Abstract
We conducted a meta-analysis to compare the outcomes of a self-expanding metallic stent (SEMS) vs. surgery for the palliative treatment of colorectal obstruction caused by advanced colorectal malignancy. The databases of MEDLINE, EMBASE, Cochrane controlled trials registry and the Chinese Wanfang were retrieved (updated to 31 August 2011) to identify eligible studies. We calculated the odds ratio or weighted mean difference and its corresponding 95 % confidence interval. In total, nine primary studies were included in this analysis. The success rate of SEMS placement was 93.9 %, with short-term and long-term complication rates of 26.2 and 16.1 %, respectively. Combined analyses revealed that the SEMS group had a similar risk of short-term complications as the surgical group (P = 0.22). Moreover, SEMS was not associated with a higher mortality risk than surgical intervention (P = 0.22) and it required a significantly shorter hospitalization time (P < 0.01); however, SEMS patients had a higher risk of long-term complications (P = 0.03). Because of great heterogeneities between patients and chemoradiotherapy, we did not analyze the survival times of the two groups. These results support the feasibility of SEMS as a palliative treatment for malignant colorectal obstruction caused by incurable malignancy, as it requires shorter hospitalization and is followed by quick recovery. However, the risk of long-term complications such as perforation and stent migration should be borne in mind.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Colorectal cancer (CRC) is one of the most common malignancies and a major cause of cancer-related death worldwide [1]. Although the incidence of CRC in developed countries has declined, it is increasing rapidly in developing countries [2]. Malignant colorectal obstruction (MCO) caused by advanced CRC and other metastatic cancers [3] often requires emergency surgical intervention such as colostomy, colorectal resection, or Hartmann’s procedure [4, 5]. These interventions are associated with a high risk of complications, some of which are life threatening. According to reports, these surgical interventions were associated with mortality and morbidity rates of 15–20 and 40–50 %, respectively [4, 6]. Many patients with MCO have multiple metastases or an unresectable primary malignancy. The ostomy that relieves MCO will never be reversed for those patients and the health-related quality of life will be compromised dramatically for their expected life span [7].
The metallic self-expanding stent (SEMS) introduced by Dohmoto et al. [8] in 1991 has been used for the palliative treatment of MCO [3], gastroduodenal obstruction [9], and bile duct obstruction [10]. In past decades, SEMS was used for treating MCO as a bridge to selective surgery for patients with curable or resectable CRC [11–13], or as an alternative for ostomy or Hartmann’s procedure for MCO in patients with advanced colorectal malignancy [3]. Although SEMS can treat MCO effectively and avoid surgical intervention in most patients with advanced CRC, the short-term (within 30 days after surgery) and long-term (from 30 days after surgery to last follow-up) mortality and morbidity rates are major concerns. In theory, SEMS requires minimal hospitalization and can improve quality of life, but it may reduce survival when the original tumor cannot be removed. Most importantly, SEMS is more tolerable than surgery and can be applied to the patients with cardiovascular or renal dysfunction; however, stent-related perforation can cause life-threat complication and even death. A randomized controlled trial by van Hooft et al. [14] indicated a high incidence of perforation of up to 18 % in the short term and 36 % in the long term. Stent migration and re-obstruction also require a repeat procedure. The oncologic effects of a stent vs. surgery remain uncertain, especially for patients with a resectable metastatic malignancy.
Using a system review and meta-analysis, we compared the outcomes of SEMS alone vs. surgical intervention for patients with an MCO caused by advanced colorectal cancer, in terms of short-term and long-term complications, mortality, and time of hospitalization.
Materials and methods
This study was conducted according to the PRISMA guidelines [15] for reporting system review and meta-analysis.
