Abstract
Purposes
The aim of this study was to assess the relationship between the pulmonary hydatid cyst size and the clinical presentation, surgical approach, and postoperative outcome. We review the problems encountered in treating large pulmonary hydatid cysts and highlight the risks associated with the rupture of the cyst and a delay of the surgical treatment.
Methods
The medical records of 169 patients surgically treated for lung hydatid cysts were reviewed. Patients were divided into two groups based on cyst size: group 1 (n = 128) with small (<10 cm) cysts and group 2 (n = 41) with giant (≥10 cm) cysts. Data related to symptoms, preoperative complications, surgical procedures performed and postoperative morbidity were analyzed and compared.
Results
In both groups, the most common symptom was chest pain, followed by dyspnea and cough, respectively. There were no differences between the two groups with respect to cyst-associated parenchymal or pleural complications before surgery (p = 0.80). In the large majority of cases, the surgical treatment was cystotomy, removal of the cystic membrane and capitonnage. Wedge resection was performed in nine patients in total (seven in group 1, two in group 2) and one patient in group 2 required a lobectomy. Decortication was required significantly more frequently in group 2 than in group 1 (p = 0.001). Sixteen patients in group 1 and 10 patients in group 2 developed postoperative complications (p = 0.19). There was no peri or postoperative mortality. There was no difference between the groups with respect to the duration of hospitalization (p = 0.17). Two patients with complicated hydatid cysts in group 1 had recurrent lesions during follow-up, whereas there was no recurrence in group 2.
Conclusion
All pulmonary hydatid cysts should be surgically treated as soon as possible after their diagnosis in order to avoid complications. Most of these lesions, regardless of size, can be surgically managed with procedures that preserve the maximal lung parenchyma and yield excellent outcomes.
Similar content being viewed by others
Explore related subjects
Discover the latest articles, news and stories from top researchers in related subjects.Avoid common mistakes on your manuscript.
Introduction
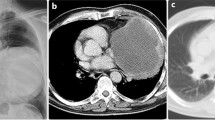
Hydatidosis caused by Echinococcus granulosus is the most common parasitic disease of the lung in humans. When an E. granulosus hexacanth becomes trapped in an arterial capillary of the lung, the larva transforms into a hydatid cyst and develops silently during the first few years [1]. Over time, such cysts enlarge to various sizes depending on their location, the elasticity of the surrounding pulmonary tissue, and the patient’s pulmonary reserve and immune response [2]. Some of these cysts rupture. In general, hydatid cysts of the lung that are 10 cm in diameter or larger are defined as “giant” [3–5].
The clinical presentation of pulmonary hydatid cysts depends on whether the lesion is intact or ruptured. In most cases, intact or asymptomatic hydatid cysts are incidental findings on chest X-rays; however, patients with large cysts may have symptoms that reflect compression of organs adjacent to the lesion. Large lung hydatid cysts can cause complications and increased morbidity, and therefore, clinicians and surgeons need to manage these cysts carefully [4]. Surgery is widely considered the best choice for treating pulmonary hydatid cysts of any size. Some surgeons treat giant hydatid cysts of the lung with various forms of resection, such as lobectomy or pneumonectomy [6–8]. Others suggest that, regardless of size, these lesions should be addressed with conservative surgical methods [4, 9]. In this study, our aim was to assess the relationship between the pulmonary hydatid cyst size and the clinical presentation and treatment approach. We retrospectively compared the findings in groups of patients with small or giant pulmonary hydatid cysts.
Materials and methods
The study involved 169 consecutive patients with pulmonary hydatid cysts who were treated surgically at Turgut Ozal Medical Center between January 2000 and December 2010, and at Erzurum Regional Training and Research Hospital between January 2009 and December 2010. Patients were evaluated with various combinations of chest roentgenography, thoracic computed tomography, and upper abdominal ultrasonography and/or computed tomography. Skin and serologic testing were not part of the routine diagnostic workup. Cysts that had ruptured into the bronchus or pleural cavity were defined as complicated. The patients were grouped according to cyst size: small (<10 cm) in group 1 or giant (≥10 cm) in group 2.
