Abstract
Purpose
The aim of this study is to review our experience in pediatric giant pulmonary hydatid cysts focusing on clinical symptoms, location of the cyst, type of the intervention, postoperative complications and long-term results.
Methods
Between June 2002 and May 2007, 118 children were operated on for hydatid lung cysts. Two groups were defined: Group 1, 32 children with giant hydatid cysts and Group 2, 86 children with non-giant cysts. The statistical significance between the groups was estimated using paired samples t test.
Results
The mean age was 11.8 years in G1 and 9.7 years in G2. All of the patients were symptomatic in G1 but only 18% in G2 (P = 0.003). The right lower lobe was most frequently involved in both G1 and G2. Surgical parenchymal resection was performed in five patients in G1 (16%) and in 2% in G2 (P = 0.033). Postoperative complications in G1 were more significant comparatively to G2 (P = 0.003).
Conclusion
Giant hydatid lung cysts represent a distinct pathology. They affect essentially adolescents and may reach a large size causing parenchymal destruction. Thus, surgical resections are frequently used and postoperative complications rate is high.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
Hydatic disease is a parasitic infection caused by the cestode, Echinococcus granulosus. It is still endemic in Mediterranean countries [1]. The lung and the liver are the most frequently involved organs. Giant hydatid cysts of the lung constitute a distinct clinical entity most frequently encountered in adolescents [2]. To date, there are few studies of giant lung hydatid cysts. All of them included both adults and children [2, 3]. To the best of our knowledge, there is only one study in the literature specially dedicated to pediatric population [4]. However, there were only three reported patients. Hence, we aimed to expose our experience in the surgical management of pulmonary giant hydatid cysts in children through reviewing 32 cases operated in our department during the last 5 years.
Patients and methods
Between June 2002 and May 2007, 118 children were operated on for hydatid lung cysts in the Department of Pediatric Surgery, University Hospital Hassan II, Fez. Our patients were separated into two groups: Group 1, children with giant hydatid cysts (G1) and Group 2, children with non-giant cysts (G2).
Lung hydatid cysts measuring more than 10 cm, in the largest diameter, were defined as giants.
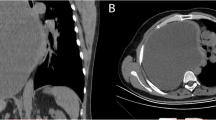
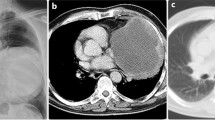
The size of the cyst was determined by conventional radiography (Fig. 1), computerized tomography (Fig. 2) and/or intraoperative findings.
Indirect hemagglutination test for echinococcosis as well as conventional radiography and abdominal ultrasonography were performed in all patients. Thoracic CT scan was done in cases of giant hydatid cysts, complicated cysts and in cases where the diagnosis of hydatid cysts was not clearly established.
In the postoperative stage, all patients have had systematically antero-posterior chest radiography per month for 3 months. Then, a conventional radiography was performed at the sixth month and at the end of the first year (Fig. 3).
A retrospective analysis was performed using clinical charts, biologic tests and radiologic investigations. Comparison between the two groups was focused on age, clinical symptoms, diameter of the cyst, location, type of the intervention, postoperative complications and long-term results. The statistical significance between the groups was estimated using Chi-square test. A P value of less than 0.05 was considered significant. Correlation coefficients were also estimated using Pearson’s test.
Results
In our series, 32 children had giant hydatid lung cysts (G1) whereas 86 children were diagnosed as having non-giant hydatid cysts (G2).
In both G1 and G2, the age was ranged between 5 and 16 years. The mean age was 11.8 years in G1, while it was found as 9.7 years in G2. The difference between the two groups was statistically non-significant (P = 0.43).
All of the patients were symptomatic in G1. The most common symptoms were cough (83%), thoracic pain (37%), hemoptysis (26%), fever (15%) and purulent sputum (12%). In G2, only 18% had clinical manifestations (P = 0.003).
In G1, 19 of the cysts (60%) were located in the right lung and 13 (40%) in the left. The right lower lobe was the most frequently involved in both G1 and G2. Nine patients (28%) presented with complicated hydatid cysts in G1; three cysts were ruptured and six were both ruptured and infected. None of the patients had reported any allergic or anaphylactic episodes after cyst rupture.
Associated liver hydatid cysts were found in 4 children in G1 and in 12 patients in G2.
Single lung ventilation and posterolateral thoracotomy were performed in all cases in G1 and in 85% in G2. The remaining patients in G2 (15%) were treated by thoracoscopy.