Literature search
We retrieved the following databases: MEDLINE (1990–31 August 2011), EMBASE (1990–31 August 2011), Cochrane controlled trials registry (updated to 31 August 2011) and Wanfang (Chinese local database, 1990–31 August 2011). The following key words were jointly used: obstruction, stent OR stenting, colorect* OR colon* OR colon OR rectum, randomized OR (randomized trial) OR (randomized controlled trial), (controlled trial) OR (clinical trial). No language limitations were applied. We also manually searched the reference lists of all eligible studies and reviews closely related to our topic, published in the last 5 years.
Inclusion and exclusion criteria
The following criteria were used for the selection of eligible studies:
-
1.
Study design: controlled trials with humans, including randomized controlled and non-randomized controlled trials.
-
2.
Study population: patients with MCO caused by advanced malignancy.
-
3.
Intervention: SEMS alone vs. any surgical treatments.
-
4.
Outcomes: short-term complications, long-term complications, mortality and time of hospitalization. (Only studies including two or more of these outcome measures were included).
The study was excluded, if the outcomes reported did not include the two arms; if they were impossible to calculate indirectly; or if the SEMS was used as a bridge to selective surgery.
Study selection and data extraction
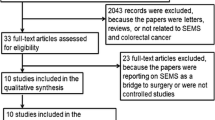
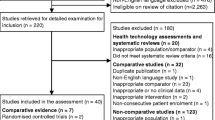
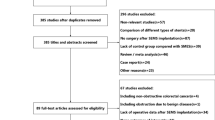
Two authors (T.W. Liang and Y. Sun) identified possible eligible studies independently and then decided on their true eligibility after discussion together. The detailed information leading to study selection or exclusion is presented in the Fig. 1. Briefly, after exclusion of duplications cited among the databases, there were 132 publications that potentially fitted our topic. Through screening the titles and abstracts, 104 studies were excluded. The full texts of 28 studies were then reviewed and 19 were excluded for one or more of the following reasons: the study was not a clinical controlled trial; SEMS was used as a bridge to selective surgery; or the study was irrelevant to our topic. Finally, nine primary studies were analyzed [3, 14, 16–22].
The following details were extracted from the original articles: the first author’s name; the publication year; the simple sizes in two arms; the study design; the obstructive parameters; the outcome parameters, including perforation and death; and information for quality assessment.
Quality assessment
The quality of primary studies, including randomized and non-randomized controlled studies, was assessed by the Newcastle–Ottawa Scale (http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp) with some modifications to fit our study [13, 23]. The modified scale consisted of four parts: patient selection, comparability of study groups, assessment of outcome, and study design (Supplement 1). A maximum of three, four, two and two stars were awarded to above four items, respectively. If the study achieved six or more stars, it was regarded as being of high quality.
Definition of outcomes
The primary outcomes in this meta-analysis were mortality within 30 postoperative days and postoperative complications. The major complications related to SEMS were colorectal perforation, stent migration and re-obstruction. Short-term complications were defined as those that manifested within 30 postoperative days, and long-term complications were defined as those that manifested from 30 postoperative days to the final follow-up or death. The secondary outcomes in this study were the success rate of stent replacement for relieving the MCO and the length of hospitalization.
A lack of data in primary studies or great heterogeneity between patients among original studies precluded us from studying other outcomes such as intervention time, readmission, or survival time.
Statistical analysis
The odds ratio (OR) and 95 % confidence interval (95 %CI) were used to judge the strength of the association for dichotomous variables, and the weighted mean difference (WMD) was used for continuous variables. The Z test was also used to determine significance (P < 0.05). Because of inherent heterogeneity among primary studies originating from different inclusion criteria and variable risk profiles for patients, a random-effect model [24], which could provide a more conservative estimate, was used to combine the data. If continuous data were reported as the median with a range, the mean with standard deviation (SD) was estimated by the method introduced by Hozo et al. [25]. The following situations were impossible for combined analysis: continuous data not presented as means with standard deviation or median with range; in dichotomous data, zero cells reported as outcomes in both the SEMS and surgical groups.
