Abstract
Aims
To study the incidence of and the factors associated with renal dialysis and transplantation in type 1 (T1DM) and type 2 diabetes (T2DM).
Methods
Data on individuals who had received dialysis treatment or renal transplant between 1 January 2004 and 31 December 2013 were extracted from the regional administrative database (Piedmont, Italy), and the crude (cumulative) incidence of dialysis was calculated. Overall cumulative survival was estimated using the Kaplan–Meier method and compared using the log-rank test. Poisson regression was used to estimate adjusted rate ratios for potential predictors of renal transplant or death.
Results
A total of 7401 persons started dialysis treatment during the decade, with a 10-year cumulative crude incidence of 16.8/100,000. Incidence was stable and consistently eightfold higher in persons with T2DM (tenfold higher in T1DM) compared to those without diabetes. The risk of dialysis in T1DM was about double that of T2DM. The mortality rate was significantly higher in diabetics than in non-diabetes (241.4/1000 vs. 153.99/1000 person-years). During the decade 2004–2013, 893 patients underwent a kidney transplant. Transplantation rates were significantly lower for diabetics than non-diabetics (16.5/1000 vs. 42.9/1000 person-years).
Conclusions
In the past decade, the incidence of dialysis has stabilized in both the general population and in diabetics in whom it remains far higher by comparison. Also mortality rates are higher, with a worse prognosis for T1DM. Diabetes poses a barrier to allotransplantation, and efforts should be made to overcome this limitation.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
The long-term complications of diabetes are a major cause of disability, reduced quality of life, and premature death [1]. Kidney disease plays a major role in this excess risk which is entangled with increased risk of cardiovascular disease [2, 3]. Diabetic kidney disease (DKD) is also the leading cause of end-stage renal disease (ESRD) in the Western world [4, 5] and one of the primary reasons for dialysis treatment and kidney transplantation. DKD is clinically diagnosed by screening for persistent increased urine albumin excretion and decreased estimated glomerular filtration rate. In addition to genetic determinants [6], hyperglycemia, dyslipidemia, elevated blood pressure, smoking, and hyperuricemia [7] are known risk factors for the onset and progression of DKD. However, the natural history and the specific risk factors of patients with DKD (i.e., not only classical diabetic nephropathy) who progress to ESRD and require dialysis or renal transplantation are poorly known or dated. Furthermore, little is documented about the role the two main types of diabetes [type 1 and type 2 diabetes mellitus (T1DM and T2DM)] play in modifying prognosis, particularly as regards the differences in the incidence and risk factors associated with renal replacement therapy (RRT), including trends in the last decade. Similarly, a data-based picture of access to and prognosis of allotransplantation and the extent to which it differs from dialysis in outcome and associated conditions (T1DM and T2DM) is missing.
To fill this gap, we retrospectively analyzed the data of a cohort of dialysis patients of an entire region (Piedmont, Italy) to reconstruct the history and characteristics of the process surrounding renal replacement in the comparison between patients with T1DM or T2DM and non-diabetic patients. A better knowledge of epidemiological data and identification of clinical predictors associated with renal replacement or mortality could be crucial to improve prevention and management strategies for ESRD in diabetic patients.
Subjects and methods
Study population and data sources
For this population-based study, we used regional administrative data from Piedmont, northwest Italy (population 4,400,000 inhabitants, approximately 7.5% of the national total). Healthcare data are stored in an automated system of databases that records outpatient healthcare services delivered (including dialysis treatment), as well as drug prescriptions and hospital discharges reimbursed by the National Health System. In respect of patient privacy, a unique anonymous identifier allows these archives to be linked together. Because the automated system is anonymous, ethical committee approval and informed consent were not required for this study.
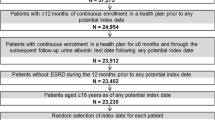
We extracted information from the regional database of outpatient treatments for all individuals who had received dialysis treatment between 1 January 2004 and 31 December 2013; an individual was defined as incident if he/she had not received dialysis treatment in the previous 12 months. Patients who were discharged from hospital with a diagnosis of acute kidney failure (ICD 9-CM: 584) or prescribed an immunosuppressive drug (ATC: L04) in the previous 12 months were excluded.