In the majority of cases, the surgical treatment was a procedure involving cystotomy, removal of the cystic membrane, and capitonnage. Unlike excision, these steps generally involve emptying the cyst and then suturing to obliterate the cavity and close its edges. Specifically, the cyst contents were evacuated by needle aspiration, and the cystic membrane was removed with ring forceps. The cyst cavity was then irrigated with saline solution, and the walls were wiped with sponges soaked in povidone-iodine (10 %). Anti-scolicidal agents were not used because of the risks of severe edema, airway spasm, and chemical pneumonia. Any bronchial openings in the cavity wall were closed with absorbable sutures in a figure-eight pattern. Once this was done, the cavity was obliterated. In the cases of small cysts, our standard procedure was to place multiple separate purse-string sutures in the cavity starting at the deepest level and ending at the lung surface. In the cases of giant cysts, we placed interrupted single U-shaped sutures in horizontal rows in the walls of the cavity starting deep and ending at the surface.
Of the patients who did not undergo the procedure described above, some underwent decortication, and others were treated with wedge resection or lobectomy. After surgery, all patients with complicated hydatid cysts or multiple hydatid cysts, or both, were placed on anthelmintic therapy (albendazole 800 mg/day for adults, 10 mg/kg/day for children) for at least 2 months. Patients with uncomplicated or single cysts received no antiparasitic medication after their operation.
The data related to symptoms, preoperative complications, surgical procedures performed, postoperative morbidity, and the length of hospitalization were collected from medical records, and the group findings were compared. The statistical analyses were done using the Yates corrected Chi-square test, Fisher’s exact test, or Mann–Whitney U test, as appropriate. P < 0.05 was considered to indicate statistical significance.
Results
Of the 169 patients, 92 were males and 77 were females, and their mean age was 33 years (range, 4–79 years). Group 1 (small cysts) had 128 patients with a mean age of 34 years (range, 4–79 years) and underwent a total of 147 surgeries. The 19 additional operations were required for bilateral pulmonary hydatid cysts (n = 16), recurrent cysts (n = 2), and repeat thoracotomy to address persistent air leakage in the early postoperative period (n = 1). One hundred and six of the patients in group 1 underwent cystotomy and capitonnage. Fifteen patients required a combination of cystotomy, capitonnage, and decortication, and seven were managed with wedge resection. None of the small cyst cases required lobectomy.
Group 2 (giant cysts) had 41 patients with a mean age of 29 years (range, 4–68 years), and underwent 44 surgeries. The additional three operations were required for bilateral hydatid cysts (n = 2) and repeat thoracotomy due to intrathoracic hematoma in the early postoperative period (n = 1). Thirty-three of the patients in group 2 underwent cystotomy and capitonnage. Fifteen patients in group 2 required cystotomy, capitonnage, and decortication; two patients were managed with wedge resection and one required lobectomy.
In both groups, the most common symptom was chest pain (68.8 %), followed by dyspnea (34.4 %) and cough (19.5 %) (Table 1). Fifty-one (39.8 %) of the 128 patients in group 1 had complicated cysts. Forty-seven of these cases (36.7 % of group 1; 92.2 % of complicated group 1 cases) were cyst ruptures into the bronchial system, and four (3.1 % of group 1; 7.8 % of complicated group 1 cases) were ruptures into the pleural space. Twenty-two (53.7 %) of the 41 patients in group 2 had complicated cysts. Thirteen of these (31.7 % of group 2; 59.1 % of complicated group 2 cases) were ruptures into the bronchial system and nine (22 % of group 2; 40.9 % of complicated group 2 cases) were ruptures into the pleural space. There were no significant differences in the overall frequencies of complicated cysts in groups 1 and 2 (p = 0.17); however, the group frequencies of cyst rupture into the pleural cavity were significantly different (p = 0.002).
Thirty-six patients in group 1 and 13 in group 2 had cyst-associated parenchymal or pleural complications prior to surgery (Table 2), but these frequencies were not significantly different (28.1 vs. 31.7 %, respectively; p = 0.80). Significantly most of the group 2 patients required decortication compared to group 1 (11.7 vs. 36.6 %, respectively; p = 0.001). Eighteen patients in group 1 and 10 in group 2 developed postoperative complications (14.1 vs. 24.4 %, respectively; p = 0.19) (Table 3). There were no peri or postoperative deaths. The mean length of hospitalization for group 1 was 14.1 days (range, 7–74 days), and that for group 2 was 13.3 days (range, 7–19 days) (p = 0.17). Two of the group 1 patients with complicated cysts developed recurrence during follow-up, whereas none of the giant cysts recurred.