To keep clinical homogeneity and prove the reliability of our study, subgroup analyses were performed by the following variables: (1) study design (prospective or retrospective); (2) types of surgical treatments. The type-I comparison was defined as SEMS vs. colostomy without tumor resection and the type-I/II comparison was defined as SEMS vs. colostomy without tumor resection or surgical treatment with tumor resection. This was because either colostomy or other surgical treatments with tumor resection were carried out for patients in the surgical arm of five original articles [14, 18, 19, 21, 22]; (3) stage IV CRC; (4) left-sided CRC; and (5) high-quality studies.
Publication bias was tested by several methods. Asymmetry of a funnel plot indicated possible publication bias. Begger and Egger’s linear regression tests [26, 27] were used to determine potential publication bias, and P < 0.05 indicated significance. All statistical tests were done by STATA software (version 10.0; Stata Corporation, College Station, TX) with two-sided P values.
Results
Primary characteristics of the included studies
Tables 1 and 2 summarize the basic information in the collective nine primary studies [3, 14, 16–22]. Our study included 410 patients. The sample sizes ranged from 21 to 123. The participants were mainly from western countries, but with one study of Chinese patients [19] and one of Japanese patients [3]. SEMS and surgery were performed to relieve MCO in 195 (47.6 %) patients and 215 patients (52.4 %), respectively. MCO was caused exclusively by advanced colorectal malignancy, especially by stage-IV CRC. The patients in six studies had left-sided MCO only [14, 16, 17, 19, 20, 22]. The age and gender distributions between the SEMS and surgical groups were comparable [WMD (95 %): 2.79 (−1.73, 7.31), P = 0.23 for age and OR (95 %): 0.93 (0.61, 1.42), P = 0.75 for gender]. Three studies [14, 16, 17] were randomized controlled trials and six [3, 18–22] were clinical controlled trials. Seven studies [3, 14, 16–19, 22] were awarded more than six stars and regarded as high quality in the subgroup analysis.
Treatment success
MCO was effectively relieved by surgery in all (100 %) cases and by SEMS in 172 (93.9 %) of 183 cases among 195 patients. The main reasons for failure of SEMS were as follows: the stent was difficult to place because of tortuous flexure of the colorectum, especially when the flexure was splenic or rectosigmoid [17, 20]; the site of obstruction was low [20]; or the colon anatomy had been altered by the tumor and a guidewire could not be passed through the obstruction [18].
Major complications of SEMS
The major complications of SEMS were colorectal perforation, stent migration, and re-obstruction. Five studies [3, 14, 18, 19, 22] reported five cases of perforation in the short term, and four studies [3, 14, 18, 22] reported eight cases of perforation in the long term. The incidence of perforation in these primary studies varied greatly. van Hooft et al. [14] reported the highest short- and long-term incidences of 18 and 36 %, respectively, while other studies reported incidences of 0–8 %. The overall incidences of short- and long-term perforation were 3.7 % (5 cases among 135 patients) and 7.6 % (8 cases among 106 patients), respectively. Although stent migration did not always cause serious adverse events, it required replacement. The incidence of stent migration was reported to range from 5.5 to 10 %, with an overall incidence of 8.9 % (12 cases/135 total patients). Interestingly, none of the primary studies mentioned the incidence of re-obstruction. Table 3 gives details about the complications of SEMS. The three studies [14, 19, 22] that focused on left-sided MCO reported incidences of short- and long-term perforation as well as stent migration of 2.4, 12.3, and 6.3 %, respectively.