Comorbidities
The presence of diabetes at the incidence date of dialysis was obtained through record linkage with the Regional Register of Diabetes (RRD), and the type of diabetes was retrieved from the information entered in the RRD by the attending diabetologist [8]; type of antidiabetic therapy (oral hypoglycemic agent and/or insulin—ATC: A10) was retrieved via record linkage with the drug prescriptions database. A patient was defined as being on oral hypoglycemic therapy if he/she had filled at least two drug prescriptions in the previous 12 months. Data on existing cardiovascular disease (CVD) at the time of entering dialysis treatment were obtained by record linkage with the regional hospital discharge database, which contains data on hospitalization of Piedmont residents wherever they may be hospitalized in Italy. Patients discharged from hospital with a diagnosis (either primary or secondary) of coronary heart disease (ICD 9-CM: 410-414) or cerebrovascular disease (ICD 9-CM: 430-438) were defined as having CVD. Finally, we also examined the data on cardiovascular drug therapies prescribed to patients on entering dialysis treatment via record linkage with the regional drug prescriptions database; a patient was defined as being on pharmacotherapy for CVD if he/she had filled at least two prescriptions in the previous 12 months for any of the following: statins (ATC: C10AA), angiotensin-converting enzyme inhibitors (ACEi; ATC: C09A, C09B), angiotensin receptor blockers (ARBs; ATC: C09C, C09D), beta blockers (ATC: C07), diuretics (ATC: C03), and calcium channel blockers (CCP; ATC: C08).
Outcomes
Patients who started dialysis treatment were followed-up for kidney transplant and mortality. Information on renal transplant was obtained by record linkage with the regional hospital discharge database by selecting diagnosis-related group (DRG) codes 302 (only kidney) and 512 (kidney and pancreas transplantation). Data on death (or transfer out of Piedmont) were obtained by record linkage with the Unique Regional Archive of residents covered by the regional health system.
Statistical analysis
The crude (cumulative) incidence of dialysis was calculated by dividing the number of residents who started treatment between 1 January and 31 December of each year between 2004 and 2013 by the total number of residents alive on 31 December of each year. Incidence was standardized by age using Poisson regression; age classes (0–45, 46–55, 56–65, 66–75, 76–85, and over 85 years) and 95% confidence intervals were calculated.
The start of follow-up was defined as the date of incidence (i.e., the first dialysis treatment) and ended at the date of death or renal transplant or transfer out of Piedmont or 31 December 2013, whichever came first. We defined as lost to follow-up patients who moved out of the region during the study period (38 persons). Cases where a patient received a kidney transplant and subsequently died were considered as two distinct outcomes. Days of follow-up were calculated as the difference between the incidence date and the date of the event under study, loss to follow-up, death, and 31 December 2013. Person-time was calculated separately for each of the two outcomes.
Overall cumulative survival probability, and survival according to type of diabetes, was estimated with the Kaplan–Meier method and compared using the log-rank test. Poisson regression was used to estimate adjusted rate ratios (RR) for available potential predictors of kidney transplant or death: age classes (0–45, 46–55, 56–65, 66–75, 76–85, 85 years or older for mortality rate; age over 65 years was the last age class for kidney transplant rate), gender, type of diabetes, in case of T2DM, type of therapy at the incidence date (oral hypoglycemic agent alone, oral hypoglycemic agent plus insulin, insulin alone, unknown), CVD at incidence date of dialysis, and cardiovascular drug therapies other than antidiabetic drugs; moreover, two 5-year periods (2004–2008 and 2009–2013) were included in the model.
Statistical analyses were performed using SAS version 9.4 (SAS Institute Inc, Cary, NC, USA) and STATA version 13 (StataCorp LLC, College Station, TX, USA).
Results
We identified 7401 subjects who started dialysis treatment during the decade 2004–2013, with a 10-year cumulative crude incidence of 16.8/100,000 residents, which remained stable during the period. The 10-year average prevalence was 84.9/100,000, with slight variations from a minimum of 78.3 in 2004 to a maximum of 90.9 in 2011. Table 1 presents the baseline characteristics of the study population divided into two 5-year periods: 2004–2008 and 2009–2013 (49 and 51% of patients, respectively). The patient population in the second half of the decade was, on average, nearly 2 years older due to the increase in the number of persons over age 75, had a higher prevalence of T2DM (29.1 vs. 25%) but a similar prevalence of CVD; in both halves of the decade, 63% of the patients were men. The prevalence of pharmacologically treated patients was significantly higher in the second half of the decade for all the main therapeutic classes considered.