Discussion
Giant hydatid cysts of the lung are known to occur more often in childhood and young adulthood than at older ages, and the suggested reasons for this are the more elastic lung tissue and incomplete immune system development in children and adolescents [3, 10]. In young patients with giant pulmonary hydatid cysts, the lesion can expand, while the remaining healthy lung tissue provides sufficient ventilation, whereas such cysts in adults typically become symptomatic before they reach a giant size [5]. In our study, 26 (63.4 %) of the 41 patients with giant hydatid cysts of the lung were aged 30 years or younger.
Pulmonary hydatid cysts can remain asymptomatic until they become very large or until they rupture. A larger hydatid cyst volume places more pressure on surrounding tissues. Such cysts are more likely to cause chest pain and cough due to bronchial and/or pleural irritation [10], and to cause dyspnea by compressing the lung parenchyma. In our study, the group with giant cysts had a slightly larger proportion of patients with dyspnea at presentation and a significantly larger proportion of patients with cough at presentation than the small-cyst group. The clinical picture of patients with ruptured hydatid lung cysts varies and depends on the direction in which the lesion perforates. When a cyst ruptures into the pleural cavity or the bronchial tree, massive numbers of E. granulosus scolices are disseminated, and this can obstruct airways or lead to anaphylactic shock. When there is rupture into a bronchus, the patient may present expectorating hydatid fluid and remnants of the cyst membrane or may have recurrent hemoptysis, purulent sputum, fever or a combination of some or all of these symptoms [11]. The rupture of a hydatid cyst into the pleural cavity is usually associated with more serious clinical presentations, such as simple or tension pneumothorax, empyema or pyopneumothorax [11].
Some authors suggest that a large diameter of a pulmonary hydatid cyst increases its propensity to rupture [4, 9]; however, we found no statistically significant difference between our small cyst and giant cyst groups with respect to the overall frequency of complicated (ruptured) lesions. According to the literature, hydatid cysts of the lung are more likely to rupture into the bronchial system [12]. We observed this in both of our study groups, but we did note that there was a significantly higher rate of rupture into the pleural cavity among the patients with giant cysts. It seems logical that a ruptured giant cyst would have more severe clinical manifestations than a ruptured small hydatid cyst, because giant hydatid lung cysts are more likely to cause pleural complications. The presence of the major vascular and bronchial structures in the central area of the lung prevents hydatid cysts in that region from expanding. Consequently, the cyst diameters tend to be larger in the more peripheral lung regions, where the bronchial and vascular structures are smaller. As hydatid cysts expand in these areas, the parenchyma that is between the lesion and the pleural space becomes compressed, such that the cyst wall is closer to the lung surface. Necrosis of the pleura caused by pressure from a growing hydatid cyst is thought to be an important factor in cyst rupture into the pleural cavity [12].
Some authors contend that oral albendazole treatment regimens are effective against hydatid cysts of the lung [13, 14]. The fundamental issue here is not the efficacy of anthelmintic therapy (mebendazole, albendazole), but whether this form of treatment leads to complications. Anthelmintic therapy causes degenerative changes in the hydatid cyst wall [15], which could increase the likelihood of rupture. Keramidas et al. [14] reported that patients with large hydatid cysts of the lung (>6-cm diameter) developed complications after anthelmintic therapy. They described problematic surgeries and postoperative courses in patients who required surgery for complications of antiparasitic treatment. Specifically, they noted that it was difficult to suture the bronchial openings due to coexisting infection, and that these closure problems led to prolonged air leakage postoperatively. In addition, other authors have suggested that the larger the diameter of the cyst, the greater the possibility that medical treatment will fail [16]. Kuzucu et al. [11] reported previously that patients with complicated hydatid cysts of the lung have higher rates of pre and postoperative complications, and require longer hospitalization and more extensive surgical procedures than uncomplicated cases. This underlines the need for immediate surgery in patients with giant hydatid cysts of the lung.