Quantitative analysis of complications
All primary studies provided information for the analysis of short-term complications. The overall incidences were 26.2 % (51 cases among 195 patients) after SEMS and 34.5 % (74 cases among 215 patients) after surgery. The results of combined analysis showed no significant difference between the two groups [OR (95 %): 0.83 (0.39, 1.79), P = 0.22; Fig. 2a)]. Seven studies [3, 14, 17, 18, 20–22] reported on the long-term complications of SEMS and surgery, and one [17] did not. Therefore, six primary studies [3, 14, 18, 20–22] provided information for combined analysis. The overall incidences were 16.1 % (25 cases among 155 total patients) after SEMS and 8.1 % (14 cases among 173 patients) after surgery. The patients who underwent SEMS had a significantly higher risk of long-term complications than those who underwent surgery [OR (95 %CI): 2.34 (1.07, 5.14), P = 0.03; Fig. 2b)]. Seven primary studies [3, 14, 17, 18, 20–22] reported on the incidence of complications overall. The incidences in the two groups were 43.9 % (68 cases among 155 total patients) and 45.1 % (78 cases among 173 total patients), respectively. The combined results indicated that patients treated with SEMS and those treated with surgery shared a similar risk of overall complications [OR (95 %CI): 1.27 (0.58, 2.77), P = 0.56].
Six [14, 16, 17, 19, 20, 22], three [14, 20, 22] and four [14, 17, 20, 22] studies provided information on the quantitative analyses of short-term, long-term, and total complications of left-sided MCO, respectively, but none reached significance [OR (95 % CI): 1.10 (0.41, 2.92), P = 0.85 for short-term complication; 3.29 (0.81, 13.38), P = 0.10 for long-term complication; 2.04 (0.61, 6.79), P = 0.25 for total complication].
Quantitative analysis of length of hospitalization
All primary studies reported on the overall length of hospitalization, and seven studies [3, 14, 16, 18–20, 22] were available for combined analysis. The patients who underwent SEMS required significantly shorter hospitalization than those who underwent surgery [WMD (95 % CI): −6.07 (−8.40, −3.74), P < 0.01; Fig. 3). Five studies [14, 16, 19, 20, 22] provided information for the analysis of the length of hospitalization required for the treatment of left-sided MCO. Patients treated with SEMS had significantly shorter hospitalization than those treated with surgery [WMD (95 %CI): −4.94 (6.90, −2.97), P < 0.01].
Quantitative analysis of mortality
The overall mortality rates in the seven studies [3, 14, 18–22] were 7.1 % (12 deaths among 169 patients) for SEMS and 11.6 % (22 deaths among 189 patients) for surgery. These combined results indicated that both procedures had similar risks of mortality [OR (95 % CI): 0.60 (0.27, 1.34), P = 0.22; Fig. 4)]. Similarly, based on the four studies [14, 19, 20, 22] there was no significant difference in the mortality of patients with left-side MCO according to whether they were treated with SEMS or surgery [OR (95 %CI): 0.66 (0.26, 1.70), P = 0.39].
Other subgroup analyses
Table 4 shows the results of comprehensive subgroup analyses. Overall complications and mortality in the two groups did not differ in any of the subgroup comparisons; however, the length of hospitalization was significantly shorter for SEMS than for surgery in all subgroup analyses except for SEMS vs. colostomy [WMD (95 %CI): −7.62 (−22.38, 7.17), P = 0.31].
Publication bias test
We inspected the symmetry of funnel plots and confirmed no publication bias for comparisons of short-term, long-term and overall complications, hospitalization and mortality (Fig. 5a–e). The results of Begger and Egger tests also indicated no publication bias, which might be attributed to the low power of statistics [26, 27] (P Begger = 0.92 and P Egger = 0.94 for short-term complication; P Begger = 0.26 and P Egger = 0.88 for long-term complication; P Begger = 1.00 and P Egger = 0.69 for overall complications; P Begger = 0.55 and P Egger = 0.67 for time of hospitalization; P Begger = 0.92 and P Egger = 0.94 for hospitalization; P Begger = 1.00 and P Egger = 0.84 for mortality).