In G1, after protection of the surrounding tissues with gauze impregnated by scolocidal agent, we systematically proceed to the injection of scolocidal agent into the cyst before cystotomy and aspiration of the cyst content. The hypertonic sodium chloride solution 10% was always used as a scolocidal agent in our series without any complications or secondary hydatidosis.
Cystotomy or cystectomy followed by the obliteration of the residual cavity (capitonnage) were the most frequently used operative techniques: 59 and 25%, respectively. In addition, five patients (16%) underwent lung resection procedures: lobectomy in three cases due to the presence of destroyed lobe and segmentectmy in two patients who had complicated cyst (i.e. infected and/or perforated cyst). Enucleation procedure was not used in G1 because of the risk of rupture.
In G2, conservative surgical procedures (enucleation, cystectomy, cystotomy) were performed in 98% (21, 64 and 13%, respectively). Segmentectomy was used in two cases only. There was a correlation between the cyst’s size and the lung resection rate (P = 0.033) (Fig. 4).
For prophylactic purpose, we used albendazole at 10 mg/kg per day for 1–3 months in postoperative period.
There was no operative mortality in the two groups. Postoperative complications in G1 were seen in eight patients (25%). Five children had air leakage for more than 8 days in which two of them developed pleural empyema. However, no one requires rethoracotomy. Two patients had atelectasia and one patient wound infection. The complication rate was within 10% in G2 (9 patients) (P = 0.003).
Discussion
Echinococcosis constitutes an important health problem throughout the world, particularly in the Mediterranean area [1]. Hydatid lung cysts may reach very large dimensions due to the asymptomatic course of the cyst’s growth and the poor socioeconomic conditions. This explains delay in diagnosis and treatment. Generally, there is no accepted size to define a hydatid cyst as “giant” [2–4]. In our study, cysts more than 10 cm in the largest diameter were regarded as giant hydatid lung cysts.
In our study and in the literature review, giant lung hydatid cysts are more frequently encountered in children older than 10 years [2, 3]. It seems obvious that the size of the cyst increases as children grow into adolescence but many studies reported the fact that the growth rates of cysts may vary between cysts in the same organ or in the same individual and between individuals [5]. Moreover, it has been reported that the immune system and the relatively higher elasticity of the lung parenchyma in children and the adolescent allows the rapid growth of cyst and hence giant hydatid cysts are more commonly seen at these ages [4, 6].
The lung hydatid disease is frequently asymptomatic in children [2]. Nevertheless, giant lung hydatid cysts were constantly symptomatic in our series with a statistical significance comparatively to no giant lung hydatid cysts. In fact, the excessive hydatid cyst volume exerts higher pressures on surrounding tissues and causes more frequently cough, hemoptysis and thoracic pain due to parietal and bronchial irritation. Other symptoms have been reported in other studies such as dyspnea, malaise, nausea, and vomiting and thoracic deformations [3].
Chest X-ray is the radiologic exam of choice. It can show the giant hydatid cyst as a round opacity occupying a part of a hemithorax [7–9]. It is also helpful to display some signs such as cavity filled with air, air–fluid level and air–fluid level associated with “water-lily or meniscus signs” suggesting complicated cysts [1, 10, 11]. Thoracic CT scan is not mandatory; however, it displays better information about the cyst, surrounding structures and helps to exclude other differential diagnosis such as encysted pleurisy, pulmonary abscess, parietal tumor or mediastinal adenopathy. Inclusion of abdominal ultrasonography in the protocol of investigation is necessary because of the coexistence of hepatic cysts (15% in our series).
It is universally established that the surgical treatment of hydatidosis aims to eradicate the parasite, to prevent the intraoperative dissemination and to close the residual cavity [12]. However, there is no consensus that the affected lung parenchyma should be resected or treated by a parenchyma-saving procedure. For many authors, lung resection techniques are indicated whenever a large cyst involves more than 50% of the lobe or when the located lobe or lung tissue has been completely destroyed [6]. For others, parenchyme-saving operations can be also suitable for patients with giant hydatid cysts [2, 3, 12]. Indeed, the resection rate in giant lung hydatid cysts varies in the literature from 6 to 13%. Nevertheless, all of these studies include both adults and children. In our study, concerning only children under 16 years old, the resection rate was higher (16%). In our series, indications for resection were giant cysts involving the entire lobe, destroyed lung parenchyma or pulmonary abscess. This could be explained by the natural history of the disease. In fact, the insidious course of the pathology in children leads to massive parenchymal destruction. Whatever, we believe that conservative surgical methods should be attempted in all cases and resection procedures performed when after drainage of the cyst, the remaining lobe is seen to contain non-functional or destroyed parenchyma.