Another consideration in treating pulmonary hydatidosis is the potential for problems during follow-up in patients on medical therapy. If the antiparasitic agent weakens the cyst wall to the point where it ruptures, urgent surgery may be required; however, many patients with this disease reside in rural areas remote from medical care, and so, anthelmintic therapy carries an additional risk in these settings [11, 17]. One group of researchers observed that the timing of pulmonary hydatid cyst rupture after the initiation of anthelmintic treatment varied considerably, from 10 days to 2 months [15]. Keramidas et al. [14] reported that most patients who developed complications during anthelmintic therapy (mebendazole or albendazole) for lung hydatid cysts presented approximately 2 months after the start of treatment. Clearly, any patient who receives medical therapy for these cysts must be followed closely for at least 2 months.
When surgically treating pulmonary hydatid cysts of the lung, procedures that maximize the protection of the lung parenchyma are always preferred. Recent reports have noted rates of 0–10.3 % for anatomical resection (lobectomy or pneumonectomy, for example) for these lesions [18, 19]. In contrast, Fracs et al. [6] reported that 26 % of patients underwent lobectomy or pneumonectomy in their series of 763 patients with hydatid cysts of the lung, Vasquez et al. [7] noted a 58 % lobectomy or pneumonectomy rate in 115 such cases, and Safioleas et al. [8] reported that 74 % of their 42 patients underwent lobectomy or pneumonectomy. These rates are markedly higher than those reported in most published series of lung hydatid disease [11, 16, 18–20]. These authors stated that their high rates of extensive lung resection reflected the large proportions of patients with giant cysts or ruptured and infected cysts in their series. However, other reports have revealed that lobectomy or pneumonectomy was needed in 0–15.7 % of patients with complicated pulmonary hydatid cysts [11, 20] and in 0–16 % of patients with giant pulmonary hydatid cysts [2–5, 9, 10, 21]. In our investigation of 169 cases of small or giant hydatid cysts of the lung, only one patient (a case of giant hydatid cyst) required lobectomy. Previously, Kuzucu, et al. [11] and Kuzucu [17] stated that radical resection is too aggressive for managing pulmonary hydatid disease, even in patients with giant cysts, multiple cysts, or lung abscesses. The surgical removal of all parasitic material from hydatid cyst sites in the lung is usually adequate. Often, the lung parenchyma that surrounds these lesions is damaged and there may be chronic congestion, hemorrhage, bronchopneumonia, or interstitial pneumonia [22]. Such inflammatory changes often resolve after surgery for cyst removal. Most authors agree that every attempt should be made to remove as little lung tissue as possible, and that resection of the pulmonary parenchyma is only indicated when the adjacent tissue is seriously damaged or infected, or when atelectatic areas are assessed as irrecoverable [1, 2, 4, 11, 18, 20, 23].
It can be difficult to determine the optimal surgical procedure when a giant hydatid cyst has compressed a considerable amount of lung parenchyma for a long period, and this decision may have to be made in the operating room. Halezeroglu et al. [2] stated that, given the good recovery of lung tissue in patients with giant hydatid lesions, the cyst size (at least as a single factor) should not be an indication for resection. Some authors have suggested that open surgery, in which the cyst membrane is removed and bronchial openings into the cyst cavity are closed (i.e., a procedure without capitonnage), is the most appropriate approach for pulmonary hydatid cysts [24, 25]. These authors found that capitonnage had no benefit in this patient group with respect to postoperative variables and short- and long-term surgical complications. However, Kosar et al. [26] and Bilgin et al. [27] noted a significantly lower frequency of postoperative complications in patients with pulmonary hydatidosis who had undergone capitonnage (as opposed to no capitonnage), and they found this procedure to be associated with a better postoperative outcome. Nabi et al. [28] investigated the surgical outcomes in 66 patients with pulmonary hydatid cysts. They observed significant postoperative complications (prolonged air leakage and empyema, for example) in their first five cases that were managed surgically without capitonnage, and they had to abandon the non-capitonnage technique on ethical grounds.
Postoperative complications can be expected in cases of giant hydatid cyst of the lung, because many of these cysts are complicated (ruptured) and larger cysts tend to communicate with more bronchi than smaller cysts. Capitonnage offers an advantage in cases of giant pulmonary hydatid cyst because of the numerous airway openings and because the number of openings and various degrees of pericystic inflammation tend to make it difficult to achieve closure with single sutures [21]. Given these issues, we also prefer to obliterate the cavity (i.e., perform capitonnage) after surgically removing the cyst membrane and closing the bronchial openings. Celik et al. [23] observed that atelectasis can develop after capitonnage of a pulmonary hydatid cyst due to obliteration of an adjacent bronchus. Shrinkage and disfigurement of the lung parenchyma after conventional capitonnage of these cysts can, indeed, be a problem, especially when addressing cavities of giant cysts. For this reason, in cases of giant pulmonary hydatid cysts, we prefer to do capitonnage using interrupted separate U-shaped sutures, rather than O-shaped purse-string sutures. However, the decision whether or not to perform capitonnage ultimately depends on the surgeon’s experience and preference.