Discussion
Advanced unresectable CRC is the major cause of MCO, although it has also been associated with other malignancies such as metastatic gastric cancer and metastatic ovarian cancer [3]. It has been reported that about one-third of patients with CRC suffer the symptoms of MCO [28] at some stage, and the most common side of obstruction is the left [29] because most CRC arises in the left side, where the lumen narrows from the ascending colon into the rectum. Traditionally, two-step surgery; namely, Hartmann’s procedure and reversal of ostomy, is needed for resectable CRC, and ostomy is needed to treat MCO in patients with advanced unresectable CRC. These invasive procedures are associated with huge morbidity and mortality risks. Since Dohmoto et al. [8] introduced the metallic stent in 1991, SEMS has been used widely to relieve gastrointestinal obstruction. In 2007, Watt et al. [30] conducted a system review to compare SEMS with surgery for relieving MCO in patients with resectable or unresectable colorectal malignancy. Based on published studies, SEMS is concluded to be safe and effective to overcome left-sided MCO, with a shorter hospital stay and a lower rate of serious events than surgery. Recently, a meta-analysis by Zhang et al. [13] confirmed that SEMS as a bridge to selective surgery increased the chance of primary anastomosis and decreased post-procedure complications and the need for stoma. SEMS has also been widely used to relieve MCO in patients with primary unresectable malignancy or multi-metastatic malignancy. Similarly, the system review indicated that SEMS is effective for relieving MCO in patients with incurable colorectal malignancy.
This meta-analysis indicated that performing SEMS instead of surgery for MCO caused by advanced unresectable malignancy was associated with shorter hospitalization and quicker recovery. Moreover, SEMS and surgical interventions such as colostomy and Hartmann’s procedures had similar risks of short-term complications and mortality; however, SEMS had a higher risk of long-term complications. Although most of these patients with a stoma would never undergo reversal of the stoma considering their survival prediction [31], the complications of stoma reversal should nevertheless be considered. All of the primary studies reported only complications of colostomy or Hartmann’s procedure. It is possible that the risks of morbidity and mortality are much higher for two-step surgery, such as Harmann’s procedure followed later by reversal of the stoma, than for SEMS [32–34]. Furthermore, the subgroup analysis for left-side MCO revealed no significant differences in the long-term and overall complications between the SEMS and surgery groups.
One of the greatest advantages of SEMS for the palliative treatment of MCO is that it eliminates the need for a stoma, which requires a high level of nursing care and compromises both psychology- and physics-related quality of life. The most common complication of stoma is dermatitis [35], while serious complications include parastomal hernia, sclerosis, and stenosis [32, 35]. SEMS is less invasive and consequently better tolerated than surgery, with less suffering. Thus, patients with organ dysfunction, such as renal or heart failure, for whom the risks of surgical morbidity and mortality were too high, were good candidates for SEMS. Cost-effectiveness was also an important advantage of SEMS [21].
Some issues of SEMS should be noted. First, colorectal perforation is a life-threatening complication, which requires emergency surgery. van Hooft et al. [14] reported the highest rates of colorectal perforation: 18 % for short-term perforation and 36 % for long-term perforation, respectively. Another four studies reported lower incidences of perforation at about 0–7.6 %. In the present study, the overall incidences of perforation were 3.7 % in the short term and 7.6 % in the long term. The reasons for perforation are unclear, but the following may be contributing factors: First, persistent high pressure on the colon wall. Insufficient dilation of an obstructive tumor can cause persistent high pressure on the colorectal wall at the site of the proximal tumor, which could lead to ischemia and necrosis. A large stent diameter could also compress the colon wall, predisposing to perforation. Second, optimal design and material of the stent might contribute to a low risk of perforation. van Hooft et al. [14] stated that an association between the incidence of perforation and the design of a new stent could not be excluded. Theoretically, less inflammatory reaction caused by better stent material might help prevent perforation. Third, prolonged and severe obstruction is associated with colonic edema and dysfunction of microvessel blood circle and this pathology would predispose to colonic perforation. Finally, the anatomic location of the stent; for example, if it is in the curved sigmoid colon, might account for a high risk of perforation. This notion was supported by a large review article by Sebastian et al. [36].
