muscle wasting during cachexia. Oxid Med Cell Longev 2018:2063179
Argilés JM, Busquets S, Stemmler B et al (2014) Cancer cachexia: understanding the molecular basis. Nat Rev Cancer 14:754–762
Ni J, Zhang L (2020) Cancer cachexia: definition, staging, and emerging treatments. Cancer Manag Res 12:5597–5605
Kasprzak A, (2021) The role of tumor microenvironment cells in colorectal cancer (CRC) cachexia. Int J Mol Sci 22
Dev R (2019) Measuring cachexia-diagnostic criteria. Ann. Palliat Med 8:24–32
Miyawaki T, Naito T, Doshita K et al (2022) Predicting the efficacy of first-line immunotherapy by combining cancer cachexia and tumor burden in advanced non-small cell lung cancer. Thorac Cancer 13:2064–2074
Go SI, Park S, Kang MH et al (2019) Clinical impact of prognostic nutritional index in diffuse large B cell lymphoma. Ann Hematol 98:401–411
Ding P, Lv J, Sun C et al (2022) Combined systemic inflammatory immunity index and prognostic nutritional index scores as a screening marker for sarcopenia in patients with locally advanced gastric cancer. Front Nutr 9:981533
Nogueiro J, Santos-Sousa H, Pereira A et al (2022) The impact of the prognostic nutritional index (PNI) in gastric cancer. Langenbecks Arch Surg 407:2703–2714
Ohashi T, Komatsu S, Ichikawa D et al (2016) Tumor index as a combined indicator of tumor depth and size in gastric cancer. Anticancer Res 36:1895–1900
Takano Y, Haruki K, Tsukihara S, et al, (2022) The impact of low serum cholinesterase levels on survival in patients with colorectal cancer. Int J Colorectal Dis
Dripps RD, Lamont A, Eckenhoff JE (1961) The role of anesthesia in surgical mortality. JAMA 178:261–266
Hayama T, Hashiguchi Y, Ozawa T et al (2022) The preoperative geriatric nutritional risk index (GNRI) is an independent prognostic factor in elderly patients underwent curative resection for colorectal cancer. Sci Rep 12:3682
Sato R, Oikawa M, Kakita T et al (2020) The prognostic value of the prognostic nutritional index and inflammation-based markers in obstructive colorectal cancer. Surg Today 50:1272–1281
Hayama T, Hashiguchi Y, Okada Y et al (2020) Significance of the 7th postoperative day neutrophil-to-lymphocyte ratio in colorectal cancer. Int J Colorectal Dis 35:119–124
Iritani S, Imai K, Takai K et al (2015) Skeletal muscle depletion is an independent prognostic factor for hepatocellular carcinoma. J Gastroenterol 50:323–332
van Vledder MG, Levolger S, Ayez N et al (2012) Body composition and outcome in patients undergoing resection of colorectal liver metastases. Br J Surg 99:550–557
Fox KM, Brooks JM, Gandra SR et al (2009) Estimation of cachexia among cancer patients based on four definitions. J Oncol 2009:693458
Mohri Y, Inoue Y, Tanaka K et al (2013) Prognostic nutritional index predicts postoperative outcome in colorectal cancer. World J Surg 37:2688–2692
Tominaga T, Nagasaki T, Akiyoshi T et al (2020) Prognostic nutritional index and postoperative outcomes in patients with colon cancer after laparoscopic surgery. Surg Today 50:1633–1643
Liu Z, Gao P, Liu S et al (2017) Tumor volume increases the predictive accuracy of prognosis for gastric cancer: a retrospective cohort study of 3409 patients. Oncotarget 8:18968–18978
Tullie LG, Sohn HM, Zylstra J et al (2016) A role for tumor volume assessment in resectable esophageal cancer. Ann Surg Oncol 23:3063–3070
Narsale AA, Carson JA (2014) Role of interleukin-6 in cachexia: therapeutic implications. Curr Opin Support Palliat Care 8:321–327
Camarero González E, Muñoz Leira V, Iglesias Guerrero M et al (1995) Protein-energy malnutrition: its effects on 4 metabolic parameters. Nutr Hosp 10:158–160
Rupert JE, Narasimhan A, Jengelley DHA, et al, (2021) Tumor-derived IL-6 and trans-signaling among tumor, fat, and muscle mediate pancreatic cancer cachexia. J Exp Med 218
Braha A, Albai A, Timar B, et al, (2022) Nutritional interventions to improve cachexia outcomes in cancer-a systematic review. Medicina (Kaunas) 58
Takayama K, Takiguchi T, Komura N et al (2023) Efficacy and safety of anamorelin in patients with cancer cachexia: post-hoc subgroup analyses of a placebo-controlled study. Cancer Med 12:2918–2928
Acknowledgements
We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
YT, KK, and KE contributed to the study conception and design. YT, KK, ST, ST, YK, HK, SI, and RS provided data acquisition and statistical analysis. YT, KK, and RS participated in manuscript preparation. NH and EK contributed to the manuscript revision. All authors have read and approved the manuscript for publication.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Below is the link to the electronic supplementary material.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Takano, Y., Kodera, K., Tsukihara, S. et al. Association of a newly developed Cancer Cachexia Score with survival in Stage I–III colorectal cancer. Langenbecks Arch Surg 408, 145 (2023). https://doi.org/10.1007/s00423-023-02883-8
Received:
Accepted:
Published:
DOI: https://doi.org/10.1007/s00423-023-02883-8