Some of our patients with giant hydatid cysts had pleural complications, and thus, required more extensive surgical procedures, such as decortication. The literature reports decortication rates of approximately 69 % for cases of pulmonary hydatid cysts with such complications [12, 29]. Aribas et al. [12] reported a rate of 14 % for radical pulmonary resection in 43 patients with lung hydatid cysts and pleural complications. These findings suggest that, although lobectomy or pneumonectomy is not generally required in this patient group, pleural complications are associated with more serious morbidity and more extensive surgery, such as decortication. Avoiding these complications is another reason why it is important to surgically treat giant pulmonary hydatid cysts as soon as possible after diagnosis.
Numerous reports have indicated that patients with giant hydatid cysts of the lung have postoperative complication rates of 10–25 %, and these are higher than those in patients with small cysts [2, 3, 5, 9, 10]. In our study, although the difference was not significant, our group with giant cysts had a higher rate of postoperative complications (24.4 %) than our group with small cysts (14.1 %), and prolonged air leak was the most common problem. However, all complications, except intrathoracic hematoma, were managed conservatively.
In summary, surgery should be performed as soon as possible after a diagnosis of pulmonary hydatidosis, and this is particularly important with giant cysts. Patients with giant hydatid cysts of the lung often have a complicated clinical picture, and these lesions may require more extensive surgery than smaller cysts. Preservation of the lung parenchyma is fundamental in the surgical management of pulmonary hydatidosis, regardless of the cyst size or presence/absence of complications. In almost all cases of this disease, it is possible to avoid radical resection and use a procedure that preserves the lung parenchyma and yields excellent outcomes.
References
Ramos G, Orduna A, Garcia-Yusta M. Hydatid cyst of the lung: diagnosis and treatment. World J Surg. 2001;25:46–57.
Halezeroglu S, Celik M, Uysal A, Senol C, Keles M, Arman B. Giant hydatid cysts of the lung. J Thorac Cardiovasc Surg. 1997;113:712–7.
Karaoglanoglu N, Kurkcuoglu IC, Gorguner M, Eroglu A, Turkyilmaz A. Giant hydatid lung cysts. Eur J Cardiothorac Surg. 2001;19:914–7.
Dakak M, Caylak H, Kavakli K, Gozubuyuk A, Yucel O, Gurkok S, et al. Parenchyma-saving surgical treatment of giant pulmonary hydatid cysts. J Thorac Cardiovasc Surg. 2009;57:165–8.
Kocer B, Gulbahar G, Han S, Durukan E, Dural K, Sakinci U. An analysis of clinical features of pulmonary giant hydatid cyst in adult population. Am J Surg. 2009;197:177–81.
Fracs JS, Alizzi A, Alward M, Konstantinow I. Thoracic hydatid disease: a review of 763 cases. Heart Lung Circ. 2008;17:502–4.
Vasquez JC, Montesinos E, Peralta J, Rojas L, DeLaRosa J, Leon JJ. Need for lung resection in patients with intact or ruptured hydatid cysts. Thorac Cardiovasc Surg. 2009;57:295–302.
Safioleas M, Misiakos EP, Dosios T, Manti C, Lambrou P, Skalkeas G. Surgical treatment for lung hydatid disease. World J Surg. 1999;23:1181–5.
Usluer O, Ceylan KC, Kaya S, Sevinc S, Gursoy S. Surgical management of pulmonary hydatid cysts. Is size an important prognostic indicator? Tex Heart Inst J. 2010;37:429–34.
Arroud M, Afifi A, El Ghazi K, Nejjari C, Bouabdallah Y. Pulmonary hydatid cysts in children: comporison study between giant and non-giant cysts. Pediatr Surg Int. 2009;25:37–40.