Our meta-analysis revealed a higher risk of long-term complications for SEMS than for surgery. Although only a small proportion of the long-term complications of SEMS was life-threatening, we should nevertheless take this into consideration. Moreover, although the incidence of long-term complications after surgery appeared to be low, some serious complications of surgery, such as wound hernia and adhesive intestinal obstruction, always occurred more than 2 years later, whereas the life expectancy of patients with MCO caused by advanced malignancy was often <2 years. Besides, as all of the primary studies focused on SEMS rather than on surgical treatment, it is likely that some of the complications of surgery were omitted. For example, dermatitis is a common complication of colostomy, but this was not mentioned in any primary studies.
Our meta-analysis did not include the oncologic outcomes of SEMS as the great heterogeneity of the patients was reported in the primary studies. The chemoradiotherapy strategies were also different. In theory, SEMS should be the optimal palliative treatment for MCO in patients with advanced unresectable malignancy. Three primary studies reported survival times after colostomy without tumor resection vs. SEMS. Xinopoulos et al. and Johnson et al. [17, 20] reported slightly longer survival after SEMS than colostomy, but without significance. On the other hand, Tomiki et al. [3] reported longer survival after colostomy than after SEMS, but again the difference was not significant. Despite limited data on how SEMS affects survival, it was evident that SEMS had a similar influence to colostomy on the overall survival time of patients with MCO caused by advanced unresectable malignancy. Thus, the effect of SEMS on the prognosis of these patients should be assessed by larger randomized controlled trials.
Like other meta-analyses, this study had potential bias and limitations [10, 13]. First, as the number of patients was small, with relatively low statistical power, the results should be interpreted with caution. Even so, this study provides useful information about treating MCO with SEMS. Second, the literature search strategy was designed before the initiation of this study, and potentially eligible studies were identified by computer-based and manual search; however, it is possible that a few eligible studies were not included. Third, the results of this meta-analysis, a type of retrospective study, could have been distorted by possible selection bias [37]. Fourth, we did not investigate the oncologic effect of SEMS vs. surgical intervention, as great heterogeneity for patients and oncologic treatments were reported in primary studies.
In summary, our meta-analysis showed SEMS to be as effective as surgery for MCO in patients with advanced unresectable colorectal malignancy, with shorter hospitalization, quicker recovery, and comparable risk of short-term complications and mortality. Considering the limitations of this study, larger sample-sized randomized controlled trials are needed to further confirm our findings.
Abbreviations
- CRC:
-
Colorectal cancer
- MCO:
-
Malignant colorectal obstruction
- SEMS:
-
Metallic self-expanding stent
- NOS:
-
Newcastle–Ottawa Scale
- OR:
-
Odds ratio
- WMD:
-
Weighted mean difference
- 95 %CI:
-
95 % Confidence interval
- SD:
-
Standard deviation
References
Jemal A, Siegel R, Xu J, Ward E. Cancer statistics, 2010. CA Cancer J Clin. 2010;60:277–300.
Hyodo I, Suzuki H, Takahashi K, Saito Y, Tanaka S, Chiu HM, et al. Present status and perspectives of colorectal cancer in Asia: colorectal Cancer Working Group report in 30th Asia-Pacific Cancer Conference. Jpn J Clin Oncol. 2010;40(Suppl 1):i38–43.
Tomiki Y, Watanabe T, Ishibiki Y, Tanaka M, Suda S, Yamamoto T, et al. Comparison of stent placement and colostomy as palliative treatment for inoperable malignant colorectal obstruction. Surg Endosc. 2004;18:1572–7.
Breitenstein S, Rickenbacher A, Berdajs D, Puhan M, Clavien PA, Demartines N. Systematic evaluation of surgical strategies for acute malignant left-sided colonic obstruction. Br J Surg. 2007;94:1451–60.