From 2004 to 2013, both crude and age and sex-adjusted incidence rates for dialysis treatment remained fairly steady 17.6/100,000 (adjusted: 33.1/100,000) in 2004 and 16.2/100,000 (adjusted: 29.8/100,000) in 2013 (Fig. 1), with no substantial variations (maximum of 18.0 in 2010 and minimum of 15.7 in 2007). Similarly, the incidence for patients with diabetes remained unchanged across the decade, albeit higher than for patients without diabetes: The incidence of dialysis treatment was consistently about eightfold higher in patients with T2DM and about tenfold higher in those with T1DM (wide annual fluctuations are due to the low number of patients with T1DM, as shown in Table 1) compared to those without diabetes, and the risk of dialysis for patients with T1DM was about twice that of patients with T2DM.
During the 10-year follow-up, a total of 893 out of 7401 patients received a kidney transplant (12% of the study population), with an overall transplant rate of 35.7/1000 person-years per year. In detail, 26 transplants in diabetic and 13 in non-diabetic patients were performed without prior dialysis and were excluded from the present analysis; 17 persons (14 with and 3 without diabetes) underwent double kidney transplantation. Transplant rates were significantly lower for patients with diabetes than for those without diabetes (16.5/1000 vs. 42.9/1000 person-years; p < 0.0001).
During the same period, a total of 4443 deaths out of 7401 patients (60% of the study population) were recorded for dialyzed patients and 73 for transplanted patients, 10 of which with T2DM and 4 with T1DM. The overall mortality rate was 177.8/1000 person-years and it was significantly higher for patients with diabetes than for those without diabetes (241.4/1000 vs. 153.99/1000 person-years; p < 0.0001). To better clarify this point, Fig. 2 shows the mean (unadjusted) survival of patients, with and without diabetes, receiving dialysis treatment: After 1 year from initiation of dialysis, 79% of patients without diabetes were alive, compared to 82% of patients with T1DM (difference not statistically significant, p = 0.8711) and 73% of patients with T2DM (difference statistically significant, p < 0.001). This disadvantage of patients with T2DM maintains for the whole period: After 5 years, 47% of patients without diabetes and 48% of T1DM patients were alive, compared to 29% patients with T2DM (Fig. 2).
Table 2 presents the crude and adjusted RRs for the two outcomes (renal transplantation and death). The likelihood of kidney transplant decreased steeply with increasing age in patients with established CVD and in patients with diabetes (both T1DM and T2DM), in which the likelihood of receiving a kidney transplant was half that of patients without diabetes. The risk of mortality increased with increasing age, in men, in patients with CVD and in those with diabetes, especially T1DM (RR 1.84, p < 0.05).
The results of multivariate analysis of post-transplantation mortality are not reported because inconsistent, given the very low number of events.
Discussion
In 2013, there were around 3.2 million patients being treated for ESRD worldwide, along with 700,000 living with kidney transplants [9]. In some countries, diabetic kidney disease is responsible for half of all new patients requiring renal replacement therapy (RRT). Initiation of dialysis treatment is a challenging time of transition for incident dialysis patients, their families and caregivers. It is also the beginning of a very costly procedure for the National Health Service and represents a relevant socioeconomic burden.
The incidence of dialysis treatment we found (168 patients per million population (pmp)) coincides precisely with the average incidence reported by other sources for Italy [10] and appears to be among the lowest in Europe [11, 12].
It remained stable for the decade between 2004 and 2013, suggesting that prevention efforts have been effective in halting the seemingly unstoppable growth of dialysis reported in the last decade of the 1990s [9].
In the last 5 years of the decade, the patient population was a little older, with a larger proportion of those with T2DM and a similar proportion of those with established cardiovascular disease. These last two aspects may reflect the global rise in T2DM prevalence and on the other hand the general reduction in CVD in the general population. Also patient management appears to have changed with time: In the last 5 years, more pharmacological treatments were reported and more patients were treated with oral hypoglycemic agents, insulin, and cardiovascular medications.