Kuzucu A, Soysal O, Ozgel M, Yologlu S. Complicated hydatid cysts of the lung: clinical and therapeutic issues. Ann Thorac Surg. 2004;77:1200–4.
Aribas OK, Kanat F, Gormus N, Turk E. Pleural complications of hydatid disease. J Thorac Cardiovasc Surg. 2002;123:492–7.
Keshmiri M, Baharvahdat H, Fattahi SH, Davachi B, Dabiri RH, Baradaran H, et al. A placebo controlled study of albendazole in the treatment of pulmonary echinococcosis. Eur Respir J. 1999;14:503–7.
Keramidas D, Mavridis G, Soutis M, Passalidis A. Medical treatment of pulmonary hydatidosis: complications and surgical management. Pediatr Surg Int. 2004;19:774–6.
Todorov T, Vutova K, Donev S, Ivanov A, Katzarov K, Takov D. The types and timing of the degenerative changes seen in the cysts during and after benzimidazole treatment of cystic echinococcosis. Ann Trop Med Parasitol. 2005;99:649–59.
Doğru D, Kiper N, Ozçelik U, Yalçin E, Göçmen A. Medical treatment of pulmonary hydatid disease: for which child? Parasitol Int. 2005;54:135–8.
Kuzucu A. Parasitic disesases of the respiratory tract. Curr Opin Pulm Med. 2006;12:212–21.
Kavukcu S, Kilic D, Tokat AO, Kutlay H, Cangir AK, Enon S, et al. Parenchyma-preserving surgery in the management of pulmonary hydatid cysts. J Invest Surg. 2006;19:61–8.
Bagheri R, Haghi SZ, Amini M, Fattahi AS, Noorshafiee S. Pulmonary hydatid cyst: analysis of 1024 cases. Gen Thorac Cardiovasc Surg. 2011;59:105–9.
Balci AE, Eren N, Eren S, Ulku R. Ruptured hydatid cysts of the lung in children: clinical review and results of surgery. Ann Thorac Surg. 2002;74:889–92.
Ekim H, Ozbay B, Kurnaz M, Tuncer M, Ekim M. Management of complicated giant thoracic hydatid disease. Med Sci Monit. 2009;15:600–5.
Sakamoto T, Gutierrez C. Pulmonary complications of cystic echinococcosis in children in Uruguay. Pathol Int. 2005;55:497–503.
Celik M, Senol C, Keles M, Halezaroglu S, Urek S, Haciibrahimoglu G, et al. Surgical treatment of pulmonary hydatid disease in children: report of 122 cases. J Pediatr Surg. 2000;35:1710–3.
Erdogan A, Ayten A, Demircan A. Methods of surgical therapy in pulmonary hydatid disease: is capitonnage advantageous. ANZ J Surg. 2005;75:992–6.
Turna A, Yılmaz MA, Haciibrahimoglu G, Kutlu CA, Bedirhan MA. Surgical treatment of pulmonary hydatid cysts: is capitonnage necessary? Ann Thorac Surg. 2002;74:191–5.
Kosar A, Orki A, Haciibrahimoglu G, Kiral H, Arman B. Effect of capitonnage and cystotomy on outcome of childhood pulmonary hydatid cysts. J Thorac Cardiovasc Surg. 2006;132:560–4.
Bilgin M, Oguzkaya F, Akcali Y. Is capitonnage unnecessary in the surgery of intact pulmonary hydatid cyst? ANZ J Surg. 2004;74:40–2.
Nabi MS, Waseem T, Tarif N, Chima KK. Pulmonary hydatid disease: is capitonnage mandatory following cystotomy? Int J Surg. 2010;8:373–6.
Ozvaran MK, Ersoy Y, Uskul B, Unver E, Yalcin E, Baran R, et al. Pleural complications of pulmonary hydatid disease. Respirology. 2004;9:115–9.
Acknowledgments
We thank Cemil Colak (Department of Biostatistics, Faculty of Medicine, Inonu University) for his valuable work analyzing the statistical data in this study.
Conflict of interest
Akin Kuzucu and Co-authors have no financial relationship with the organization that sponsored the research.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Kuzucu, A., Ulutas, H., Reha Celik, M. et al. Hydatid cysts of the lung: lesion size in relation to clinical presentation and therapeutic approach. Surg Today 44, 131–136 (2014). https://doi.org/10.1007/s00595-012-0484-2
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00595-012-0484-2