Postoperative complications are expected in patients with giant cysts because of the frequence of complicated cysts having communications with more bronchi. The complication rates reported in the literature varies between 17 and 19% in giant hydatid lung cysts [2, 3]. In our study, the complication rate was within 25% and it was statistically significant. However, there was no correlation between the location of the cysts or the age of patients and postoperative complications.
Albendazole have been recently used in the management of lung hydatid cyst as an alternative to surgical treatment particularly in small lung hydatid cysts. However, in giant lung hydatid cysts, response rate are generally low [13–15]. Thus, we believe that the medical therapy in giant hydatid cysts should be kept for inoperable cases due to anesthetic contraindications or combined with surgical treatment when there is a high risk of recurrence.
Conclusion
Giant hydatid lung cysts represent a distinct pathology. They affect essentially adolescents and may reach a large size causing parenchymal destruction. Thus, surgical resections are frequently used and postoperative complications rate is high.
References
Dogan R, Yüksel M, Cetin G (1989) Surgical treatment of hydatid cysts of the lung: report on 1055 patients. Thorax 44:192–199
Karaoglanoglu N, Kurkcuoglu NC, Gorguner M, Eroglu A, Turkyilmaz A (2001) Giant hydatid lung cysts. Eur J Cardiothorac Surg 19:914–917. doi:10.1016/S1010-7940(01)00687-X
Halezeroglu S, Celik M, Uysal A, Senol C, Keles M, Arman B (1997) Giant hydatid cysts of the lung. J Thorac Cardiovasc Surg 113:712–717. doi:10.1016/S0022-5223(97)70228-9
Lamy AL, Cameron BH, LeBlanc JG, Culham JA, Blair GK, Taylor GP (1993) Giant hydatid lung cysts in the Canadian northwest: outcome of conservative treatment in three children. J Pediatr Surg 28:1140–1143
Romig T, Zeyhle E, Macpherson CNL, Rees PH, Were JBO (1986) Cyst growth and spontaneous cure in hydatid disease. Lancet
Symbas PN, Aletras H (1994) Hydatid disease of the lung. In: Shields TW (ed) General thoracic surgery. Williams and Wilkins, Philadelphia
Hafsa C, Belguith M, Golli M (2005) Imagerie du kyste hydatique du poumon chez l’enfant. J Radiol 86:405–410
Anadol D, Gocmen A, Kiper N (1998) Hydatid disease in childhood: a retrospective analysis of 376 cases. Pediatr Pulmonol 26:190–196. doi:10.1002/(SICI)1099-0496(199809)26:3<190::AID-PPUL6>3.0.CO;2-P
Celik M, Senol C, Keles M, Halezeroglu S, Urek S, Haciibrahimoglu G et al (2000) Surgical treatment of pulmonary hydatid disease in children: report of 122 cases. J Pediatr Surg 35:1710–1713
Ozçelik C, Inci I, Toprak M (1994) Surgical treatment of pulmonary hydatidosis in children: experience in 92 patients. J Pediatr Surg 29:392–395. doi:10.1016/0022-3468(94)90575-4
Solak H, Yeniterzi M, Yüksek T (1990) The hydatid cysts of the lung in children and results of surgical treatment. Thorac Cardiovasc Surg 38:45–47
Hasdiraz L, Oguzkaya F, Bilgin M (2006) Is lobectomy necessary in the treatment of pulmonary hydatid cysts? ANZ J Surg 76:488–490. doi:10.1111/j.1445-2197.2006.03761.x
Morris DL, Marriner S, Bogan J, Burrows F, Skeene-Smith H, Clarkson MJ (1985) Albendazole: objective evidence of response in human hydatid disease. JAMA 253:2053–2057
Gil-Grande LA, Boixeda D, Garcia-Hoz F, Barcena R, Lledo A, Suarez E, Pascasio JM, Moreira V (1983) Treatment of liver hydatid disease with mebendazole: a prospective study of thirteen cases. Am J Gastroenterol 78:584–588
Senyuz OF, Yesildag E, Celayir S (2001) Albendazole therapy in the treatment of hydatid liver disease. Surg Today 31:487–491. doi:10.1007/s005950170106
Acknowledgments
The authors are sincerely thankful for Prof. Mohammed Benzagmout for his contribution in the manuscript.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Arroud, M., Afifi, M.A., Ghazi, K.E. et al. Lung hydatic cysts in children: comparison study between giant and non-giant cysts. Pediatr Surg Int 25, 37–40 (2009). https://doi.org/10.1007/s00383-008-2256-z
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00383-008-2256-z