Leong QM, Aung MO, Ho CK, Sim R. Emergency colorectal resections in Asian octogenarians: factors impacting surgical outcome. Surg Today. 2009;39:575–9.
Cuffy M, Abir F, Audisio RA, Longo WE. Colorectal cancer presenting as surgical emergencies. Surg Oncol. 2004;13:149–57.
Jansen L, Koch L, Brenner H, Arndt V. Quality of life among long-term (>/=5 years) colorectal cancer survivors—systematic review. Eur J Cancer. 2010;46:2879–88.
Dohmoto M. New method: endoscopic implantation of rectal stent in palliative treatment of malignant stenosis. Endosc Dig. 1991;3:1507–12.
Chandrasegaram MD, Eslick GD, Mansfield CO, Liem H, Richardson M, Ahmed S, et al. Endoscopic stenting versus operative gastrojejunostomy for malignant gastric outlet obstruction. Surg Endosc. 2011. doi:10.1007/s00464-011-1870-3.
Saleem A, Leggett CL, Murad MH, Baron TH. Meta-analysis of randomized trials comparing the patency of covered and uncovered self-expandable metal stents for palliation of distal malignant bile duct obstruction. Gastrointest Endosc. 2011;74:321–7 (e1–3).
van Hooft JE, Bemelman WA, Oldenburg B, Marinelli AW, Holzik MF, Grubben MJ, et al. Colonic stenting versus emergency surgery for acute left-sided malignant colonic obstruction: a multicentre randomised trial. Lancet Oncol. 2011;12:344–52.
Pirlet IA, Slim K, Kwiatkowski F, Michot F, Millat BL. Emergency preoperative stenting versus surgery for acute left-sided malignant colonic obstruction: a multicenter randomized controlled trial. Surg Endosc. 2011;25:1814–21.
Zhang Y, Shi J, Shi B, Song CY, Xie WF, Chen YX. Self-expanding metallic stent as a bridge to surgery versus emergency surgery for obstructive colorectal cancer: a meta-analysis. Surg Endosc. 2011. doi:10.1007/s00464-011-1835-6.
van Hooft JE, Fockens P, Marinelli AW, Timmer R, van Berkel AM, Bossuyt PM, et al. Early closure of a multicenter randomized clinical trial of endoscopic stenting versus surgery for stage IV left-sided colorectal cancer. Endoscopy. 2008;40:184–91.
Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gotzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. Ann Intern Med. 2009;151:W65–94.
Fiori E, Lamazza A, De Cesare A, Bononi M, Volpino P, Schillaci A, et al. Palliative management of malignant rectosigmoidal obstruction. Colostomy vs. endoscopic stenting. A randomized prospective trial. Anticancer Res. 2004;24:265–8.
Xinopoulos D, Dimitroulopoulos D, Theodosopoulos T, Tsamakidis K, Bitsakou G, Plataniotis G, et al. Stenting or stoma creation for patients with inoperable malignant colonic obstructions? Results of a study and cost-effectiveness analysis. Surg Endosc. 2004;18:421–6.
Vemulapalli R, Lara LF, Sreenarasimhaiah J, Harford WV, Siddiqui AA. A comparison of palliative stenting or emergent surgery for obstructing incurable colon cancer. Dig Dis Sci. 2010;55:1732–7.
Law WL, Choi HK, Chu KW. Comparison of stenting with emergency surgery as palliative treatment for obstructing primary left-sided colorectal cancer. Br J Surg. 2003;90:1429–33.
Johnson R, Marsh R, Corson J, Seymour K. A comparison of two methods of palliation of large bowel obstruction due to irremovable colon cancer. Ann R Coll Surg Engl. 2004;86:99–103.
Varadarajulu S, Roy A, Lopes T, Drelichman ER, Kim M. Endoscopic stenting versus surgical colostomy for the management of malignant colonic obstruction: comparison of hospital costs and clinical outcomes. Surg Endosc. 2011;25:2203–9.