As expected, the incidence of dialysis treatment was consistently eightfold to tenfold higher (3.5–8-fold when age adjusted incidence is considered) in patients with diabetes compared to those without diabetes, yet, strikingly, the dialysis incidence rate by the presence of diabetes remained unchanged during the last 10 years. This finding contrasts with recent Austrian [13] data, suggesting that the reported 38% growth rate of diabetes-related ESRD may have slowed. Other older observations dating from 2007 for Australia–New Zealand [14] indicated a steady 10-year increment in the number of diabetes patients. In the UK [15], initiation of RRT in diabetes patients increased from 12.3 to 27.6 pmp between 1995 and 2009. While throughout the 1990s, nephrologists were reluctant to put diabetic patients on dialysis, the number of incident dialysis patients with diabetes increased up to 2010 followed by a sort of plateau as eligibility criteria for dialysis broadened. Our findings are in line with the 2016 official report of the European Renal Association-European Dialysis and Transplant Association (ERA-EDTA) [4] which pinpointed 2008 as the year when the rise in the incidence rate of RRT in the general population ended, as also seen for the subgroup of diabetic patients, and a slight reduction in incident cases began.
Although diabetic patients are referred earlier and develop fewer complications, the risk of dialysis for patients with T1DM was about twice that for patients with T2DM. Moreover, the risk of mortality increased with increasing age and was higher in men than women and in those with comorbidities. In the most recent paper on the subject published in 2011, Steenkamp [16], using figures based on the UK register, found that the unadjusted first year after 90-day survival for patients starting RRT in 2010 was 87.3%, representing a slight increase over the previous year (86.6%), and 84.7% in patients with diabetes. To attempt a comparison between those data and ours, it should be borne in mind that we included all incident dialysis patients regardless of age and that we did not exclude subjects who died during the first 90 days after initiation of dialysis: This may explain the seemingly lower survival rate in our cohort. Despite these differences in methodology, it could be roughly said that the figures do not differ so much. Notably, the adjusted 10-year risk of death for dialysis-treated patients with T1DM was 84% higher than for patients without diabetes. As a whole, these data point to the greater burden of renal complications in this type of diabetes.
A link emerged between insulin and oral hypoglycemic agents (OHA) use (alone or in combination) and mortality in patients with T2DM. This finding is neither new nor surprising. In the last years, numerous observational studies have found insulin to be a marker of poor outcomes, including mortality. A plausible explanation is that there is a typical indication bias, without any causal role. In other words, these therapies are likely to reflect the gravity of disease.
As expected history of CVD appears to be a negative prognostic factor for mortality, confirming that CVD is the leading cause of death in all dialyzed subjects.
The likelihood of dialysis-treated patients receiving a kidney transplant decreased with increasing age, and patients with diabetes (irrespective of type of diabetes and therapy) had half the chance of undergoing surgery. Indeed, patients with T2DM and ESRD are less likely to be selected for renal transplantation because they are generally thought to be more complex and burdened with more comorbidities. This, however, is not confirmed by the relative risks reported in Table 2 where, despite the multivariate model controlling for comorbidities, the probability of transplantation remains low. Also CVD emerged as a negative factor for transplantation, very likely for the same reasons. Interestingly, no correlations were found for sex, type of diabetes, and cardiovascular therapy (except for patients treated with ACE inhibitors). As regards mortality in transplanted patients, 73 deaths (8.2%) were recorded following transplant, a figure in line with other recent observations [17].
The main strength of this study is the completeness of data on treatment, procedures, hospitalization, and mortality rates of the population of an entire region, and the reliable algorithm for retrieving treated patients. The main limitation is the lack of clinical data, since we were unable to link patient prognosis to disease characteristics.
In conclusion, this study provides an in-depth update on RRT and renal transplantation. Our data show that the incidence of dialysis treatment has stabilized, whereas the percentage of diabetic patients appears to have reached a plateau. Nevertheless, mortality rates are higher for diabetic patients regardless of age, with T1DM showing the worst prognosis. We found that diabetes still poses a barrier, probably unjustified, to allotransplantation. Efforts should be made to overcome this limitation.
References
The Emerging Risk Factors Collaboration (2011) Diabetes mellitus, fasting glucose, and risk of cause-specific death. N Engl J Med 364:829–841
D’Errico MM, Mangiacotti A, Graziano D et al (2017) Kidney disease measures are associated with the burden of coronary atherosclerosis, independently of diabetes. Acta Diabetol 54(11):1065–1068
Bacci S, Gargano A, di Lorenzo A et al (2016) Urinary albumin excretion correlates with carotid intima-media thickness in offspring of patients with type 2 diabetes and albuminuria. Acta Diabetol 53(6):1045–1048
Pippias M, Jager KJ, Kramer A et al (2016) The changing trends and outcomes in renal replacement therapy: data from the ERA-EDTA Registry. Nephrol Dial Transplant 31(5):831–841. https://doi.org/10.1093/ndt/gfv327
Foley RN, Collins AJ (2007) End-stage renal disease in the United States: an update from the United States Renal Data System. J Am Soc Nephrol 18:2644–2648
De Matthaeis A, Di Lorenzo A, Gargano A et al (2016) Chronic inflammation in offspring of patients with type 2 diabetes and albuminuria. Acta Diabetol 53(1):125–126
Hayashino Y, Okamura S, Tsujii S et al (2016) Association of serum uric acid levels with the risk of development or progression of albuminuria among Japanese patients with type 2 diabetes: a prospective cohort study [Diabetes Distress and Care Registry at Tenri (DDCRT 10)]. Acta Diabetol 53(4):599–607
Gnavi R, Karaghiosoff L, Dalmasso M, Bruno G (2006) The Piedmont Diabetes Register: opportunities and limits for epidemiological purposes. Epidemiol Prev 30(1):59–64
http://archive.eucomed.org/disease-sectors/community-homecare/dialysis. Last Access March 2018
Nordio M, Limido A, Conte F et al (2016) Italian Registry Dialysis and Transplant 2011–2013. 33(3) (Article in Italian)
Ward MM (2008) Socioeconomic status and the incidence of ESRD. Am J Kidney Dis 51(4):563–572. https://doi.org/10.1053/j.ajkd.2007.11.023
Connor TM, Oygar DD, Gale DP et al (2013) Incidence of end-stage renal disease in the Turkish-Cypriot population of Northern Cyprus: a population based study. PLoS ONE 8(1):e54394. https://doi.org/10.1371/journal.pone.0054394
Prischl FC, Auinger M, Säemann M et al (2015) Austrian Dialysis and Transplant Registry. Diabetes-related end-stage renal disease in Austria 1965–2013. Nephrol Dial Transplant 30(11):1920–1927. https://doi.org/10.1093/ndt/gfv113
Villar E, Chang SH, McDonald SP (2007) Incidences, treatments, outcomes, and sex effect on survival in patients with end-stage renal disease by diabetes status in Australia and New Zealand (1991–2005). Diabetes Care 30(12):3070–3076
Hill CJ, Fogarty DG (2012) Changing trends in end-stage renal disease due to diabetes in the United Kingdom. J Ren Care 38(Suppl 1):12–22. https://doi.org/10.1111/j.1755-6686.2012.00273.x (Review)
Steenkamp R, Shaw C, Feest T (2013) UK Renal Registry 15th annual report: chapter 5 survival and causes of death of UK adult patients on renal replacement therapy in 2011: national and centre-specific analyses. Nephron Clin Pract 123(Suppl 1):93–123. https://doi.org/10.1159/000353324
Neovius M, Jacobson SH, Eriksson JK, Elinder CG, Hylander B (2014) Mortality in chronic kidney disease and renal replacement therapy: a population-based cohort study. BMJ Open 4(2):e004251. https://doi.org/10.1136/bmjopen-2013-004251
Acknowledgements
CBG and RG contributed to the literature search, study design, data collection, data interpretation, and writing; PC and RP helped in data analysis and interpretation; MS and GC contributed to data interpretation; and BT helped in the literature search and writing support. Dr. Carlo Giorda is the guarantor of this work and, as such, had full access to all the data in the study, and takes responsibility for the integrity of the data and the accuracy of the data analysis. He confirms that all authors consent to publication of this manuscript. There is no funding to report for this submission.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical standard
This is an observational study and data were collected retrospectively. The Local Health Authority of Piedmont region was responsible for collecting and processing these data. The study was commissioned by the Local Health Authority. No ethical approval was required according to Italian law 211/2003, which explains that no ethics committee permission is required for this kind of study.
Informed consent
According to Italian privacy law, no patient’s or relative’s consent is required for large retrospective population-based studies and if data are published only in aggregated form.
Additional information
Managed by Antonio Secchi.
Rights and permissions
About this article
Cite this article
Giorda, C.B., Carnà, P., Salomone, M. et al. Ten-year comparative analysis of incidence, prognosis, and associated factors for dialysis and renal transplantation in type 1 and type 2 diabetes versus non-diabetes. Acta Diabetol 55, 733–740 (2018). https://doi.org/10.1007/s00592-018-1142-y
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1007/s00592-018-1142-y