Carne PW, Frye JN, Robertson GM, Frizelle FA. Stents or open operation for palliation of colorectal cancer: a retrospective, cohort study of perioperative outcome and long-term survival. Dis Colon Rectum. 2004;47:1455–61.
Athanasiou T, Al-Ruzzeh S, Kumar P, Crossman MC, Amrani M, Pepper JR, et al. Off-pump myocardial revascularization is associated with less incidence of stroke in elderly patients. Ann Thorac Surg. 2004;77:745–53.
DerSimonian R, Laird N. Meta-analysis in clinical trials. Control Clin Trials. 1986;7:177–88.
Hozo SP, Djulbegovic B, Hozo I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med Res Methodol. 2005;5:13.
Begg CB, Mazumdar M. Operating characteristics of a rank correlation test for publication bias. Biometrics. 1994;50:1088–101.
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315:629–34.
Deans GT, Krukowski ZH, Irwin ST. Malignant obstruction of the left colon. Br J Surg. 1994;81:1270–6.
Biondo S, Pares D, Frago R, Marti-Rague J, Kreisler E, De Oca J, et al. Large bowel obstruction: predictive factors for postoperative mortality. Dis Colon Rectum. 2004;47:1889–97.
Watt AM, Faragher IG, Griffin TT, Rieger NA, Maddern GJ. Self-expanding metallic stents for relieving malignant colorectal obstruction: a systematic review. Ann Surg. 2007;246:24–30.
Salem L, Anaya DA, Roberts KE, Flum DR. Hartmann’s colectomy and reversal in diverticulitis: a population-level assessment. Dis Colon Rectum. 2005;48:988–95.
Chow A, Tilney HS, Paraskeva P, Jeyarajah S, Zacharakis E, Purkayastha S. The morbidity surrounding reversal of defunctioning ileostomies: a systematic review of 48 studies including 6,107 cases. Int J Colorectal Dis. 2009;24:711–23.
Huynh H, Trottier DC, Soto CM, Moloo H, Poulin EC, Mamazza J, et al. Laparoscopic colostomy reversal after a Hartmann procedure: a prospective series, literature review and an argument against laparotomy as the primary approach. Can J Surg. 2011;54:133–7.
Molina Rodriguez JL, Flor-Lorente B, Frasson M, Garcia-Botello S, Esclapez P, Espi A, et al. Low rectal cancer: abdominoperineal resection or low Hartmann resection? A postoperative outcome analysis. Dis Colon Rectum. 2011;54:958–62.
Caricato M, Ausania F, Ripetti V, Bartolozzi F, Campoli G, Coppola R. Retrospective analysis of long-term defunctioning stoma complications after colorectal surgery. Colorectal Dis. 2007;9:559–61.
Sebastian S, Johnston S, Geoghegan T, Torreggiani W, Buckley M. Pooled analysis of the efficacy and safety of self-expanding metal stenting in malignant colorectal obstruction. Am J Gastroenterol. 2004;99:2051–7.
Verstraete M. Value and limitation of meta-analysis. Pathophysiol Haemost Thromb. 2002;32:278–81.
Acknowledgments
This study was supported by a Self-Raised Research Grant Approved by Department of Public Health of Guang Xi Province, China (Grant No.: Z2012706).
Conflict of interest
None of the authors have any conflicts of interest to declare.
Author information
Authors and Affiliations
Corresponding author
Additional information
T. W. Liang and Y. Sun contributed equally to this study.
Electronic supplementary material
Below is the link to the electronic supplementary material.
Rights and permissions
About this article
Cite this article
Liang, Tw., Sun, Y., Wei, Yc. et al. Palliative treatment of malignant colorectal obstruction caused by advanced malignancy: a self-expanding metallic stent or surgery? A system review and meta-analysis. Surg Today 44, 22–33 (2014). https://doi.org/10.1007/s00595-013-0665-7
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-013-0665-7